Abstract
Aim
The aim of the present study was to investigate the cross-sectional association between physical activity levels with depressive symptoms, anxiety symptoms, and positive mental well-being in a sample of the UK public social distancing owing to COVID-19.
Method
This paper presents pre-planned interim analyses of data from a cross-sectional epidemiological study. Levels of physical activity during COVID-I9 social distancing were self-reported. Mental health was measured using the Beck Anxiety and Depression Inventory. Mental wellbeing was measured using The Short Warwick-Edinburgh Mental Well-being Scale. Participants also reported on sociodemographic and clinical data. The association between physical activity and mental health was studied using regression models.
Results
902 adults were included in this study (63.8% of women and 50.1% of people aged 35–64 years). After adjusting for covariates, there was a negative association between moderate-to-vigorous physical activity per day in hours and poor mental health (OR = 0.88, 95% CI = 0.80–0.97). Similar findings were obtained for moderate-to-severe anxiety symptoms, moderate-to-severe depressive symptoms and poor mental wellbeing.
Conclusions
In the present sample of UK adults social distancing owing to COVID-19 those who were physically active have better overall mental health. Owing, to the cross-sectional design of the present study the direction of the association cannot be inferred.
Keywords: COVID-19, SARS-COV-2, Mental health, Social distancing, Physical activity
Highlights
-
•
We investigated the association between physical activity and mental health in the UK public during COVID-19 “lockdown”.
-
•
In this sample of UK adults those who were physically active had better overall mental health.
-
•
Owing, to the cross-sectional design of the present study the direction of the association cannot be inferred.
1. Introduction
In March 2020, the WHO declared the COVID-19 outbreak a global pandemic. COVID-19 is caused by SARS-CoV-2, a variant of coronavirus. As of June 12, 2020 (07:00am CET), more than 7,514,559 cases have been diagnosed globally, with over 421,458 fatalities https://coronavirus.jhu.edu/map.html. COVID-19 is a respiratory virus that is transmitted by large respiratory droplets and direct contact with infected secretions. Therefore, on March 23, 2020 the UK government enforced restrictions that limited the movement of people to reduce the risk of transmission, referred to in this paper as social distancing. Citizens were required to stay at home to help stop the spread of coronavirus, apart for very limited purposes: 1) shopping for basic necessities, for example food and medicine, which must be as infrequent as possible 2) one form of exercise a day, for example a run, walk, or cycle – alone or with members of an individual's household 3) any medical need, including to donate blood, avoid or escape risk of injury or harm, or to provide care or to help a vulnerable person and 4) travelling for work purposes, but only where not possible to work from home. It should also be noted here that prior to the implementation of this population measure, individuals who were at high risk of serious complications if they contracted COVID-19, lived with someone who was at high risk of serious complications if contracted COVID-19, and the elderly were encouraged to engage in social distancing.
The World Health Organisation has recognised that such social distancing measures may result in people becoming more anxious, angry, stressed, agitated, and withdrawn (World Health Organisation, 2020). Recent research has shown that levels of poor mental health are high during COVID-19 related social distancing. For example, in one study of 932 UK adults social distancing owing to COVID-19, 36.8% of the population reported having poor mental health (Smith et al., 2020). Moreover, poor mental health was associated with being female, a younger age, lower annual income, being a current smoker and having a physical multimorbidity. Other research has found similar findings (Wang et al., 2020).
Engaging in physical activity may influence mental health during social distancing related to COVID-19. A large body of literature exists showing that regular and sustained participation in physical activity is associated with positive mental health. For example, a meta-analyses of 49 prospective studies concluded that available evidence supports the notion that physical activity can confer protection against the emergence of depression regardless of age and geographical region (Schuch et al., 2018). Another meta-analyses concluded that available evidence suggests that engaging in physical activity protects against anxiety symptoms and disorders (McDowell et al., 2019). Other research on mental health per se has also shown a similar association (White et al., 2017).
However, although physical activity has been shown to be beneficial for mental health, the role physical activity may play in relation to mental health during social distancing owing to COVID-19 is currently not known. It is presumed that physical activity will protect against poor mental health in this situation, but to date, it has not been empirically investigated. This evidence will be important as inactive individuals with poor mental health may require additional support as countries continue to manage peri-COVID-19 and plan forward for a post-COVID-19 recovery phase.
Therefore, the aim of the present study was to investigate, through an epidemiological survey, cross-sectional associations between physical activity and depressive symptoms, anxiety symptoms, and positive mental well-being in a sample of the UK public social distancing owing to COVID-19. It should be noted here that cross-sectional surveys provide information on the relationships between physical activity and mental health but provide no evidence of direction of causal effects.
