Abstract
Superspreaders are critical infectious resources in multiple infectious diseases. They can be asymptomatic or present mild symptoms but can transmit pathogens to susceptible populations, leading to severe symptoms, and even death. Early identification of this population is extremely important to inhibit the spread of infectious diseases. Right now, the whole global world is suffering from a devastating infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In this article, a superspreader cluster event in coronavirus disease 2019 (COVID-19) was identified by tracking contacting histories of infected patients. This cluster was found to be originated from an asymptomatic SARS-CoV-2 carrier, which resulted in 13 secondary cases getting infected. All the secondary patients presented with non-typical symptoms of COVID-19, such as fever, dry cough, and myalgia, one of which died of respiratory failure at the end. From this cluster, we learn that people with older ages, low immunity, multiple underlying diseases, especially pulmonary diseases, can contribute to a poor prognosis. Thus, asymptomatic superspreaders of COVID-19 can be extremely dangerous and must be handled time-efficiently.
Keywords: Asymptomatic, Coronavirus, COVID-19, SARS-CoV-2, Superspreader
Introduction
Coronavirus is an enveloped single-stranded and positive-sensed helical RNA virus belonging to the Orthocoronavirinae family. It can be widely distributed in humans, other mammals, birds, and bats, leading to acute and persistent infections.1 In December 2019, there were multiple cases of non-typical pneumonia found in Wuhan, China, many of them were found having an exposure history to Huanan Seafood Supermarket.2 The pathogen was finally determined to be a novel coronavirus through virus isolation and gene identification. On 2020, January 12th, the World Health Organization (WHO) denominated this virus to be 2019 Novel Coronavirus (2019-nCov). Until Jun 17th, 2020, more than 8,214,571 cases have been confirmed in the global world and 444,853 patients died of novel coronavirus disease (COVID-19) in 176 countries from Johns Hopkins Coronavirus Research Center, a real-time updated data bank.3 A total of 2,141,306 cases are confirmed and 117,033 cases are dead of COVID-19 in the United States. COVID-19 now has been a global pandemic, millions of people are struggling to survive. Innumerable people are facing up to unemployment, and the global economy is suffering a devastating setback.
In the early hypothesis related to the interactions between host and pathogens, scientists believe that infected people may have an equal chance to transmit pathogens to secondary cases. However, some scientists observe there is a 20/80 rule existing in infectious diseases, which is believed that 20% of infected cases contribute to 80% of infected cases.4 This 20/80 rule is applicable in many transmissions of infectious pathogens among different species. A basic reproductive number named R0 is a fundamental epidemiological parameter to characterize infectious disease outbreaks, it indicates an average number of secondary infections originated from an index individual during the whole period of infectious disease, suggesting the severity of infectious diseases.4 R0 of COVID-19 is estimated to be 2 to 4 which is quite similar to influenza.5 However, a group of people named superspreaders can transmit pathogens disproportionately to more than an average number of secondary cases, and are likely to promote the speed and scale of outbreaks.6,7 Usually, superspreaders transmit at least 10 individuals, sometimes even up to 100 secondary cases.6
Superspreaders are recorded in the histories of multiple infectious diseases. Two superspreaders are reported in Hong Kong epidemic in coronavirus induced severe acute respiratory syndrome (SARS) in 2003. The first index patient was estimated to infect at least 138 secondary cases since March 3rd, 2003 in the Prince of Wales Hospital.8 The number of people infected by the second index patient was not clear, however, it was estimated at least 300 people were infected with the contact of this patient.6 Three superspreaders also occurred in Middle East respiratory syndrome coronavirus (MERS-CoV) occurred in 2015. The first superspreader transmitted the virus to a total of 27 secondary cases in the same hospital, and the second and third superspreaders infected at least 73 and 24 tertiary cases, respectively.9 Ebola virus belongs to the filovirus family and leads to severe hemorrhagic fever in human beings with a mortality rate of 90%. It had a devastating outbreak in Western Africa in 2014–2015. This outbreak can be traced back to several superspreaders who contributed to the secondary cases.7 There are a few case reports about the superspreaders in COVID-19 as well. From recent news, an England businessman, who might be infected in Singapore when having a conference, headed to France, Switzerland, and England consequently, resulting in at least 11 secondary cases infected.10,11 Moreover, a superspreader in Korea infected at least 37 people during a church-related and daily-routine activity.12 Another Indian preacher, who just had a trip from COVID-19 epicenter Italy and Germany, went preaching in at least 10 villages in Punjab State without any self-isolation until this patient felt ill and died. Because of him, 19 people have been confirmed 2019-nCov positive, more than 200 people are waiting for the testing results, and at least 15,000 people have to be under a strict quarantine.13
Although superspreaders are rare cases in plenty of infectious diseases, early identification of superspreaders is very significant in reducing infected cases and preventing outbreaks. Here, we report a superspreader cluster from Chongqing, an asymptomatic index patient transmitted to 13 persons unintendedly, and whether other individuals get infected are still unknown. This superspreader patient A was not found first. However, many secondary cases were discovered initially from the same family, all of them had a close contacting history with patient A who had a recent travel history from Wuhan and did not show any symptoms. Thus, this asymptomatic patient A was excavated and deemed to be a superspreader of COVID-19. From learning this superspreader event cluster, we highly recommend identifying superspreaders timely by tracking contacting histories from infected cases as early as possible to prevent consequent transmission and outbreaks.
