Abstract
Background.
Youth with chronic medical conditions (YCMC) use alcohol at levels similar to their healthy peers but face elevated risk for adverse health consequences. As salient reasons to abstain from or limit drinking (RALD) among YCMC are unknown, we sought to identify clusters of RALD and test associations with use behaviors.
Methods.
Eligible YCMC (ages 9–18) recruited from outpatient clinics reported their use behaviors and importance of potential RALD. Cluster analysis was used to discern RALD patterns, which were examined as predictors of alcohol use using multivariate regression.
Results.
Among 398 participants, 30.9% reported past year alcohol use. Concerns about impacts on medications, school, and disease status were the most frequently endorsed RALD; prior negative experiences with alcohol and family history were the least frequently endorsed. Five RALD clusters were identified for all YCMC and two for recent drinkers. Compared to the cluster with high endorsement of multiple general and health-related RALD, those predominantly citing concerns about addiction and those not strongly endorsing any RALD consistently reported greater alcohol use. Among recent drinkers, the cluster characterized by low concern across multiple RALD also consistently reported greater alcohol use compared to their counterparts expressing moderate concern.
Conclusions.
For YCMC, RALD are complex but endorsement of multiple general and health-related RALD is associated with less use, and health concerns are especially prevalent. More research is needed to understand how salient RALD can inform tailored interventions that aim to delay and reduce substance use and improve health outcomes for YCMC.
Keywords: Adolescents, Alcohol Use, Chronic Disease Care, Health Promotion, Substance Use and Perception
1. Introduction
Alcohol is the most commonly used substance among adolescents (Miech et al., 2016) and adolescent alcohol use is associated with both acute (Bonomo et al., 2001; Zeigler et al., 2005) and chronic (Bonomo et al., 2004) harms. Youth with chronic medical conditions (YCMC, including those requiring ongoing medical or pharmaceutical management such as diabetes or cystic fibrosis) have comparable levels of alcohol consumption as their healthy peers (Wisk et al., 2016) yet face unique alcohol-related risks like disease exacerbation, medication interactions, and treatment non-adherence (Price et al., 2010; Turner et al., 2001; Weitzman et al., 2018; Weitzman et al., 2015). Thus, insights into this group’s beliefs and attitudes are especially important for prevention and intervention to avert such detrimental consequences.
An expansive body of research identifies impelling factors for alcohol use among youth in general (Patrick et al., 2013). Reasons youth abstain from or limit drinking (RALD) are often multi-factorial (Anderson et al., 2011; Epler et al., 2009; Kuntsche et al., 2005; Rinker et al., 2013); existing work has identified attitudes and values that counter use may reflect concerns for harming one’s reputation, physical self, or self-control (Epler et al., 2009; Huang et al., 2011; Rinker et al., 2013), as well as social class (Mackie et al., 2011). RALD that reflect goals to avert the potential for health harm have shown unclear associations with drinking behaviors for healthy youth (Epler et al., 2009; Patrick et al., 2008). In contrast, there is little evidence about what motivates or prevents alcohol use among YCMC. Older age, cognitive ability, negative modeling, and propensity to take risks have been associated with poor decision making about alcohol use among adolescent cancer survivors and youth with asthma (Hollen et al., 2019). However, initial interventions to improve these groups’ decision-making around alcohol use were ineffective (Hollen et al., 2013), but it is unclear whether lack of efficacy stems from poor targeting of the intervention relative to youth motivations for use. Future behavioral interventions may be more persuasive if informed by a better understanding of RALD among YCMC.
The experience of chronic illness itself likely plays a substantial role in shaping the motivations, decisions and alcohol use behaviors of medically vulnerable youth (Weitzman et al., 2019). Pediatric-onset chronic illness may interfere with normal roles and developmental milestones (Wisk et al., 2017); as such, concerns about alcohol use harming one’s reputation – a protective factor for some youth (Yeager et al., 2018) – may be offset by perceptions that consuming alcohol in social situations signifies wellness and maturity and provides an avenue for social connection (Weitzman et al., 2019). Worry that heavy alcohol use early in life poses added risk for health harm and disease in later life does not consistently protect against alcohol use for healthy youth (Brown et al., 2015). Yet for youth with chronic conditions, worries about alcohol’s adverse health effects may represent more realistic and credible near-term concerns, which bear on highly salient goals to avoid disease exacerbation, protect well-being, and ensure medication safety/efficacy (Weitzman et al., 2018; Weitzman et al., 2019; Weitzman et al., 2015). Avoiding disruptions in educational participation associated with poor health – including where drinking contributes to disease exacerbations – may be especially important for YCMC, who face inequalities in educational attainment related to living with a chronic illness (Wisk et al., 2017).
To address gaps in our understanding of alcohol use motivations among medically vulnerable youth, we sought to characterize RALD among YCMC, and to test whether RALD are associated with alcohol use behaviors. Findings may have important implications for development of preventive interventions and delivery of clinical guidance to reduce alcohol use in this population (Lunstead et al., 2019).
