Abstract
The Benign Paroxysmal Positional Vertigo (BPPV) represents the first cause of peripheral vertigo in populations and it is determined by a displacement of otoconial fragments within the semicircular canals. Following the patient’s head movements, these fragments, moving by inertia, incorrectly stimulate the canals generating vertigo. The BPPV is diagnosable by observing the nystagmus that is generated in the patient following the Dix-Hallpike maneuver used for BPPV diagnosis of vertical semi-circular canal, and, following the supine head yaw test used for lateral semi-circular canal. Correctly identifying the origin of this specific peripheral vertigo, would mean to obtain a faster diagnosis and an immediate resolution of the problem for the patient. In this context, this study aims to identify precise training activities, aimed at the application of specific diagnostic maneuverers for algorithm decisions in support of medical personnel. The evaluations reported in this study refer to the data collected in the Emergency Department of the Cardarelli Hospital of Naples. The results obtained, over a six-month observation period, highlighted the advantages of the proposed procedures in terms of costs, time and number of BPPV diagnoses.
Key words: benign paroxysmal positional vertigo, emergency department, diagnostic algorithm
Introduction
Vertigo is a distortion of perception of one’s own body movement or the environment around us, and it is caused by a vestibular apparatus disorder. The balance disorders represent one of the most common symptoms in clinical practice,1,2 and in cases of greater severity, often determine access to Emergency Departments (ED).3
Vertigo, in most cases, has a benign peripheral aetiology4 and the most frequent peripheral pathologies encountered in populations are acute vestibular syndrome and BPPV. Although it is possible that vertigo might be an expression of a more serious pathology affecting the central nervous system such as cerebellar or encephalic trunk stroke.5-9 It is also the most frequent symptom complained of by patients who go to Emergency Departments.10,11 Every year in the United States of America, visits for vertigo and/or balance disorders amount to about 5.6 million and represent 4% of the reasons for accessing Emergency Departments, at a cost of 4.4 billion dollars. The medical personnel approach is mainly focused on the differential diagnosis between peripheral origin vertigo and central origin vertigo.12 To correctly understand the patient’s acute clinical picture, neurotological skills are required by the emergency doctor.13
In the literature, a diagnostic bed-side algorithm was proposed, based on the analysis of nystagmus and Head Impulse Tests (HIT), allowing it to provide indications for differential diagnosis with high sensitivity and specificity.14 Although many studies confirm the preferential use of neuroimaging techniques for differential diagnosis rather than clinical examination,15,16 this involves not only high healthcare costs, but also a delay in diagnosing peripheral vertigo such as BPPV, susceptible as it is known as an immediate resolution with only rehabilitative treatment.
BPPV has a high population incidence17 and is easily diagnosed by observing the nystagmus characteristic generated by Dix-Hallpike and supine Head Yaw Test (HYT)18,19 even in the absence of specific instruments such as Frenzel goggles for nystagmus video, although diagnostic sensibility without video- Frenzel or simple Frenzel goggles is lower. On the contrary, if the nystagmus signs appear different from the characteristic ones, we must exclude pathologies of different origins. However, BPPV is not often identified and treated quickly in the Emergency Department.20-22
This study aims to evaluate the percentage of patients affected by BPPV who turned to the Cardarelli Hospital emergency department and the effectiveness of an exclusive diagnostic algorithm prepared for diagnosing BPPV. The obvious purpose is to reduce the time associated with long, unnecessary and expensive diagnostic procedures, avoiding the use of neuroimaging techniques and favouring clinical examination.
Materials and Methods
For the aim of the study 363 consecutive patients were selected, recruited in the Cardarelli Hospital Emergency Room from 30 April to 31 October 2018. The ages were between 18 and 93 years (average age 58,8 years), 203 patients were female (56%), and 160 were male (44%).
