Abstract
Purpose
The coronavirus disease 2019 (COVID-19) pandemic has propelled health care workers to the front lines against the pandemic. In addition to anxiety related to infection risks, trainees have the additional burden of learning and career planning while providing care in an uncertain and rapidly changing environment. We conducted a survey to evaluate the practical and psychosocial impact on radiation oncology fellows during the first month of the pandemic.
Methods and Materials
A 4-part survey was designed and distributed to the fellows in our program. The survey was designed to evaluate the impact of the pandemic on scope of activity and well-being (“Impact on You”) and to identify key lessons learned and social factors (“About You”) using Likert scales and open-ended response options. The survey included items from the Oldenburg Burnout questionnaire.
Results
A total of 17 participants (71%) responded to the survey. Although there was a significant reduction in the mean time spent on in-person clinics (13.5 h/wk [pre-COVID] vs 9.3 h/wk [3 weeks into the COVID emergency response]; P = .002), this was replaced by virtual consults and other COVID-related activities. The proportion of respondents demonstrating features of burnout in the domains of “disengagement” and “exhaustion” was 71% and 64%, respectively. However, there was also evidence of resilience, with 47% respondents “feeling energized.” Top “concerns” and “negative changes” identified related to learning, infection risk and safety, patient care, coping, and concerns about their home country. Top “positive changes” highlighted include work culture, appreciation for leadership caring for the team, the insistence on evidence to guide change, and the implementation of virtual health care.
Conclusions
Negative impact needs to be anticipated, acknowledged, and managed. We anticipate understanding the positives that have emerged under these extraordinary circumstances is the “silver lining” of the pandemic, giving us tools and the best leverage to plan for the future.
Introduction
On March 11, 2020, the World Health Organization declared the novel coronavirus disease 2019 (COVID-19) outbreak a pandemic. At the time, there were 128,000 confirmed cases worldwide, with 103 cases in Canada. The Ontario Premier declared a state of emergency on March 17, and the province began its rapid escalation of pandemic response in our cities and hospitals, with shutting down of all nonessential services, including elective surgeries.1 In the following days, the world as we know it changed rapidly, and health care workers (HCWs) were propelled to the front lines of the fight against this pandemic. Over the next days and weeks, there were frequent changes in expectations and responsibilities as information surrounding COVID-19 evolved. To comply with social distancing recommendations, there was a rapid adoption of virtual meeting technologies, the creation and implementation of a virtual clinical care delivery model, and a rapid escalation in the dissemination of information that was required daily. Published evidence to guide decision-making during a pandemic was limited in 2019 and was mostly based on response to the SARS epidemic2; 2020 has seen a rapidly growing body of evidence that provided critical guidance to understand the world.3, 4, 5
The Radiation Oncology Fellowship Program at the University of Toronto is one of the largest of its kind globally, providing postcertification radiation oncologists from different corners of the world with a place to further their clinical and research expertise before establishing their careers. Over 70% of the current cohort of fellows are from outside Canada, and they are at the institution to capitalize on its rich resources of clinical and technical mentorship and supervision and the network of peers pursuing the same goals.
Being away from home during a fellowship maybe both personally exciting and professionally demanding. Trainees must adapt rapidly to a new organizational structure to deliver care, develop new social networks, fulfill their learning objectives, and plan for their future careers during this time. Many are separated from family, and others need to care for their family in a new city while fulfilling their career development objectives. COVID-19 has exacerbated many of the stresses on these individuals by creating uncertainty, concerns for redeployment, and demands for rapid adaptation in addition to fulfilling existing institutional and personal expectations. The declaration of a state of emergency in Ontario triggered the rapid implementation of many coordinated emergency response measures and other reactive changes across society and within the university and hospitals (Table 1).
Table 1.