2. Materials and Methods
2.1. Study Design and Sample
As part of a larger survey study to validate an alcohol use screening tool (Levy et al., 2016), we ascertained self-report alcohol use behaviors and reasons to abstain from or limit alcohol use among a medically heterogeneous clinical cohort of adolescents with a pediatric-onset chronic disease. The study recruited youth presenting for routine care between June 2013 and July 2015 at clinics offering subspecialty care for: type 1 diabetes (endocrinology), juvenile idiopathic arthritis (rheumatology), moderate persistent asthma or cystic fibrosis (pulmonology), or inflammatory bowel disease (including ulcerative colitis or Crohn’s disease, gastroenterology) at Boston Children’s Hospital. Approximately 100 youth were recruited from each clinic, with purposive oversampling of youth in middle and late adolescence to ensure sufficient sample size to evaluate drinking behaviors. Parents provided consent for children ages nine through 11 years, and youth ages 12 to 18 years were assented with a waiver of parental consent under the approval of the Boston Children’s Hospital Institutional Review Board. In total, this study approached 523 youth, of which, 404 consented and were subsequently enrolled (77.2% consent rate). All survey items were administered using an online structured assessment delivered on a tablet computer configured with a polarizing screen for privacy. A detailed report of methods has been published previously (Weitzman et al., 2015). Our sample included 398 participants who had complete data on RALD and alcohol use behaviors.
2.2. Survey Measures
Sociodemographic Characteristics:
Participants reported their age in years, current grade in school, sex, race/ethnicity, number of parents/guardians in the household, and highest level of education attained by a parent. Mental health was evaluated with the 5 item mental health inventory of the SF-36 short form (Ware et al., 1993); higher scores indicate better mental health. As 378 respondents (95%) had sufficient data to calculate the mental health score (i.e., at least three of the five items), missing scores were imputed using the mean score of participants with a calculated score.
Alcohol Use Behaviors:
Alcohol use was assessed via the Diagnostic Interview Schedule for Children (Shaffer et al., 2003), including lifetime, past year and past three-month alcohol use; for youth reporting past three-month use, binge drinking and total alcohol volume consumed during that period were also assessed. Binge drinking was defined using the National Institute on Alcohol Abuse and Alcoholism age and sex cutoffs (National Institute on Alcohol Abuse and Alcoholism et al., 2015). Past three-month total alcohol volume (hereafter referred to as total volume) was obtained by multiplying respondents’ numeric responses to: “In the last three months, on how many days did you have something to drink” and “When you drank in the last three months, how many drinks did you usually have on one occasion?”
Reasons to Abstain or Limit Drinking.
We modified existing RALD identified in the literature (Bernards et al., 2009) to make them age and developmentally appropriate for use with adolescents with chronic conditions, and included items that align with general RALD domains (Epler et al., 2009). Youth were prompted, “Sometimes people choose not to drink. How important to you are the following reasons not to drink?” and presented with fourteen potential reasons to abstain from alcohol use (three of which were only shown to participants who indicated that they had ever consumed alcohol). For each RALD, respondents were asked to select “Very important,” “Somewhat important,” or “Not important.” RALD statements included: “Drinking is not healthy;” “It could make my [disease] worse;” “Alcohol might make my medications not work well;” “I worry about becoming an alcoholic;” “Someone in my family has had a problem with alcohol and I don’t want the same sort of problem;” “I don’t want to lose control while drunk;” “I don’t want to disappoint my parents;” “I don’t want to disappoint my healthcare team;” “I don’t want my friends to think badly of me;” “I don’t want to get into trouble;” “I want to do well in school and alcohol would affect my school work;” and (among drinkers only) “I feel sick when I drink;” “I don’t like the taste of alcohol;” and “I had a problem in the past because of alcohol and I don’t want to have a problem again.”
Participants were also asked, “Are there any other reasons why you do not drink?” and were provided with a free text, open response field in which they could write their answers; 221 participants provided any response. A primary reader initially reviewed and thematically coded free text responses; the full team of investigators collaboratively reviewed, discussed, and confirmed all coding assignments on a consensus protocol over several iterations. Sixteen indicators were created to reflect endorsement of each identified theme (Appendix 1); responses mentioning multiple themes were coded as such and responses that stated there were no other reasons were not identified as belonging to any of the 16 identified themes.
2.3. Analytic Approach
Clustering algorithms were implemented in R 3.5.2 (R Foundation for Statistical Computing, Vienna, Austria) and analyses conducted using SAS 9.4 (SAS Institute, Cary, NC). Statistical significance was considered at p<0.05. Summary statistics were computed to characterize the study sample overall and by past year alcohol use. Differences in demographic characteristics by lifetime use were compared using Kruskal-Wallis or Chi Square (χ2) tests, as appropriate.
Exploratory cluster analyses were performed using Ward’s minimum-variance clustering method to group (A) all participants who shared a similar response pattern across eleven potential RALD (all RALD except the three that were shown to drinkers only) as well as 16 indicators for free text responses and (B) participants who reported any past three-month alcohol use and shared a similar response pattern across fourteen potential RALD and 16 indicators for free text responses. Ward’s method minimizes the total within-cluster variance (such that clusters are maximally similar within themselves) and merges clusters with minimum cluster (Euclidean) distance; the ‘NbClust’ package (Charrad et al., 2014) was used to assess multiple fit indices for potential cluster solutions and select the cluster solution that is ruled optimal by the majority of these indices. A final solution of five clusters was selected for all participants (A) and an additional two clusters were selected among past three-month drinkers (B). Clusters were used to define two mutually exclusive and exhaustive categorical variables (A, for all YCMC, and B, for all past three-month drinkers). Multivariate regression analyses with generalized estimating equations (GEE), to account for clustering within clinic of recruitment, were used to determine if cluster assignment was associated with alcohol use behaviors, adjusting for participant age, sex, race/ethnicity, household status (number of parents in the home) and mental health score. GEE models with binomial, Poisson, and Gaussian distributions were selected based on outcome distributions.
