Abstract
Purpose
Multiple studies suggest response to mental health treatment is worse for people of lower socioeconomic status, a group who also express more mental illness stigma. Worse response to treatment may lead to greater therapeutic pessimism, an important component of stigma. However, familiarity with mental illness is associated with lower levels of stigma. This study therefore examines whether, among the general public, socioeconomic status moderates the relationships between familiarity and stigma related outcomes: knowledge; attitudes; and desire for social distance.
Methods
We carried out secondary analysis of data from the Attitudes to Mental Illness survey, collected annually from different general population samples from 2009-17, and every two years from 2017-19. Three separate multiple linear regression models examined factors associated with each outcome, with interaction tests between socioeconomic status and familiarity. Stigma related knowledge was measured using the Mental Health Knowledge Schedule (MAKS), which includes items on treatment effectiveness and recovery, thus addressing aspects of therapeutic pessimism. Attitudes were measured using the Community Attitudes towards the Mentally Ill Scale; and desire for social distance using the Reported and Intended Behaviour scale.
Results
In lower socioeconomic groups, personal experience was more frequent, while familiarity with someone else was less frequent. Interaction tests were significant for stigma related knowledge (p<0.0001) and desire for social distance (p=0.0118), but not for attitudes (p=0.057). The direction of the interaction differed between knowledge and the other outcomes. In lower socioeconomic groups the positive effect of familiarity on knowledge was weaker, as hypothesised, but for attitudes and desire for social distance, its effect was stronger.
Conclusions
Our results support the promotion of familiarity through encouraging discussion of mental health problems within social networks. However, lower stigma related knowledge among people with personal experience in lower socioeconomic groups suggests different responses to mental illness among these groups are needed.
Keywords: Familiarity, Mental health, Socioeconomic status, Stigma, Time to change, Anti-stigma programme
Highlights
-
•
Familiarity with mental illness is associated with lower levels of stigma.
-
•
Different experiences of familiarity may lead to moderation by socioeconomic group.
-
•
The effect of familiarity on knowledge is weaker in lower socioeconomic groups.
-
•
The results suggest more therapeutic pessimism in lower socioeconomic groups.
1. Introduction
Stigma and discrimination against people with mental illness have substantial impact on public health in England, contributing to inequalities (Hatzenbuehler et al., 2013) including: poor access to mental and physical healthcare (Mai et al., 2011); reduced life expectancy (Laursen et al., 2007); exclusion from higher education and employment (Unit, 2004); increased risk of contact with criminal justice systems; victimisation (Clement et al., 2011); poverty and homelessness.
A number of surveys (Bhavsar et al., 2014; Cechnicki et al., 2011; Corrigan & Watson, 2007; Hansson et al., 2016; Robinson & Henderson, 2018, pp. 1–10; Wang et al., 2007) have found that people of lower socioeconomic status express more stigmatising views. This may then exacerbate the experience of mental illness for people in these groups, who also have a relatively higher prevalence of mental ill health (McManus et al., 2016). In line with this finding, England’s Time to Change anti-stigma programme shifted the target group of its social marketing campaign in 2016, from middle socioeconomic status groups, as defined using the Market Research Association classification based on occupation, to low-to middle socioeconomic groups (González-Sanguino et al., 2019). The original social marketing campaign was launched in 2009 and has been delivered through bursts of mass media and social media activity lasting several weeks, usually twice a year. The initial campaign focussed on awareness raising about stigma and ‘mythbusting’ to challenge stereotypes and improve knowledge, for example about the prevalence of mental health problems. This was followed in 2010 by awareness raising about prejudicial attitudes and discriminatory behaviour; since 2011 the campaign has focussed on the importance of supportive behaviour towards people with mental health problems, for example as friends, relatives, or colleagues.
The higher prevalence of mental illness in lower socioeconomic groups appears at odds with the higher levels of stigma in these groups, given the consistent finding that familiarity with someone with a mental illness, either oneself or someone else, is strongly related to lower levels of stigma. The association in question; between both personal experience and experience via a relationship such as a friend, family member, or colleague, and more positive stigma related outcomes, including stigma related knowledge, attitudes and desire for social distance to mental illness, has been found in surveys of the general public (Evans-Lacko, S., C. Henderson, and G. Thornicroft, 2013a,Evans-Lacko, S., et al. 2013b; Henderson et al., 2016, 2020; Robinson & Henderson, 2018, pp. 1–10). Further, providing some level of familiarity through a contact intervention, structured according to the evidence base on facilitators of intergroup contact (Al Ramiah & Hewstone, 2013), can result in stigma reduction (Mehta et al., 2015).