Timeline of key events in response to the pandemic in Ontario, and for Radiation Oncology fellows at the University of Toronto Department Of Radiation Oncology
| Mar 13 | University of Toronto Postgraduate Medical Education
|
| Mar 14 | Request from institutional leadership
|
| Mar 16 | Border closed for international flights entering Canada |
| Mar 17 | Ontario premier announces state of emergency (beginning of social distancing) |
| Mar 17 | Weekly virtual meetings by education leads with all radiation oncology trainees implemented |
| Mar 20 | Fellows participate in an internal redeployment, including:
|
| Mar 21 | Hospitals (Princess Margaret) announce no-visitor policy |
| Mar 31 | Princess Margaret Cancer Center requests trainee redeployment plan |
| Apr 6-17 | Survey dissemination |
The need to understand the impact of the pandemic on our trainees is strong. With no real precedence to rely on, we need to generate data to support our trainees while optimizing response to patient care needs. The voice of our fellows potentially encapsulates how we as a discipline perceive and are reacting to the pandemic. We anticipate that understanding both the negatives and the positives that are emerging under these extraordinary circumstances may provide the best information to plan for the future. We designed and implemented a survey of our fellows with these objectives in mind.
Methods and Materials
A 4-part survey was designed by the training program leads (PC, JC, RW), in collaboration with the co-chief fellows (AP, SBG), and distributed anonymously through the University of Toronto Department of Radiation Oncology office.
All radiation oncology fellows actively enrolled in our program (n = 24) received an invitation to participate. The fellows are sited at the 2 cancer centers, Princess Margaret Cancer Center (n = 18) and Odette Cancer Center (n = 6), within the Department of Radiation Oncology. The fellowship program is, in general, 1 year in duration with the option of extending to a second year. Although most of our fellows work in a single site for the entire year, some share their time across more than one disease site. Our current cohort of fellows (n = 24) constitutes 14, 9, and 1 in their first, second, and third years of fellowship, respectively, with a male-to-female ratio of 3:1 and 75% international learners (n = 18).
The survey was distributed online in an anonymized fashion at the beginning of the pandemic (between weeks 3 and 5 of the pandemic emergency in Ontario). The first request was sent on April 6, the third week of the pandemic. Two reminders were sent, and the survey was closed on April 17. Only the first part of the survey probing into changes in the scope of activity and workload was “mandatory” because the information was required for departmental pandemic response planning. The remainder was optional.
Questionnaire development and data collection
The survey was designed to probe into changes in (1) scope of activity, (2) well-being (“Impact on You”), (3) key lessons learned, and (4) social factors (“About You”) using structured items, Likert scales, and open-ended response options (Appendix E1).
Section 1 was designed to explore the scope of activity. Respondents were asked to provide an estimate of the number of hours in a week that were spent on 15 key activities (contouring, clinic, research, tumor board, etc) both before and after the pandemic. Section 2, entitled “Impact on You,” was designed to capture concerns our fellows may have during the COVID-19 pandemic using 27 items. Respondents scored each item using a 5-point Likert scale (1 = strongly agree, 5 = strongly disagree). The first 11 items were created specifically for this survey based on face validity. The remaining 16 items were adapted from the Oldenburg Burnout Inventory (OBI). Section 3 on key lessons learned asked respondents to identify their top 3 concerns and the top 3 positive and negative changes they had witnessed or experienced since the pandemic. Section 4, “About You,” captured social factors that were expected to influence how the pandemic affected individuals, including living arrangements and country of origin. Because workload and workflow responses may vary by hospital and disease-site group, these are collected here. Information regarding the gender of the participants and the specific year of training was not collected to preserve the anonymity of the respondents.
Data analysis
Descriptive statistics were used to summarize questionnaire results. The mean and the standard deviations (SDs) were calculated for time estimates for different activities. The modified OBI was scored based on the subtotal for the disengagement and exhaustion domains. For technical reasons, the OBI was scored on a 5-point scale instead of the 4-point scale on the original. “Neither agree nor disagree” was scored as 2.5 for the purpose of score calculations. We used the cutoff scores recommended by Peterson et al,6 where ≥2.25 for exhaustion and ≥2.1 for disengagement are used to suggest the presence of burnout. Open-ended questions were analyzed using a thematic analysis approach.
Results
Participants
A total of 17 participants (71%) responded to the survey, and 15 (63%) provided complete responses to the optional part of the survey (sections 2-4). The majority of participants (10 of 15, 66.7%) lived in condominium living spaces of 37.1 to 111.0 m2. Five respondents lived alone, and 10 shared their accommodation with at least 1 individual. The respondents worked with many diverse disease sites, with the highest number of fellows in the head and neck site group (n = 3). The majority of respondents (n = 16, 94%) were from Princess Margaret Cancer Center (PM). The characteristics of respondents are highlighted in Table 2.
