Abstract
Introduction
During the 2018–2019 influenza season, vaccination coverage among U.S. children was 62.6%. The purpose of this study was to estimate the prevalence of influenza vaccinations among pediatric patients seen in U.S. health centers, and to explore potential disparities in vaccination coverage among subpopulations. Funded by the Health Resources and Services Administration (HRSA) within the U.S. Department of Health and Human Services, these health centers provide primary and preventive care to underserved and vulnerable individuals and families in order to reduce health disparities based on economic, geographic, or cultural barriers.
Methods
Cross-sectional data, analyzed in 2019, came from the most recent waves of the Health Center Patient Survey (2009, 2014). The sample consisted of children ages 2–17 years receiving care from HRSA-funded health centers. The outcome of interest was self- or parent-reported receipt of influenza vaccine in the past year. Multivariable logistic regression was used to estimate the adjusted prevalence rate ratios for the association between demographic characteristics (age, sex, race/ethnicity, poverty level, urban/rural residence, geographic region), health-related variables (receipt of well-child check-up, asthma diagnosis), and influenza vaccination.
Results
Influenza vaccination coverage among pediatric health center patients increased from 46.6% in 2009 to 67.8% in 2014. In the adjusted model for 2014, there were few statistically significant differences in vaccination coverage among subpopulation groups, however American Indian/Alaska Native children had 31% increased vaccination coverage compared with non-Hispanic White children (aPRR: 1.31, 95% CI: 1.02–1.60) and children living in the South had 26% decreased vaccination coverage compared with those living in the Northeast (aPRR: 0.74, 95% CI: 0.54–0.93).
Conclusions
Influenza vaccination coverage among pediatric health center patients in 2014 exceeded the national average (as of 2018–2019), and few differences were found among at-risk subpopulations. HRSA-funded health centers are well-positioned to further increase the vaccination rate among children living in underserved communities.
Keywords: Influenza, Vaccination coverage, U.S. health centers, Underserved populations, Safety net, Children
1. Introduction
Vaccinations, extolled as one of the greatest public health achievements of the 20th century, continue to be a critical tool for mitigating death and disease in the United States (U.S.) and globally. For a single-year birth cohort, it is estimated that routine childhood vaccination prevents nearly 20 million cases of disease in the U.S., including over 40,000 deaths [1]. Moreover, avoided morbidity and mortality due to vaccination is estimated to save $13.5 billion in direct costs and $68.8 billion in total societal costs over the cohort’s lifetime [2]. Despite the remarkable outcomes provided by recommended vaccines they remain underutilized among children, due to barriers to accessing vaccination services, vaccination exemptions, and parental vaccine hesitancy [3], [4], [5].
In the U.S. each fall, the Centers for Disease Control and Prevention and the American Academy of Pediatrics recommend seasonal influenza vaccination for everyone six months of age and older, excluding those with medical contraindications [6], [7]. And each year, public health departments and primary care providers work to implement this recommendation. Historically, underserved populations, such as those living below the federal poverty line, and those who are uninsured or underinsured, have lower seasonal influenza vaccination rates [8], [9], [10], leaving those individuals and their communities more susceptible to influenza and related complications. Young children are at particularly high risk for severe influenza complications [11], [12]. Estimates from the 2018–2019 influenza season based on the National Immunization Survey-Flu indicate that the childhood influenza vaccination rate was nearly 63%—an increase of almost 5 percentage points from the 2017–2018 influenza season [13]. While this marks a positive shift, the coverage rate remains below the national benchmark of 70% [14].
Health care providers caring for the underserved are uniquely positioned to help prevent seasonal influenza infections through vaccination and to increase community immunity in the areas they serve. Health centers funded by the Health Resources and Services Administration (HRSA) within the U.S. Department of Health and Human Services, under Section 330 of the U.S. Public Health Service Act [15] provide high quality, accessible, and affordable primary and preventative health care to underserved and vulnerable populations across the U.S. in order to reduce health disparities based on economic, geographic, or cultural barriers. In 2018, HRSA-funded health centers served over 28 million patients, including over 8.7 million children ages 0 through 17 years, which represents one in nine U.S. children [16], [17]. Health centers operate with a sliding scale fee structure for patients, based on their income level. With over 91% of patients living at or below 200% of the federal poverty guideline [16], the Health Center Program provides a model of low cost, high quality health care that can contribute to improving utilization of preventative health services including seasonal influenza vaccination [18]. Given the program’s reach among children within underserved communities, health centers are cornerstones in promoting public health in general and influenza community immunity in particular [19].
To date, there have been no studies examining influenza vaccine uptake among patients seen in HRSA-funded health centers. Only one previous study, published in 2003, has examined pediatric vaccinations in the context of health centers, however it focused on the childhood immunization schedule rather than seasonal influenza vaccinations. That study found few disparities in childhood immunizations, and the authors hypothesized that enabling services provided by health centers facilitated access to timely vaccinations [20]. In 2010, the Advisory Committee for Immunization Practices (ACIP) recommended universal seasonal influenza vaccinations among those six months of age and older [21], [22]. Thus, this study sought to examine the rates of pediatric influenza vaccinations among health center patients before and after the ACIP recommendation.
The current study contributes to the literature by examining, for the first time, the prevalence of influenza vaccine administration among children served by HRSA-funded health centers. The strengths of the study include the use of HRSA datasets which are nationally representative of U.S. individuals who receive primary and preventive care from health centers, as well as the analysis of several sociodemographic characteristics to explore potential disparities in influenza vaccine uptake across pediatric subpopulations in underserved communities. Based on previous studies which have documented minimal disparities in health care access and utilization among health centers [15], [23], [24], [25], we hypothesized that we would find few disparities in pediatric influenza vaccinations in these settings.