Materials and methods
Study design and participants
All patients enrolled in this study agreed and signed the consent forms. This retrospective study was approved by the Ethics Committee of The First Affiliated Hospital from Chongqing Medical University and Chongqing University Three Gorges Hospital. All 2019-nCov positive results were confirmed by qRT-PCR from the throat swab specimen. All results of clinical tests were collected from electronic medical systems from Chongqing University Three Gorges Hospital. These patients are the secondary cases infected from the superspreader patient A, and were not intendedly divided into different treatment groups. They received antivirus treatments according to their medical conditions. The superspreader was identified after tracing back contacting histories from those secondary cases. The most common antivirus treatment for those COVID-19 patients were lopinavir 200 mg & ritonavir 50 mg, 1 or 2 tablets, q12 h or tid, or abidol, 0.2 g tid, or hydroxychloroquine 0.4 g, qd; thymopentin was also applied to enhance the immunity of the patients.
Results
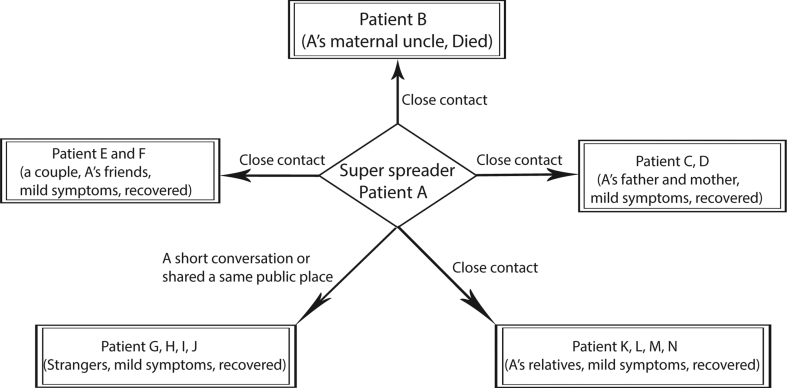
This superspreader event involved in 13 known secondary cases (Fig. 1). After a close contact, the patient A's father, mother, maternal uncle, four other relatives and his two friends were infected. Another two saleswomen and two customers in the supermarket were infected only by a short conversation or just a pass-by with the superspreader patient A. All these secondary cases manifested non-specific and respiratory symptoms, such as a low-degree fever, cough, fatigue, headache, and muscle ache, with a patchy opacity or ground-glass lesions in both lungs shown in chest computed tomographic (CT) scan, except his maternal uncle (patient B), who presented a severe respiratory failure and died at last.
Figure 1.
A superspreader cluster event. Patient A is the asymptomatic superspreader. B–N are the secondary infected cases.