However, in the absence of such facilitators (including equal status, acquaintanceship, collaboration, and information to reduce stereotypes) prejudice may be unaffected or worsen following contact (Al Ramiah & Hewstone, 2013). Further, research in some groups with high levels of contact such as mental health professionals suggests that compared to the general population, desire for social distance is as high (Lauber et al., 2004) and therapeutic pessimism is higher (Jorm et al., 1999). These findings suggest that factors which cause variations in the experience of contact and familiarity may moderate their impact on stigma outcomes.
While familiarity is likely to lead to better knowledge of mental illness, it may also lead views that are biased by the individual’s experience. Given the importance of therapeutic pessimism as a contributor to stigma (Henderson et al., 2014; Knaak et al., 2017), it seems likely that within the general public factors that affect the course of mental illnesses and their responsiveness to treatment may moderate the effect of familiarity on stigma outcomes. Familiarity may have a less positive impact on outcomes when it involves one or more people with less treatment responsive illnesses.
A number of studies suggest response to treatment varies by socioeconomic status. For example, Cohen et al reported that residents of middle- and high-income census tracts were more likely to respond to treatment of late-life depression and less likely to report suicidal ideation than residents of low income census tracts (Cohen et al., 2008). Jakubovski et al also found that other indicators of low socioeconomic status such as low income, education and unemployment were most discriminative in predicting a poor response to treatment of major depressive disorder (Jakubovski & Bloch, 2014). Many other studies also support this association (Ronalds et al., 2018), including a meta-analysis by Finegan et al who found seventeen studies that measured at least one indicator of socioeconomic status and its relationship with psychological therapy outcomes, and concluded that there is some evidence to indicate that socioeconomic deprivation is associated with poorer treatment outcomes (Finegan et al., 2018). Thus the experience of familiarity may vary by socioeconomic status, such that people in lower income groups have contact with people who are experiencing more severe symptoms. This may contribute to greater therapeutic pessimism; more frequent endorsement of stereotypes; and greater desire for social distance.
Therefore, differences in the nature of the experience of familiarity by socioeconomic status may lead to its moderation of the association between familiarity and stigma outcomes. However, this may not apply equally across all stigma outcomes; variable experiences of responsiveness to treatment may influence responses to stigma related knowledge questions (Evans-Lacko et al., 2010) more than they influence attitudes or desire for social distance. Prominent stigma theories distinguish these aspects of stigma for example as steps in the process of stigmatisation (Link & Phelan, 2001). Thus, in different socioeconomic contexts, familiarity and the lack thereof may have differential effects on each of whether and how someone with a mental health problem is labelled and what stereotype is attached to that label; what affective reactions and how much separation then result; and how much status loss ensues.
To begin to explore this question this study uses secondary data analysis to examine whether and how socioeconomic status moderates the relationship between familiarity and the stigma outcomes: mental health related knowledge; mental health related attitudes; and desire for social distance with people with mental illness among the general public. We hypothesise that familiarity may not have as positive an effect on stigma outcomes among lower socioeconomic groups.
2. Methods
2.1. Data source
The Attitudes to Mental Illness survey has been carried out by the agency Kantar TNS annually from 2008-17 and every two years from 2017-2019 as a part of the evaluation of England’s Time to Change anti-stigma programme. In 2009, the outcome measures for stigma related knowledge and desire for social distance were added to the pre-existing survey of attitudes. There are approximately 1700 respondents surveyed each year. The survey uses a quota sampling frame to ensure the survey sample is nationally representative of adult residents aged 16 or over and living in private households in England. Census small area statistics and the Postcode Address File define sample points that are randomly selected and stratified by Government Office Region and social status. One respondent per sampled household is selected based on the quota requirements. All survey interviews are carried out in respondents’ homes by fully trained personnel. Sampling errors were calculated on an assumption of a simple random sampling method. Additional information on the survey methods can be found in the Attitudes to Mental Illness 2014 Research Report (TNS BMRB, 2015).
2.2. Measures
2.2.1. Mental health related knowledge
Mental health related knowledge was measured by the Mental Health Knowledge Schedule (MAKS) (Evans-Lacko et al., 2010). The MAKS comprises two parts, Part A which includes six items covering stigma-related mental health knowledge areas: help seeking, recognition, support, employment, treatment and recovery; and Part B which includes six items that inquire about classification of various conditions as mental illnesses. The standardised total score of stigma-related knowledge (Part A) was used; where a higher standardised MAKS score indicates greater knowledge. Overall test-retest reliability of the MAKS is 0.71 (Lin’s concordance statistic) and the overall internal consistency among items is 0.65 (Cronbach’s alpha). These were calculated using a previous dataset (Evans-Lacko et al., 2010).