2. Methods
2.1. Data source and study sample
We conducted secondary analysis of data from the Health Center Patient Survey, a nationally representative survey of people who receive care from U.S. health centers funded by HRSA. The survey is conducted periodically (every 4–6 years) by HRSA’s Bureau of Primary Health Care and is designed to capture information on patient sociodemographic characteristics, health conditions, health behaviors, access to and utilization of health care services, and satisfaction with care. Survey questions are based on other established national health surveys, including the National Health Interview Survey, National Ambulatory Medical Care Survey, Medical Expenditure Panel Survey, and National Health and Nutrition Examination Survey.
Sample selection is based on a stratified three-stage random sampling design. First, health center organizations are sampled, stratified by funding stream, size, U.S. Census region, urban/rural location, and number of care delivery sites per health center organization. Then, up to three care delivery sites per health center organization are sampled. Finally, individual patients from each site are sampled. Patients are eligible for the survey if they had at least one medical visit to the health center site in the past year. Surveys are conducted through computer-assisted personal interviews by trained field interviewers. For children ages 12 and under, parents or other knowledgeable caregivers respond to the survey; children ages 13 and over respond to the survey themselves, after parental/caregiver assent is obtained.
The 2014 Health Center Patient Survey was most recently fielded survey, when a total of 7,002 patients were surveyed between October 2014 and April 2015. Among patients who were screened and determined to be eligible, 91% completed an interview. The previous fielding was the 2009 Health Center Patient Survey, which included a total of 4,562 patients surveyed between September and December 2009; in this fielding, 98% of patients who were screened and deemed eligible completed an interview. Institutional Review Board approval for the original data collections in both 2009 and 2014 was obtained from Research Triangle International, the organization that administered the survey on behalf of HRSA. For the current study, conducted in 2019, the analytic sample of pediatric health center patients included 1,093 children between the ages of 2 and 17 years from the 2014 survey, and 464 children from the 2009 survey.
2.2. Measures
We examined receipt of annual influenza vaccine, as assessed by parent- or self-reported responses to two questions. The first question asked about influenza vaccination injection: “During the past 12 months, {have you/has NAME} had a flu shot? A flu shot is usually given in the fall and protects against influenza for the flu season. The flu shot is injected in the arm. Do not include an influenza vaccine sprayed in the nose.” The second question asked about influenza vaccination nasal spray: “During the past 12 months, {have you/has NAME} had a flu vaccine sprayed in {your/his/her} [26] nose by a doctor or other health professional? This vaccine is usually given in the fall and protects against influenza for the flu season.” For this study, we combined responses to both questions to create a dichotomous outcome measure to capture the receipt of an annual influenza vaccine (yes vs. no).
Sociodemographic covariates of interest included patient age, sex, race/ethnicity, family poverty level, urban/rural residence, and U.S. Census region. We also included two health-related variables, specifically, receipt of a well-child check-up in the past 12 months and lifetime diagnosis of asthma (an indicator of a high-risk population).
2.3. Statistical analysis
We examined the rates of influenza vaccination among pediatric health center patients in 2009 versus 2014. We also stratified vaccination rates by age group (2–5 years, 6–11 years, 12–17 years) to determine whether rates declined with age, as is found in national trends [27]. We limited subsequent analyses to the 2014 sample of pediatric patients, the most recent year of health center data available, to assess potential disparities in receipt of influenza vaccines among this population after the ACIP issued its 2010 recommendation for universal vaccination. We first examined the distribution of sociodemographic and health characteristics for patients, and conducted bivariate analyses and chi-square tests of independence with design-based F statistics to assess the associations between receipt of influenza vaccine and each of the characteristics of interest. We set statistical significance at p < 0.05, and calculated 95% confidence intervals for each estimate. Finally, we conducted multiple logistic regression to examine the independent associations between each covariate of interest and receipt of an annual influenza vaccine. Results are presented as adjusted prevalence rate ratios (PRRs), which represent the likelihood that children with specific characteristics of interest received an annual influenza vaccine, relative to other children in meaningful reference groups while holding all other correlates constant. About 28% of the sample had missing income data, therefore we created a separate category for “missing income” in order to retain these observations. We conducted all analyses using STATA/SE, version 15.1, and employed weights based on the survey’s sampling design to produce estimates that adjusted for the complex sampling design and were representative of the underlying population.
3. Results
3.1. Receipt of annual influenza vaccine, 2009 vs. 2014
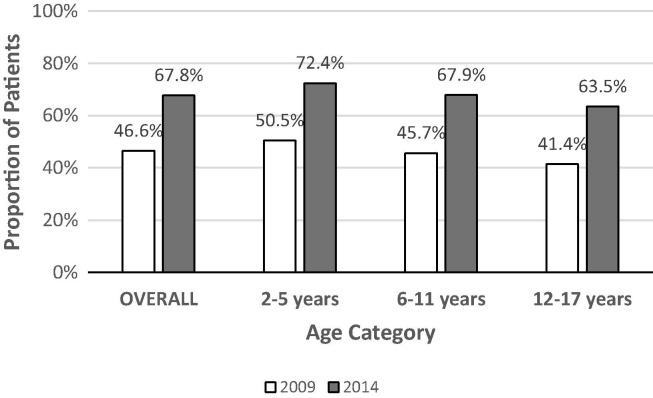
The overall rate of influenza vaccination among pediatric patients seen in HRSA-funded health center increased from 47% in 2009 to 68% in 2014, a 45% increase over 5 years (Fig. 1 ). Increases in vaccination coverage were seen across all three age groups. The largest relative increase occurred among youth 12 to 17 years, from 41% in 2009 to 64% in 2014, a 54% increase (23 percentage points). In both 2009 and 2014, there was an inverse dose–response relationship between vaccination and patient age, with the youngest age group (2–5 years) having the highest rates of vaccination and the oldest age group (12–17 years) having the lowest rates.