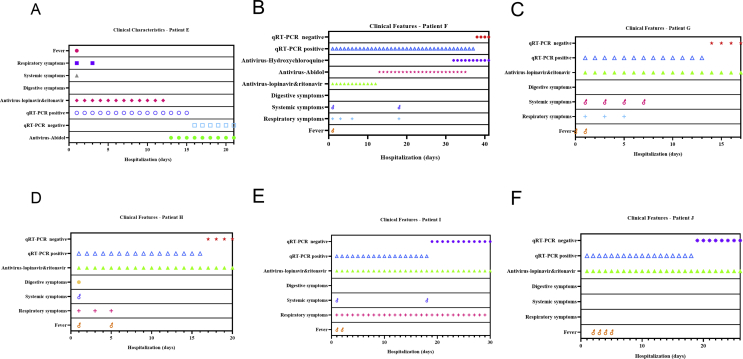
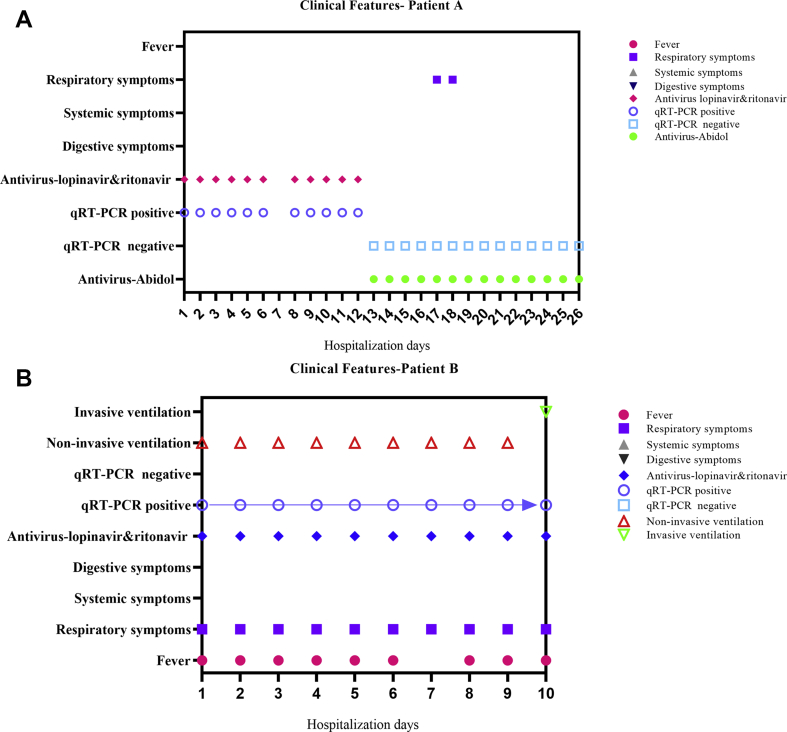
These secondary cases were discovered initially. Patient E (male, 34 years old) was detected as 2019-nCov positive by the nucleic acid test after 7 days of close contact with index patient A, and presented with fever, headache, dry cough at the 10th day. The latent period was around 10 days. Antivirus therapy lasted 21 days, and the nucleic acid test turned into negative after 15 days of antivirus therapy. The total length of hospital stay was 21 days. Patient F (female, 28 years old) was patient E's wife and tested as 2019-nCov positive after 7 days of close contact with patient A. She manifested with fever, headache, dry cough, fatigue, chest distress on the 10th day after the contact. The latent period was 10 days, antivirus therapy lasted 41 days, and the nucleic acid test turned into negative after 37 days of antivirus therapy. The total length of hospital stay was 41 days. Patient G and H were sales-service staff working in a supermarket where they had a short conversation with patient A 7 days ago before patient G and patient H's onset of clinical symptoms. Patient G (female, 47 years old) showed fatigue, fever, poor appetite, wet cough, chest pain, and distress after a short conversation with patient A. She stayed in the hospital for 17 days and was received a 17-day antivirus therapy. The nucleic acid test turned into negative after 13-day treatment with antivirus. The latent period was 7 days. Patient H (female, 36 years old), presented with low-degree fever, poor appetite, fatigue, headache, muscle ache after close contact with patient A, the antivirus and total length of hospital stay was 20 days, and the nucleic acid test turned into negative after 16 days of antivirus treatment. The latent period was 7 days. Patient I and J brushed past patient A in the supermarket and got infected. Patient I (female, 36 years old) presented with low-degree fever, cough with yellow sputum, short of breath exacerbated with activity. The total length of hospital-stay and antivirus treatment was 30 days, and the nucleic acid test turned to negative after 18-day antivirus treatment. The latent period was 11 days. Patient J (female, 15 years old) only showed low-degree fever but without any respiratory or symptomatic symptoms. The total length of hospital-stay and antivirus treatment was 26 days, and the nucleic acid test turned into negative after 18-day antivirus treatment. The latent period was 14 days. Other infected patients' medical information was not collected due to different hospitalization. All their clinical information is shown in Fig. 2. The time length ranged from close contact to the onset of clinical symptoms and positive nucleic acid tests, and the time-length of turning into negative nucleic acid tests after anti-virus treatment is summarized in Fig. 3.
Figure 2.
The clinical features of each secondary case during their hospitalization. (A) clinical feature of patient E. (B) clinical features of patient F. (C) clinical features of patient G. (E) clinical features of H. (E) clinical features of patient I. (F) clinical features of patient J.