We performed two sensitivity analyses: (1) adjustment for non-imputed mental health score as a covariate in multivariate models for the N=378 participants who completed the mental health inventory and (2) replicating final multivariate analyses among an older cohort (N=219 high school juniors, seniors, or college students). Results were substantively consistent across these specifications.
3. Results
The majority of the sample was white/non-Hispanic (72.4%, Table 1) with college-educated parents (70.1%). Approximately half the sample was male (51.3%) and the average age was 15.6 years (SD=2.1). Nearly four-in-ten youth (37.7%, Table 2) reported lifetime alcohol use and 30.9% reported past year alcohol use; 21.1% reported past three-month use, of which 45.2% reported binge-level consumption. Over one-third (34.5%) of past three-month drinkers consumed at least 12 drinks during that time and had a mean of 2.15 binge events. Differences in past year consumption were seen by age, grade, and mental health – with those who drank alcohol reporting lower mental health scores (Table 1).
Table 1 -.
Sample Sociodemographics and Health Characteristics by Past Year and Three-Month Alcohol Use
| Total | Any Past Year Use | Any Past 3-Month Use | ||||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | p-value | N | % | p-value | |
| Total | 398 | 123 | 30.9% | 84 | 21.1% | |||
| Age (years), Mean | 15.61 | 16.98 | <0.001 | 17.20 | <0.001 | |||
| Standard deviation | 2.10 | 1.12 | 1.04 | |||||
| Grade in School | <0.001 | <0.001 | ||||||
| 4th – 6th | 28 | 7.0% | 0 | 0.0% | 0 | 0.0% | ||
| 7th – 8th | 43 | 10.8% | 3 | 7.0% | 1 | 2.3% | ||
| 9th – 10th | 108 | 27.1% | 13 | 12.0% | 5 | 4.6% | ||
| 11th – 12th | 163 | 41.0% | 71 | 43.6% | 45 | 27.6% | ||
| College | 56 | 14.1% | 36 | 64.3% | 33 | 58.9% | ||
| Sex | 0.671 | 0.795 | ||||||
| Male | 194 | 48.7% | 58 | 29.9% | 42 | 21.6% | ||
| Female | 204 | 51.3% | 65 | 31.9% | 42 | 20.6% | ||
| Race/Ethnicity | 0.238 | 0.082 | ||||||
| White, non-Hispanic | 288 | 72.4% | 92 | 31.9% | 65 | 22.6% | ||
| Black, non-Hispanic | 30 | 7.5% | 8 | 26.7% | 5 | 16.7% | ||
| Other, non-Hispanic | 18 | 4.5% | 9 | 50.0% | 7 | 38.9% | ||
| Hispanic | 52 | 13.1% | 12 | 23.1% | 5 | 9.6% | ||
| Unknown | 10 | 2.5% | 2 | 20.0% | 2 | 20.0% | ||
| Parental Education | 0.554 | 0.700 | ||||||
| ≤High school/GED | 60 | 15.1% | 16 | 26.7% | 9 | 15.0% | ||
| Some college | 38 | 9.5% | 11 | 28.9% | 8 | 21.1% | ||
| College graduate | 156 | 39.2% | 44 | 28.2% | 33 | 21.2% | ||
| Graduate degree | 123 | 30.9% | 45 | 36.6% | 30 | 24.4% | ||
| Unknown | 21 | 5.3% | 7 | 33.3% | 4 | 19.0% | ||
| Household Status | 0.190 | 0.902 | ||||||
| Two parents | 292 | 73.4% | 84 | 28.8% | 60 | 20.5% | ||
| One parent/foster care | 97 | 24.4% | 37 | 38.1% | 22 | 22.7% | ||
| Unknown | 9 | 2.3% | 2 | 22.2% | 2 | 22.2% | ||
| Clinical Site | 0.482 | 0.572 | ||||||
| Endocrinology | 97 | 24.4% | 27 | 27.8% | 17 | 17.5% | ||
| Gastroenterology | 98 | 24.6% | 34 | 34.7% | 25 | 25.5% | ||
| Pulmonology | 101 | 25.4% | 27 | 26.7% | 20 | 19.8% | ||
| Rheumatology | 102 | 25.6% | 35 | 34.3% | 22 | 21.6% | ||
| Mental Health Score, Mean | 74.80 | 72.01 | 0.054 | 74.32 | 0.614 | |||
| Standard deviation | 16.01 | 17.87 | 15.62 | |||||
Data are from 398 respondents to clinic-based survey. Column percentage is shown in the ‘Total’ column; row percentage (prevalence of past year and past three-month alcohol use) is shown elsewhere unless otherwise specified.
Table 2 -.