2. Methods
This paper presents pre-planned interim analysis of data from a cross-sectional epidemiological study, administered through an online survey. The study was launched on March 17, 2020, 17 days after the first case of COVID-19 was diagnosed in the UK. The study was approved by the Anglia Ruskin University Research Ethics Committee (March 16, 2020).
Participants were recruited through social media and through national media outlets (BBC, March 26th 2020) and by distributing an invite to participate through existing researcher networks. Adults aged 18 years and over, currently residing in the UK and social-distancing (i.e. following UK government enforced restrictions that limited movement of people) due to COVID-19 were eligible to participate. Participants were directed to a data encrypted website where they indicated their consent to participate after reading an information sheet. Before completing the survey participants were asked if they were currently social distancing and over 18 years of age, if the participants response was affirmative to both questions then the participant was asked to complete the survey and if the response was no to either of those questions then the participants was asked to not complete the survey.
2.1. Exposure variable
Participants were asked to recall the minutes of vigorous and moderate physical activity they currently undertake on an average day. Vigorous physical activities refer to activities that take hard physical effort and make you breathe much harder than normal. Moderate activities refer to activities that take moderate physical effort and make you breathe somewhat harder than normal. Participants were asked: 1) “How much time on an average day have you spent in vigorous activity since social distancing?“; and 2) “How much time on an average day have you spent in moderate activity since social distancing?” Responses were reported in hours and minutes. Physical activity when social distancing was included in the analyses as a dichotomous (sufficient physical activity per day: yes or no) and a continuous variable (number of minutes of moderate-to-vigorous physical activity per day). Following the WHO recommendations on physical activity levels per week (i.e., at least 150 min of moderate physical activity and/or 75 min of vigorous physical activity in adults aged ≥18 years), sufficient physical activity per day was defined as approximatively 21 min of moderate physical activity and/or 11 min of vigorous physical activity per day.
2.2. Outcome variable
Mental health was measured using the Becks Anxiety Inventory (BAI) and Becks Depression Inventory (BDI). These are both 21-item questionnaires with higher BAI and BDI scores indicating more severe anxiety and depressive symptoms. The short Warwick-Edinburgh Mental Well-being Scale is a 7-item measure of mental well-being (Ng Fat et al., 2017; Stewart-Brown et al., 2009). Poor mental health was defined as the presence of at least one of the following three criteria: moderate-to-severe anxiety symptoms (BAI score ≥16), moderate-to severe depressive symptoms (BDI score ≥20) (Carney et al., 2011) and poor mental wellbeing (SWEMWBS metric score ≤15.8). (Warwick Medical School, 2020). Mental health is a multi-component construct. Although traditional aspects of mental health have been considered in isolation, they may be experienced simultaneously. Therefore, we created a mental health score to capture a wider range of aspects of mental health in individuals than usually is examined.
2.3. Covariates
Demographic data was collected, including sex, age (in 10-year age bands), marital status (single/separated/divorced/widowed or married/in a domestic partnership), employment, and annual household income (<£15,000, £15,000-<£25,000, £25,000-<£40,000, £40,000<£60,000, ≥£60,000).
Measures of health status included whether respondents were a current smoker and consumer of alcohol (y/n), and the presence of physical multimorbidity (i.e., more than three chronic diseases, this is consistent with previous research). Chronic physical diseases included obesity, hypertension, myocardial infarction, angina pectoris and other coronary diseases, other cardiac diseases, varicose veins of lower extremities, osteoarthritis, chronic neck pain, chronic low back pain, chronic allergy (excluding allergic asthma), chronic bronchitis, emphysema or chronic obstructive pulmonary disease (COPD), type 1 diabetes, type 2 diabetes, diabetic retinopathy, cataract, peptic ulcer disease, urinary incontinence or urine control problems, hypercholesterolemia, chronic skin disease, chronic constipation, liver cirrhosis and other hepatic disorders, stroke, chronic migraine and other.