All patients were subjected to medical history, neurological examinations and diagnostic evaluations following the our BPPValgorithm. The most frequent concomitant diseases were hypertension, diabetes, atrial fibrillation, previous stroke. The diagnostic evaluation was performed by emergency room doctors who had completed a 10 hours weekly training for 1 month under the guidance of an Otolaryngologist and an Audiologist. The training was composed of theoretical lessons, video analysis of patients with BPPV and practical lessons on patients. The ED doctors were instructed on the correct execution of Dix-Hallpike maneuver and HYT with Frenzel goggles and given algorithms for the correct BPPV interpretation. When, at the end of the evaluation the algorithm suggested a BPPV, the patient was transferred to the ENT department to confirm the diagnosis. With the diagnosis confirmed, the rehabilitation maneuver was carried out without using any other clinical or radiological investigations.
If the clinical and neurological evaluations and the algorithm did not suggest a BPPV, the ED requested a neuroradiological diagnostic study and proceeded to transfer the patient to the Brief Emergency Department Observation to guarantee other specialist consultations, including one by the expert ENT doctor. All patients were evaluated within 12 hours by an expert ENT doctor.
Algorithm BPPV
The BPPV-Algorithm (BPPV-A), is a diagnostic algorithm based on the observation of spontaneous nystagmus signs and generated by the Dix-Hallpike HYT (Figure 1).
The first step involves studying the patient in an upright position to highlight the presence or absence of spontaneous Nystagmus (Ny).
If the spontaneous Ny is not observed on the horizontal plane, the doctor performs first of all the Dix-Hallpike. If this maneuver is positive, and there is the appearance of paroxysmal transitory nystagmus characterized by a geotropic torsional component on the frontal plane and an up-beating component on the vertical plane, it suggests a BPPV of Posterior Semicircular Canal (PSC). If the Dix-Hallpike is negative, then the HYT is performed. The appearance of a bidirectional paroxysmal geotropic or apogeotropic nystagmus indicates a BPPV of the Lateral Semicircular Canal (LSC), with respective non-ampullary or ampullary canal involvement. In both cases, the ED doctor sent the patient to an ENT doctor. If also HYT is negative, the ED doctor provides other diagnostic tests on the subject.
If the presence of a spontaneous nystagmus with rapid component on the horizontal plane is proven, the HYT is performed first of all. The appearance of bi-directional paroxysmal transitory Ny suggests to the ED doctor to send the patient to the ENT doctor to confirm BPPV diagnosis. Instead, the presence of unidirectional persistent and stationary Ny during the maneuver suggests further subject investigations on the patient.
Finally, in the case of spontaneous Ny on the frontal plane (spontaneous torsional Ny) or on the sagittal plane (vertical spontaneous Ny), the patient is immediately sent for neurological and neuroradiological examinations, because the feedback suggests an injury to the central vestibular system.
Figure 1.

The BPPV-Algorithm (BPPV-A). The exam begins with a seated patient. In the presence of a pseudo-spontaneous Nystagmus (Ny), the patient is subjected to supine Head Yaw Test (HYT). If the HYT is positive (bidirectional, bipositional, paroxysmal Ny on side), the vestibular examination is performed; if the HYT is negative (monodirectional, not paroxysmal Ny on side) further investigations are carried out. If spontaneous nystagmus is absent, the HYT and Dix-Hallpike maneuver are performed. If the Dix-Hallpike maneuver is positive, the vestibular examination is performed; if the maneuver is negative, further investigations are carried out. Vertical or torsional spontaneous nystagmus are not included.
Results
The 363 patients arrived in the emergency room, with entry diagnosis of acute vertigo, were classified by triage in 178 green code (49%), 173 (47,6%) yellow code, 12 (3%) red code.
The most associated symptoms to the entry diagnosis of acute vertigo were: nausea/vomit in 128 patients (35%), headache in 36 patients (10%), balance disorder in 199 patients (55%).
The most frequent concomitant diseases were hypertension (228 patients, 62,8%), diabetes (70 patients, 19%), atrial fibrillation (44 patients, 12%), previous stroke (21 patients, 5,7%).
All patients were subjected to medical history, neurological evaluation and BPPV-A. Out of a total of 363 patients, 188 (52%) had BPPV, 83 (23%) patients had a peripheral acute vestibular deficit, 19 patients (5%) with other peripheral pathologies, and 73 (20%) with central vertigo (Figure 2).
