Abstract
Health-care workers are crucial to any health-care system. During the ongoing COVID-19 pandemic, health-care workers are at a substantially increased risk of becoming infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and could come to considerable harm as a result. Depending on the phase of the pandemic, patients with COVID-19 might not be the main source of SARS-CoV-2 infection and health-care workers could be exposed to atypical patients, infected family members, contacts, and colleagues, or live in communities of active transmission. Clear strategies to support and appropriately manage exposed and infected health-care workers are essential to ensure effective staff management and to engender trust in the workplace. These management strategies should focus on risk stratification, suitable clinical monitoring, low-threshold access to diagnostics, and decision making about removal from and return to work. Policy makers need to support health-care facilities in interpreting guidance during a pandemic that will probably be characterised by fluctuating local incidence of SARS-CoV-2 to mitigate the impact of this pandemic on their workforce.
Introduction
An adequate level of staffing is crucial to maintain patient care during the ongoing COVID-19 pandemic.1 Frontline health-care staff assess and manage patients with COVID-19, patients presenting with emergencies not related to COVID-19, and patients with essential routine care needs. One of the greatest risks to the health-care system is a high rate of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection among health-care workers and the consequent lack of skilled staff to ensure a functioning local or regional response to the pandemic.2 This risk has been increased by the need for rapid scaling up of intensive care unit (ICU) capacity in affected regions, the redeployment of clinical staff to frontline positions (eg, ICUs or COVID-19 wards), and the recruitment of less experienced staff (eg, newly qualified students or health-care staff moving from their specialism) to the workforce in response to the pandemic.3, 4
Health-care workers could acquire SARS-CoV-2 at work through direct or indirect contact with infected patients or other health-care workers, or as a result of ongoing community transmission. Community transmission of SARS-CoV-2 is targeted by public health measures, whereas infection by patient or health-care worker contact is primarily addressed by facility-based infection prevention and control (IPC) measures. However, sources of infection might not be clear and this uncertainty can have negative effects on the clinical workforce. IPC measures are extensive in hospitals managing patients infected with SARS-CoV-2 and, broadly speaking, include rigorous cleaning and disinfection to reduce environmental contamination and the use of personal protective equipment (PPE), isolation, and cohorting.5
National and international recommendations for risk assessment and management of hospital health-care staff working with patients infected with SARS-CoV-2 are detailed and publicly available.6, 7, 8, 9 However, recommendations might not be easily transferrable because health-care systems are highly variable in terms of their structure and workforce composition.10 Available guidance can become rapidly unsuitable when the situation at the frontline of health-care delivery is continuously changing. Therefore broad recommendations need to be translated into locally applicable and pragmatic solutions. In this Personal View, we outline and discuss possible approaches to inform development of local policy related to health-care worker exposure and management during the COVID-19 pandemic.
Risk of SARS-CoV-2 infection in the clinical workforce
Several emerging viral diseases are known to have had a major effect on health-care workers, which is currently being observed also with SARS-CoV-2.11, 12 In an early case series from Wuhan, China, 29% of patients with SARS-CoV-2 were health-care workers and were assumed to have acquired the infection in hospital.13 Deaths among health-care workers infected with SARS-CoV-2 are rare and have mostly affected those older than 50 years.14, 15 Tragically, health-care workers rehired from retirement to help at the frontline have commonly experienced the highest mortality when compared with their working-age counterparts.16, 17 With an increasing understanding of the disease, the proportion of health-care workers contracting COVID-19 in hospital has decreased, but stringent IPC measures and continued vigilance are needed.18