2.2.2. Mental health related attitudes
Public attitudes towards mental health was measured using a shortened version of the Community Attitudes towards the Mentally Ill scale (CAMI) (Taylor & Dear, 1981) developed for the first wave of the survey conducted in 1993. The questionnaire includes 26 of the original 40 items of the CAMI and an added item on employment-related attitudes. Items cover attitudes about social exclusion, benevolence, tolerance and support for community mental health care and were rated from 1 (strong disagreement) to 5 (strong agreement). The standardised total score of the CAMI was used and a higher score indicates less stigmatising attitudes. The overall internal consistency of the CAMI is 0.87 (Cronbach’s alpha) (Evans-Lacko, S., C. Henderson, and G. Thornicroft, 2013a).
2.2.3. Desire for social distance
Desire for social distance was measured using the four-item intended behaviour (IB) subscale of the Reported and Intended Behaviour Scale (RIBS) (Evans-Lacko et al., 2011). This assesses the level of desired future contact with people with mental health problems, in terms of four different contexts: living with, working with, living nearby and continuing a relationship with someone. These were derived from the Star Social Distance Scale (Star, 1952). RIBS IB is scored so that a higher score indicates more positive behaviour: less desire for social distance, and the total score was standardised. The overall test-retest reliability of total RIBS score is 0.75 (Lin’s concordance statistic) and the overall internal consistency among items is 0.85 (Cronbach’s alpha) (Evans-Lacko et al., 2011).
2.2.4. Socioeconomic status
Socioeconomic status (SES) of the respondent was categorised into one of four categories using the Market Research Society’s classification system (AB, C1, C2 and DE). Classification was based on the occupation of the household’s chief income earner: AB represents professional/managerial occupations, C1 represents other non-manual occupations, C2 represents skilled manual occupations and DE represents semi-/unskilled manual occupations or people dependent on state benefits.
2.2.5. Familiarity with mental health problems
Familiarity was measured using the following question: Who is the person closest to you who has or has had some kind of mental illness? Potential responses included: immediate family, partner, other family, friend, acquaintance, work colleague, self, other or no-one known. These responses were then categorised into three groups (self, other and none).
2.3. Statistical analysis
Descriptive statistics for participant demographics were reported for all survey years combined (2008–2019). They were also reported by socioeconomic status to illustrate potential differences with other characteristics, particularly familiarity. All analyses were weighted by gender, age and ethnicity to reflect population characteristics in England. Survey sampling weights were also applied in all analyses so that respondents reflected a nationally representative sample in terms of sociodemographic characteristics with each region of England. These are taken directly from the UK Government’s Office for National Statistics.
Three separate multiple linear regression models examined the relationship of familiarity with mental health problems (Self, Other and None) with: (i) public knowledge (MAKS); (ii) public attitudes (CAMI); and (iii) public desire for social distance (RIBS IB) from people with mental health problems. All models used the standardised scores of the measures as the dependent variables and therefore results were interpreted in standard deviation units.
All the models included a fixed effect for year using a categorical dummy variable. Covariates were included to control for differences in participant demographics as previous survey data have shown these to be associated with each stigma outcome (Evans-Lacko, S., C. Henderson, and G. Thornicroft, 2013a Henderson et al., 2016, 2020; Robinson & Henderson, 2018, pp. 1–10): gender (Female and Male), age category (16–24, 25–44, 45–64 and 65+), ethnicity (Asian, Black, Other and White), region (North East, North West, Yorkshire and the Humber, East Midlands, West Midlands, East of England, South East, South West and London) and socioeconomic status (AB, C1, C2 and DE). For each categorical variable listed above, the final category was used as the reference group. Interactions between socioeconomic status and familiarity were used to test our hypothesis that socioeconomic status will moderate the relationship between familiarity and each stigma outcome. The interaction term was added to each initial model and tested for statistical significance using a Wald test. A significance level of 0.05 was used. All analyses were carried out using Stata version 15.1.
3. Results
3.1. Survey sample characteristics
Table 1 provides the demographics of the 19,104 participants combined from all survey years (2008–2019) and demonstrates noticeable differences in the sample characteristics by socioeconomic status. The proportion of participants with familiarity through personal experience increases as socioeconomic status decreases from AB to DE. However, the proportion of participants with ‘other’ familiarity decreases as socioeconomic status decreases.
Table 1.