Specifically, 151 BPPV were found from lithiasis of PSC, of which 89 (59%) of the posterior right semicircular canal and 62 (41%) of the left posterior semicircular canal. There were also 37 BPPV from lithiasis of LSC, of which 21 (57%) involving the nonampullary arm, geotropic form (15 patients, equal to 71% with involvement of the right lateral semicircular canal and 6 patients equal to 29% of BPPV with involvement of the left lateral semicircular canal), and 16 (43%) involving the ampullary arm, apogeotropic form (10 patients, equal to 62% with involvement of the right lateral semicircular canal, and 6 patients, equal to 38% with involvement of the left lateral semicircular canal) (Figure 3).
Reliability of BPPV-A
Thanks to the BPPV-A, the BPPV was diagnosed by ED doctors in 188 patients and confirmed in all patients by the otorhinolaryngologist within a maximum of 12 hours. On the same day, all the patients underwent rehabilitation manoeuvre by the audiometric technician, and after 7 days, they were subjected to a new vestibular examination.
All patients who had been excluded from the BPPV diagnosis underwent a brain CT which, in 33 cases (19%), detected the presence of central pathology; specifically, 4 patients (12%) presented with brain metastates and primary neoplasia, 12 patients (36%) had a transient ischemic attack, 11 patients (33%) had ischemic stroke, 3 patients (9%) with haemorrhagic stroke and 3 patients (9%) with other central pathologies.
The other 142 patients, in whom the CT was negative, were admitted to the Short Observation Department pending further consultations. Of these, 83 (58%) presented an acute vestibular deficit.
None of the patients with a negative algorithm result received a final diagnosis of BPPV, thus confirming the high reliability of BPPV-A. Therefore, in our study the sensitivity and specificity in the diagnosis of BPPV using BPPV-A were 100%.
In 7% of cases otorhinolaryngologist have noticed a mismatch between diagnostic hypothesis and final diagnosis: especially the Dix-Hallpike manouvre has generated sometimes a horizontal nystagmus that was interpretated by ED doctors as a lythiasis of posterior semicircular canal.
Discussion
In this study, conducted on an unselected population of patients presented to the emergency ward for acute vertigo, was tested the effectiveness and reliability of a bed-side diagnostic algorithm (BPPV-A), that was able to identify the presence of a BPPV.
There were 410 who accessed the emergency department due to vertigo in the six months of the study, but only 363 of these patients actually had a pathology of vestibular origin.23 In fact, the patient often identified “vertigo” as a series of other symptoms that are actually part of the broad chapter of pseudo-vertigo not attributable to other problems such as those related to anxiety disorders (panic attacks, agoraphobia), intoxication, vasovagal crisis, orthostatic hypotension, etc. All patients enrolled in the study underwent the BPPV-A.
The symptoms that most accompanied the entry diagnosis of acute vertigo were in order of frequency: nausea and vomiting, headache, imbalance.
The identified comorbidities were arterial hypertension, diabetes mellitus, atrial fibrillation, coronary heart disease and previous stroke. No significant correlation between sex and nature of vertigo was identified, nor was age identified to be a predisposing factor. The BPPV in this study was diagnosed in 188 of a total 363 patients (51.7%). In 151 patients (80%), the PSC was affected and LSC in 37 patients (20%). No prevalence was found between the left and right sides. In all 188 patients identified with BPPV-A, the diagnosis was confirmed within 12 hours of accessing the emergency room by the competent doctor and always within 12 hours the patients underwent rehabilitation by the audiometric technician. The clinical check was performed 7 days later. The 175 patients who did not have a BPPV underwent further investigation. Although vertigo often has a benign peripheral aetiology,24 as in the case of BPPV, diagnosis is often late and involves an unnecessary and considerable recourse of neuroimaging techniques for differential diagnosis. The training offered to ED doctors and the algorithm provided to them have enabled, on one hand, an early and precise diagnosis and, on the other, immediate rehabilitation therapy with problem resolution within 12 hours of accessing the emergency department. This diligent patient management has also led to a reduction in health spending costs deriving from the missed execution of CT and MRI in 188 patients positive to BPPVA. The savings achieved were around € 48,316.00 in the six months of the study. It is therefore possible to argue that the BPPVA allowed an early diagnosis of BPPV in the ED with resolution of the vertigo within 12 hours of accessing the emergency department and a saving of approximately 257,00 euros for each patient, using as a reference the Regional Catalog of Specialist Services of the Campania Region. Our study shows some limitations. Even if we hadn’t diagnostic errors, we suppose that ED doctors could have some difficulties in cases of lythiasis of multiple canals; in these cases we recommend to pay attention especially to the parossistic character of nystagmous. The principal difficulty was to memorize the steps of algorithm. When they get used to the algorithm, they had no more problems.