The risk profile for SARS-CoV-2 exposure and infection among health-care workers differs substantially from other groups. In designated COVID-19 wards or hospitals, health-care workers are at high risk of infection. Potential exposure to SARS-CoV-2 is inherent to their work and is prevented only by excellent adherence to all IPC measures, including the use of appropriate PPE. There is uncertainty about what is optimal PPE, but it is clear that standardised and rigorous application of PPE and other IPC measures can dramatically reduce nosocomial transmissions.19, 20
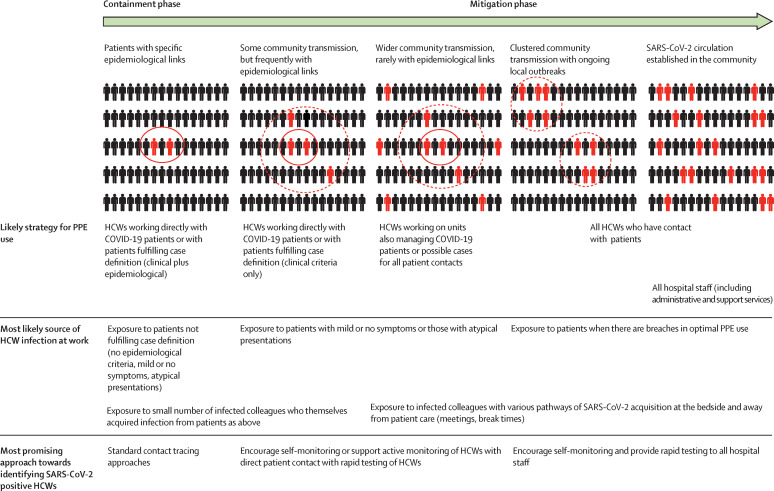
Health-care workers are likely to be in contact with patients and colleagues who have atypical, few, or no symptoms while still being highly contagious.21, 22, 23 A high proportion of such individuals will be present in the hospital, including in areas with insufficient awareness or identified need of IPC measures, as the virus spreads (figure ). Particular attention is needed for health-care workers looking after patients who are highly dependent and live in long-term care facilities, which may be built to resemble home-like environments, compromising the ability to apply stringent PPE and other IPC measures.24 Similarly, the presence of oligosymptomatic health-care workers infected with SARS-CoV-2 in situations during which PPE is not usually applied, such as scheduled meetings, grand rounds, educational events, and break times, will become more likely as the pandemic progresses.25
Figure.
Representation of the interaction between phases of SARS-CoV-2 public health management, PPE use in acute care hospitals, transmission patterns, and approach to evaluation of HCWs
HCWs=health-care workers. PPE=personal protective equipment. SARS-CoV-2=severe acute respiratory syndrome coronavirus 2.
Finally, with increasing community transmission, the highest risk of SARS-CoV-2 exposure for health-care workers could be outside of the hospital. Many health-care workers will contract SARS-CoV-2 through interactions with infected family members or other close contacts, or from the community in areas with active, unmitigated transmission.26, 27 Improper PPE use, suboptimal adherence to IPC measures, and having a family member with COVID-19 can double or triple the risk of subsequent health-care worker SARS-CoV-2 infection.28 A detailed study of the prevalence of SARS-CoV-2 among mildly symptomatic health-care workers in Dutch hospitals shows that many infections were most likely acquired in the community.29, 30
SARS-CoV-2 infection risk stratification
Defining the risk of a health-care worker being infected with SARS-CoV-2 can be the first step towards selecting the most appropriate monitoring and evaluation approach.6, 8, 9, 31, 32 Risk categories for in-hospital exposures are frequently based on the type of contact that has taken place and whether PPE was used consistently and appropriately. Additional specifications are sometimes included in risk assessment algorithms—eg, presence during aerosol-generating procedures or exact distancing from patients with COVID-19 (usually closer or further than 2 m).31, 33
Focusing on adherence to PPE implies that the optimal PPE for all potential contact situations is known and available. However, the effect of optimal PPE and other IPC measures is being debated because robust evidence to match PPE and IPC interventions to the risk profile of a given exposure is scarce.34, 35, 36 Exposures to SARS-CoV-2 via community cases and infected colleagues can be frequent depending on the phase of the outbreak. Risk assessment of health-care worker exposure, in our opinion, is going to be most useful in epidemic phases with low rates of community transmission. In all other situations, all health-care workers should be considered at moderate to high risk of contracting SARS-CoV-2, especially when extended IPC measures, including some use of PPE, cannot be implemented for all patient contacts and staff interactions. Data showing that viral shedding and potential SARS-CoV-2 transmission could occur 2–3 days before symptom onset highlight the importance of wearing adequate PPE in hospitals during phases of high SARS-CoV-2 incidence.37 Therefore, risk-appropriate PPE and optimal adherence to IPC measures will reduce the risk of health-care worker infection to that encountered in the community.
Monitoring of health-care workers at risk of SARS-CoV-2
Guidance provided by Peking Union Medical College Hospital (Beijing, China) suggests that all health-care workers in close contact with patients with COVID-19, regardless of PPE use, should undergo nasopharyngeal and oropharyngeal PCR testing and a full blood count after an unspecified block period of work in the designated area.38 Further management decisions are determined by the results of these tests but, if negative, health-care workers are monitored for 1 week and could resume work after this time if asymptomatic.