Table 2.
Characteristics of the respondents
| Characteristics | No. |
|---|---|
| Country of origin (before fellowship) | |
| Canada | 1 |
| India | 2 |
| Ireland | 1 |
| Mexico | 1 |
| Saudi Arabia | 1 |
| Not answered | 9 |
| Living arrangements | |
| Lives alone | 5 |
| With roommate | 4 |
| With spouse/family (adults only) | 5 |
| With family (with children) | 1 |
| Size of accommodation, m2 | |
| 0.1-9.0 | 1 |
| 9.1-37.0 | 2 |
| 37.1-70.0 | 6 |
| 70.1-111.0 | 4 |
| Not answered | 2 |
| Primary disease site∗ | |
| Breast | 1 |
| Central nervous system | 4 |
| Gastrointestinal | 1 |
| Head and neck | 3 |
| Lymphoma | 1 |
| Pediatrics | 2 |
| Sarcoma | 1 |
| Not answered | 2 |
Fellow can be attached to >1 site group.
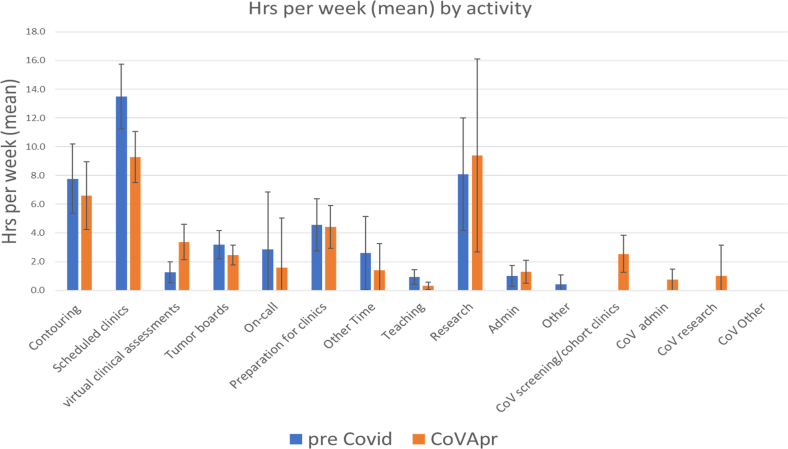
Scope of activities
The mean number of total work hours per week pre-COVID (41.6 [SD 14.9] h/wk) and at week 3 into the COVID emergency response (week 3-COVID) were not significantly different (44.5 [SD 12.5] h/wk). There was a significant reduction in the mean time spent on contouring (7.8 h/wk [pre-COVID] vs 6.6 h/wk [week 3-COVID]; P = .002) and the mean time spent on scheduled in-person clinics (13.5 [SD 4.2] h/wk [pre-COVID] vs 9.3 [SD 3.2] h/wk [week 3-COVID]; P = .002) as we transitioned into virtual health care delivery. There was also a statistically significant reduction in attendance at peer review rounds, preparation for clinics and rounds, and teaching hours. Respondents reported a modest increase in time spent on research activities (8.1 [SD 6.8] h/wk [pre-COVID] vs 9.4 [SD 12.1] h/wk [week 3-COVID]; P = .53). On average, the reduction in time spent on regular clinical activities was replaced by virtual consults (4.4 [SD 5.4] h/wk) and COVID-related activities. These included COVID screening clinics (2.5 [SD 2.3] h/wk), COVID-related research (1.0 [SD 3.9] h/wk), and administrative activities (0.7 [SD 1.3] h/wk). The average time spent on various key activities pre-COVID and at week 3 into the COVID-19 pandemic is highlighted in Table 3 and Figure 1.
Table 3.