Alcohol Use Behaviors Overall and by Identified Clusters
| Total | All YCMC | Past 3- Month Drinkers | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lifetime Use | Past Year Use | Past 3-Month Use | Past Month Use | Age of Onset | Any Binge Use | Times Binge Drank | Total Volume | Had ≥12 Drinks | |||
| All YCMC | 398 | 37.7% | 30.9% | 21.1% | 13.3% | 15.43 (1.93) | 45.2% | 2.15 (4.63) | 15.86 (25.75) | 34.5% | |
| Cluster A | *** | *** | *** | *** | NS | † | † | * | NS | ||
| Unconcerned | 66 | 69.7% | 59.1% | 48.5% | 34.8% | 15.07 (1.67) | 56.3% | 3.56 (6.63) | 25.91 (36.31) | 46.9% | |
| Addiction focused | 89 | 50.6% | 42.7% | 25.8% | 18.0% | 15.47 (1.87) | 56.5% | 1.61 (2.31) | 16.26 (22.12) | 39.1% | |
| School focused | 63 | 31.7% | 23.8% | 15.9% | 7.9% | 16.10 (2.10) | 30.0% | 2.20 (4.16) | 15.70 (26.38) | 30.0% | |
| Short term impacts | 97 | 29.9% | 25.8% | 17.5% | 8.2% | 15.55 (2.23) | 23.5% | 0.47 (1.07) | 6.06 (9.49) | 11.8% | |
| Multiple impacts | 83 | 12.0% | 7.2% | 2.4% | 1.2% | 15.20 (2.10) | 0.0% | - | 3.50 (3.54) | 0.0% | |
| Drinkers | 84 | - | - | - | 63.1% | 15.55 (1.64) | 45.2% | 2.15 (4.63) | 17.50 (27.83) | 34.5% | |
| Cluster B | NS | NS | * | ** | * | ** | |||||
| Emboldened | 36 | - | - | - | 72.2% | 15.44 (1.58) | 61.1% | 3.86 (6.43) | 27.28 (35.73) | 52.8% | |
| Conscientious | 48 | - | - | - | 56.3% | 15.63 (1.70) | 33.3% | 0.88 (1.81) | 10.17 (17.00) | 20.8% | |
For each outcome (column), column percentages or mean and standard deviation are shown.
NS-not significant,
p<0.1,
p<0.05,
p<0.01,
p<0.001
Cluster A reflects the five mutually exclusive and exhaustive clusters identified by the cluster analysis performed among all respondents (youth with chronic medical conditions, YCMC; N=398).
Cluster B reflects the two mutually exclusive and exhaustive clusters identified by the cluster analysis performed among all respondents who reported any alcohol use in the past three-months (drinkers; N=84).
3.1. RALD among all YCMC
There was wide variation in endorsement of individual RALD: more than three-quarters of YCMC endorsed wanting to do well in school and potential interaction between alcohol and medications as very important while fewer than one-quarter endorsed a prior problem with alcohol as a very important RALD. Endorsement of RALD was largely similar across clinics (Appendix 2). The first cluster analysis identified five mutually exclusive and exhaustive clusters based on RALD (Figure). The ‘multiple impacts’ cluster (N=83, referent cluster in multivariate analyses) rated most RALD as very important and individuals in this cluster were the most likely to provide a free-text RALD. The ‘short term impacts’ cluster (N=97) similarly placed high importance on tangible, near-term RALD (e.g., wanting to do well in school and concerns about medication interactions), but placed less importance on more putative RALD (e.g, worrying about becoming an alcoholic). Predominant RALD for the ‘addiction focused’ cluster (N=89) included not wanting to lose control while drunk and family history of problems with alcohol. A cluster of ‘school focused’ youth (N=63) reported highest concern for wanting to do well in school. Finally, the ‘unconcerned’ cluster (N=66) had the lowest endorsement of importance across all RALD.
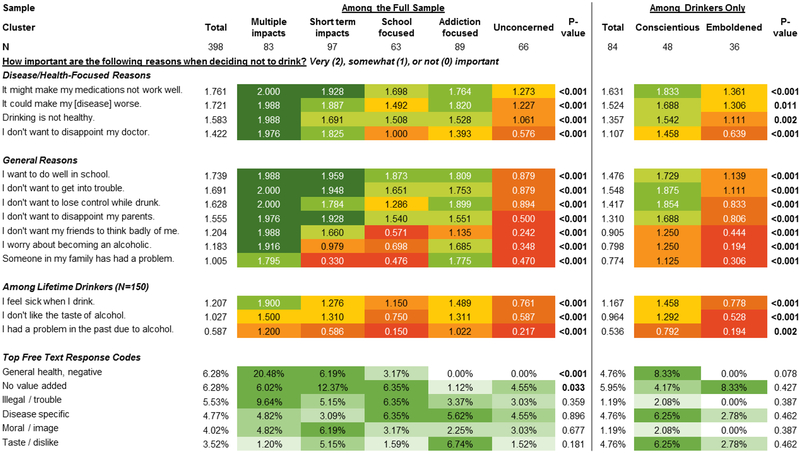
Figure -. Heat Map of Reasons to Abstain from or Limit Drinking (RALD) by Identified Clusters.
Figure depicts mean scores on each reason to abstain from or limit drinking (RALD) item (scored: 2-very important; 1-somewhat important; 0-not important) and the prevalence of reporting the most frequently endorsed free text codes, both overall and for each cluster. Darker green shading reflects more concern (for RALD) or greater endorsement (for free text). P-values indicate the comparison of mean scores or prevalence across clusters; bolded values indicate significant differences at p<0.05. Results are presented for the first cluster analysis among the full sample (N=398) including five mutually exclusive and exhaustive clusters, and the second cluster analysis among respondents who reported any alcohol use in the past three-months (‘drinkers’; N=84) including two mutually exclusive and exhaustive clusters.
Clusters were significantly different with respect to age (unconcerned was the oldest) and grade in school. Differences were also observed by sex (unconcerned were the mostly likely to be male) and by mental health (unconcerned had the lowest mental health score; data not shown).