Calls have been made by health-care workers to improve availability of testing for asymptomatic health-care staff and allow screening.39 In our opinion, this approach has the distinct disadvantage of requiring very frequent evaluation, given that intermittent testing might not capture asymptomatic SARS-CoV-2 positive individuals. For example, in a case series of 13 patients with asymptomatic SARS-CoV-2 infection, eight were RT-PCR negative up to 14 days after first identification of SARS-CoV-2 and could well have been missed by fortnightly screening.40 We therefore do not favour regular general SARS-CoV-2 testing of health-care workers by PCR as an effective monitoring approach.
An alternative to intermittent PCR testing is to adopt a responsive approach to monitoring health-care workers. Most national monitoring systems incorporate some form of daily (self) screening for fever and assessment of respiratory symptoms.6, 9, 33, 41, 42 Stringent documentation and reporting requirements are an additional burden on health-care workers who are already stretched by the demands of patient care. Active symptom monitoring by public health authorities or their delegates of health-care workers deemed at risk of SARS-CoV-2 infection in occupational health is not feasible once an epidemic is in the exponential phase. Self-monitoring and reporting are more feasible but must be combined with excellent communication from occupational health officers to ensure that health-care workers feel adequately supported and have a point of contact to discuss any concerns or questions. Very low threshold access to occupational health to report any feelings of illness is crucial. Health-care workers might be concerned about whether such symptoms could indicate SARS-CoV-2 infection and might be reluctant to report mild symptoms because they feel that they are burdening the system. Furthermore, even mild symptoms can be indicative of SARS-CoV-2 infection, as shown when enhanced access (whereby all people with any respiratory symptoms or generalised symptoms suggestive of an infection are invited for testing) to testing was made available at a group of hospitals in the Netherlands.43 Direct access to occupational health has the additional advantage of enabling some psychosocial screening of the effect of working during the COVID-19 pandemic.
Confirming SARS-CoV-2 infection: diagnostic evaluation of health-care workers
Testing should be made available widely to symptomatic health-care workers and auxiliary acute health-care staff. The importance of supporting health-care worker access to SARS-CoV-2 testing in the case of symptoms cannot be overemphasised, particularly when the source of infection shifts from individual patients who are clearly identifiable to widespread viral transmission. Interactions with colleagues who are also at increased risk of exposure and infection could become classed as high-risk procedures.
During the period of unmitigated community transmission in the UK, access to testing for health-care workers, including those with symptoms, could not be guaranteed at a time when the medical workforce was under severe pressure from soaring SARS-CoV-2 cases. After roll-out in a single UK National Health Service trust, 18% of symptomatic staff tested positive for SARS-CoV-2 in the first 2 weeks of the test being available, showing that there is potentially a large pool of infected individuals working in hospitals in a setting with sustained community transmission.44
Many countries prioritise health-care workers for SARS-CoV-2 testing, often on the basis of reported symptoms and regardless of a confirmed exposure. For example, Switzerland and the Netherlands recommend rapid access to SARS-CoV-2 PCR testing and results for health-care workers because this information is used for decision making about deployment of medical staff.45, 46
Decision making on health-care worker removal from and return to work
The most suitable approach towards managing removal from and return to work of health-care workers depends on the pursued public health strategy (ie, containment or mitigation) and the current pressures on the health-care system.
During containment, standard quarantine and isolation should also be applied to health-care workers given that a special provision for health-care workers is unlikely to be necessary or helpful. Premature redeployment of quarantined or isolated health-care workers will probably be needed only in exceptional cases—eg, for highly specialised staff.
When testing of all symptomatic individuals cannot be guaranteed, as is often the case in a mitigation phase, PCR testing of symptomatic health-care workers should be prioritised and can be used to reduce workforce depletion caused by quarantine and isolation of symptomatic health-care workers. The pressures on a given health-care system are considerable; however, it is difficult to justify a special status for health-care workers from a public health perspective because of the bidirectional nature of SARS-CoV-2 infections among this group. Although health-care workers can acquire SARS-CoV-2 at work, introducing transmission into the community, they may also bring SARS-CoV-2 into the hospital following community exposures. PCR testing of asymptomatic quarantined health-care workers will provide false reassurance for exposed individuals with early negative results who go on to develop disease later on in the defined quarantine period.