2.4. Statistical analyses
Differences in the sample characteristics by level of physical activity per day were tested with chi-squared tests for categorical variables and analysis of variance (ANOVA) for the number of chronic physical conditions. The prevalence of poor mental health, moderate-to-severe anxiety symptoms, moderate-to-severe depressive symptoms, and poor mental wellbeing was further estimated in the overall population and by level of physical activity per day. Effect sizes were calculated using Cramer's V for all variables except the number of chronic physical conditions (eta-squared). Finally, associations between moderate-to-vigorous physical activity per day in hours (independent variable) and several mental health outcomes (poor mental health, moderate-to-severe anxiety symptoms, moderate-to-severe depressive symptoms, and poor mental wellbeing; dependent variables) were examined in regression models adjusted for sex, age, marital status, employment, income, current smoking, current alcohol consumption, and the number of chronic physical conditions. The level of statistical significance was set at p-value < 0.05. All analyses were performed with R 3.6.2 (The R Foundation).
3. Results
There were 902 adults included in this study (63.8% of women and 50.1% of people aged 35–64 years; Table 1 ). Age ≥65 years, being married/in a domestic partnership and being unemployed were characteristics significantly more frequently associated with individuals who engaged in >90 min rather than 0–30 min of moderate-to-vigorous physical activity per day, while the distribution of income significantly varied by physical activity level. The prevalence of poor mental health, moderate-to-severe anxiety symptoms, moderate-to-severe depressive symptoms, and poor mental wellbeing in the overall population was 35.8%, 30.7%, 18.8%, and 9.9%, respectively (Table 2 ), and these figures significantly decreased with increasing physical activity.
Table 1.
Sample characteristics (overall and by level of physical activity per day).
| Characteristics | Category | Overall (N = 902) | Moderate-to-vigorous physical activity per day |
Effect sizea | P-valueb | ||
|---|---|---|---|---|---|---|---|
| 0–30 min (n = 330) | >30–90 min (n = 277) | >90 min (n = 295) | |||||
| Sex | Male | 36.2% | 38.3% | 34.9% | 35.1% | 0.03 | 0.603 |
| Female | 63.8% | 61.7% | 65.1% | 64.9% | |||
| Age | 18–34 years | 31.6% | 39.7% | 31.8% | 22.4% | 0.18 | <0.001 |
| 35–64 years | 50.1% | 52.4% | 50.5% | 47.1% | |||
| ≥65 years | 18.3% | 7.9% | 17.7% | 30.5% | |||
| Marital status | Single/separated/divorced/widowed | 44.8% | 54.5% | 39.1% | 39.2% | 0.15 | <0.001 |
| Married/in a domestic partnership | 55.2% | 45.5% | 60.9% | 60.8% | |||
| Employment | No | 41.4% | 37.3% | 34.7% | 52.2% | 0.16 | <0.001 |
| Yes | 58.6% | 62.7% | 65.3% | 47.8% | |||
| Annual income | <£15,000 | 14.6% | 20.5% | 8.1% | 14.0% | 0.13 | <0.001 |
| £15,000-<£25,000 | 18.5% | 18.0% | 15.4% | 21.9% | |||
| £25,000-<£40,000 | 23.0% | 17.4% | 28.6% | 24.0% | |||
| £40,000-<£60,000 | 21.0% | 21.4% | 23.4% | 18.2% | |||
| ≥£60,000 | 23.0% | 22.6% | 24.5% | 21.9% | |||
| Current smoking | No | 88.3% | 86.6% | 90.9% | 87.8% | 0.06 | 0.248 |
| Yes | 11.7% | 13.4% | 9.1% | 12.2% | |||
| Current alcohol consumption | No | 32.7% | 34.6% | 31.8% | 31.4% | 0.03 | 0.655 |
| Yes | 67.3% | 65.4% | 68.2% | 68.6% | |||
| Number of chronic physical conditions | Mean (standard deviation) | 1.74 (2.02) | 1.69 (2.03) | 1.71 (1.99) | 1.83 (2.05) | 0.00 | 0.675 |
Abbreviation: ANOVA analysis of variance. Moderate-to-vigorous physical activity per day was self-reported and was used as a three-category variable (0–30, >30–90 and > 90 min). Values are percentages unless otherwise stated.
Effect size was calculated using Cramer's V for categorical and eta-squared for the number of chronic physical conditions (continuous variable).
P-values were based on chi-squared tests for categorical variables and ANOVA for the number of chronic physical conditions (continuous variable).
Table 2.