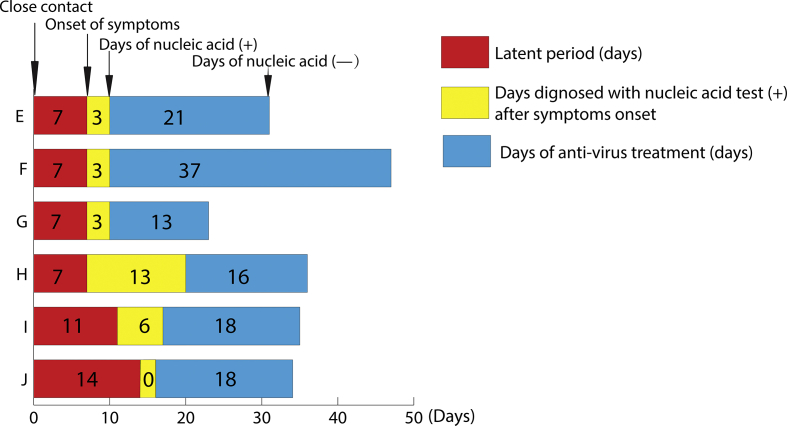
Figure 3.
The latent periods of COVID-19, the days of symptoms onset, the days that nucleic acid test was positive, and the days that nucleic acid test was negative after antivirus treatments from the secondary patients E, F, G, H, I, J. Red indicates the latent periods of SARS-CoV-2 infection after the close contact between the secondary patients and the superspreader patient A. The joint between red and yellow indicates the onset time of COVID-19 symptoms. The end of yellow bar indicates how many days the patients were received the nucleic acid tests and it was positive after the onset of symptoms. Blue indicates how many days of anti-virus treatments were used to turn the nucleic acid test into negative. The end of the blue bar indicates the time of the nucleic acid test turned into negative.
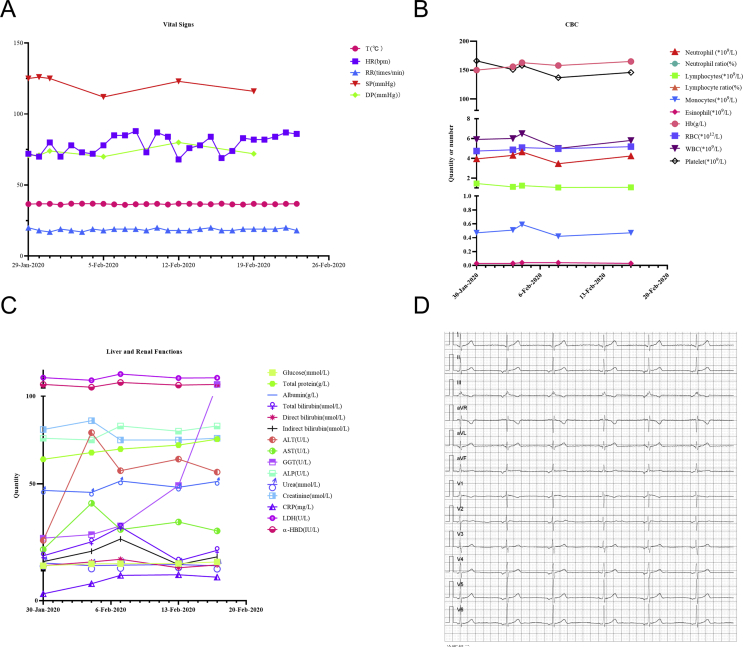
After collecting medical histories from those secondary patients, the superspreader (patient A) was identified. He was a young man aged 24 and had a recent living history in Wuhan. He was tested to be positive of 2019-nCov with oropharyngeal sample on Jan 26th, 2019, which was 19 days after his return from Wuhan. During this period, although no symptoms presented, he carried the virus and floated to several places. When admitted to hospital, his vital signs were not significant (Fig. 4A). He had a history of hepatitis B, dyslipidemia, hypoglycemia, and slight liver dysfunction (Fig. 4B and C). His ECG showed there was a junctional escape rhythm (Fig. 4D). Patient A was diagnosed as the mild type of COVID-19 (The diagnosis criteria are, 1. Mild clinical manifestations. 2. No significant pneumonia presentation in imaging tests) according to The Diagnosis and Treatment Guideline for COVID-19 in China (the sixth edition).14 . The total hospital stay and antivirus treatment lasted 26 days, his temperature ranged from 36.3 °C to 37 °C, no other symptoms were presented except for occasionally chest discomfort and dyspnea last only two days. His nucleic acid test was still positive after a 12-day antivirus treatment with lopinavir & ritonavir. Thus, abidol hydrochloride was used to replace lopinavir & ritonavir and the nucleic acid test turned into negative immediately after using abidol (Fig. 5A). Six times of chest CT scan was performed during the hospital-stay which lacked significant features of COVID-19 infection, such as ground-glass or patchy lesions, except multiple solid nodules in both lungs related to old lesions which were not altered after antivirus treatment (Fig. 6A and B). From this case, we know that long-term usage of lopinavir & ritonavir combining with abidol might be a potential therapeutic treatment for COVID-19.
Figure 4.
Clinical tests from patient B. (A) the result of the vital signs. (B) the result of complete blood count (CBC) test. (C) the test result of liver and renal functions. (D) the electrocardiograph. All these tests were performed during the hospitalization.