The role of PCR testing is different for symptomatic individuals. Home isolation periods range from a minimum of 7 days (under certain conditions) in France and the UK, to 14 days in Germany and Italy, and isolation is often recommended independently of whether SARS-CoV-2 has been identified by testing. In most cases, an additional requirement of at least 48 h without symptoms before ending isolation is also specified. In the Netherlands, infected health-care workers who are considered crucial for the care of patients with COVID-19 can return to work after 24 h without symptoms, so shorter isolation periods are conceivable.6, 8, 31, 42, 45, 46 PCR testing of health-care workers should be used to ensure that isolation of symptomatic staff is limited to individuals who have been confirmed as SARS-CoV-2 positive.39, 45
In some cases, PCR testing is recommended to support rapid return to work of infected health-care workers if they become negative on PCR before the isolation period has elapsed. For example, German guidance recommends that health-care workers who required hospital treatment can return to work immediately if two PCR tests at least 24 h apart are negative.31, 47 In Switzerland, re-testing of health-care workers infected with SARS-CoV-2 at the end of the isolation period is proposed for those working in high-risk areas (haemato-oncology, ICUs, transplant units) and those with prolonged disease.45
There is considerable uncertainty about the relevance of prolonged detection of SARS-CoV-2 on PCR testing for transmissibility; therefore, the role of repeat testing to determine redeployment of health-care workers after SARS-CoV-2 infection is unclear. For health-care workers with confirmed SARS-CoV-2 infection, testing at the end of the isolation period is sometimes used to confirm suitability for return to work, often with two PCR tests at least 24 h apart.42, 48
However, in practice, these recommendations are problematic. A study comparing RT-PCR testing and virus culture found that patients with mild symptoms were positive by RT-PCR for up to 28 days, whereas no infectious virus could be recovered after day 10 post illness onset.49 Therefore, a symptom-based algorithm that informs when isolated health-care workers should return to work appears to be best when exposed or infected health-care workers are considered crucial to service maintenance and extended periods of quarantine or isolation are not feasible. Studies are ongoing to assess the possible role of serology as a marker for viral clearance in people with mild illness.
Navigating the effect of the management strategy on health-care workers
The exact algorithm for managing exposed and infected health-care workers should aim to safeguard staff wellbeing and reduce onwards transmissions to colleagues and patients without undermining the ability to maintain an adequate service, which is often a difficult balance. The exact configuration of the health-care setting and IPC strategies will affect the success of the management strategy and might require different approaches during different phases of the pandemic, especially when the use of PPE and sources of health-care worker infection are shifting (table ).
Table.
Advantages and disadvantages of HCW monitoring, evaluation, and management during the COVID-19 pandemic
| Advantages | Disadvantages | |
|---|---|---|
| Monitoring HCW contacts | ||
| Risk assessment of HCW contacts | Can identify HCWs at considerable risk of acquiring SARS-CoV-2 in the health-care setting and focus resources on active monitoring or proactive laboratory testing; can support implementation of quarantine measures for a specific group of HCWs, minimising the effect on the workforce and maximising containment of SARS-CoV-2 within the health-care environment | Can reduce awareness that interactions with any patients with COVID-19 (known or unknown) carry some risk of nosocomial transmission to HCWs; can be confusing when understanding of the optimal PPE remains unclear; can undermine HCW engagement with key IPC measures other than PPE (eg, hand hygiene and physical distancing) in the erroneous belief that these are ineffective; might not be relevant in settings where some level of PPE is universally recommended (eg, wearing of surgical masks for all patient contacts) and there is high adherence to other IPC measures |
| Use of (self)quarantine after contact | Can maximise containment of SARS-CoV-2 within the health-care environment, especially in HCWs who may have no, few, or atypical symptoms; can reduce HCW anxiety about contracting SARS-CoV-2 in the workplace from colleagues with known exposure | Can rapidly deplete the workforce, particularly in cases of HCWs infected with SARS-CoV-2 exposing many colleagues or when there is uncontrolled community transmission, with HCWs exposed outside of the hospital; might not be relevant in settings where some level of PPE is universally recommended (eg, wearing surgical mask for all patient contacts) and there is high adherence to other IPC measures |
| Symptom monitoring of HCWs | ||