Fig. 1.
Receipt of Seasonal Influenza Vaccine among U.S. Pediatric Patients (2–17 years) Served by HRSA-Funded Health Centers, Overall and by Age, 2009 and 2014. Data Sources: 2009 and 2014 Health Center Patient Survey.
3.2. Characteristics of pediatric patients receiving care in HRSA-Funded Health Centers, 2014
In 2014, 29% of HRSA-funded health center pediatric patients in the analytic sample were between the ages of 2 and 5 years, and another 33% were between 12 and 17 years, with the remainder between 6 and 11 years (Table 1 ). There were slightly more male patients (55%) than female patients. The most common racial/ethnic group among pediatric patients was Hispanic (53%), followed by non-Hispanic White (22%) and non-Hispanic Black (18%). About 60% of the sample lived below the federal poverty level. Over 40% of pediatric patients lived in rural areas, and slightly more lived in the West (36%) and South (29%) compared with the Northeast (20%) and the Midwest (15%). Almost 80% of children had received a well-child check-up in the past year, and about 29% had a lifetime diagnosis of asthma.
Table 1.
Sociodemographic Characteristics of U.S. Pediatric Patients, ages 2–17 years, Served by HRSA-Funded Health Centers (N = 1,093).
| n | Weighted % | 95% CI | |
|---|---|---|---|
| Age | |||
| 2–5 years | 400 | 28.9 | 23.1–35.5 |
| 6–11 years | 425 | 38.3 | 31.8–45.2 |
| 12–17 years | 268 | 32.8 | 25.5–41.1 |
| Sex | |||
| Male | 550 | 54.7 | 48.0–61.2 |
| Female | 543 | 45.3 | 38.9–52.0 |
| Race/Ethnicity | |||
| White, non-Hispanic | 97 | 22.3 | 16.1–30.0 |
| Black, non-Hispanic | 171 | 17.6 | 11.8–25.5 |
| Hispanic | 669 | 52.6 | 43.6–61.4 |
| American Indian/Alaska Native | 101 | 1.2 | 0.6–2.1 |
| Other | 55 | 6.4 | 3.2–12.4 |
| Federal Poverty Level | |||
| ≥ 200% FPL | 67 | 10.3 | 6.0–17.2 |
| 101–199 FPL | 230 | 30.5 | 24.4–37.4 |
| ≤ 100% FPL | 584 | 59.2 | 51.3–66.7 |
| Missing | 212 | 28.4 | 20.8–37.5 |
| Urban/Rural Residence | |||
| Urban | 613 | 57.4 | 44.3–69.5 |
| Rural | 480 | 42.6 | 30.5–55.7 |
| Geographic Region | |||
| Northeast | 166 | 20.3 | 11.4–33.6 |
| South | 356 | 29.0 | 18.9–41.7 |
| Midwest | 108 | 14.8 | 7.1–28.2 |
| West | 463 | 36.0 | 24.6–49.3 |
| Well-Child Check-up, past year | |||
| Yes | 867 | 79.9 | 73.2–85.2 |
| No | 226 | 20.1 | 14.8–26.8 |
| Asthma | |||
| Yes | 276 | 28.6 | 23.5–34.4 |
| No | 816 | 71.4 | 65.6–76.5 |
Data Source: 2014 Health Center Patient Survey.
CI: confidence interval. FPL: federal poverty level.
3.3. Factors associated with receipt of annual influenza vaccine among pediatric patients in HRSA-Funded health Centers, 2014
In unadjusted analyses, only two characteristics were associated with receipt of annual influenza vaccination among health center pediatric patients in 2014 (Table 2 ). Specifically, a larger proportion of children living in urban settings received a influenza vaccine than those living in rural settings (74% vs. 59%, p = 0.0137). In addition, children living in the Northeast and the West had higher rates of influenza vaccination than those living in the South and the Midwest (range: 53%-81%, p = 0.0066). There were no statistically significant associations between influenza vaccination and child age, sex, race/ethnicity, federal poverty level, well-child check-up, and asthma diagnosis. After adjusting for all covariates simultaneously in the multiple logistic regression, the association between urban/rural residence and influenza vaccines was no longer statistically significant (Table 3 ). However, children living in the South had a 26% decreased prevalence of influenza vaccine receipt, compared with those living in the Northeast (aPRR = 0.74, 95% CI: 0.54–0.93). In addition, American Indian/Alaska Native children had a 31% increased prevalence of influenza vaccine receipt relative to non-Hispanic White children (aPRR = 1.31, 95% CI: 1.02–1.60).
Table 2.
Unadjusted Prevalence Rates for Receipt of Seasonal Influenza Vaccine among U.S. Pediatric Patients, ages 2–17 years, Served by HRSA-Funded Health Centers.