Figure 5.
The clinical features from patient A (superspreader) and patient B. (A) patient A. (B) patient B.
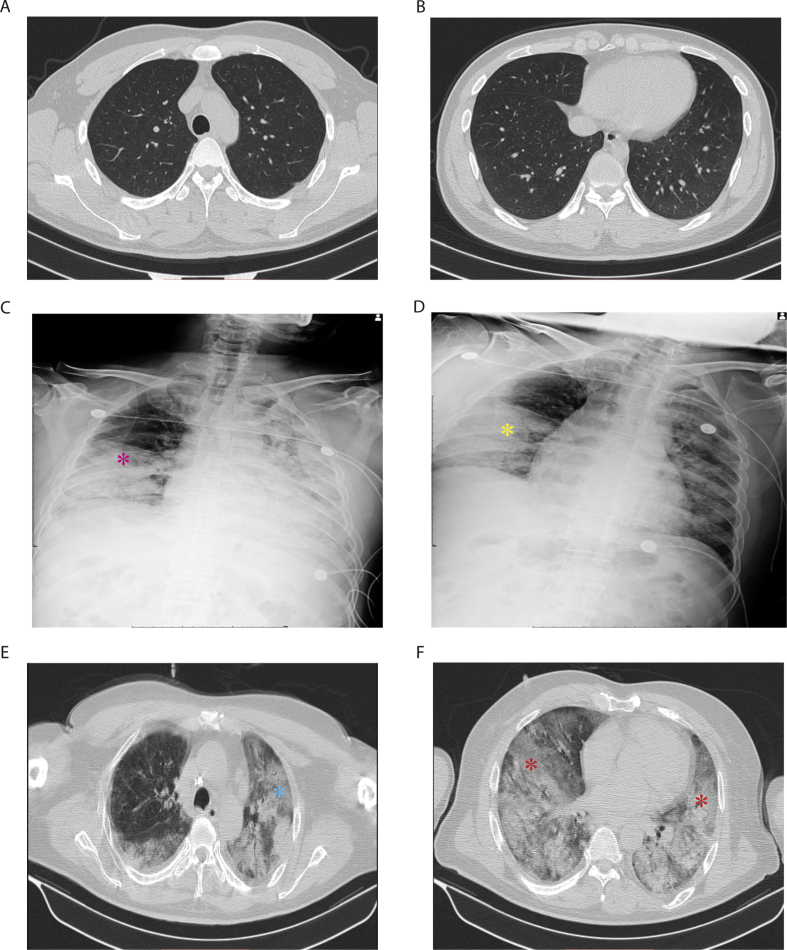
Figure 6.
(A) and (B) are the chest CTs from the asymptomatic super spreader patient A when admitted. There are no significant COVID-19 patchy lesions in this patient. (C) and (D) are the X-rays from Patient B on an 26th, Jan 27th, 2020, respectively. The pink dot indicates the patchy lesions in the inferior lobe of right lung (C). The yellow dot indicates the aggravation of the patchy lesion as the progression of the infection. (E) and (F) are the chest CTs from patient B on Jan 29th, 2020, which is four days before his death. The ground-glass lesions can be seen in blue (E) and red dots (F).
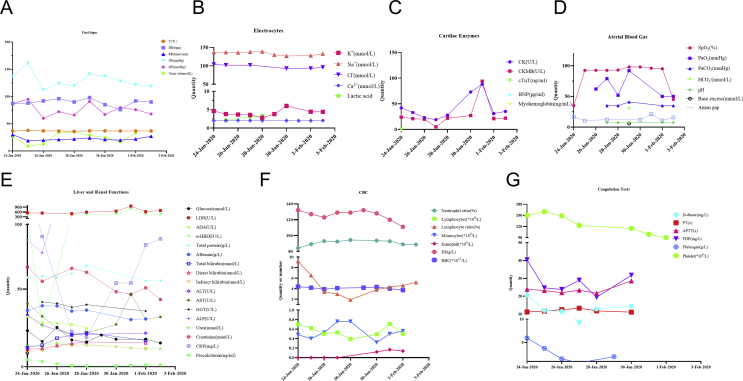
Patient B (male, 52 years old) was patient A's maternal uncle. He had a close contacting history on Jan 9th, 2020 with patient A who just returned from Wuhan. After a 10-day latent period, patient B had a fever, palpitation, shortness of breath, which were exacerbated especially after activities and could be relieved after taking rest. Before Jan 24th, 2020, the patient was transferred to several hospitals and diagnosed with severe pneumonia, type I respiratory failure, diabetic ketosis, type II diabetes mellitus, hepatitis B, steatohepatitis, hypoproteinemia, subclinical hypothyroidism, and treated with supportive measurements. The patient B was diagnosed with 2019-nCov positive with the nucleic acid test by Local Center for Disease Control and Prevention, and transferred to Chongqing University Three Gorges Hospital for further treatment on Jan 24th, 2020 where the total length of stay was 10 days. His vital signs were stable when admitted. Body examination demonstrated rales in both lungs. Antivirus treatments were started immediately after admission. Antibiotics against bacteria were used in this patient since he had an increased neutrophils. Methylprednisolone was used for anti-inflammation. Non-invasive ventilator was used to assist ventilation. H1N1 and influenza B were tested negative. ECG showed no other significant changes except for an electrical alteration. His nucleic test was continuously positive after admission (Fig. 5B). The chest X-ray on Jan 26th and 27th, 2020 indicated interstitial changes in both lungs, scattered patchy lesions with blurred edges in the middle and inferior right lung and the whole left lung, and a small amount of pleural infusion in both left and right cavities (Fig. 6C and D). Chest CT on Jan 29th, 2020 showed an increased density of interstitial patchy lesions (Fig. 6E and F). His blood pressure was 161/95 mmHg, temperature was 37.8 °C, and respiration rate was 30 times/min during the admission; During a 10-day hospitalization, his temperature ranged from 36.1 °C to 37.8 °C, and respiration rate ranged from 20 to 30 times/min. All his results of clinical tests are shown in Fig. 7. A five-day blood-culture indicated negative for aerobic and anaerobic bacteria. As the infection progressed, the patient suddenly lost consciousness and presented shallow breathing with a dropped blood oxygen saturation to 38% at the 10th day. This patient unfortunately demised from respiratory failure even a positive cardio-pulmonary resuscitation was administered.