| Active (eg, at the start of shifts or through regular telephone or email reporting) | Can support the reliable reporting of signs and symptoms compatible with SARS-CoV-2 infection; can lead to earlier identification of symptomatic HCWs, and therefore support targeted timely testing to reduce exposure of colleagues and patients; can be an opportunity to interact with HCWs about their general psychological and physical wellbeing to provide wider support | Can present a considerable administrative and resource challenge, depending on the exact method of active monitoring and selection of HCWs who undergo active monitoring; can lead to a rapid depletion of staff if minor symptoms lead to (self)isolation without SARS-CoV-2 testing; might be a drain on resources, especially in cases of clusters involving multiple HCWs and in settings where large sections of a hospital are dedicated to the care of patients with COVID-19 |
| Self-monitoring | Can reduce the barrier to HCW SARS-CoV-2 testing, if a simple algorithm is combined with clear advice on how to access testing; can involve the majority of HCWs in one facility, thereby detecting SARS-CoV-2 cases among personnel resulting from known and unknown exposures within and outside of the health-care setting; can be supported using digital tools, such as symptom monitoring apps | Can be unreliable if HCWs do not consider self-monitoring sufficiently important, or do not disclose symptoms when present, or when atypical or very mild symptoms are frequent among affected HCWs; can lead to a rapid depletion of staff if minor symptoms lead to (self)isolation without SARS-CoV-2 testing; might be ineffective unless clear contacts in occupational health or their delegates are defined and accessible to advise on required measures when symptoms are detected |
| SARS-CoV-2 testing of HCWs: identification of cases | ||
| Regular testing (screening) | Can detect asymptomatic or mildly symptomatic cases and can reduce the risk of nosocomial transmission to other staff and patients; can provide an opportunity to check in at regular intervals with occupational health or other public health authority delegates | Can have a major impact on testing capacity depending on volume and frequency of HCW testing, potentially with few cases detected; can provide insufficient information if done intermittently, because positive HCWs might have been infected for an unknown period of time before being sampled and negative HCWs could become positive in the time between tests; might increase the sense of insecurity among staff if large numbers of asymptomatic or mildly symptomatic positive HCWs are identified, when the relevance of this finding for onward transmission is unclear (especially in settings with universal PPE for all patient contacts and high adherence to other IPC measures); can engender a potentially misdirected sense of security to staff |
| Responsive testing (to symptoms) | Can support rapid identification of HCWs infected by SARS-CoV-2 to provide adequate clinical support and inform self-isolation; can provide a sense of security to staff working in close proximity with colleagues (eg, ICUs, operating theatres, emergency departments); can represent an efficient use of resources, especially if the threshold for accessing testing is low, sampling is carried out rapidly after onset of symptoms, and results are available in a timely fashion | Can lead to delays in identification of symptomatic SARS-CoV-2 positive HCWs by relying on (self-) identification of symptoms if pathways to accessing testing are unclear or cumbersome, or if HCWs feel uncomfortable with accessing testing because of fear or stigma; might not identify asymptomatic or oligosymptomatic SARS-CoV-2 positive HCWs who could theoretically represent a source of infection for other staff or patients |
| Management of SARS-CoV-2 infected HCWs | ||
| Application of standard isolation duration | Can prevent a difficult to justify disconnect between public health measures and special provisions for HCWs; could ensure that the risk of introduction of SARS-CoV-2 from the health-care setting to the community is minimised | Might result in staff shortages, especially if isolation is symptom-driven rather than limited to individuals who are confirmed to be SARS-CoV-2 positive |
| Repeat PCR testing | Can identify HCWs no longer shedding SARS-CoV-2 and therefore assumed to have a low risk of transmitting the virus to other staff and patients; can provide a sense of security to staff working in close proximity with colleagues (eg, ICUs, operating theatres, emergency departments); can provide reassurance of safety to return to work in areas with high-risk patients (eg, on haemato-oncology or transplant units) | Might worsen staff shortages, particularly when the link between SARS-CoV-2 detection and transmissibility is unclear for infected people who are no longer symptomatic |
| SARS-CoV-2 serology testing | Could identify HCWs after SARS-CoV-2 infection and who might have some protection; could support more directed deployment of HCWs after SARS-CoV-2 infection | Could falsely reassure HCWs of being immune to SARS-CoV-2 when the correlates and duration of protection are insufficiently understood; could produce misleading data owing to the current lack of validated, scalable tests |
HCW=health-care worker. ICU=intensive care unit. IPC=infection prevention and control. PPE=personal protective equipment. SARS-CoV-2=severe acute respiratory coronavirus 2.
With proper use of PPE and good adherence to IPC measures, the risk of SARS-CoV-2 infection of health-care workers caring for patients with COVID-19 is considered to be very low. Physical distancing should be encouraged for contact with colleagues, such as during meetings, joint meals, and in office spaces.