Scope of activities
| (PreCoV) Mean hours | (CoV) Mean hours | Mean difference, h | Paired t test P value |
|
|---|---|---|---|---|
| Contouring | 7.8 | 6.6 | –1.2 | .012 |
| Scheduled clinics | 13.5 | 9.3 | –4.1 | .002 |
| Virtual clinical assessments | 1.3 | 3.4 | 1.8 | .002 |
| Tumor boards | 3.2 | 2.5 | –0.7 | .009 |
| On call | 2.9 | 1.6 | –1.1 | .575 |
| Preparation for clinics | 4.6 | 4.4 | –0.1 | .770 |
| Other | 1.9 | 1.4 | –0.4 | .578 |
| Teaching | 0.9 | 0.3 | –0.6 | .025 |
| Research | 8.1 | 9.4 | 1.6 | .534 |
| Administrative duties | 1 | 1.3 | 0.2 | .555 |
| Other duties | 0.2 | 0 | –0.2 | .336 |
| COVID screening cohort clinics | 0 | 2.5 | 2.5 | - |
| COVID administrative duties | 0 | 0.7 | 0.7 | - |
| COVID research | 0 | 1 | 1 | - |
| COVID other duties | 0 | 0.1 | 0.1 | - |
| Total | 41.6 | 44.5 | 2.9 | .492 |
Abbreviations: COVID = coronavirus disease; PreCoV = pre-COVID; CoV = week 3 COVID.
Figure 1.
Bar graph demonstrating the scope of activities before coronavirus disease (COVID) (blue) versus week 3 of COVID (orange).
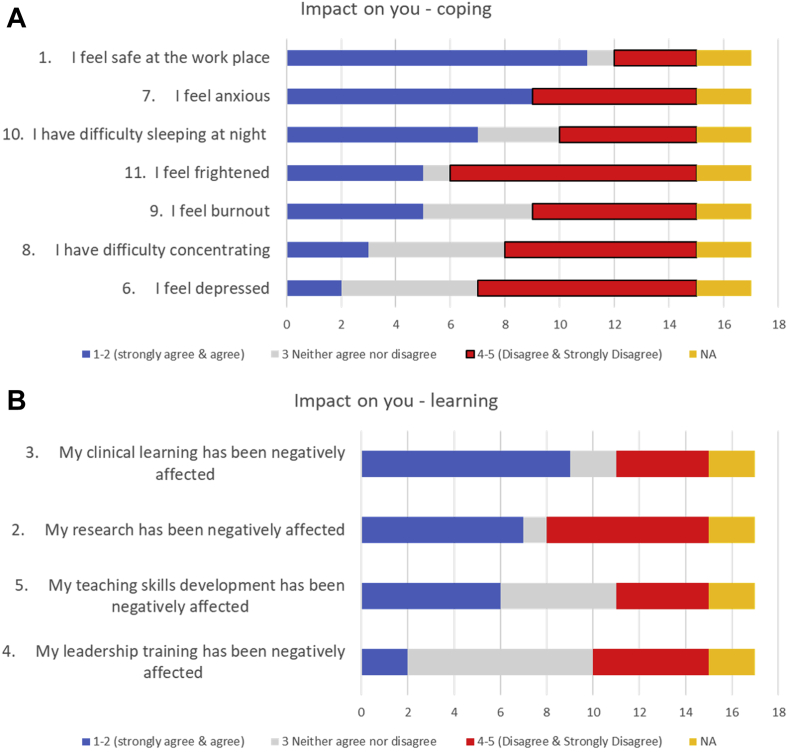
The Impact on You
Although most fellows (11 of 15, 73%) felt safe at the workplace, 3 (20%) did not. The majority of respondents felt anxious (9 of 15, 60%) and had difficulty sleeping at night (7 of 15, 46.7%). Although less prevalent, others endorsed that they felt frightened (5 of 15, 33.3%), felt burned out (5 of 15, 33.3%), had difficulty concentrating (3 of 15, 20%), and felt depressed (2 of 15, 13%). Learning was negatively affected most significantly in areas of clinical learning (9 of 15, 60%), research (7 of 15, 46.7%), teaching skills (6 of 15, 40%), and leadership training (2 of 15, 13%) (Fig 2).
Figure 2.
Participants’ responses to questions regarding the impact of coronavirus disease 2019 (COVID-19) on (A) coping and (B) learning (Appendix E1: Survey, Part 2a: Questions 1-11).