Figure 7.
All these tests are from patient B during the hospitalization. (A) the vital signs. (B) the result of the electrocyte test. (C) result of cardiac enzymes. (D) result of arterial blood gas test. (E) the result from liver and renal functions. (F) the result of CBC test. (G) the result of coagulation test.
Although the number of these collected secondary cases are small and limited, we can see the incubation periods were around 7 days–14 days for those secondary cases getting infected from an asymptomatic superspreader based on their medical histories. The treatment with lopinavir 200 mg & ritonavir 50 mg, 1 or 2 tablets, q12 h or tid, or abidol, 0.2 g tid, or hydroxychloroquine 0.4 g, qd; combined with thymopentin were able to reverse positive nucleic acid tests of 2019-nCov to be negative. Most of the secondary cases infected from the superspreader of COVID-19 may have a good prognosis. However, superspreaders can be asymptomatic or present mild symptoms, but can transmit 2019-nCov to susceptible populations. Susceptible populations with older ages, lower immunity, multiple underlying diseases, especially pulmonary diseases, tend to present a poor prognosis. Thus, asymptomatic superspreaders of COVID-19 can be an extremely dangerous source of infection and must be handled time-efficiently. Wearing face masks can be an efficient method to protect susceptible populations.
Discussion
COVID-19 is an undergoing global pandemic and has triggered the global health emergency alert at present. It is controversial whether 2019-nCov is originated from bats or other animals.15 Subsequently, this virus is majorly transmitted by person-to-person in terms of aerosol. However, the oral-fecal method, close contact, secreted fluids can be routes of transmission as well.16, 17, 18 Some study shows that sialic acid is an extracellular glycosylated protein with a ubiquitous component, which is a critical receptor for coronavirus.19 The spike protein on SARS-CoV (severe acute respiratory syndrome-associated coronavirus) has an intense binding affinity with human ACE2 demonstrated by biochemical interaction and crustal structure.20 The spike protein on 2019-nCov shares a similarity of 76.5% in amino acid sequences with SARS-Cov.21 ACE2 on pneumocytes II is the receptor of viral S spike, that's the reason why 2019-nCov attack the respiratory system rather than other systems, which can be a potential target for therapeutic treatment.22,23 However, no evidence shows whether ACEI or ARB therapeutic drugs may impact the progression of this virus.