Monitoring and identifying health-care workers with symptoms compatible with or suggestive of SARS-CoV-2 infection is essential to ensure appropriate triaging of staff for duty, further evaluation, and follow-up. There are considerable psychological and social strains on health-care workers because they work in a highly stressful and demanding environment and could have negative psychological effects caused by concerns over PPE availability; therefore, monitoring policies should consider how to incorporate the rapid assessment of psychosocial needs of health-care workers.
Rapid and low-threshold access to SARS-CoV-2 testing and results for health-care workers are key to maintaining an adequate workforce. Regular screening of health-care workers by PCR is unlikely to be an effective means of workforce management until evidence-based algorithms to define target staff and frequency of testing are developed, and even then negative tests might offer a false sense of reassurance. Clear algorithms must exist for handling the possible scenarios from testing of symptomatic health-care workers, in principle those who are SARS-CoV-2 negative and those who are SARS-CoV-2 positive with or without clinical illness. These algorithms need to detail the exact pathway to inform return to work and include advice and support for household contacts of health-care workers who are SARS-CoV-2 positive. One logical consequence of offering testing to symptomatic health-care workers is to support rapid return to work of those who are SARS-CoV-2 negative and clinically able to work. When adequate staffing cannot be maintained and rapid redeployment of SARS-CoV-2 infected health-care workers is necessary, re-testing could identify health-care workers no longer shedding the virus, but the relevance of ongoing shedding is unclear.
The roles of serological testing and prophylaxis (responsive or long term) for health-care workers remain to be defined. It is hoped that evidence of previous infection will correlate with the presence of neutralising antibodies and could identify health-care workers at a low risk of reinfection for voluntary supported deployment in COVID-19 wards. Trials of (chemo)prophylaxis for health-care workers have started recruitment in various countries—eg, COVIDAXIS in France (NCT04328285) and BCG-CORONA in the Netherlands (NCT04328441)—but are not expected to report for some time.
Conclusion
Specific recommendations for monitoring health-care workers for potential SARS-CoV-2 infection should be available for all staff who are expecting to see or currently managing patients with COVID-19. We feel that in a strict containment phase with low levels of community circulation, management strategies should closely align with those defined for exposed and infected members of the general public, meaning that quarantine and isolation will be stringently applied. Given that outbreaks put excess pressure on the health-care system, special provisions for health-care workers are unlikely to be needed or justifiable. However, beyond this stage, algorithms for accelerated redeployment of mildly symptomatic health-care workers might be necessary to safeguard adequate staffing levels for patient care, and a very low threshold for access to testing should be instituted to support this. Clearly, health-care workers returning to work must prioritise their clinical and psychological wellbeing and consequent ability to re-enter the workspace. On the whole, health-care staff have been observed to be extremely dedicated to ensure that their patients are adequately cared for under very difficult circumstances. Supporting health-care workers in self-monitoring and self-care, providing them with easy access to diagnostics and medical and psychosocial support, and offering clear guidance for safe and timely transitioning back to work will strengthen patient care as a whole and could ultimately improve outcomes for many patients and health-care workers.
Acknowledgments
Acknowledgments
This manuscript is part of the output from RECOVER (Rapid European COVID-19 Emergency research Response), which has received funding from the EU Horizon 2020 research and innovation programme (grant agreement number 101003589). The funder had no role in the writing of the manuscript or the decision to submit for publication. The views and opinions expressed in this Personal View are those of the authors.
Contributors
All authors contributed to the concept of the manuscript and identified relevant data. JAB wrote the first draft of the manuscript, which was critically revised and approved by all authors.
Declaration of interests
We declare no competing interests.