Participant demographics for all survey years combined and by socioeconomic status, un-weighted frequency and weighted percent (2008-2019)
| AB (n=3410) | C1 (n=4965) | C2 (n=3901) | DE (n=6828) | Total (n=19104) | |
|---|---|---|---|---|---|
| Gender, n (%) | |||||
| Female | 1701 (49.0) | 2652 (52.3) | 1858 (46.3) | 3955 (55.4) | 10166 (51.3) |
| Male | 1709 (51.0) | 2313 (47.7) | 2043 (53.7) | 2873 (44.6) | 8938 (48.7) |
| Age, mean (SD) | 48.0 (18.2) | 42.7 (19.4) | 45.0 (18.9) | 48.9 (20.5) | 46.0 (19.7) |
| Age group, n (%) | |||||
| 16-24 | 268 (8.5) | 899 (18.5) | 524 (14.6) | 935 (14.5) | 2626 (14.5) |
| 25-44 | 1043 (37.4) | 1658 (39.5) | 1360 (36.4) | 2018 (30.3) | 6079 (35.8) |
| 45-64 | 1169 (36.1) | 1375 (28.5) | 1162 (33.5) | 1844 (27.9) | 5550 (30.9) |
| 65+ | 930 (18.0) | 1033 (13.5) | 855 (15.5) | 2031 (27.3) | 4849 (18.8) |
| Ethnicity, n (%) | |||||
| Asian | 179 (6.0) | 365 (8.1) | 256 (6.5) | 457 (6.7) | 1257 (7.0) |
| Black | 74 (2.4) | 214 (4.7) | 166 (4.3) | 361 (5.2) | 815 (4.3) |
| Other | 62 (2.2) | 151 (3.2) | 70 (1.8) | 110 (1.6) | 393 (2.2) |
| White | 3083 (89.4) | 4207 (84.0) | 3389 (87.4) | 5839 (86.5) | 16518 (86.5) |
| Socio-economic Status, n (%) | |||||
| AB | 3410 (20.6) | ||||
| C1 | 4965 (30.8) | ||||
| C2 | 3901 (20.2) | ||||
| DE | 6828 (28.4) | ||||
| Familiarity with mental health, n (%) | |||||
| Self | 183 (5.5) | 262 (5.5) | 223 (6.1) | 591 (9.2) | 1259 (6.7) |
| Other | 2223 (66.5) | 2793 (57.7) | 2018 (53.2) | 3048 (46.0) | 10082 (55.3) |
| None | 946 (28.0) | 1793 (36.8) | 1588 (40.7) | 2985 (44.8) | 7312 (38.0) |
| Campaign awareness (since 2012), n (%) | |||||
| Yes | 646 (30.6) | 900 (29.1) | 693 (29.2) | 1039 (24.5) | 3278 (28.1) |
| No | 1548 (69.4) | 2264 (70.9) | 1774 (70.8) | 3300 (75.5) | 8886 (71.9) |
| Region, n (%) | |||||
| North East | 166 (4.5) | 215 (4.2) | 203 (5.7) | 345 (5.6) | 929 (5.0) |
| North West | 433 (12.3) | 648 (12.1) | 541 (15.1) | 1036 (17.1) | 2658 (14.2) |
| Yorkshire & the Humber | 369 (9.7) | 428 (8.1) | 405 (11.0) | 673 (11.2) | 1875 (9.9) |
| East Midlands | 238 (6.7) | 435 (8.5) | 328 (8.9) | 622 (9.0) | 1623 (8.3) |
| West Midlands | 330 (9.1) | 475 (9.3) | 411 (11.1) | 814 (11.7) | 2030 (10.3) |
| East of England | 435 (12.0) | 621 (11.7) | 401 (11.2) | 657 (9.2) | 2114 (10.9) |
| London | 438 (14.6) | 777 (17.2) | 553 (12.7) | 1066 (14.6) | 2834 (15.0) |
| South East | 658 (20.5) | 880 (18.6) | 662 (15.2) | 968 (13.0) | 3168 (16.7) |
| South West | 343 (10.6) | 486 (10.3) | 397 (9.1) | 647 (8.6) | 1873 (9.7) |
3.2. Relationships between stigma related outcome measures and familiarity within categories of socioeconomic status
3.2.1. Mental health-related public knowledge
Table 2 presents the results of the initial model to examine the relationship between mental health-related knowledge and familiarity. Results shows mental health-related knowledge is associated with familiarity (p<0.001) and higher socioeconomic group (p<0.001).
Table 2.