| Weighted % | 95% CI | P-Value | |
|---|---|---|---|
| OVERALL | 67.8 | 61.5–73.5 | … |
| Age | |||
| 2–5 years | 72.4 | 60.0–82.1 | 0.512 |
| 6–11 years | 67.9 | 57.3–77.0 | |
| 12–17 years | 63.5 | 53.1–72.9 | |
| Sex | |||
| Male | 65.2 | 56.9–72.8 | 0.378 |
| Female | 70.8 | 60.9–79.0 | |
| Race/Ethnicity | |||
| White, Non-Hispanic | 58.5 | 45.2–70.7 | 0.187 |
| Black, Non-Hispanic | 59.3 | 44.0–73.0 | |
| Hispanic | 73.6 | 64.8–80.8 | |
| American Indian/Alaska Native | 82.8 | 64.4–92.7 | |
| Other | 72.9 | 39.4–91.8 | |
| Federal Poverty Level | |||
| ≥ 200% FPL | 63.3 | 37.2–83.4 | 0.606 |
| 101–199 FPL | 66.9 | 55.8–76.5 | |
| ≤ 100% FPL | 72.2 | 61.6–80.8 | |
| Missing | 63.0 | 51.2–73.5 | |
| Urban/Rural Residence | |||
| Urban | 74.1 | 66.0–80.9 | 0.014 |
| Rural | 59.2 | 49.9–67.9 | |
| Geographic Region | |||
| Northeast | 81.0 | 70.4–88.5 | 0.007 |
| South | 52.6 | 41.7–63.3 | |
| Midwest | 63.7 | 41.3–81.4 | |
| West | 74.2 | 68.4–79.2 | |
| Well-Child Check-up, past year | |||
| Yes | 69.4 | 62.0–75.9 | 0.238 |
| No | 61.2 | 48.7–72.4 | |
| Asthma | |||
| Yes | 65.2 | 52.5–76.1 | 0.590 |
| No | 68.8 | 61.8–75.1 |
Data Source: 2014 Health Center Patient Survey.
Bold values is p < 0.05.
CI: confidence interval. FPL: federal poverty level.
Table 3.
Adjusted Associations for Receipt of Seasonal Influenza Vaccine among U.S. Pediatric Patients, ages 2–17 years, Served by HRSA-Funded Health Centers.
| aPRR | 95% CI | P-Value | |
|---|---|---|---|
| Age | |||
| 2–5 years | 1.00 | ||
| 6–11 years | 0.99 | 0.81–1.17 | 0.897 |
| 12–17 years | 0.91 | 0.56–1.26 | 0.632 |
| Sex | |||
| Male | 1.00 | ||
| Female | 1.12 | 0.94–1.30 | 0.175 |
| Race/Ethnicity | |||
| White, Non-Hispanic | 1.00 | ||
| Black, Non-Hispanic | 0.90 | 0.59–1.20 | 0.523 |
| Hispanic | 1.10 | 0.84–1.37 | 0.402 |
| American Indian/Alaska Native | 1.31 | 1.02–1.60 | 0.040 |
| Other | 1.04 | 0.53–1.54 | 0.890 |
| Federal Poverty Level | |||
| ≥ 200% FPL | 1.00 | ||
| 101–199 FPL | 1.11 | 0.71–1.51 | 0.555 |
| ≤ 100% FPL | 1.16 | 0.74–1.58 | 0.380 |
| Missing | 1.14 | 0.56–1.71 | 0.620 |
| Urban/Rural Residence | |||
| Urban | 1.00 | ||
| Rural | 0.84 | 0.68–1.00 | 0.062 |
| Geographic Region | |||
| Northeast | 1.00 | ||
| South | 0.74 | 0.54–0.93 | 0.021 |
| Midwest | 0.83 | 0.50–1.17 | 0.331 |
| West | 0.98 | 0.81–1.15 | 0.826 |
| Well-Child Check-up, past year | |||
| Yes | 1.00 | ||
| No | 0.88 | 0.71–1.04 | 0.138 |
| Asthma | |||
| Yes | 0.99 | 0.81–1.18 | 0.954 |
| No | 1.00 |
Data Source: 2014 Health Center Patient Survey.
Bold values is p < 0.05.
aPRR: adjusted prevalence rate ratio. CI: confidence interval. FPL: federal poverty level.
4. Discussion
Among U.S. children ages 2–17 years receiving care from HRSA-funded health centers, there was a 21 percentage point increase in annual influenza vaccinations between 2009 (prior to the 2009 ACIP recommendation) and 2014, from 47% to 68% of patients. The 2014 influenza vaccination rate among this traditionally underserved population exceeded the 2013–2014 rate seen among U.S. children nationally (59%) by almost 10 percentage points. The age-related pattern seen in health center pediatric patients, showing lower vaccination rates with increasing age, was similar to the pattern in the general U.S. population [28]. Several subpopulations of health center patients exceeded the national benchmark of 70% uptake, including young children (ages 2–5 years), American Indian/Alaska Native and Hispanic children, and those living under the federal poverty level, in urban locations, and in the Northeast and West. One possible explanation for the increased influenza vaccinations among these subgroups is that health centers may deliver childhood vaccines through the federal Vaccines for Children Program, which provides free or low-cost vaccines for uninsured, underinsured, and Medicaid-insured children, as well as American Indian/Alaska Native children [29]. Another potential explanation is that HRSA implemented new activities during this timeframe to promote continuous quality improvement among its grantees, including publicly disseminating clinical performance data and implementing a pay-for-performance program [30]. Additional studies are needed to assess potential differential impacts of these quality improvement efforts on specific subpopulations. Although these results demonstrate a vast improvement in influenza vaccinations among this population within a 5-year span, there is a continuing need to further increase vaccination rates. Plans-Rubió’s (2012) study of community immunity against influenza viruses suggests that 80% vaccination coverage is required in healthy persons (and 90% in high-risk persons) to establish a sufficient network of protection in the U.S [31].