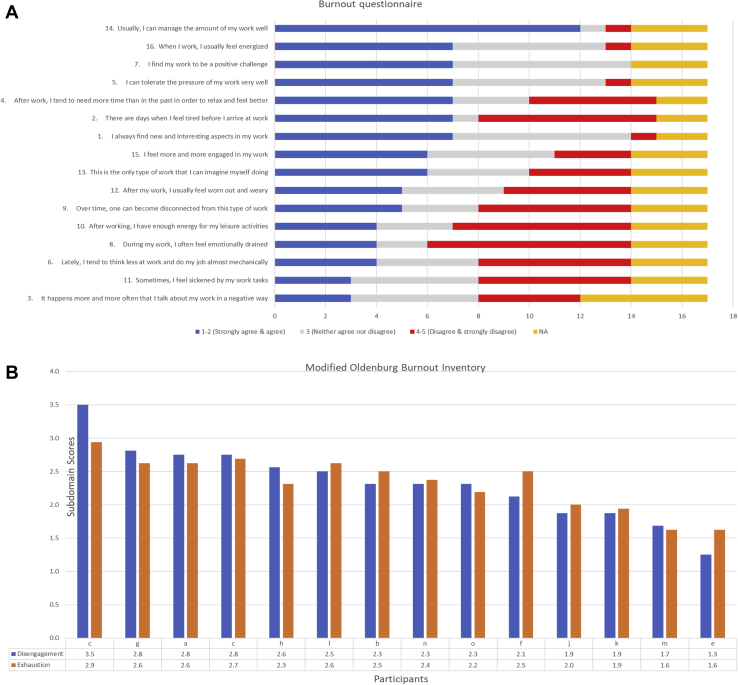
The modified OBI was completed by 14 participants. The proportion of respondents demonstrating features of burnout was 71% (10 of 14) and 64% (9 of 14) in the domains of “disengagement” and “exhaustion,” respectively. However, there was also evidence of resilience, with 47% (7 of 15) respondents feeling energized (Fig 3A-B).
Figure 3.
(A) Depicts the participants’ responses to the modified Oldenburg Burnout Questionnaire and (B) depicts scores for exhaustion and disengagement domains among various respondents. (Higher scores indicate more burnout with cutoff scores ≥2.25 for exhaustion and ≥2.1 for disengagement; Appendix E1: Survey, Part 2b: Questions 1-16).
Key lessons learned and negative and positive changes
Top 3 concerns and negative changes
There were 30 responses for top concerns and 20 for top negative changes. The themes that emerged overlapped significantly and are therefore organized under similar thematic headings (Table 4, Table 5, Table 6).
Table 4.
Top 3 concerns
Infection Risk and Safety
Patient care
Concern about learning
Coping
Concern about home country
|
Table 5.
Top 3 negative changes
Concerns about learning
Patient care
Coping
Impact on interactions
Institutional organization
|
Table 6.
Top 3 positive changes
Work culture
Leadership caring for the team
Reliance on evidence to guide change
Virtual health care
|
The key themes that emerged around top concerns were “concerns about learning,” “infection risk and safety,” “patient care,” “coping,” and thoughts about their “home country.” Fellows highlighted concerns about the impact of the pandemic on their learning due to reduced clinical exposure, the potential need for redeployment, and the ability to continue with research. The concern for infection risk and safety was consistent with what has been experienced by the general population and included concerns about affecting family members, being the source of infection for others, and the availability and adequacy of personal protection equipment. Concerns for patient care spanned from the impact of delays and a surge of patient volumes on outcomes, with particular concerns around the impact on treatments that are limited and resource-intensive (eg, brachytherapy), the effect of their delay on patient outcomes, and the subsequent recovery efforts that would be required and how they would look. Respondents highlighted the emotional stress associated with caring for patients whose care was being delayed or affected by the pandemic (quote 1). Psychological impact, including anxiety, concern about causing harm to someone else, and the increased need for self-reflection and improvement, was described. Given most of our fellows are international trainees, there were a lot of concerns about what was happening at home (country), reflecting, perhaps, a sense of guilt of not being able to provide support there (quote 2). The sentiment of inequity was highlighted in one instance, reflecting the impact of the power imbalances among trainees, staff, and the organization at large, which deserves awareness and attention (quote 3).
-
•
Quote 1: “Having to repeatedly reassure patients that their treatment delays due to COVID-19 are not going to adversely affect their treatment outcomes.”