Alcohol use behaviors differed substantially by clusters (Table 2). Compared to the multiple impacts cluster, all other clusters had higher unadjusted odds of lifetime, past year, and past three-month alcohol use (Table 3). After adjusting for sociodemographics and clustering within clinic, the unconcerned and addiction focused clusters showed consistently elevated adjusted odds of use (e.g., past year alcohol use for addiction focused OR: 5.33, 95%CI: 3.02–9.40 and unconcerned OR: 6.89, 95%CI: 2.87–16.53) compared to the multiple impacts cluster.
Table 3 -.
Multivariate Regression Predicting Alcohol Use Behaviors by Cluster Membership
| Any Lifetime Use | Any Past Year Use | Any Past 3 Month Use | Any Past Month Use | Age of Onset | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Cluster A (All YCMC) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | β (SE) | β (SE) |
| Unconcerned | 16.79*** (5.26–53.63) |
5.73** (1.78–18.47) |
18.54*** (7.31–47.02) |
6.89*** (2.87–16.53) |
38.12*** (16.29–89.22) |
13.52*** (4.97–36.80) |
43.86*** (10.02–192) |
13.11*** (3.07–56.04) |
−0.13 (0.44) |
−0.20 (0.30) |
| Addiction focused | 7.47*** (4.64–12.01) |
4.05*** (2.74–5.97) |
9.56*** (6.67–13.72) |
5.33*** (3.02–9.40) |
14.11*** (6.89–28.91) |
6.91*** (3.40–14.05) |
17.97*** (3.76–85.87) |
8.49* (1.61–44.70) |
+0.27 (0.36) |
+0.20 (0.15) |
| School focused | 3.40** (1.38–8.33) |
1.82 (0.72–4.60) |
4.01** (1.49–10.80) |
2.12 (0.67–6.70) |
7.64** (2.23–26.18) |
3.64* (1.06–12.53) |
7.07† (0.92–54.39) |
3.15 (0.34–28.94) |
+0.90 (0.98) |
+1.12 (0.81) |
| Short term impacts | 3.11** (1.46–6.62) |
2.50† (0.96–6.53) |
4.46*** (2.06–9.64) |
3.37** (1.51–7.53) |
8.61*** (3.00–24.65) |
5.96*** (2.43–14.62) |
7.37* (1.07–50.66) |
4.87 (0.70–33.83) |
+0.35 (0.64) |
+0.48 (0.35) |
| Multiple impacts |
1.00
(reference) |
1.00
(reference) |
1.00
(reference) |
1.00
(reference) |
1.00
(reference) |
1.00
(reference) |
1.00
(reference) |
1.00
(reference) |
0.00
(reference) |
0.00
(reference) |
| Any Binge Drinking | Times Binge Drank | Total Volume | ≥12 Drinks, Past 3 Mo | Age of Onset | ||||||
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Cluster B (Drinkers) | OR (95%CI) | OR (95%CI) | IRR(95%CI) | IRR(95%CI) | β (SE) | β (SE) | OR (95%CI) | OR (95%CI) | β (SE) | β (SE) |
| Emboldened | 3.14***
(2.22–4.44) |
3.34** (1.36–8.22) |
4.41***
(2.47–7.88) |
2.86*** (1.69–4.86) |
+17.11** (6.39) |
+7.81 (5.45) |
4.25*** (2.14–8.42) |
2.69*** (1.56–4.64) |
−0.18 (0.25) |
−0.35* (0.16) |
| Conscientious |
1.00
(reference) |
1.00
(reference) |
1.00
(reference) |
1.00
(reference) |
0.00
(reference) |
0.00
(reference) |
1.00
(reference) |
1.00
(reference) |
0.00
(reference) |
0.00
(reference) |
p<0.1,
p<0.05,
p<0.01,
p<0.001.
Unadjusted models account for clustering within clinic of recruitment
Adjusted models control for age, sex, race/ethnicity, household status, and mental health score, and account for clustering within clinic of recruitment
Lifetime, past year, past 3 month, past month, binge drinking, and ≥12 drinks (in the past 3 months) were modeled with logistic regression, times binging was modeled with Poisson regression, and total volume and age of onset were modeled with linear regression.
Cluster A reflects the five mutually exclusive and exhaustive clusters identified by the cluster analysis performed among all respondents (youth with chronic medical conditions, YCMC; N=398).
Cluster B reflects the two mutually exclusive and exhaustive clusters identified by the cluster analysis performed among all respondents who reported any alcohol use in the past three-months (drinkers; N=84).
3.2. RALD among recent drinkers
The second cluster analysis identified two mutually exclusive and exhaustive clusters based on RALD (Figure). The ‘conscientious drinkers’ (N=48, referent cluster in multivariate analyses) highly endorsed not wanting to get in trouble or lose control while drunk and interactions with medications or their disease. The ‘emboldened drinkers’ (N=36) had the lowest prevalence of endorsing very important across all RALD; however, this cluster’s highest RALD endorsement was for the importance of disease and medication related reasons. Clusters were relatively similar in their sociodemographic make-up with the exception of sex: emboldened drinkers were more likely to be male (63.9%) while conscientious drinkers more likely to be female (39.6%; data not shown).