Regression analyses of predictors of mental health related knowledge (MAKS), attitudes (CAMI) and behaviour (RIBS IB) among the general public
| Knowledge: Standardised MAKS score (n=16943) |
Attitudes: Standardised CAMI score (n=18551) |
Intended behaviour: Standardised RIBS IB score (n=16943) |
||||
|---|---|---|---|---|---|---|
| Predictors | Standardised effect size (95% CI) | P-value | Standardised effect size (95% CI) | P-value | Standardised effect size (95% CI) | P-value |
| Year | ||||||
| 2019 | *0.25 (0.19, 0.32) | <0.001 | *0.32 (0.26, 0.39) | <0.001 | *0.29 (0.23, 0.36) | <0.001 |
| 2017 | *0.17 (0.10, 0.23) | <0.001 | *0.25 (0.18, 0.31) | <0.001 | *0.29 (0.23, 0.36) | <0.001 |
| 2016 | *0.16 (0.09, 0.22) | <0.001 | *0.25 (0.18, 0.32) | <0.001 | *0.21 (0.14, 0.27) | <0.001 |
| 2015 | *0.16 (0.09, 0.23) | <0.001 | *0.20 (0.13, 0.26) | <0.001 | *0.17 (0.11, 0.23) | <0.001 |
| 2014 | *0.12 (0.05, 0.19) | <0.001 | *0.18 (0.11, 0.24) | <0.001 | *0.19 (0.12, 0.25) | <0.001 |
| 2013 | 0.03 (-0.04, 0.09) | 0.415 | *0.08 (0.02, 0.15) | 0.013 | *0.11 (0.05, 0.18) | 0.001 |
| 2012 | 0.03 (-0.03, 0.10) | 0.348 | 0.05 (-0.02, 0.11) | 0.137 | *0.07 (0.01, 0.14) | 0.026 |
| 2011 | -0.01 (-0.08, 0.05) | 0.700 | 0.01 (-0.05, 0.08) | 0.651 | 0.03 (-0.04, 0.09) | 0.399 |
| 2010 | -0.03 (-0.09, 0.04) | 0.445 | *0.07 (0.002, 0.13) | 0.041 | *0.09 (0.03, 0.16) | 0.004 |
| 2009 (ref) | -- | -- | -0.003 (-0.07, 0.06) | 0.917 | -- | -- |
| 2008 (CAMI ref) | -- | -- | ||||
| Gender | ||||||
| Female | *0.15 (0.12, 0.18) | <0.001 | *0.16 (0.13, 0.19) | <0.001 | -0.01 (-0.04, 0.01) | 0.296 |
| Male (ref) | -- | -- | -- | -- | -- | -- |
| Age | ||||||
| 16-24 | *0.06 (0.01, 0.11) | 0.026 | 0.02 (-0.02, 0.07) | 0.323 | *0.52 (0.47, 0.57) | <0.001 |
| 25-44 | *0.17 (0.13, 0.21) | <0.001 | *0.13 (0.09, 0.16) | <0.001 | *0.45 (0.41, 0.49) | <0.001 |
| 45-64 | *0.25 (0.21, 0.29) | <0.001 | *0.22 (0.19, 0.26) | <0.001 | *0.40 (0.36, 0.44) | <0.001 |
| 65+ (ref) | -- | -- | -- | -- | -- | -- |
| Ethnicity | ||||||
| Asian | -0.06 (-0.12, 0.002) | 0.062 | *-0.44 (-0.49, -0.39) | <0.001 | *-0.37 (-0.44, -0.31) | <0.001 |
| Black | -0.02 (-0.09, 0.06) | 0.676 | *-0.36 (-0.42, -0.29) | <0.001 | *-0.25 (-0.33, -0.16) | <0.001 |
| Other | -0.03 (-0.14, 0.08) | 0.598 | *-0.24 (-0.34, -0.14) | <0.001 | *-0.20 (-0.31, -0.10) | <0.001 |
| White (ref) | -- | -- | -- | -- | -- | -- |
| Socioeconomic Status | ||||||
| AB (high-SES) | *0.35 (0.30, 0.39) | <0.001 | *0.40 (0.36, 0.44) | <0.001 | *0.31 (0.27, 0.35) | <0.001 |
| C1 | *0.21 (0.17, 0.24) | <0.001 | *0.28 (0.24, 0.31) | <0.001 | *0.20 (0.17, 0.24) | <0.001 |