Prevalence of poor mental health, moderate-to-severe anxiety symptoms, moderate-to-severe depressive symptoms, and poor mental wellbeing in the overall population and by physical activity level.
| Population | Poor mental health |
Moderate-to-severe anxiety symptoms |
Moderate-to-severe depressive symptoms |
Poor mental wellbeing |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence | Effect sizea | P-valueb | Prevalence | Effect sizea | P-valueb | Prevalence | Effect sizea | P-valueb | Prevalence | Effect sizea | P-valueb | |
| Overall | 35.8 | – | – | 30.7 | – | – | 18.8 | – | – | 9.9 | – | – |
| Moderate-to-vigorous physical activity per day | ||||||||||||
| 0–30 min | 47.0 | 0.18 | <0.001 | 41.2 | 0.18 | <0.001 | 28.2 | 0.18 | <0.001 | 14.8 | 0.13 | <0.001 |
| >30–90 min | 32.1 | 27.4 | 14.1 | 8.3 | ||||||||
| >90 min | 26.8 | 22.0 | 12.9 | 5.8 | ||||||||
Participants were considered to have poor mental health if they displayed moderate-to-severe anxiety symptoms, moderate-to-severe depressive symptoms and/or poor mental wellbeing. Oderate-to-vigorous physical activity per day was self-reported and was used as a three-category variable (0–30, >30–90 and > 90 min).
Effect size was calculated using Cramer's V.
P-values were based on chi-squared tests.
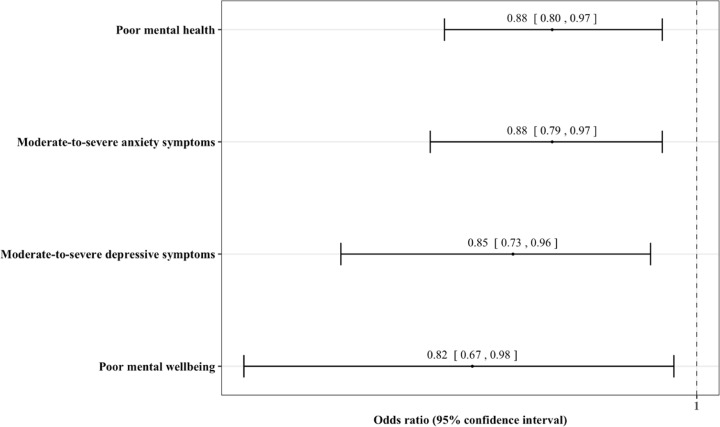
Finally, after adjusting for several potential confounding factors (sex, age, marital status, employment, income, current smoking, current alcohol consumption, and the number of chronic physical conditions), there was a negative association between moderate-to-vigorous physical activity per day in hours (independent variable) and poor mental health (dependent variable; OR = 0.88, 95% CI = 0.80–0.97; Fig. 1 ). Similar findings were obtained for moderate-to-severe anxiety symptoms, moderate-to-severe depressive symptoms and poor mental wellbeing.
Fig. 1.
Associations between physical activity and several psychiatric outcomes in UK self-isolated adults during the COVID-19 pandemic.
Abbreviation: COVID-19 coronavirus disease 2019. Participants were considered to have poor mental health if they displayed moderate-to-severe anxiety symptoms, moderate-to-severe depressive symptoms and/or poor mental wellbeing.
Moderate-to-vigorous physical activity per day was self-reported and was included in the logistic regression models as a continuous variable (physical activity per day in hours).
Logistic regression analyses were adjusted for sex, age, marital status, employment, income, current smoking, current alcohol consumption, and the number of chronic physical conditions.
4. Discussion
In the present sample of the UK public social distancing owing to COVID-19 there was a negative association between moderate-to-vigorous physical activity per day in hours and poor mental health, after controlling for several important covariates. Moreover, similar findings were found for depression and anxiety symptoms as well as poor mental wellbeing.
Taken together the present findings suggest that participating in higher levels of physical activity during COVID-19 self-isolation is associated with better total mental health status. These findings support that of the literature during non-pandemic times (McDowell et al., 2019; Schuch et al., 2018; White et al., 2017). Several plausible mechanisms may explain the observed association between higher levels of physical activity and better reported mental health during the COVID-19 pandemic including increases in neurogenesis and reductions in inflammatory and oxidant markers (Schuch et al., 2016), as well as improvements in self-esteem (Schuch et al., 2018). However, it is important to highlight that owing to the cross-sectional design employed in the present study it is not known whether mental health problems lead to lower levels of physical activity or whether lower levels of physical activity lead to mental health problems. It is likely that the relationship is bi-directional. These findings suggest that those who have low levels of physical activity during COVID-19 social distancing may need to be targeted with support for their mental health going forward. Indeed, high levels of self-reported anxiety observed in a previous article in a sample of UK adults social distancing owing to COVID-19 are especially concerning and could precipitate a future public health crisis if left untreated (Smith et al., 2020).