Figure 2.
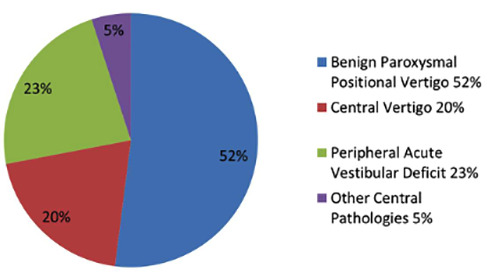
Emergency Room Access for Acute Vertigo. Out of a total of 363 patients, 188 (52%) had BPPV, 83 (23%) patients had a peripheral acute vestibular deficit, 19 patients (5%) with other peripheral pathologies, and 73 (20%) with central vertigo.
Figure 3.
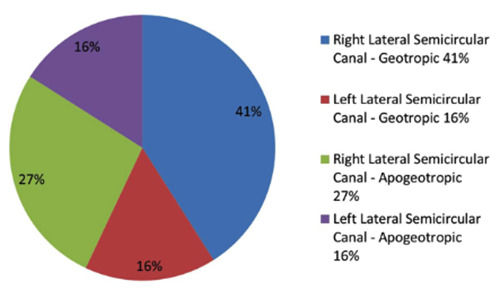
BPPV: semicircular canals involved. Out of 37 BPPV from lithiasis of LSC: the right non-ampullary arm (geotropic form) was involved in 41% and the left non-ampullary arm (geotropic form) was involved in 16%; the right ampullary arm (apogeotropic form) was involved in 27% and the left ampullary arm (apogeotropic form) was involved in 16%.
Conclusions
Even with the limitations reported, our work shows that an important and effective synergy can be created with emergency room doctors. The correct information and training and the close collaboration with the vestibologist specialist have enabled the emergency room doctors to identify patients affected by BPPV early and effectively, avoiding waste of time and significantly reducing costs for the healthcare system.
References
- 1.Lai YT, Wang TC, Chuang LJ, Chen MH, Wang PC. Epidemiology of vertigo: a National Survey. Otolaryngol Head Neck Surg 2011;145:110-6. [DOI] [PubMed] [Google Scholar]
- 2.Yin M, Ishikawa K, Wong WH, Shibata Y. A clinical epidemiological study in 2169 patients with vertigo. Auris Nasus Larynx 2009;36:30-5. [DOI] [PubMed] [Google Scholar]
- 3.Kerber KA, Meurer WJ, West BT, Fendrick AM. Dizziness presentations in U.S. emergency departments, 1995-2004. Acad Emerg Med 2008;15:744-50. [DOI] [PubMed] [Google Scholar]
- 4.Post RE, Dickerson LM. Dizziness: a diagnostic approach. Am Fam Physician 2010;82:361-89. [PubMed] [Google Scholar]
- 5.Armato E, Ferri E, Pinzani A, Ulmer E. Cerebellar haemorrhage mimicking acute peripheral vestibulopathy: the role of the video head impulse test in differential diagnosis. Acta Otorhinolaryngol Ital 2014;34:288-91. [PMC free article] [PubMed] [Google Scholar]
- 6.Casani AP, Dallan I, Cerchiai N, Lenzi R, Cosottini M, Sellari-Franceschini S. Cerebellar infarctions mimicking acute peripheral vertigo: how to avoid misdiagnosis? Otolaryngol Head Neck Surg 2013;148:475-81. [DOI] [PubMed] [Google Scholar]
- 7.Grad A, Baloh RW. Vertigo of vascular origin. Clinical and electronystagmographic features in 84 cases. Arch Neurol 1989;46:281-4. [DOI] [PubMed] [Google Scholar]
- 8.Huon LK, Wang TC, Fang TY, Chuang LJ, Wang PC. Vertigo and stroke: a national database survey. Otol Neurotol 2012;33:1131-5. [DOI] [PubMed] [Google Scholar]
- 9.Lee CC, Su YC, Ho HC, Hung SK, Lee MS, Chou P, et al. Risk of stroke in patients hospitalized for isolated vertigo: a fouryear follow-up study. Stroke 2011;42:48-52. [DOI] [PubMed] [Google Scholar]
- 10.Newman-Toker DE, Hsieh YH, Camargo CA, Pelletier AJ, Butchy GT, Edlow JA. Spectrum of dizziness visits to US emergency departments: cross-sectional analysis from a nationally representative sample. Mayo Clin Proc 2008;83:765-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ozono Y, Kitahara T, Fukushima M, Michiba T, Imai R, Tomiyama Y, et al. Differential diagnosis of vertigo and dizziness in the emergency department. Acta Otolaryngol 2014;134:140-5. [DOI] [PubMed] [Google Scholar]