In adjusted analyses among past three-month drinkers, the emboldened drinkers were more likely to binge drink (OR: 3.34, 95%CI: 1.36–8.22), had a greater number of binge drinking events (incidence rate ratio: 2.86, 95%CI: 1.69–4.86), were more likely to have consumed at least 12 drinks in the past three-months (OR: 2.69, 95%CI: 1.56–4.64), and initiated drinking at a younger age (−0.35 years; p=0.032) compared to the conscientious drinkers.
4. Discussion
Reasons to abstain from or limit drinking were complex and often multifactorial for YCMC in this study. Disease-related RALD were among the most frequently endorsed and associated with less alcohol use; clusters with the lowest endorsement of these RALD reported the highest rates of alcohol use and highest levels of alcohol consumption. Findings align with prior reports that concern for staying healthy and avoiding disease exacerbations or condition-specific risks may be central to decision making regarding alcohol use among medically vulnerable youth (Weitzman et al., 2019), and add heft to reports about the potential protective effects of knowledge about alcohol-medication interactions and risk to safety/efficacy of treatments (Weitzman et al., 2018).
Across groups, predominant general concerns were concentrated around doing well in school and avoiding getting into trouble, factors that distinguish the multiple impacts and school focused group especially. Discussing with YCMC the impact of alcohol on learning and memory may be important for alcohol use interventions, consistent with recommendations for brief interventions generally. The addiction-focused group reported the second highest rate of alcohol use; concerns for addiction may stem from residing in contexts where alcohol use may be common, enabled or expected, hence screening YCMC for a family history of alcohol or substance use, or other contextual influences, may help to ensure access to countervailing information and helpful resources. Psychosocial and financial burdens of having a child with chronic illness are substantial for families (Creswell et al., 2014; Pollock et al., 2013; Wisk et al., 2012; Witt et al., 2011) and these stressors could contribute to family and child substance use. Taking a holistic family-centered approach to screening, prevention, and support for YCMC may be especially important.
Clusters with high alcohol use – and greatest risk for acute harms – tended to be less concerned about ‘common’ RALD that may be applicable to all youth (like reputation) yet these clusters endorsed health as relatively more important than other potential RALD. Centering conversations on disease-specific alcohol interactions may also be an effective strategy for brief interventions to reduce alcohol use among YCMC in this higher activity group. These conversations may be particularly important for the substantial proportion of YCMC who are not aware or knowledgeable about the impact of alcohol on their conditions (Harstad et al., 2017; Lunstead et al., 2019).
While health-related RALD were generally rated with high importance by the majority of YCMC and were associated with reduced use, we observed a further protective association for those endorsing RALD spanning multiple domains. Specifically, clusters with the lowest rates of any alcohol use and lowest rates of alcohol consumption were those that assigned high importance across multiple RALD, including both short- and long-term focused RALD. Although we could not explicitly test whether endorsement of multiple, unrelated RALD are causally linked to less alcohol use in this study, prior work has identified that multi-component interventions may be particularly impactful for curtailing alcohol use (Foxcroft et al., 2012; Koning et al., 2011). While interventions that deliver multiple messages, spanning a range of potential RALD, may provide maximum reach to YCMC as a group overall (i.e., by casting a wide net), understanding the impact of specific messages on subgroups of youth can advance the science of tailored/targeted preventive interventions.
We found important differences in the age distributions among clusters of RALD with younger participants more likely to endorse larger numbers of RALD. Our findings on the association between age and RALD are consistent with a previous study, which found that, among healthy middle school students, RALD were noted to decrease significantly over only three years and drinking experience was shown to accelerate this decline (Merrill et al., 2016). As youth age and develop more specific motivations, interventions may need to be tailored to more specific concerns. The cross-sectional design of our study limits testing whether RALD change over time for YCMC; yet, sensitivity analyses revealed that our findings were consistent among a sub-sample of older youth, suggesting that at least some of the factors motivating abstaining from or limiting alcohol use remain salient in older adolescence when youth are more likely to experiment with alcohol. Youth may further increase alcohol use and experience changing motivation to use once in more alcogenic post-high school environments (Johnson et al., 2004; Patrick et al., 2011), so longitudinal evaluations are needed to fully define changes in RALD and the impact of RALD on behaviors over time among YCMC. Honing developmentally targeted interventions that emphasize greater breadth of messages centered on preventing initiation and re-enforcing non-use for younger adolescents that advance to more focused messages as adolescents age may be effective.
Several limitations should be noted. First, although our data represent a medically heterogeneous sample of adolescents, all participants were recruited from clinics affiliated with a single pediatric hospital in the Northeast and may have limited generalizability. YCMC who do not regularly seek subspecialty medical care may be underrepresented in our sample and these youth may also be the most likely to engage in alcohol use. If this is the case, this study may have missed clusters of heavier drinkers who may need more intensive and/or community-based interventions for alcohol use. Second, given our sample size, we were limited in the number of clusters we could uncovered; it is possible that there are conceptually distinct sub-clusters that we were underpowered to uncover with this sample. Finally, we provided participants with a pre-specified list of potential RALD based on review of the literature and consultation with clinical experts, but this list was not exhaustive and might yet oversimplify complex decision making. Further, the relative weight that youth place on pre-specified RALD (both overall and at certain ages) may not have be fully captured in the survey rating scheme. Despite these design limitations, we uncovered distinct clusters defined by pre-specified and free text RALD that strongly associated with alcohol use, suggesting identification of RALD that may play a role in tempering alcohol use among YCMC.