Results of this study indicate that HRSA-funded health centers are effectively providing equitable access to seasonal influenza vaccination to a wide spectrum of medically underserved pediatric patients. Health centers have a long history of reducing health care disparities by providing access to primary and preventive care to medically underserved and vulnerable populations [15], [23], [24], [25]. The 2014 health center data on influenza vaccinations corroborated this pattern, revealing few disparities with the exception of statistically significant lower rates among pediatric patients in the South (53%, compared with 81% in the Northeast) and significantly higher rates among American Indian/Alaska Native patients (83%, compared with 59% among non-Hispanic White patients). Previous studies have identified several institutional factors which may contribute to health centers’ ability to provide equitable access to services across a broad range of clinical domains, such as cancer screening, chronic condition management, prenatal care, and well-visit check-ups. These institutional factors include the provision of supportive services (e.g., care coordination, health education, translation, transportation), early and widespread implementation of electronic health records, and recognition as patient-centered medical homes [26], [32], [33]. Strengthening access to and quality of primary care broadly through these efforts may translate to increased use of specific services including influenza vaccinations, and fewer missed opportunities for influenza vaccinations. Indeed, Yue and colleagues (2019) found that adult health center patients who used support services had a 16 percentage point higher likelihood of receiving an influenza vaccine compared with those who did not use support services [32]. Given the demonstrated and potential efficacy of these factors in improving health care provided by health centers, HRSA has invested hundreds of millions of dollars to accelerate and optimize the adoption of health information technology, as well as incentivize the adoption of the patient-centered medical home model of care through its Quality Improvement Awards [30]. While previous studies have found positive effects of these innovations on access to care, quality of care, and disparities [26], [32], [33], additional analyses may examine their potential impact specifically on pediatric influenza vaccine uptake.
Our finding of lower rates of pediatric influenza vaccination among health center patients in the South was consistent with patterns identified using the National Immunization Survey and the National Health Interview Survey [28], [34], [35], suggesting opportunities to geographically target interventions and resources to improve the uptake of influenza vaccines in this region. Results from this study can be leveraged to inform efforts by HRSA-funded Primary Care Associations and Health Center Controlled Networks that work with health centers in the South [36], [37]. Additional research is needed to better understand the underlying factors that lead to lower influenza vaccinations among children seen in health centers in the South.
Racial/ethnic disparities in childhood influenza vaccination are well established in the literature, although the findings are mixed. Studies of young children (under age 3) have found that White children have higher vaccination coverage than Black or Hispanic children [38], [39], while national estimates of all children up to age 17 show that White children have similar vaccination rates to Black children and lower rates than Hispanic children [27], [40]. In contrast, our study found no statistically significant differences between these three racial/ethnic groups among the population of pediatric patients served by HRSA-funded health centers. The lack of disparities found within these settings may be a reflection of the Health Center Program’s mission to provide culturally competent, patient-centered, comprehensive primary care regardless of individuals’ ability to pay, as well as supportive services that promote access to health care [41]. In particular, HRSA requires that health centers incorporate cultural competency activities to address the unique needs of the populations they serve. This includes arranging interpretation and translation services for patients with limited English-speaking ability, providing resources and training to staff on delivering culturally sensitive services and bridging cultural differences, and regularly conducting needs assessments to improve service delivery with a particular focus on patient population characteristics that impact health status or health care access/utilization (e.g., social factors, physical environment, cultural/ethnic factors, language needs, housing status). In addition, health centers are directed by governing boards that must be composed of a patient majority; at least 51% of board members must be patients at the health center and must reflect the population served in terms of demographic factors such as race/ethnicity and gender.
We also found that the 2014 influenza vaccination rate among American Indian/Alaska Native pediatric health center patients was notably higher than the national average for American Indian/Alaska Native children in 2013–2014 (83% vs. 66%) [27], [40]. Researchers using the National Health Interview Survey have also reported higher influenza vaccination coverage among American Indian/Alaska Native children compared with other racial/ethnic groups[35], which may reflect clinical recommendations to target vaccination efforts for this subpopulation [42].
Our results showed that about 43% of pediatric health center patients lived in rural areas, twice the proportion of children living in rural settings in the U.S. in general [43], [44]. Although rural pediatric patients were less likely to receive influenza vaccinations than urban patients in the unadjusted analysis, there were no differences based on urban/rural status in the adjusted analysis, indicating that health centers are successfully serving areas with lower access to care overall.
4.1. Limitations
There are study limitations worth mentioning. First, while the results are generalizable to the population of underserved pediatric patients seen in HRSA-funded health centers, they are not representative of the general U.S. child population. Although the findings apply only to a specific subgroup, they represent 8.7 million U.S. children ages 17 and under, a not insignificant number. Second, because the Health Center Patient Survey includes patients of all ages, the sample of pediatric patients is relatively limited, and the small sample sizes for certain subgroups may have limited our ability to detect statistically significant differences. Third, although influenza vaccines are recommended for infants starting at 6 months, it was not possible to examine vaccination among health center patients younger than 2 years because of how age was coded in the dataset; therefore we were unable to obtain estimates of influenza vaccination for this age group. In addition, two influenza vaccine doses are recommended for children 6 months through 8 years in their first vaccination season but the Health Center Patient Survey does not ask whether children received 1 or 2 doses or whether it was their first time receiving a vaccine, therefore it was not possible to distinguish between the proportion of children with full versus partial influenza vaccination coverage.
Another limitation is potential recall bias. Specifically, parents may not accurately remember details of their child’s influenza vaccinations, and children 13 years and over who respond for themselves on the survey may be less reliable in reporting their health care utilization in general and in particular may be less aware that they received an influenza vaccine. Under these circumstances, our study may underestimate the prevalence of annual influenza vaccination.