- 12.Jung I, Kim JS. Approach to dizziness in the emergency department. Clin Exp Emerg Med 2015;2:75-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cappello M, di Blasi U, di Piazza L, Ducato G, Ferrara A, Franco S, et al. Dizziness and vertigo in a department of emergency medicine. Eur J Emerg Med 1995;2:201-11. [DOI] [PubMed] [Google Scholar]
- 14.Vanni S, Pecci R, Edlow JA, Nazerian P, Santimone R, Pepe G, et al. Differential Diagnosis of Vertigo in the Emergency Department: A Prospective Validation Study of the STANDING Algorithm. Front Neurol 2017;8:590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahsan SF, Syamal MN, Yaremchuk K, Peterson E, Seidman M. The costs and utility of imaging in evaluating dizzy patients in the emergency room. Laryngoscope 2013;123:2250-3. [DOI] [PubMed] [Google Scholar]
- 16.Ammar H, Govindu R, Fouda R, Zohdy W, Supsupin E. Dizziness in a community hospital: central neurological causes, clinical predictors, and diagnostic yield and cost of neuroimaging studies. J Community Hosp Intern Med Perspect 2017;7:73-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatr 2007;78:710-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bhattacharyya N, Baugh RF, Orvidas L, Barrs D, Bronston LJ, Cass S, et al. Clinical practice guideline: benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg 2008;139:S47-81. [DOI] [PubMed] [Google Scholar]
- 19.von Brevern M, Bertholon P, Brandt T, Fife T, Imai T, Nuti D, Newman-Toker D. Benign paroxysmal positional vertigo: Diagnostic criteria consensus document of the committee for the classification of vestibular disorders of the bárány societ. Acta Otorrinolaringol Esp 2017;68:349-60. [DOI] [PubMed] [Google Scholar]
- 20.Kerber KA, Burke JF, Skolarus LE, Meurer WJ, Callaghan BC, Brown DL, et al. Use of BPPV processes in emergency department dizziness presentations: a population-based study. Otolaryngol Head Neck Surg 2013;148:425-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kerber KA, Forman J, Damschroder L, Telian SA, Fagerlin A, Johnson P, et al. Barriers and facilitators to ED physician use of the test and treatment for BPPV. Neurol Clin Pract 2017;7:214-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lloyd M, Mackintosh A, Grant C, McManus F, Kelly AM, Karunajeewa H, et al. Evidence-based management of patients with vertigo, dizziness, and imbalance at an Australian metropolitan health service: an observational study of clinical practice. Physiother Theory Pract 2020;36:818-25. [DOI] [PubMed] [Google Scholar]
- 23.Newman-Toker DE, Cannon LM, Stofferahn ME, Rothman RE, Hsieh YH, Zee DS. Imprecision in patient reports of dizziness symptom quality: a cross-sectional study conducted in an acute care setting. Mayo Clin Proc 2007;82:1329-40. [DOI] [PubMed] [Google Scholar]
- 24.Karatas M. Central vertigo and dizziness: epidemiology, differential diagnosis, and common causes. Neurologist 2008;14:355-64. [DOI] [PubMed] [Google Scholar]


