Highlights
-
•
After severe SARS-CoV2 infection, radiological abnormalities such as encephalopathies may be seen.
-
•
An extensive radiological encephalopathy may not correlate with abnormalities in cerebrospinal fluid.
-
•
An extensive radiological encephalopathy does not correlate with the severity of symptoms.
Keywords: SARS-CoV2, COVID-19, Coronavirus, Neuroradiological lesions, Neurological symptoms, Encephalopathy
Abstract
Concerning the letter by Moriguchi et al., we describe our experience with a case of encephalopathy with and atypical damage on magnetic resonance imaging (MRI) in a patient with severe infection due to the SARS-CoV2 virus. A 56-year-old woman, without previous pathologies, developed cough, fever, and respiratory failure for five days, after returning from a 6-day trip to Venice. Chest radiography shows a large bilateral interstitial infiltrate. In the first 24 hours, she was admitted to the Intensive Care Unit (ICU) for severe respiratory failure and positive protein chain reaction-PCR in nasal exudate. She needed intubation for ten days. In the first 48 hours outside the ICU, she developed an acute confusional syndrome (hyperactive delirium). Neurological examination showed temporal-spatial disorientation and incoherent fluent speech.
An electroencephalogram (EEG) showed generalized hypovoltaic activity. Cranial magnetic resonance imaging showed a bilateral and symmetrical increase in the supratentorial white matter's signal intensity, with a discrete thickening of both temporal lobes, with a slight increase in signal intensity and a sequence of normal diffusion. The lumbar puncture showed no changes (glucose 71 mg/dL, protein 30 mg/dL, 1 leukocyte). Within 72 hours of starting symptoms, she was neurologically asymptomatic. Our final diagnosis was an inflammatory encephalopathy related to a SARS-CoV2 infection.
The appearance of SARS-CoV2 was described in December 2019 in China, but it was not until March 2020 when the pandemic reached Spain. Although this virus mainly presents a respiratory involvement, we have observed the appearance of neurological symptoms (headache, myalgia, hyposmia/anosmia, dysgeusia, insomnia) and diseases (stroke, encephalitis, or Guillain-Barré syndrome) (Mao et al., 2020, Li et al., 2020, Helms et al., 2020, De Melo Espíndola et al., 2020).
Concerning the letter by Moriguchi et al., we describe our experience with a case of encephalopathy with an atypical damage on magnetic resonance imaging (MRI) (Moriguchi et al., 2020).
A 56-year-old woman, without previous pathologies, came to the Emergency Department (ED) for cough, fever, and respiratory failure for five days, after returning from a 6-day trip to Venice. Chest radiography shows a large bilateral interstitial infiltrate. The analysis also highlighted lactate dehydrogenase: 537 U/L, C-reactive protein: 76.7 mg/L, d-dimer: 1041 ng/Ml, Interleukin-6: 26, and procalcitonin levels: 0.07 ng/ml. Arterial blood gas showed: pH 7.50, pO2: 32.9, and pCO2: 29.4. She did not develop leukocytosis nor kidney failure.
In the first 24 hours, she was admitted to the Intensive Care Unit (ICU) for acute severe respiratory failure, with 70% oxygen saturation despite oxygen therapy, and extensive bilateral pneumonia secondary to SARS-CoV2 (positive protein chain reaction-PCR in nasal exudate). She required intubation for ten days, and received ceftriaxone, ritonavir/lopinavir, corticosteroids, and hydroxychloroquine, with clinical improvement. In the first 48 hours outside the ICU, she developed an acute confusional syndrome (hyperactive delirium). On neurological examination, she exhibited temporal-spatial disorientation, incoherent fluent speech, without other neurological symptoms.
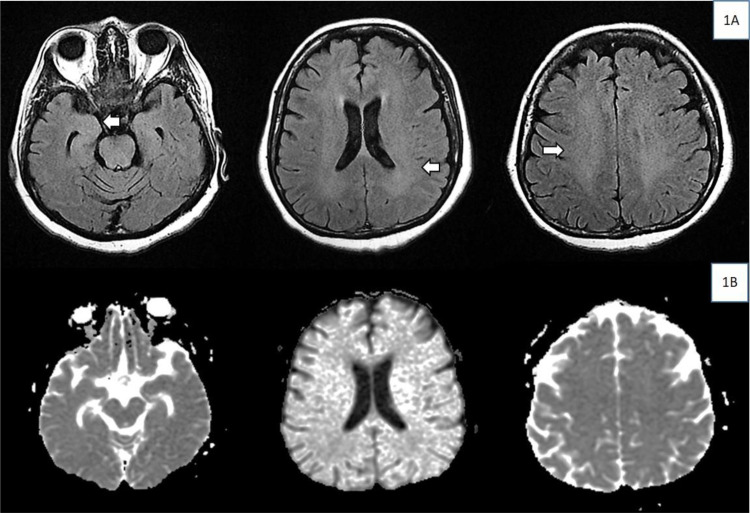
An electroencephalogram (EEG) was performed in the first 48 hours, showing generalized hypovoltaic activity, not related to the drugs present at that time. Cranial magnetic resonance imagine was also performed, which showed a bilateral and symmetrical increase in the signal intensity of the supratentorial white matter, with a discrete thickening of both temporal lobes with a slight increase in signal intensity, and a sequence of normal diffusion (Figure 1 ). The lumbar puncture showed no changes (glucose 71, protein 30, 1 leukocyte). Within 72 hours of starting symptoms, she was neurologically asymptomatic. Our final diagnosis was an inflammatory encephalopathy related to SARS-CoV2 infection.
Figure 1.
Increased signal intensity of the supratentorial white matter bilaterally and symmetrically (1A), with a slight thickening and increased signal of both temporal lobes. There is no restriction on diffusion sequence (1B).
We consider the possibility that the demonstrated radiological lesions are secondary to an inflammatory reaction, instead of a tissue injury due to viral invasion.
Conflict of interest, funding source, and ethical approval
The authors declare the absence of conflict of interests and agree with the contents of the manuscript. All the data are original, they have not been sent for evaluation to any other journal. The data have not been presented in any congress or conferences. No author has received partial or total funding from any public or private institution in relation to this article.
Authors declare the absence of study sponsors in the study design, in the collection analysis, interpretation of data, and the decision to submit the manuscript for publication. We did not have any writing assistance.
This work has been evaluated and approved by the Medical Investigation Commission of our center in April 2020.
References
- De Melo Espíndola O., Siqueira M., Nascimento Soares C., Sales Dantas de Lima M.A., Celestino Bezerra Leite A.C., Queiroz Campos Araujo A. Patients with COVID-19 and neurological manifestations show indetectable SARS-CoV2 RNA leves in the cerebrospinal fluid. Int J Infect Dis. 2020;96:567–569. doi: 10.1016/j.ijid.2020.05.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helms J., Kremer S., Merdji H., Clere-Jehl R., Schenk M., Kummerlen C. Neurologic features in severe SARS-CoV-2 infection. New Engl J Med. 2020 doi: 10.1056/NEJMc2008597. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y.C., Bai W.Z., Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. 2020:1–4. doi: 10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling Mao, M. Wang, S. Chen, Q. He, J. Chang, C. Hong, et al. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: a retrospective case series study. JAMA in press. 10.1101/2020.02.22.20026500. [DOI]
- Moriguchi T., Harii N., Goto J., Harada D., Sugawara H., Takamino J. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. 2020;94:55–58. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]