Additionally, the survey includes limited parental or household information, such as parents’ education level or health literacy, so it was not possible to assess the association between several potentially relevant family characteristics and pediatric patients’ influenza vaccine uptake. In particular, children ages 13 and over were not asked about their health insurance coverage, so we were unable to examine influenza vaccination rates based on insurance status. However, previous research has cited a positive correlation between state-level Medicaid reimbursement and influenza vaccination rates among poor children across three separate influenza seasons [45], which may be particularly relevant for improving vaccination rates among health center patients, given that nearly half are Medicaid or CHIP beneficiaries [16]. Similarly, the study did not examine the role of knowledge, attitudes, and practices toward vaccines among parents of pediatric health center patients, which might influence the decision to obtain influenza vaccinations. Recent literature illustrates that parental concerns about seasonal influenza vaccine exist, including beliefs that the vaccine causes influenza illness, the vaccine is unnecessary because influenza illness is mild, and the vaccine is not effective [46], [47], [48], [49]. Beyond concerns specific to influenza vaccine, more generalized concerns may influence decisions to vaccinate. Concerns over safety and vaccine ingredients, number of vaccines administered, mistrust of the mainstream medical system, and the belief that vaccination should be a personal choice persist, and are often shaped by a parent’s social sphere of influence [50], [51], [52], [53].
Finally, the Health Center Patient Survey was last conducted in 2014–2015, so the data are now several years old. However, examining the 2014 data is still informative in terms of comparing to national averages and providing a baseline for comparing pediatric influenza vaccine rates in the future. The next wave of the survey is planned to be conducted in summer/fall of 2020, which will provide valuable information to ascertain whether HRSA-funded health centers have continued to increase influenza vaccine uptake among their pediatric patients, and to examine any current disparities impacting subpopulations of interest. Furthermore, future research should use these anticipated data to examine how the COVID-19 pandemic may impact patients’ perceptions of vaccines and influence vaccine uptake. Additional research is needed to further explore patient, family, provider, and organizational factors that may influence influenza vaccination among children receiving care at HRSA-funded health centers.
5. Conclusions
Notwithstanding the limitations mentioned above, this study provides the first nationally representative estimates of influenza vaccination rates among pediatric patients receiving care from HRSA-funded health centers, both overall and for subpopulations based on demographic and health-related factors. Results reveal opportunities to increase pediatric influenza vaccination in health centers so that all subpopulations can attain and surpass the national benchmark of 70% coverage. Possible strategies to improve influenza vaccine coverage include partnering with state and regional Primary Care Associations, which are tasked with providing programmatic, clinical, and financial training and technical assistance to safety-net providers, to support health centers in developing immunization strategies tailored to their localized communities [36]. Additionally, health information technology can be used to better facilitate important vaccine conversations, including patient and provider reminders and prompts in electronic health record systems and patient portals [54], [55], [56]. Other potential vehicles for improvement include parent education, proactive appointment scheduling, and strong provider recommendations [48], [57]. Findings suggest that HRSA-funded health centers can serve as critical providers in engaging and serving diverse constituencies, reducing disparities in influenza vaccination, and increasing immunity among the nation’s most underserved communities.
6. Financial disclosure
The authors have no financial disclosures.
7. Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the official policies of the US Department of Health and Human Services or the Health Resources and Services Administration, nor does mention of the department or agency names imply endorsement by the US government.
CRediT authorship contribution statement
Lydie A. Lebrun-Harris: Conceptualization, Methodology, Software, Formal analysis, Writing - original draft, Supervision. Judith A. Mendel Van Alstyne: Conceptualization, Writing - original draft. Alek Sripipatana: Conceptualization, Methodology, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2020.07.021.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Orenstein W.A., Ahmed R. Simply put: Vaccination saves lives. PNAS. 2017;114(16):4031–4033. doi: 10.1073/pnas.1704507114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou F., Shefer A., Wenger J. Economic evaluation of the routine childhood immunization program in the United States, 2009. Pediatrics. 2014;133(4):577–585. doi: 10.1542/peds.2013-0698. [DOI] [PubMed] [Google Scholar]
- 3.Hill H.A., Elam-Evans L.D., Yankey D., Singleton J.A., Kang Y. Vaccination Coverage Among Children Aged 19–35 Months - United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67(40):1123–1128. doi: 10.15585/mmwr.mm6740a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mellerson J.L., Maxwell C.B., Knighton C.L., Kriss J.L., Seither R., Black C.L. Vaccination Coverage for Selected Vaccines and Exemption Rates Among Children in Kindergarten - United States, 2017–18 School Year. MMWR Morb Mortal Wkly Rep. 2018;67(40):1115–1122. doi: 10.15585/mmwr.mm6740a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy People 2020 Midcourse Review. 2014
- 6.Grohskopf L.A., Sokolow L.Z., Broder K.R., Walter E.B., Fry A.M., Jernigan D.B. MMWR Recommendations and reports : Morbidity and mortality weekly report Recommendations and reports. 2018. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices-United States, 2018–19 Influenza Season; pp. 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams WW, Lu PJ, O'Halloran A, et al. Surveillance of Vaccination Coverage among Adult Populations - United States, 2015. Morbidity and mortality weekly report Surveillance summaries (Washington, DC : 2002). 2017;66(11):1-28 [DOI] [PMC free article] [PubMed]
- 8.Jerant A., Fiscella K., Tancredi D.J., Franks P. Health insurance is associated with preventive care but not personal health behaviors. J American Board Family Medicine : JABFM. 2013;26(6):759–767. doi: 10.3122/jabfm.2013.06.130054. [DOI] [PubMed] [Google Scholar]
- 9.Simon A.E., Ahrens K.A., Akinbami L.J. Influenza Vaccination Among US Children With Asthma, 2005–2013. Academic Pediat. 2016;16(1):68–74. doi: 10.1016/j.acap.2015.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Srivastav A., Zhai Y., Santibanez T.A., Kahn K.E., Smith P.J., Singleton J.A. Influenza vaccination coverage of Vaccine for Children (VFC)-entitled versus privately insured children, United States, 2011–2013. Vaccine. 2015;33(27):3114–3121. doi: 10.1016/j.vaccine.2015.04.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention National Center for Immunization and Respiratory Diseases. Children and Influenza (Flu). https://www.cdc.gov/flu/highrisk/children.htm. Accessed August 7, 2019
- 12.Bourgeois F.T., Valim C., Wei J.C., McAdam A.J., Mandl K.D. Influenza and other respiratory virus-related emergency department visits among young children. Pediatrics. 2006;118(1):e1–e8. doi: 10.1542/peds.2005-2248. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention National Center for Immunization and Respiratory Diseases. National Press Conference Kicks Off 2019-2020 Flu Vaccination Campaign. 2019; https://www.cdc.gov/flu/spotlights/2018-2019/flu-vaccination-campaign.htm.