| C2 | *0.10 (0.05, 0.14) | <0.001 | *0.13 (0.09, 0.17) | <0.001 | *0.12 (0.08, 0.16) | <0.001 |
| DE (low-SES) (ref) | -- | -- | -- | -- | -- | -- |
| Familiarity with mental health | ||||||
| Self | *0.77 (0.71, 0.83) | <0.001 | *0.86 (0.80, 0.91) | <0.001 | *0.82 (0.77, 0.87) | <0.001 |
| Other | *0.44 (0.41, 0.47) | <0.001 | *0.55 (0.52, 0.58) | <0.001 | *0.56 (0.52, 0.59) | <0.001 |
| None (ref) | -- | -- | -- | -- | -- | -- |
| Region n (%) | ||||||
| North East | *0.15 (0.07, 0.23) | <0.001 | *0.33 (0.26, 0.40) | <0.001 | *0.22 (0.14, 0.30) | <0.001 |
| North West | *0.13 (0.07, 0.18) | <0.001 | *0.26 (0.21, 0.32) | <0.001 | *0.26 (0.20, 0.32) | <0.001 |
| Yorks & Humb | *0.19 (0.13, 0.26) | <0.001 | *0.33 (0.27, 0.39) | <0.001 | *0.31 (0.24, 0.37) | <0.001 |
| East Midlands | *0.14 (0.07, 0.20) | <0.001 | *0.20 (0.14, 0.26) | <0.001 | *0.20 (0.13, 0.26) | <0.001 |
| West Midlands | *0.09 (0.03, 0.15) | 0.002 | *0.20 (0.14, 0.25) | <0.001 | *0.19 (0.13, 0.25) | <0.001 |
| East of England | *0.10 (0.04, 0.16) | 0.002 | *0.21 (0.16, 0.27) | <0.001 | *0.18 (0.12, 0.24) | <0.001 |
| South East | *0.09 (0.03, 0.14) | 0.001 | *0.19 (0.14, 0.24) | <0.001 | *0.15 (0.09, 0.20) | <0.001 |
| South West | *0.14 (0.08, 0.21) | <0.001 | *0.30 (0.24, 0.36) | <0.001 | *0.18 (0.12, 0.24) | <0.001 |
| London (ref) | -- | -- | -- | -- | -- | -- |
*Statistically significant at the p<0.05 level
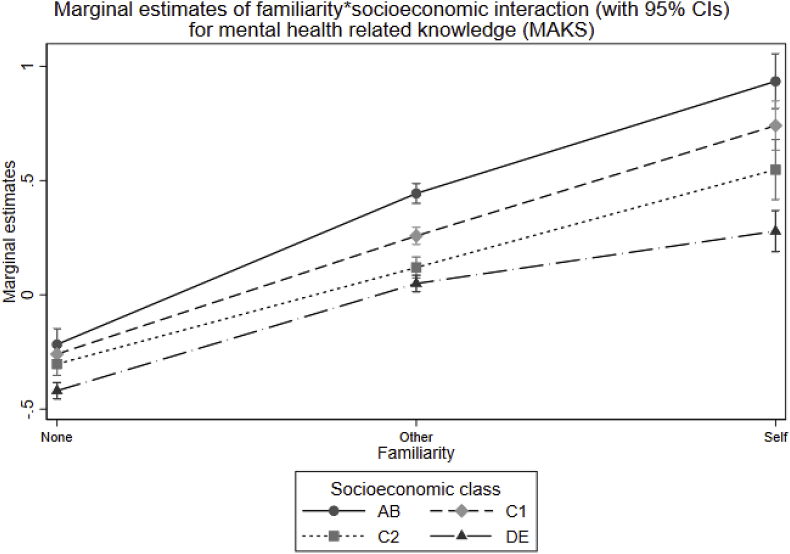
Fig. 1 displays the predictive margins from the regression analysis on mental health-related knowledge for each category of familiarity and socioeconomic status within the interaction term. It illustrates stronger knowledge as the level of familiarity increases (none; other; self) and how the strength of this relationship differs among categories of socioeconomic status. The association between stigma related knowledge and familiarity is weaker in lower socioeconomic groups and strengthens as socioeconomic class increases. The marginal estimate difference between self-familiarity and no familiarity is 0.7 within the DE class, 0.85 within the C1 class, 1.0 within the C2 class and increases to 1.15 within the AB class. A joint Wald test was performed and showed strong evidence that all coefficients associated with the interaction between socioeconomic status and familiarity were significantly different from zero (p<0.001). The results of the regression analysis including standardised effect sizes, 95% confidence intervals and p values are shown in Supplementary Table 1.
Fig 1.
Predictive margins with 95% confidence intervals for the interaction between familiarity and socioeconomic status for mental health-related public knowledge (MAKS).