References
- 1.Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maxwell DN, Perl TM, Cutrell JB. “The art of war” in the era of coronavirus disease 2019 (COVID-19) Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa229. https://doi.org.10.1093/cid/ciaa229 published online March 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Qiu H, Tong Z, Ma P, et al. Intensive care during the coronavirus epidemic. Intensive Care Med. 2020;46:576–578. doi: 10.1007/s00134-020-05966-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phua J, Weng L, Ling L, et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8:506–517. doi: 10.1016/S2213-2600(20)30161-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng VCC, Wong S-C, Chen JHK, et al. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020;41:493–498. doi: 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.European Centre for Disease Prevention and Control Contact tracing: public health management of persons, including healthcare workers, having had contact with COVID-19 cases in the European Union. Feb 25, 2020. https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-public-health-management-contact-novel-coronavirus-cases-EU.pdf
- 7.European Centre for Disease Prevention and Control Novel coronavirus disease 2019 (COVID-19) pandemic: increased transmission in the EU/EEA and the UK—sixth update. March 12, 2020. https://www.ecdc.europa.eu/sites/default/files/documents/RRA-sixth-update-Outbreak-of-novel-coronavirus-disease-2019-COVID-19.pdf
- 8.WHO Health workers exposure risk assessment and management in the context of COVID-19 virus. March 4, 2020. https://apps.who.int/iris/bitstream/handle/10665/331340/WHO-2019-nCov-HCW_risk_assessment-2020.1-eng.pdf
- 9.Centers for Disease Control and Prevention Interim US guidance for risk assessment and public health management of healthcare personnel with potential exposure in a healthcare setting to patients with coronavirus disease (COVID-19) March 7, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html
- 10.Pavolini E, Kuhlmann E. Health workforce development in the European Union: a matrix for comparing trajectories of change in the professions. Health Policy. 2016;120:654–664. doi: 10.1016/j.healthpol.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Suwantarat N, Apisarnthanarak A. Risks to healthcare workers with emerging diseases: lessons from MERS-CoV, Ebola, SARS, and avian flu. Curr Opin Infect Dis. 2015;28:349–361. doi: 10.1097/QCO.0000000000000183. [DOI] [PubMed] [Google Scholar]
- 12.Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020;92:568–576. doi: 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalised patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention Characteristics of health care personnel with COVID-19—United States, Feb 12–April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:477–481. doi: 10.15585/mmwr.mm6915e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 16.Zhan M, Qin Y, Xue X, Zhu S. Death from COVID-19 of 23 health care workers in China. N Engl J Med. 2020;382:2267–2268. doi: 10.1056/NEJMc2005696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Istituto Superiore di Sanità Epidemia COVID-19—aggiornamento nazionale. March 8, 2020. https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_7-maggio-2020.pdf
- 18.Xiang Y-T, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwartz J, King C-C, Yen M-Y. Protecting health care workers during the coronavirus disease 2019 (COVID-19) outbreak: lessons from Taiwan's severe acute respiratory syndrome response. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa255. published online March 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Verbeek JH, Rajamaki B, Ijaz S, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev. 2020;4:CD011621. doi: 10.1002/14651858.CD011621.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou P, Huang Z, Xiao Y, Huang X, Fan X-G. Protecting Chinese healthcare workers while combating the 2019 novel coronavirus. Infect Control Hosp Epidemiol. 2020;41:745–746. doi: 10.1017/ice.2020.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chang. Xu H, Rebaza A, Sharma L, Dela Cruz CS. Protecting health-care workers from subclinical coronavirus infection. Lancet Respir Med. 2020;8:e13. doi: 10.1016/S2213-2600(20)30066-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26:672–675. doi: 10.1038/s41591-020-0869-5. [DOI] [PubMed] [Google Scholar]
- 24.McMichael TM, Currie DW, Clark S, et al. Epidemiology of COVID-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382:2005–2011. doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Belingheri M, Paladino ME, Riva MA. Beyond the assistance: additional exposure situations to COVID-19 for healthcare workers. J Hosp Infect. 2020;105:353. doi: 10.1016/j.jhin.2020.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Muhi S, Irving LB, Buising KI. COVID-19 in Australian healthcare workers: early experience of the Royal Melbourne Hospital emphasises the importance of community acquisition. Med J Aust. 2020;213:44. doi: 10.5694/mja2.50664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu J, Ouyang L, Guo P, et al. Epidemiological, clinical characteristics and outcome of medical staff infected with COVID-19 in Wuhan, China: a retrospective case series analysis. medRxiv. 2020 https://www.medrxiv.org/content/10.1101/2020.03.09.20033118v1 published online March 13. (preprint). [Google Scholar]