Highly attention must be paid to non-symptomatic carriers since they are one of the most important infection origins and can markedly transmit the virus to other individuals.24 Superspreaders are a group of people who have mild or even no symptoms, but carry a large number of pathogens and can transmit pathogens to at least 10, or even 100 individuals after their onset of diseases. Multiple reasons can lead to a superspreader event. Firstly, superspreaders may carry a higher dose of virus with a higher virulence and a higher affinity to human cells rather than the normal populations. Secondly, a close contact or droplets transmission by talking, coughing, sneezing, touching a contaminated surface, sharing food or a closed space, contacting the same public facility, such as handles in the office or subway, buttons in elevators, all are very common transmission ways in our daily lives. Thirdly, the pathogen is brand-new and everyone is susceptible and easily infected. Fourthly, specific age, gender, gene susceptibility, underlying diseases, low immune status, living habits, sleeping deprivation, are all contributors to a superspreader event. In American traditional culture, healthy people tend not to wear face masks, which is also a contributing factor to the rapid spreading of 2019-nCov. Fifthly, misdiagnosis, delayed hospital admission, and inter-hospital transfers can lead to a superspreader event as well. Lastly, a closed and poorly ventilated environment facilitates the transmission of pathogens. Other reasons, such as co-infection with other pathogens, alterations of airflow dynamics, immunodeficiency, or use of immunodepression drugs are all causes leading to a superspreader event.4 Thus, it is extremely important to identify superspreaders at the beginning stage.
However, since superspreaders are usually identified by a retrospective study in epidemiology, it is very difficult to discover those groups of spreaders at the early onset of diseases. How can we identify superspreaders timely? Firstly, the whole-genome sequencing and proteomics might be ideal methods to determine the gene and protein features of pathogens, to discover virulence factors, replication-related enzymes, or endocytosis and exocytosis associated proteins of the pathogens. Secondly, tracking contacting histories from the secondary and tertiary infected individuals can be very useful to understand transmission methods and incubation time. Thirdly, cell phone apps. Infected individuals can use cell phone apps to remotely record and report their contacting histories, the onset of diseases, symptoms to the medical system. As infectious diseases have various latent periods, it will be easier to track infected individuals.
There are several strategies to prevent or reduce the superspreader event. Firstly, making an early diagnosis. The best way to prevent a superspreader event is to make early diagnosis of superspreaders, isolate and treat them as early as possible. Secondly, reducing regional migration and enhancing surveillance. These methods are crucial strategies to reduce a superspreader event.25 The outbreak of COVID-19 occurred right before and during the Chinese Spring Festival when three billions of people were traveling throughout the country, which is an inevitable trigger to the outbreak.26 Thirdly, reducing the inter-hospital transfer of infected patients. Forthly, wearing personal protective equipment is extremely helpful, such as face masks, gloves, safety glasses, shoe covers. Wearing a face mask is super important since it reduces the spreading pathogens from the infected population, cuts off the transmission route, and protects the susceptible population. The reason why Taiwan, Japan, and Korea have good control of COVID-19 with a low prevalence and incidence is that all of their nations wear face masks before the outbreak. As medical suppliers are in an urgent shortage, self-made face masks are highly recommended when go to public places. Fifthly, decrease unnecessary exposure to crowded public places or social gatherings. Sixly, disinfect working and household areas with specialized sanitizer. Seventhly, wash hands frequently. Lastly, keep social distancing.
Why individuals infected from the same COVID-19 superspreader have a different prognosis? There are multiple reasons. 1. Age. Age plays a significant role in the progression of COVID-19. The mortality rate increases as age increases. It is reported that the mortality rate is under 1% when younger than age 60. However, it is increased to approximately 3%, 8% and 15% in age groups of 60–70, 70–80, and over–80, respectively.5 From our clinical cases, the superspreader patient A was 24 years old, and the secondary cases infected 2019-nCov aged between 20 and 50, except the expired patient B aged 52.2. Comorbidities. All patients infected from patient A were healthy without any other significant underlying diseases. However, the expired patient B had several comorbidities, such as poorly-controlled diabetes mellitus, diabetic ketosis, tuberculosis, HBV infection, and hypoalbuminemia. All these comorbidities exacerbated the poor prognosis. 3. Complications. Multiple complications may deteriorate the progression of COVID-19. The patient B might have severe secondary pulmonary bacterial infection, which aggravated the poor prognosis. 4. Virus virulence. Strong virus virulence may lead to severe clinical consequences rather than weaker ones. 5. Exposure time to the infected resource. The longer exposure it is, the higher risk might be. 6. Delayed diagnosis. The timely diagnosis and reasonable treatment were delayed in patient B since he was transferred to several hospitals, which also contributed to his poor prognosis.
In summary, superspreaders are critically important infected populations usually presenting asymptomatic or mild symptoms, however, they contribute most secondary infected cases. Highly attention must be paid to superspreaders. Moreover, making a timely diagnosis and isolating superspreaders in the early stage, tracking contacting histories, and cutting off transmission methods are highly recommended. Finally, wearing face masks is highly encouraged which can be a crucial strategy to reduce further spreading of 2019-nCov.