-
•
Quote 2: “Being far from my family and unable to help them if needed.”
-
•
Quote 3: “I am feeling that my health and safety are less important than my staff’s health and safety.”
In terms of negative changes, the key themes were concerns about learning, patient care, coping, social interactions, and institutional organization. The impact on learning was most frequently cited (9 of 20), followed by descriptions about the impact on coping (Table 5).
Top 3 positive changes
Twenty-seven unique responses were offered, which were categorized under the broad themes of improvement in work culture, appreciation for leadership caring for the team, the insistence on evidence to guide change, more control of time, and the implementation of virtual health care (Table 6). The sense of culture change and the impact of good leadership and the focus on evidence translating into a feeling of being supported permeated through what was perceived as positive. Respondents highlighted improved teamwork and a sense of people coming together for the greater good; they observed that there was lots of hard work and effort and that everyone was taking the issues seriously and following recommendations. Open communication and insistence on evidence to guide change were also noted as examples our trainees felt positive about. Some reported more time for research, reading, and self-reflection as one of the positives of the pandemic. Virtual health care implementation was cited by many as a positive development, be it by phone or by videoconferencing, to provide patient care.
Discussion
Our survey, conducted during a time of rapid change in response to the COVID-19 pandemic, found changes in activities predominantly around supporting virtual and other COVID-related clinical activities. The majority of our respondents (71%) experienced features of burnout. Top concerns overlapped with negative changes observed, focusing on areas such as learning, social interactions, patient care, and the ability to cope. Concerns about the home country were particular to our fellowship cohort, where 75% (18 of 24) are international learners. The perception of inequity was described by one respondent, emphasizing the need for heightened awareness of the words we use and the actions we take. Positive changes outnumbered the negative. Good leadership that encouraged culture change, especially in a time of turmoil, together with the rapid implementation of virtual care, was valued as the “silver lining” of the pandemic for us.
Rapid change is the hallmark of life during the COVID-19 pandemic. Reacting to this change has resulted in universal psychological and physical impact, albeit in different ways for different individuals. This group of international trainees endorse this as well. Increased risk of psychological disorders like anxiety and depression has been documented among HCWs.7, 8, 9, 10 Lu et al conducted a cross-sectional study of 2299 participants and reported that frontline workers in close contact with infected patients scored higher on anxiety, depression, and fear scales, and they were 1.4 to 2.0 times more likely to experience psychological disorders.8 The increased risk of psychological disorders is expected to be higher for the oncology community, which has pre-existing risk factors11,12 like high occupational demand, caring for the terminally ill, and lack of social support. Shanafelt et al13 have summarized key considerations for understanding sources of anxiety and supporting health care professionals, which can be classified as “hear me,” “protect me,” “prepare me,” “support me,” and “care for me.” Barry et al described several strategies to improve social support in the era of social distancing, including virtual coffee mornings, meditation lounges, and a novel system called “Buddy Up,” encouraging virtual connections despite physical distancing wherein groups of 2 or 3 commit to daily check-ins and monitor each other for stress via phone call, email, or text message.14 This is particularly critical in reducing burnout in a pandemic that is expected to persist.
Today’s trainees will be tomorrow’s leaders with the responsibility to handle future pandemics and spearhead crisis management. The lessons learned yesterday in previous emergencies2,15 and from the current pandemic3,5,16 will inform future crisis management. Being encouraged to see the big picture and taking note of what works well and what does not can be an invaluable learning experience that is easily overlooked that is but well-contextualized with guidance. Lee et al4 described advocacy and a coordinated response across various levels of organization from the government to the clinical department as the focus of their effective pandemic response. Dale et al17 described “communicating clearly, delegating authority, and focusing on people and sustainability” as 3 pillars credited with successful crisis and emergency response preparedness. The “positive changes” observed are likely some of the most valuable lessons—what was “felt” and should be preserved.