- 28.Chou R, Dana T, Buckley DI, Selph S, Fu R, Totten AM. Epidemiology of and risk factors for coronavirus infection in health care workers: a living rapid review. Ann Intern Med. 2020 doi: 10.7326/M20-1632. published online May 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sikkema RS, Pas S, Nieuwenhuijse DF, et al. COVID-19 in healthcare workers in three hospitals in the south of the Netherlands, March 2020. medRxiv. 2020 https://www.medrxiv.org/content/10.1101/2020.04.26.20079418v1 published online May 1. (preprint). [Google Scholar]
- 30.Reusken CB, Buiting A, Bleeker-Rovers C, et al. Rapid assessment of regional SARS-CoV-2 community transmission through a convenience sample of healthcare workers, the Netherlands, March 2020. Euro Surveill. 2020;25:2000334. doi: 10.2807/1560-7917.ES.2020.25.12.2000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robert Koch Institut Kontaktpersonennachverfolgung bei respiratorischen Erkrankungen durch das Coronavirus SARS-CoV-2. March 18, 2020. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Kontaktperson/Management.html
- 32.Health Protection Surveillance Centre Risk assessment of healthcare workers with potential workplace exposure to COVID-19 case (V8.1) April 16, 2020. https://www.hse.ie/eng/staff/workplace-health-and-wellbeing-unit/covid-19-guidance/risk-assessment-of-healthcare-worker-exposure-to-covid-19.pdf
- 33.Government of Canada Public health management of cases and contacts associated with coronavirus disease 2019 (COVID-19) April 10, 2020. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/interim-guidance-cases-contacts.html
- 34.Bartoszko JJ, Farooqi MAM, Alhazzani W, Loeb M. Medical masks vs N95 respirators for preventing COVID-19 in health care workers: a systematic review and meta-analysis of randomised trials. Influenza Other Respir Viruses. 2020;14:365–373. doi: 10.1111/irv.12745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones RM, Bleasdale SC, Maita D, Brosseau LM. A systematic risk-based strategy to select personal protective equipment for infectious diseases. Am J Infect Control. 2020;48:46–51. doi: 10.1016/j.ajic.2019.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wong SC, Kwong RT-S, Wu TC, et al. Risk of nosocomial transmission of coronavirus disease 2019: an experience in a general ward setting in Hong Kong. J Hosp Infect. 2020;105:119–127. doi: 10.1016/j.jhin.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kimball A, Hatfield KM, Arons M, et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility—King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:377–381. doi: 10.15585/mmwr.mm6913e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li T. Diagnosis and clinical management of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection: an operational recommendation of Peking Union Medical College Hospital (V2.0) Emerg Microbes Infect. 2020;9:582–585. doi: 10.1080/22221751.2020.1735265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Black JRM, Bailey C, Przewrocka J, Dijkstra KK, Swanton C. COVID-19: the case for health-care worker screening to prevent hospital transmission. Lancet. 2020;395:1418–1420. doi: 10.1016/S0140-6736(20)30917-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhou X, Li Y, Li T, Zhang W. Follow-up of asymptomatic patients with SARS-CoV-2 infection. Clin Microbiol Infect. 2020;26:957–959. doi: 10.1016/j.cmi.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Santé publique France Infection au nouveau coronavirus (SARS-CoV-2), COVID-19, France et Monde. April 15, 2020. https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/articles/infection-au-nouveau-coronavirus-sars-cov-2-covid-19-france-et-monde#block-242833
- 42.Health Protection Surveillance Centre Interim guidance for coronavirus—healthcare worker management by occupational health (version 16) Jan 31, 2020. https://www.hse.ie/eng/staff/workplace-health-and-wellbeing-unit/covid-19-guidance/occupational-health-interim-guidance-for-coronavirus.pdf
- 43.Kluytmans M, Buiting A, Pas S, et al. SARS-CoV-2 infection in 86 healthcare workers in two Dutch hospitals in March 2020. medRxiv. 2020 https://www.medrxiv.org/content/10.1101/2020.03.23.20041913v3 published online March 31. (preprint). [Google Scholar]
- 44.Keeley AJ, Evans C, Colton H, et al. Roll-out of SARS-CoV-2 testing for healthcare workers at a large NHS Foundation Trust in the United Kingdom, March 2020. Euro Surveill. 2020;25:2000433. doi: 10.2807/1560-7917.ES.2020.25.14.2000433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Swissnoso Public health management of healthcare workers, having had unprotected contact with COVID-19 cases in Switzerland. March 19, 2020. https://www.swissnoso.ch/forschung-entwicklung/aktuelle-ereignisse/
- 46.Rijksinstituut voor Volksgezondheid en Milieu Uitgangspunten inzetten en testen zorgmedewerkers. April 17, 2020. https://lci.rivm.nl/lci.rivm.nl/covid-19/bijlage/zorgmedewerkersinzetentestbeleid
- 47.Robert Koch Institut Optionen zum Management von Kontaktpersonen unter medizinischem Personal (auch bei Personalmangel) in Arztpraxen und Krankenhäusern) April 3, 2020. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/HCW.html
- 48.Robert Koch Institut COVID-19: kriterien zur entlassung aus dem krankenhaus bzw aus der häuslichen Isolierung. April 14, 2020. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Entlassmanagement.html
- 49.Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581:465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]