- 14.U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy People 2020. 2010; https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives. [PubMed]
- 15.Lebrun L.A., Shi L., Zhu J. Racial/ethnic differences in clinical quality performance among health centers. J Ambul Care Manage. 2013;36(1):24–34. doi: 10.1097/JAC.0b013e3182473523. [DOI] [PubMed] [Google Scholar]
- 16.Health Resources and Services Administration Bureau of Primary Health Care. 2018 Uniform Data System (UDS). 2019.
- 17.United States Census Bureau. Quick Facts United States 2010-2018; QuickFacts provides statistics for all states and counties, and for cities and towns with a population of 5,000 or more. Available at: https://www.census.gov/quickfacts/fact/table/US/AGE295218. Accessed Ocotber 7, 2019
- 18.Health Resources and Services Administration. Health Center Library 2019; https://bphc.hrsa.gov/datareporting/health-center-library. Accessed September 7, 2019.
- 19.Fine P.E. Herd immunity: history, theory, practice. Epidemiol Rev. 1993;15(2):265–302. doi: 10.1093/oxfordjournals.epirev.a036121. [DOI] [PubMed] [Google Scholar]
- 20.Schempf A.H., Politzer R.M., Wulu J. Immunization coverage of vulnerable children: a comparison of health center and national rates. Med Care Res Rev MCRR. 2003;60(1):85–100. doi: 10.1177/1077558702250246. [DOI] [PubMed] [Google Scholar]
- 21.Fiore AE, Uyeki TM, Broder K, et al. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Recommendations and reports : Morbidity and mortality weekly report Recommendations and reports. 2010;59(Rr-8):1-62. [PubMed]
- 22.Immunization Action Coalition. Vaccine Timeline: Historic Dates and Events Related to Vaccines and Immunization. http://www.immunize.org/timeline/.
- 23.Shi L., Lebrun-Harris L.A., Daly C.A. Reducing disparities in access to primary care and patient satisfaction with care: the role of health centers. J Health Care Poor Underserved. 2013;24(1):56–66. doi: 10.1353/hpu.2013.0022. [DOI] [PubMed] [Google Scholar]
- 24.Jones E., Shi L., Hayashi A.S., Sharma R., Daly C., Ngo-Metzger Q. Access to oral health care: the role of federally qualified health centers in addressing disparities and expanding access. Am J Public Health. 2013;103(3):488–493. doi: 10.2105/AJPH.2012.300846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jones E., Lebrun-Harris L.A., Sripipatana A., Ngo-Metzger Q. Access to mental health services among patients at health centers and factors associated with unmet needs. J Health Care Poor Underserved. 2014;25(1):425–436. doi: 10.1353/hpu.2014.0056. [DOI] [PubMed] [Google Scholar]
- 26.Hu R., Shi L., Sripipatana A. The Association of Patient-centered Medical Home Designation With Quality of Care of HRSA-funded Health Centers: A Longitudinal Analysis of 2012–2015. Med Care. 2018;56(2):130–138. doi: 10.1097/MLR.0000000000000862. [DOI] [PubMed] [Google Scholar]
- 27.CDC. Flu Vaccination Coverage, United States, 2013–14 Influenza Season. Flu Vax View 2014; https://www.cdc.gov/flu/fluvaxview/coverage-1314estimates.htm#by-race-children. . Accessed April 6, 2020.
- 28.CDC. Estimates of Flu Vaccination Coverage among Children — United States, 2017–18 Flu Season. Flu Vax View 2018. Accessed September 19, 2019. https://www.cdc.gov/flu/fluvaxview/coverage-1718estimates-children.htm.
- 29.CDC. Vaccines for Children Program (VFC). https://www.cdc.gov/vaccines/programs/vfc/about/index.html.
- 30.Health Resources and Services Administration Bureau of Primary Health Care. Quality Improvement Awards (QIA). 2019. Accessed April 27, 2020. https://bphc.hrsa.gov/program-opportunities/quality.
- 31.Plans-Rubio P. The vaccination coverage required to establish herd immunity against influenza viruses. Prev Med. 2012;55(1):72–77. doi: 10.1016/j.ypmed.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 32.Yue D., Pourat N., Chen X. Enabling Services Improve Access To Care, Preventive Services, And Satisfaction Among Health Center Patients. Health Aff (Millwood). 2019;38(9):1468–1474. doi: 10.1377/hlthaff.2018.05228. [DOI] [PubMed] [Google Scholar]
- 33.Chuang E., Pourat N., Chen X. Organizational Factors Associated with Disparities in Cervical and Colorectal Cancer Screening Rates in Community Health Centers. J Health Care Poor Underserved. 2019;30(1):161–181. doi: 10.1353/hpu.2019.0014. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention National Center for Immunization and Respiratory Diseases. Early-Season Flu Vaccination Coverage–United States, November 2018. Flu Vax View 2018; https://www.cdc.gov/flu/fluvaxview/nifs-estimates-nov2018.htm.