The pandemic has forced many changes. Our trainees observed rapid changes to be a source of stress and that a rapid-fire stream and overall large volume of email communications can be exhausting. Regular virtual meetings with trainees and their representatives in which the rationale behind the decisions was discussed with an opportunity to hear concerns from our trainees and provide important reinforcement beyond the communication of facts were an example of clear communication that worked well for us. An effective solution to reduce foot traffic (eg, inpatient care and coverage of a radiation clinic dedicated to managing acute radiation reaction issues) was required. Our fellows and residents collaborated with education leads and created core teams to support clinical care in areas that were previously distributed across multiple staff physicians and trainees while maintaining continuity and quality of care. Fellows contributed to clinical discussions that enabled implementation and testing of novel protocols to reduce treatment duration, hospital visits, and infection risk. The implementation of each of these projects highlighted the effectiveness of different communication and leadership styles and their impact on rapid adoption and problem resolution. Fellows’ schedules were modified, and remote access tools for contouring and other clinical systems to enable work from home were rapidly implemented to ameliorate some of the psychological effects and infection risks. From a psychosocial perspective, we recognized that our trainees needed additional support, although the most effective strategies were unknown at the time. We implemented regular weekly videoconference meetings, which served as a mechanism to share information, but more importantly, to provide a regular touchpoint, to acknowledge the pressures our trainees were facing, and to share personal experiences and coping strategies, evidence-based learning, and existing and emerging wellness resources. We made deliberate efforts to mount virtual events, preserve positive events such as a trainee graduation ceremony to encourage social interactions and the expression of support for each other, and explore different ways of maximizing interpersonal support through videoconferencing technologies. We hope our responses, which blend advocacy, communication, empowerment, and a focus on people, facilitated the flattening of the many stresses that the pandemic imposed on us.
The adoption of telehealth for clinical care delivery was highlighted to be an important positive change. At our institution, the rapid design and adoption of a virtual clinical management system bridged the transition from an in-person care delivery system to a mix of in-person and telehealth model. Although technology that enables telehealth has been available for many years (Ontario Telehealth Network; OTN was founded in April 200618), its uptake has been gradual and adoption partial until now. Smith et al19 warns of the barriers to telehealth, including clinician willingness and acceptance, reimbursement, and health care system organization. Finding the best way of integrating our trainees into virtual care is the next step that is required to ensure the sustainability of this positive change. Early experiences reported by our trainees cite a reduction in their involvement in clinical care, planning, tumor board, and quality assurance round discussions. How best to augment verbal and visual cues to guide decision-making has not been the focus of medical training. Innovative ways of integrating other data points that can be ascertained through telehealth and determining when and how to integrate telehealth is both a science and an art that requires mentors, medical educators, and learners to define and disseminate.20
Our study has some limitations, including the relatively small number of respondents within a single department, the inability to analyze the effect of social factors on our fellows’ responses, and the possibility of conformity bias. To preserve anonymity, we were unable to take into consideration important social factors such as financial, childbearing, and other family responsibilities,7,21 but we hope this, in turn, minimized the possibility of bias. Our survey was conducted at the beginning of the pandemic at a time of rapid change. How these factors will evolve over time is unclear. The possibility of redeployment to internal medicine/COVID units was real and communicated to our trainees early on in the pandemic, although the fellows were not redeployed to provide direct care to COVID patients at the time of the survey. The impact on the fellows would likely have been higher if redeployment to direct COVID care was required. We plan to repeat the survey as the pandemic progresses to capture changes over time. Despite these limitations, we believe our study provides valuable insights into the concerns of radiation oncology fellows and highlights the positive changes that were brought about by COVID-19, changes that are valued both today and for the future.
Conclusions
Change is the hallmark of life during the COVID-19 pandemic. The negative impact needs to be anticipated, acknowledged, and managed. Positive changes brought about by a need to care for each other and a sharp focus on what matters the most gave us a silver lining from the pandemic.
Footnotes
Sources of support: No funding was received from any funding agencies, either public or commercial.
Disclosures: None to declare.
Supplementary material for this article can be found at https://doi.org/10.1016/j.adro.2020.07.004.