Findings from the present study must be interpreted in light of its limitations. First, participants were asked to self-report their physical activity level and thus potentially introducing self-reporting bias into the findings. Second, a high proportion of adults in the present study met physical activity guidelines, especially the proportion of those over 65 engaging in >90 min of moderate to vigorous physical activity. It is possible that this may be partially explained by self-selection bias. Finally, we did not record data on whether people were shielding (i.e. unable to leave the home for any reason). However, most participants in the present study were young to middle-age adults and thus not including such data in the analyses is unlikely to influence the present findings.
In conclusion, in the present sample of UK adults social distancing owing to COVID-19 those who were physically active have better overall mental health. Owing, to the cross-sectional design of the present study the direction of the association cannot be inferred. The authors of the present manuscript believe that there is no need for further self-reported cross-sectional studies on this topic within the UK population. Researchers should now focus on utilizing longitudinal data when available to infer the direction of the association.
Funding
None.
Declaration of competing interest
None.
References
- Carney C.E., Moss T.G., Harris A.L., Edinger J.D., Krystal A.D. Should we be anxious when assessing anxiety using the Beck Anxiety Inventory in clinical insomnia patients? Journal of Psychiatric Research. 2011;45(9):1243–1249. doi: 10.1016/j.jpsychires.2011.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hooft E.A.J., van Hooff M.L.M. The state of boredom: Frustrating or depressing? Motivation and Emotion. 2018;42(6):931–946. doi: 10.1007/s11031-018-9710-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDowell C.P., Dishman R.K., Gordon B.R., Herring M.P. Physical activity and anxiety: A systematic review and meta-analysis of prospective cohort studies. American Journal of Preventive Medicine. 2019;57(4):545–556. doi: 10.1016/j.amepre.2019.05.012. [DOI] [PubMed] [Google Scholar]
- Ng Fat L., Scholes S., Boniface S., Mindell J., Stewart-Brown S. Evaluating and establishing national norms for mental wellbeing using the short warwick–edinburgh mental well-being Scale (SWEMWBS): Findings from the health survey for england. Quality of Life Research. 2017;26(5):1129–1144. doi: 10.1007/s11136-016-1454-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuch F.B., Deslandes A.C., Stubbs B., Gosmann N.P., Silva C. T. B. da, Fleck M.P. de A. Neurobiological effects of exercise on major depressive disorder: A systematic review. Neuroscience & Biobehavioral Reviews. 2016;61:1–11. doi: 10.1016/j.neubiorev.2015.11.012. [DOI] [PubMed] [Google Scholar]
- Schuch F.B., Vancampfort D., Firth J., Rosenbaum S., Ward P.B., Silva E.S., Hallgren M., Ponce De Leon A., Dunn A.L., Deslandes A.C., Fleck M.P., Carvalho A.F., Stubbs B. Physical activity and incident depression: A meta-analysis of prospective cohort studies. American Journal of Psychiatry. 2018;175(7):631–648. doi: 10.1176/appi.ajp.2018.17111194. [DOI] [PubMed] [Google Scholar]
- Smith L., Jacob L., Yakkundi A., McDermott D., Armstrong N.C., Barnett Y., López-Sánchez G.F., Martin S., Butler L., Tully M.A. Correlates of symptoms of anxiety and depression and mental wellbeing associated with COVID-19: A cross-sectional study of UK-based respondents. Psychiatry Research. 2020;291:113138. doi: 10.1016/j.psychres.2020.113138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart-Brown S., Tennant A., Tennant R., Platt S., Parkinson J., Weich S. Internal construct validity of the warwick-edinburgh mental well-being Scale (WEMWBS): A rasch analysis using data from the scottish health education population survey. Health and Quality of Life Outcomes. 2009;7(1):15. doi: 10.1186/1477-7525-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warwick Medical School . Collect, score, analyse and interpret WEMWBS. 2020. Warwick medical School.https://warwick.ac.uk/fac/sci/med/research/platform/wemwbs/using/howto/ [Google Scholar]
- White R.L., Babic M.J., Parker P.D., Lubans D.R., Astell-Burt T., Lonsdale C. Domain-specific physical activity and mental health: A meta-analysis. American Journal of Preventive Medicine. 2017;52(5):653–666. doi: 10.1016/j.amepre.2016.12.008. [DOI] [PubMed] [Google Scholar]
- World Health Organisation . 2020. Mental health and psychosocial considerations during the COVID-19 outbreak. [Google Scholar]