The coronavirus disease 2019 (COVID-19) pandemic exposed numerous deficiencies of the US primary care infrastructure. The system is overstretched with little to no surge capacity to deal with crisis situations, its reach restrained due to overreliance on brick-and-mortar clinics, and its behavior overwhelmingly more reactive than preventive. Even before the outbreak, US primary care physicians faced excessive patient panel sizes in an environment of a workforce shortage.1 , 2 Without enough time to provide all the necessary acute, chronic, and preventive care for their patients, primary care physicians are forced to prioritize acute care; not surprisingly, patients receive only half of all the recommended chronic and preventive care services.3 On top of these, stunning disparities in access, quality, and affordability of primary care persist, especially in rural and vulnerable populations where doctors are in short supply.4 These system failures — however damaging during normal times — have been magnified exponentially by the unprecedented challenge of COVID-19.
As primary care systems reorganize on the fly to fight COVID-19, many are turning to tools such as telemedicine, pre-visit planning, and centralized population health management. Telemedicine has been indispensable in delivering care to patients sheltered at home, while minimizing risks to providers. Before COVID-19, only 28% of US physicians were using telemedicine5; today it is the preferred, if not dominant, method of delivering care.6 Pre-visit planning strategies such as clinic schedule sweeping, pre-visit screening of patients, and triaging visit priorities — once regarded as “nice-to-have” protocols — have been adopted as “must-haves” quickly and widely. Systems that have been flirting with centralizing their population health services to improve care quality have accelerated their transitions to free up primary care physicians to handle the surge of COVID-19 patients. These rapid transformations happening in health systems across the country, born out of necessity, present an opportunity — a silver lining — to fix primary care.
A Paradigm Shift for Telemedicine
When all is done, the COVID-19 pandemic will likely be seen as a tipping point for telemedicine in the United States — the point when it was no longer considered a niche service, but an essential piece of care delivery. At one institution — Stanford University — the volume of telehealth and video visits leaped from 400 per day to 3000 in a period of just 2 weeks when the pandemic hit California. Nationally, widespread telemedicine adoption was powered by the loosening of payer restrictions by Medicare and some private insurances.7 The longer COVID-19 lasts, the more it will push the envelope on the breadth, depth, and comprehensiveness of care that can be accomplished through virtual visits. What we need now is a national telemedicine curriculum to be taught in residencies and medical schools,8 , 9 and for Congress to make coverage for telemedicine visits permanent.
Let Patients Help Their Providers With Patient-Generated Data
Since the start of the COVID-19 pandemic, nurses have held the primary care front lines. Nurses assess, advise, and direct patients to the most appropriate level of care, conserving access to physicians for those who need them most. They follow-up and monitor COVID-19 patients for clinical deterioration. Nurses are a scarce resource. Tools such as Apple’s COVID-19 screening app, created with the Centers for Disease Control and Prevention, gather patient-generated data and help patients contextualize their symptoms and determine if they need to see a clinician.10 This general approach of using patient-generated data to connect patients with the right level of care when, where, and how they need it should be broadened to all primary care intake processes. Integration of technology-assisted tools including symptom-checker apps, Web-based screeners, and wearable devices into health systems’ electronic health records (EHRs) holds promise to make the most of every precious encounter between patients and physicians.
Prevention Will be Ignored if Not Done Between Visits
The COVID-19 pandemic led to a dramatic shift in operational priorities from improving general population health and chronic disease management to identifying patients with and at risk for the virus. Nearly all preventive care has been postponed and chronic disease management programs scaled back or put on hold. These inter-visit efforts require significant time and resources that are not currently available. Before the COVID-19 pandemic, systems were slow to adopt centralized strategies that leverage team-based care and technology, despite demonstrated benefits on quality of care.11 The post-COVID-19 era presents a crucial opportunity to overcome the hurdles of culture change in a time when systems are pressured to reimagine nearly all aspects of daily work. The alternative to prioritizing and centralizing preventive care is to exhaust our already overextended teams, asking them to catch up for lost time once systems emerge from this pandemic.