Supplementary data
References
- 1.Young L. Timeline: How Canada has changed since coronavirus was declared a pandemic. https://globalnews.ca/news/6800118/pandemic-one-month-timeline Available at:
- 2.Mukherjee R.K., Back M.F., Lu J.J., Shakespeare T.P., Wynne C.J. Hiding in the bunker: Challenges for a radiation oncology department operating in the Severe Acute Respiratory Syndrome outbreak. Australas Radiol. 2003;47:143–145. doi: 10.1046/j.0004-8461.2003.01165.x. [DOI] [PubMed] [Google Scholar]
- 3.Achard V., Tsoutsou P., Zilli T. Radiotherapy in the time of the Coronavirus pandemic: When less is better. Int J Radiat Oncol Biol Phys. 2020;107 doi: 10.1016/j.ijrobp.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee A.W.M., Xu Z.-Y., Lin L. Advocacy to provide good quality oncology services during the COVID-19 pandemic—Actions at 3-levels. Radiother Oncol. 2020;149:25–29. doi: 10.1016/j.radonc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simcock R., Thomas T.V., Estes C. COVID-19: Global radiation oncology’s targeted response for pandemic preparedness. Clin Transl Radiat Oncol. 2020;22:55–68. doi: 10.1016/j.ctro.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peterson U., Demerouti E., Bergstrom G., Samuelsson M., Asberg M., Nygren A. Burnout and physical and mental health among Swedish healthcare workers. J Adv Nurs. 2008;62:84–95. doi: 10.1111/j.1365-2648.2007.04580.x. [DOI] [PubMed] [Google Scholar]
- 7.Cao W., Fang Z., Hou G. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020;288:112936. doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verma S., Mythily S., Chan Y.H., Deslypere J.P., Teo E.K., Chong S.A. Post-SARS psychological morbidity and stigma among general practitioners and traditional Chinese medicine practitioners in Singapore. Ann Acad Med Singapore. 2004;33:743–748. [PubMed] [Google Scholar]
- 10.Chen Y., Zhou H., Zhou Y., Zhou F. Prevalence of self-reported depression and anxiety among pediatric medical staff members during the COVID-19 outbreak in Guiyang, China. Psychiatry Res. 2020;288:113005. doi: 10.1016/j.psychres.2020.113005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hlubocky F.J., Back A.L., Shanafelt T.D. Addressing burnout in oncology: Why cancer care clinicians are at risk, what individuals can do, and how organizations can respond. Am Soc Clin Oncol Educ Book. 2016;35:271–279. doi: 10.1200/EDBK_156120. [DOI] [PubMed] [Google Scholar]
- 12.Nissim R., Malfitano C., Coleman M., Rodin G., Elliott M. A qualitative study of a compassion, presence, and resilience training for oncology interprofessional teams. J Holist Nurs. 2019;37:30–44. doi: 10.1177/0898010118765016. [DOI] [PubMed] [Google Scholar]
- 13.Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323:2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 14.Barry A, Murphy T, Prince R, May T, Zimmermann C, Elliott M. Time to ‘buddy up’-simple strategies to support oncologists during the coronavirus disease 2019 pandemic [e-pub ahead of print]. Adv Radiat Oncol.https://doi.org/10.1016/j.adro.2020.04.004. Accessed July 27, 2020. [DOI] [PMC free article] [PubMed]
- 15.Gay H.A., Santiago R., Gil B. Lessons learned from Hurricane Maria in Puerto Rico: Practical measures to mitigate the impact of a catastrophic natural disaster on radiation oncology patients. Pract Radiat Oncol. 2019;9:305–321. doi: 10.1016/j.prro.2019.03.007. [DOI] [PubMed] [Google Scholar]
- 16.Meattini I., Franco P., Belgioia L. Radiation therapy during the coronavirus disease 2019 (COVID-19) pandemic in Italy: A view of the nation’s young oncologists. ESMO Open. 2020;5 doi: 10.1136/esmoopen-2020-000779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dale C., Welling L., Clearfield C. How one Seattle health system is managing the COVID-19 crisis. https://hbr.org/2020/04/how-one-seattle-health-system-is-managing-the-covid-19-crisis Available at:
- 18.Wikipedia OTN. https://en.wikipedia.org/wiki/Ontario_Telemedicine_Network Available at:
- 19.Smith A.C., Thomas E., Snoswell C.L. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19) J Telemed Telecare. 2020 doi: 10.1177/1357633X20916567. 1357633x20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hollander J.E., Carr B.G. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382:1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 21.Xiao H., Zhang Y., Kong D., Li S., Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26 doi: 10.12659/MSM.923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.