- 35.Tian C., Wang H., Wang W., Luo X. Influenza vaccination coverage among US children from 2004/2005 to 2015/2016. J Public Health (Oxford, England) 2019;41(1):e62–e69. doi: 10.1093/pubmed/fdy081. [DOI] [PubMed] [Google Scholar]
- 36.Health Resources and Services Administration Bureau of Primary Health Care. Primary Care Associations. 2019. Accessed April 27, 2020. https://bphc.hrsa.gov/qualityimprovement/strategicpartnerships/ncapca/associations.html
- 37.Health Resources and Services Administration Bureau of Primary Health Care. Health Center Controlled Networks. 2018. Accessed April 27, 2020. https://bphc.hrsa.gov/qualityimprovement/strategicpartnerships/hccn.html.
- 38.Anandappa M., Adjei Boakye E., Li W., Zeng W., Rebmann T., Chang J.J. Racial disparities in vaccination for seasonal influenza in early childhood. Public Health. 2018;158:1–8. doi: 10.1016/j.puhe.2018.01.030. [DOI] [PubMed] [Google Scholar]
- 39.Santibanez T.A., Grohskopf L.A., Zhai Y., Kahn K.E. Complete Influenza Vaccination Trends for Children Six to Twenty-Three Months. Pediatrics. 2016;137(3):e20153280. doi: 10.1542/peds.2015-3280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.CDC. Flu Vaccination Coverage, United States, 2018–19 Influenza Season. Flu Vax View 2019;. Accessed October 7, 2019. https://www.cdc.gov/flu/fluvaxview/coverage-1819estimates.htm.
- 41.Health Resources and Services Administration Bureau of Primary Health Care. What is a Health Center? . https://bphc.hrsa.gov/about/what-is-a-health-center/index.html. Accessed April 6, 2020.
- 42.American Academy of Pediatrics Committee on Infectious Diseases. Recommendations for Prevention and Control of Influenza in Children, 2018-2019. Pediatrics. 2018;142(4) [DOI] [PubMed]
- 43.New Census Data Show Differences Between Urban and Rural Populations [press release]. U.S. Census Bureau, December 08, 2016 2016.
- 44.Number of children Key facts about the number of children 2019. Accessed November 25, 2019. https://www.childtrends.org/indicators/number-of-children.
- 45.Yoo B.K. How to improve influenza vaccination rates in the U.S. J Prevent Med Public Health = Yebang Uihakhoe chi. 2011;44(4):141–148. doi: 10.3961/jpmph.2011.44.4.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fogel B.N., Hicks S.D. “Flu-Floppers”: Factors Influencing Families' Fickle Flu Vaccination Patterns. Clin Pediatr (Phila). 2020;59(4–5):352–359. doi: 10.1177/0009922819901002. [DOI] [PubMed] [Google Scholar]
- 47.Nekrasova E., Stockwell M.S., Localio R. Vaccine hesitancy and influenza beliefs among parents of children requiring a second dose of influenza vaccine in a season: An American Academy of Pediatrics (AAP) Pediatric Research in Office Settings (PROS) study. Hum Vaccin Immunother. 2020:1–8. doi: 10.1080/21645515.2019.1707006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bauer K.E., Agruss J.C., Mayefsky J.H. Partnering with parents to remove barriers and improve influenza immunization rates for young children. J Am Assoc Nurse Pract. 2020 doi: 10.1097/JXX.0000000000000381. [DOI] [PubMed] [Google Scholar]
- 49.Goss M.D., Temte J.L., Barlow S. An assessment of parental knowledge, attitudes, and beliefs regarding influenza vaccination. Vaccine. 2020;38(6):1565–1571. doi: 10.1016/j.vaccine.2019.11.040. [DOI] [PubMed] [Google Scholar]
- 50.Mendel-Van Alstyne J.A., Nowak G.J., Aikin A.L. What is 'confidence' and what could affect it?: A qualitative study of mothers who are hesitant about vaccines. Vaccine. 2018;36(44):6464–6472. doi: 10.1016/j.vaccine.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 51.Hospital CSMCs should be rewritten as: C.S. Mott Children's Hospital. National Poll on Children's Health. Mott Poll Report: Do Parents Have Selective Hearing about Flu Vaccine for Children? 2018. Accessed April 14, 2020. https://mottpoll.org/reports/do-parents-have-selective-hearing-about-flu-vaccine-children.
- 52.Geoghegan S., O'Callaghan K.P., Offit P.A. Vaccine Safety: Myths and Misinformation. Front Microbiol. 2020;11:372. doi: 10.3389/fmicb.2020.00372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shui I., Kennedy A., Wooten K., Schwartz B., Gust D. Factors influencing African-American mothers' concerns about immunization safety: a summary of focus group findings. J Natl Med Assoc. 2005;97(5):657–666. [PMC free article] [PubMed] [Google Scholar]
- 54.Kahn K.E., Santibanez T.A., Zhai Y., Bridges C.B. Association between patient reminders and influenza vaccination status among children. Vaccine. 2018;36(52):8110–8118. doi: 10.1016/j.vaccine.2018.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jones Cooper S.N., Walton-Moss B. Using reminder/recall systems to improve influenza immunization rates in children with asthma. J Pediatr Health Care. 2013;27(5):327–333. doi: 10.1016/j.pedhc.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 56.Dombkowski K.J., Cowan A.E., Reeves S.L., Foley M.R., Dempsey A.F. The impacts of email reminder/recall on adolescent influenza vaccination. Vaccine. 2017;35(23):3089–3095. doi: 10.1016/j.vaccine.2017.04.033. [DOI] [PubMed] [Google Scholar]
- 57.Kahn K.E., Santibanez T.A., Zhai Y., Bridges C.B. Association between provider recommendation and influenza vaccination status among children. Vaccine. 2018;36(24):3486–3497. doi: 10.1016/j.vaccine.2018.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.