4.1. Conclusion
Concerns about the impact of alcohol on chronic disease and medication interactions may be uniquely protective for YCMC. Future research is needed to understand how these salient RALD can be incorporated into targeted interventions and whether doing so delays or reduces use and improves health outcomes. Specifically, interventions that use tailored and targeted messaging to help YCMC understand their particular vulnerabilities and influence behavior may be impactful and could offer enormous return on investment for the growing population of youth living with a chronic illness, a complex and costly group.
Supplementary Material
Acknowledgements:
The authors acknowledge the contributions of Aria Wiseblatt in assisting with the preparation of this manuscript for submission and Julie Lunstead and Elizabeth Harstad in assisting with thematic coding of free-text responses. In addition, the authors thank Drs. Fatma Dedeoglu, Laurie Fishman, Katharine Garvey, Andrew MacGinnitie, Paul Rufo, and Joseph Wolfsdorf for facilitating access to patients and enabling this research. This work was supported by grants from the National Institutes of Health (1R01AA021913-01; PIs: Levy and Weitzman) and the Agency for Healthcare Research and Quality (K12HS022986; PI: Finkelstein), and by the Boston Children’s Hospital OFD/BTREC/CTREC Faculty Career Development Fellowship (400384; PI: Wisk).
Footnotes
Financial disclosure: The authors have no financial relationships or conflicts of interest.
References
- Anderson KG, et al. , 2011. To drink or not to drink: motives and expectancies for use and nonuse in adolescence. Addict Behav. 36(10), 972–979. doi: 10.1016/j.addbeh.2011.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernards S, et al. , 2009. ‘I have no interest in drinking’: a cross-national comparison of reasons why men and women abstain from alcohol use. Addiction. 104(10), 1658–1668. doi: 10.1111/j.1360-0443.2009.02667.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonomo Y, et al. , 2001. Adverse outcomes of alcohol use in adolescents. Addiction. 96(10), 1485–1496. doi: 10.1080/09652140120075215 [DOI] [PubMed] [Google Scholar]
- Bonomo YA, et al. , 2004. Teenage drinking and the onset of alcohol dependence: a cohort study over seven years. Addiction. 99(12), 1520–1528. doi: 10.1111/j.1360-0443.2004.00846.x [DOI] [PubMed] [Google Scholar]
- Brown SL, & West C, 2015. Sequencing the threat and recommendation components of persuasive messages differentially improves the effectiveness of high- and low-distressing imagery in an anti-alcohol message in students. Br J Health Psychol. 20(2), 324–340. doi: 10.1111/bjhp.12103 [DOI] [PubMed] [Google Scholar]
- Charrad M, et al. , 2014. NbClust: An R Package for Determining the Relevant Number of Clusters in a Data Set. Journal of Statistical Software. 61(6), 1–36. [Google Scholar]
- Creswell PD, et al. , 2014. Parental depressive symptoms and childhood cancer: the importance of financial difficulties. Support Care Cancer. 22(2), 503–511. doi: 10.1007/s00520-013-2003-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epler AJ, et al. , 2009. Reasons for abstaining or limiting drinking: a developmental perspective. Psychol Addict Behav. 23(3), 428–442. doi: 10.1037/a0015879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foxcroft DR, & Tsertsvadze A, 2012. Universal alcohol misuse prevention programmes for children and adolescents: Cochrane systematic reviews. Perspect Public Health. 132(3), 128–134. doi: 10.1177/1757913912443487 [DOI] [PubMed] [Google Scholar]
- Harstad E, et al. , 2017. Substance Use Among Adolescents with Attention-Deficit/Hyperactivity Disorder: Reasons for Use, Knowledge of Risks, and Provider Messaging/Education. J Dev Behav Pediatr. 38(6), 417–423. doi: 10.1097/DBP.0000000000000461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollen PJ, et al. , 2019. Comparison of two cohorts of medically at-risk adolescents engaging in substance use (asthmatics and cancer survivors): Clinical predictors for monitoring care. J Am Assoc Nurse Pract doi: 10.1097/JXX.0000000000000171 [DOI] [PubMed] [Google Scholar]
- Hollen PJ, et al. , 2013. A substance use decision aid for medically at-risk adolescents: results of a randomized controlled trial for cancer-surviving adolescents. Cancer Nurs. 36(5), 355–367. doi: 10.1097/NCC.0b013e31827910ba [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang JH, et al. , 2011. Endorsed reasons for not drinking alcohol: a comparison of college student drinkers and abstainers. J Behav Med. 34(1), 64–73. doi: 10.1007/s10865-010-9272-x [DOI] [PubMed] [Google Scholar]
- Johnson TJ, & Cohen EA, 2004. College students’ reasons for not drinking and not playing drinking games. Subst Use Misuse. 39(7), 1137–1160. [DOI] [PubMed] [Google Scholar]
- Koning IM, et al. , 2011. Why target early adolescents and parents in alcohol prevention? The mediating effects of self-control, rules and attitudes about alcohol use. Addiction. 106(3), 538–546. doi: 10.1111/j.1360-0443.2010.03198.x [DOI] [PubMed] [Google Scholar]
- Kuntsche E, et al. , 2005. Why do young people drink? A review of drinking motives. Clin Psychol Rev. 25(7), 841–861. doi: 10.1016/j.cpr.2005.06.002 [DOI] [PubMed] [Google Scholar]