Contributors
Xuejing Yu conceived and wrote the manuscript. Dongchuan Ran and Jinhui Wang contributed to the study design and literature research. Yuan Qin contributed to the collection and interpretation of chest CT. Ruishan Liu, Xueli Shi, Yiping Wang, Chang Xie, and Jia Jiang were responsible for collecting medical histories and sorting medical data. Jianzhong Zhou contributed to the study design and providing a guide for writing the manuscript.
Conflict of interest
We declare no competing interests.
Acknowledgment
We really appreciate those patients involved in this study to share the valuable epidemic information to the public. In the meantime, we are very grateful to all the medical staff in the frontline combating with 2019-nCov. It's them risking their lives to guard and protect the health of all our human beings.
Footnotes
Peer review under responsibility of Chongqing Medical University.
References
- 1.Paul S., Masters S.P. Coronaviridae. Field Virol. 2013;28:825. [Google Scholar]
- 2.Chen N., Zhou M., Dong X. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coronavirus Covid-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins Univeristy (JHU) 2020. [Google Scholar]
- 4.Stein R.A. Super-spreaders in infectious diseases. Int J Infect Dis. 2011;15(8):510–513. doi: 10.1016/j.ijid.2010.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mark N. 2020. A Seattle Intensivist's One-Pager on COVID-19. [Google Scholar]
- 6.Riley S., Fraser C., Donnelly C.A. Transmission dynamics of the etiological agent of SARS in Hong Kong: impact of public health interventions. Science. 2003;300(5627):1961–1966. doi: 10.1126/science.1086478. [DOI] [PubMed] [Google Scholar]
- 7.Wong G., Liu W., Liu Y., Zhou B., Bi Y., Gao G.F. MERS, SARS, and ebola: the role of super-spreaders in infectious disease. Cell Host Microbe. 2015;18(4):398–401. doi: 10.1016/j.chom.2015.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee N., Hui D., Wu A. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348(20):1986–1994. doi: 10.1056/NEJMoa030685. [DOI] [PubMed] [Google Scholar]
- 9.Cowling B.J.P.M., Fang V.J., Wu P., Leung G.M., Wu J.T. Preliminary epidemiological assessment of MERS-CoV outbreak in South Korea, May to June 2015. Euro Surveill. 2015:7–13. doi: 10.2807/1560-7917.es2015.20.25.21163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Super-spreaders: What Are They and How Are They Transmitting Coronavirus?.
- 11.UK Coronavirus 'superspreader' Says His Thoughts Are with Those Infected. 2020. [Google Scholar]
- 12.'Superspreader' in South Korea Infects Nearly 40 People with Coronavirus. 2020. [Google Scholar]
- 13.India Quarantines 15,000 after 'super-Spreader' Dies of Virus. 2020. [Google Scholar]
- 14.The Diagnosis and Treatment Guideline for COVID-19 in China (The Sixth Edition) 2020. [Google Scholar]
- 15.Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang J., Wang S., Xue Y. Fecal specimen diagnosis 2019 novel coronavirus-infected pneumonia. J Med Virol. 2020 doi: 10.1002/jmv.25742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 18.Xia J., Tong J., Liu M., Shen Y., Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020;92(6):589–594. doi: 10.1002/jmv.25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The beginning and end of the virus replication cycle. Basic Virol. 2007:85. [Google Scholar]
- 20.Li F., Li W., Farzan M., Harrison S.C. Structure of SARS coronavirus spike receptor-binding domain complexed with receptor. Science. 2005;309(5742):1864–1868. doi: 10.1126/science.1116480. [DOI] [PubMed] [Google Scholar]
- 21.Xu X., Chen P., Wang J. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 2020;63(3):457–460. doi: 10.1007/s11427-020-1637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.To K.F., Tong J.H., Chan P.K. Tissue and cellular tropism of the coronavirus associated with severe acute respiratory syndrome: an in-situ hybridization study of fatal cases. J Pathol. 2004;202(2):157–163. doi: 10.1002/path.1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jia H.P., Look D.C., Shi L. ACE2 receptor expression and severe acute respiratory syndrome coronavirus infection depend on differentiation of human airway epithelia. J Virol. 2005;79(23):14614–14621. doi: 10.1128/JVI.79.23.14614-14621.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pan X., Chen D., Xia Y. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. Lancet Infect Dis. 2020;20(4):410–411. doi: 10.1016/S1473-3099(20)30114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zeliang Chen W.Z., Lu Yi, Guo Cheng. From SARS-CoV to wuhan 2019-nCoV outbreak: similarity of early epidemic and prediction of future trends. BioRxiv. 2020 [Google Scholar]
- 26.Scholes G.D., Li G., Ma Y., Wang J., Zheng J. Chinese spring festival editorial. J Phys Chem Lett. 2019;10(3):701. doi: 10.1021/acs.jpclett.9b00263. [DOI] [PubMed] [Google Scholar]