3.2.2. Mental health-related public attitudes
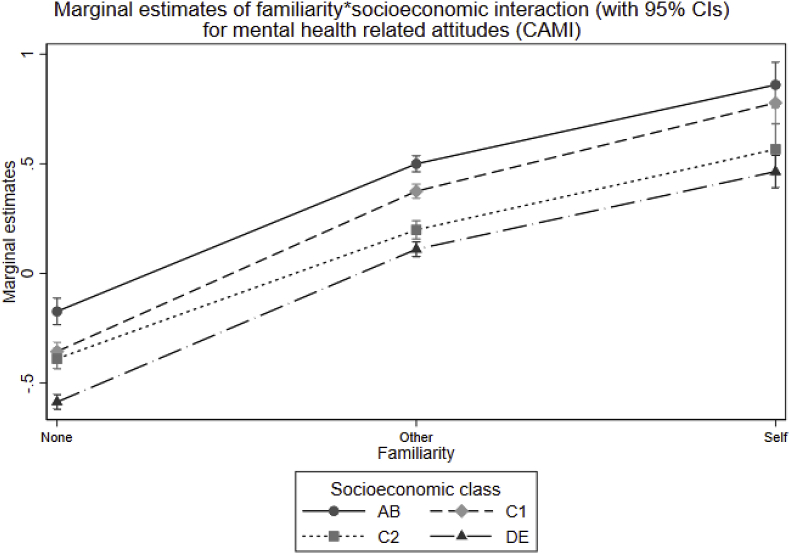
Table 2 presents the results of the initial model to examine the relationship between mental health-related public attitudes and familiarity. Results show mental health-related public attitudes are more positive in groups with familiarity (p<0.001) and in higher socioeconomic groups (p<0.001).
Fig. 2 displays the predictive margins from the regression analysis on mental health-related attitudes for each category of familiarity and socioeconomic status within the interaction term, which illustrates the relationship of more positive attitudes as the level of familiarity increases. The strength of this relationship differs only modestly among categories of socioeconomic status and shows no distinct pattern. The association is strongest in the those from socioeconomic group C1 and weakest for those from socioeconomic group C2, with a marginal estimate difference between self-familiarity and no familiarity of 1.14 and 0.96 respectively. The socioeconomic groups AB and DE also show a strong association is present with a marginal estimate difference of 1.03 and 1.05 respectively. A joint Wald test was performed and didn’t give a statistically significant result that the coefficients associated with the interaction were different from zero (p=0.057). The results of the regression analysis including standardised effect sizes, 95% confidence intervals and p values are shown in Supplementary Table 1.
Fig 2.
Predictive margins with 95% confidence intervals for the interaction between familiarity and socioeconomic status for mental health-related public attitudes (CAMI).
3.2.3. Public desire for social distance from mental health problems
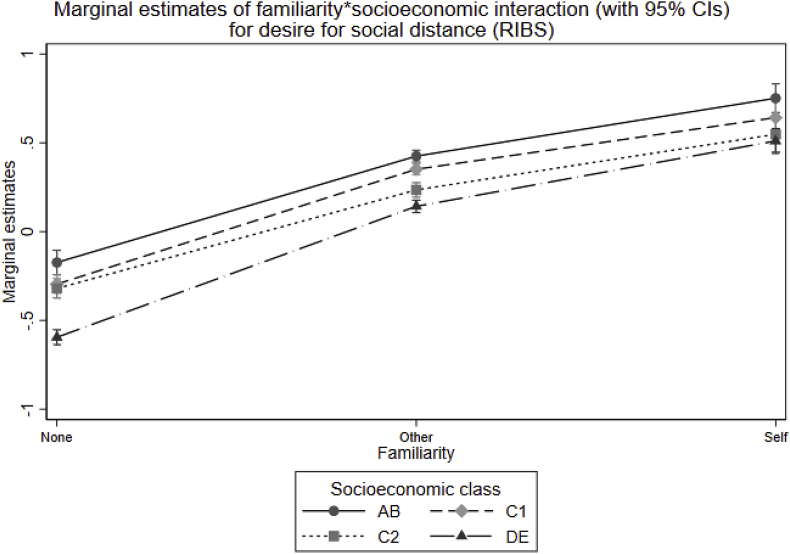
Table 2 presents the results of the initial model to examine the relationship between public desire for social distance from mental health problems and familiarity. Results show less desire for social distance among people with familiarity (p<0.001) and higher socioeconomic groups (p<0.001).
Fig. 3 displays the predictive margins from the regression analysis on desire for social distance from mental health problems for each category of familiarity and socioeconomic status within the interaction term. This illustrates an increase in willingness for social contact (or decreased desire for social distance) from mental health problems as the level of familiarity increases and how this relationship differs among levels of socioeconomic status. The association between desire for social distance and familiarity is strongest in the those from socioeconomic group DE and weakest for those from socioeconomic group C2, with a marginal estimate difference between self-familiarity and no familiarity of 1.11 and 0.87 respectively. Socioeconomic groups AB and C1 show a relatively strong association with a marginal estimate difference of 0.92 and 0.94 respectively. A joint Wald test was performed and showed evidence that all coefficients associated with the interaction between socioeconomic status and familiarity were significantly different from zero (p=0.0118). The results of the regression analysis including standardised effect sizes, 95% confidence intervals and p values are shown in Supplementary Table 1.