Future Directions and Challenges
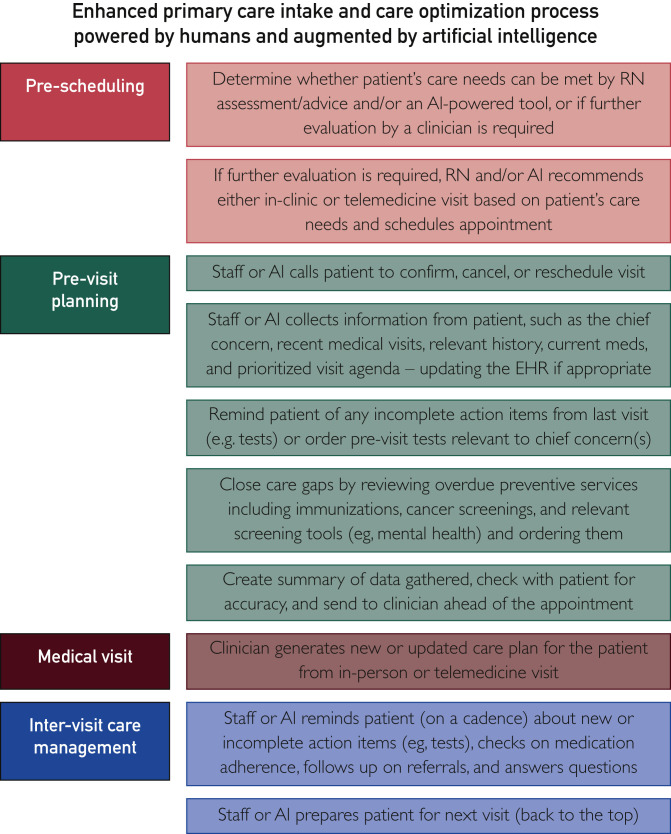
Integrating telemedicine, patient-generated data, and preventive care into a retooled primary care intake and care optimization process is achievable (Figure ). Such an approach would be powered by humans and augmentable by artificial intelligence.12 Up until the recent loosing of restrictions on virtual care, the primary barriers to telemedicine adoption were payer coverage and regulatory limitations. Looking to the future, the lack of reimbursement for pre-visit planning and inter-visit care management activities will be a key driver of change. Human and technical challenges exist: for patients, convenience, privacy, and data security are chief concerns; for providers, fears about data overload, technology/EHR interoperability, and workflow integration are paramount. Health systems’ willingness to invest in primary care teams, relaxation of rules around patient-generated data use, workforce training, and advancement to value-based payments are necessary to achieve this vision.
Figure.
Enhanced primary care intake and care optimization process powered by humans and augmented by artificial intelligence. AI = artificial intelligence; EHR = electronic health record; RN = registered nurse.
Primary care must retool to meet the challenge of COVID-19 and emerge in the post-crisis world better equipped to care for a wounded nation, and possibly millions of patients who have delayed usual care for months on end. Although issues of over-empaneled providers, workforce shortage, and disparities in access, quality, and affordability of care will not disappear after COVID-19; we can use tools such as telemedicine, pre-visit planning, and population health management — powered by humans and artificial intelligence — to expand primary care’s reach in all communities, increase system capacity and visit efficiency, and prioritize prevention to keep patients healthy. The COVID-19 pandemic taught us valuable lessons. Let us not squander this opportunity to make primary care better.
Acknowledgments
The authors thank Ms Grace Hong for assistance with the figure.
Footnotes
See alsopage 1835
Potential Competing Interests: Dr Lin serves as the Chair of the National Telemedicine Curriculum Task Force for the Society of Teachers of Family Medicine (STFM) in a volunteer role. STFM had no role in the preparation of this manuscript or the decision to approve publication of the manuscript. The remaining authors report no potential competing interests.
Supplemental Online Material
References
- 1.Altschuler J., Margolius D., Bodenheimer T., Grumbach K. Estimating a reasonable patient panel size for primary care physicians with team-based task delegation. Ann Fam Med. 2012;10(5):396–400. doi: 10.1370/afm.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Association of American Medical Colleges The Complexities of Physician Supply and Demand: Projections from 2017 to 2032. https://www.aamc.org/system/files/c/2/31-2019_update_-_the_complexities_of_physician_supply_and_demand_-_projections_from_2017-2032.pdf Updated April 2019. Accessed April 1, 2020.
- 3.McGlynn E.A., Asch S.M., Adams J. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 4.Agency for Healthcare Research and Quality . 2018. 2018 National Healthcare Quality and Disparities Report.https://www.ahrq.gov/research/findings/nhqrdr/nhqdr18/index.html Updated October 2019. Accessed April 1, 2020. [Google Scholar]
- 5.American Medical Association Physicians’ motivations and requirements for adopting digital health: adoption and attitudinal shifts from 2016 to 2019. https://www.ama-assn.org/system/files/2020-02/ama-digital-health-study.pdf Updated February 2020. Accessed April 1, 2020.
- 6.Topol E. Telemedicine is essential amid the COVID-19 crisis and after it. The Economist. https://www.economist.com/open-future/2020/03/31/telemedicine-is-essential-amid-the-covid-19-crisis-and-after-it Updated March 31, 2020. Accessed April 1, 2020.
- 7.Centers for Medicare & Medicaid Services Medicare Telemedicine Health Care Provider Fact Sheet. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet Updated March 17, 2020. Accessed April 1, 2020.
- 8.American Medical Association AMA encourages telemedicine training for medical students, residents. https://www.ama-assn.org/press-center/press-releases/ama-encourages-telemedicine-training-medical-students-residents Updated June 15, 2016. Accessed April 1, 2020.
- 9.Theobald M., Brazelton T. STFM Forms Task Force to Develop a National Telemedicine Curriculum, from STFM. Ann Fam Med. 2020;18(3):285–286. [Google Scholar]
- 10.Centers for Disease Control and Prevention CDC Statement on COVID-19 Apple App. https://www.cdc.gov/media/releases/2020/s0327-statement-covid-19-apple-app.html Updated March 27, 2020. Accessed April 1, 2020.
- 11.Ashburner J.M., Horn D.M., O’Keefe S.M. Chronic disease outcomes from primary care population health program implementation. Am J Manag Care. 2017;23(12):728–735. [PubMed] [Google Scholar]
- 12.Lin S.Y., Mahoney M.R., Sinsky C.A. Ten ways artificial intelligence will transform primary care. J Gen Intern Med. 2019;34(8):1626–1630. doi: 10.1007/s11606-019-05035-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.