- Levy S, et al. , 2016. A Screening Tool for Assessing Alcohol Use Risk among Medically Vulnerable Youth. PLoS One. 11(5), e0156240. doi: 10.1371/journal.pone.0156240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunstead J, et al. , 2019. Screening and Counseling for Alcohol Use in Adolescents With Chronic Medical Conditions in the Ambulatory Setting. J Adolesc Health 64(6), 804–806. doi: 10.1016/j.jadohealth.2019.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackie CJ, et al. , 2011. A systematic evaluation and validation of subtypes of adolescent alcohol use motives: genetic and environmental contributions. Alcohol Clin Exp Res. 35(3), 420–430. doi: 10.1111/j.1530-0277.2010.01359.x [DOI] [PubMed] [Google Scholar]
- Merrill JE, et al. , 2016. Trajectories and correlates of reasons for abstaining or limiting drinking during adolescence. Addict Behav. 52, 1–7. doi: 10.1016/j.addbeh.2015.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech RA, et al. , 2016. Monitoring the Future National Survey Results on Drug Use 1975–2015: Volume 1, Secondary School Students. Retrieved from Ann Arbor, Mi: http://www.monitoringthefuture.org/pubs/monographs/mtf-vol1_2015.pdf [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism, & American Academy of Pediatrics, 2015. Alcohol Screening and Brief Intervention for Youth: A Practitioner’s Guide. Retrieved from Rockville, MD: https://pubs.niaaa.nih.gov/publications/Practitioner/YouthGuide/YouthGuide.pdf [Google Scholar]
- Patrick ME, & Maggs JL, 2008. Short-term changes in plans to drink and importance of positive and negative alcohol consequences. J Adolesc. 31(3), 307–321. doi: 10.1016/j.adolescence.2007.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, & Schulenberg JE, 2011. How trajectories of reasons for alcohol use relate to trajectories of binge drinking: National panel data spanning late adolescence to early adulthood. Dev Psychol. 47(2), 311–317. doi: 10.1037/a0021939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, & Schulenberg JE, 2013. Prevalence and predictors of adolescent alcohol use and binge drinking in the United States. Alcohol Res. 35(2), 193–200. [PMC free article] [PubMed] [Google Scholar]
- Pollock EA, et al. , 2013. Correlates of physiological and psychological stress among parents of childhood cancer and brain tumor survivors. Acad Pediatr. 13(2), 105–112. doi: 10.1016/j.acap.2012.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price S, et al. , 2010. Methotrexate use and alcohol. Clin Exp Rheumatol. 28(5 Suppl 61), S114–116. [PubMed] [Google Scholar]
- Rinker DV, & Neighbors C, 2013. Reasons for not drinking and perceived injunctive norms as predictors of alcohol abstinence among college students. Addict Behav. 38(7), 2261–2266. doi: 10.1016/j.addbeh.2013.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, et al. , 2003. Scoring Manual: Diagnostic Interview Schedule for Children (DISC-IV). Retrieved from New York, NY: [Google Scholar]
- Turner BC, et al. , 2001. The effect of evening alcohol consumption on next-morning glucose control in type 1 diabetes. Diabetes Care. 24(11), 1888–1893. [DOI] [PubMed] [Google Scholar]
- Ware JE, et al. , 1993. SF-36 Health Survey Manual and Interpretation Guide. Retrieved from Boston, MA: http://www.worldcat.org/title/sf-36-health-survey-manual-and-interpretation-guide/oclc/476071432?referer=di&ht=edition [Google Scholar]
- Weitzman ER, et al. , 2018. Alcohol Use and Alcohol-Interactive Medications Among Medically Vulnerable Youth. Pediatrics. 142(4). doi: 10.1542/peds.2017-4026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzman ER, et al. , 2019. Perspectives on substance use among youth with chronic medical conditions and implications for clinical guidance and prevention: A qualitative study. PLoS One. 14(1), e0209963. doi: 10.1371/journal.pone.0209963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzman ER, et al. , 2015. Alcohol and Marijuana Use and Treatment Nonadherence Among Medically Vulnerable Youth. Pediatrics. 136(3), 450–457. doi: 10.1542/peds.2015-0722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisk LE, & Weitzman ER, 2016. Substance Use Patterns Through Early Adulthood: Results for Youth With and Without Chronic Conditions. Am J Prev Med 51(1), 33–45. doi: 10.1016/j.amepre.2016.01.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisk LE, & Weitzman ER, 2017. Expectancy and Achievement Gaps in Educational Attainment and Subsequent Adverse Health Effects Among Adolescents With and Without Chronic Medical Conditions. J Adolesc Health 61(4), 461–470. doi: 10.1016/j.jadohealth.2017.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisk LE, & Witt WP, 2012. Predictors of delayed or forgone needed health care for families with children. Pediatrics. 130(6), 1027–1037. doi: 10.1542/peds.2012-0668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witt WP, et al. , 2011. Healthcare-Related Financial Burden among Families in the U.S.: The Role of Childhood Activity Limitations and Income. J Fam Econ Issues 32(2), 308–326. doi: 10.1007/s10834-011-9253-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeager DS, et al. , 2018. Why Interventions to Influence Adolescent Behavior Often Fail but Could Succeed. Perspect Psychol Sci 13(1), 101–122. doi: 10.1177/1745691617722620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeigler DW, et al. , 2005. The neurocognitive effects of alcohol on adolescents and college students. Prev Med. 40(1), 23–32. doi: 10.1016/j.ypmed.2004.04.044 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.