Fig 3.
Predictive margins with 95% confidence intervals for the interaction between familiarity and socioeconomic status for public desire for social distance from mental health problems (RIBS IB).
4. Discussion
4.1. Findings
The sample characteristics suggest a complicated relationship between familiarity and socioeconomic status. The higher proportion of participants with familiarity though personal experience in low socioeconomic groups suggest prevalence of mental illness is higher, consistent with epidemiological studies (McManus et al., 2016). In contrast, a lower proportion of participants in lower socioeconomic groups report familiarity with others. This could reflect lower awareness of and communication about mental health in lower socioeconomic groups.
The results show that both socioeconomic status and familiarity are independently associated with stigma related outcomes. While the reasons for more negative stigma outcomes among lower socioeconomic groups in the absence of familiarity are not known, they may include lower levels of education (Ilic N et al., 2016) or poorer access to mental health services (Foundation, 2014). Similarly, while the mechanisms of effect of familiarity have not been clearly elucidated, they may operate through the same mediators that make intergroup contact effective as reducing other forms of prejudice-increased empathy, reduced anxiety and better knowledge (Pettigrew & Tropp, 2008).
The interaction term between socioeconomic status and familiarity for the knowledge outcome suggests that, as hypothesised, the positive effect of familiarity on stigma related knowledge is weaker in lower socioeconomic status groups, particularly for those with personal experience. One possible reason for this is a poorer treatment outcome, either as a result of worse treatment itself or response to treatment (or both), and this could lead to those ‘familiar’ with mental illness expressing relatively more therapeutic pessimism. This results in lower scores on the MAKS as the items focus on response to treatment and recovery. In addition, experience that mental health problems result from social issues may result in therapeutic pessimism and deter treatment seeking.
In contrast, the interaction between socioeconomic status and familiarity for attitudes and desire for social distance shows the effect of familiarity is still powerful for lower socioeconomic groups, appearing to partially mitigate the effect of socioeconomic status on those without such familiarity. In groups exposed to more social adversity, familiarity may lead to a particularly strong appreciation of social determinants, which in turn may have a de-stigmatising effect (Clement et al., 2010).
4.2. Strengths and limitations
This analysis used a nationally representative dataset from a tailored annual survey for the evaluation of Time to Change. The survey includes different aspects of stigma as outcome measures which is particularly important as we have shown different direction of results can arise.
A limitation of our study is that while the results support our hypothesis that poorer treatment response in lower socioeconomic groups leads to lower measures of stigma related knowledge, we are not able to examine this directly in this sample. This would require detailed knowledge about the illness and treatment experiences not only of those reporting personal experience but also of those with whom those reporting familiarity have a relationship. This would probably require a larger sample. In addition, qualitative methods could be used to better understand how socioeconomic status influences stigma outcomes, and how socioeconomic status and potentially other factors moderate the effects of familiarity. The inclusion of other measures of socioeconomic status not available in this survey, for example education and income, could also increase our understanding of these results.
4.3. Implications
Our results both support the approach taken by anti-stigma programmes such as Time to Change and also suggest it may have limitations. Soon after its launch in 2009, a key message added to the Time to Change social marketing campaign was the importance of talking about mental health, in part to increase comfort and confidence in supporting someone with a mental illness. Greater openness is also likely to increase the proportion of the population familiar with someone with a mental illness, as is supported by the results of the Attitudes to Mental Illness survey (Henderson & Robinson, 2017). In turn, familiarity is associated with reduced stigma. From its launch in 2009 until 2016, the social marketing campaign targeted middle income groups (B and C). Since 2016 the target group overlaps but now includes some of those on lower incomes (C and D), although not the lowest. As our results show lower rates of familiarity in lower socioeconomic groups and a strong effect of familiarity on attitudes and desire for social distance, this approach appears well justified and likely to be effective.
However, our results also suggest lower stigma related knowledge in spite of personal experience among people in lower socioeconomic groups. Their more negative views about one’s ability to recover and the helpfulness of treatment are in keeping with previous work suggesting treatment outcomes are worse in low income groups. This may be due to greater exposure to the social determinants of mental ill health, such as material disadvantage and job security (Foundation, 2014), or to problems with some treatments which make them less acceptable to or less effective. A better understanding of the reasons for this greater pessimism may lead to more effective responses, whether medical, psychological or social. Given the evidence for social determinants of mental ill health, it seems that the developments of social responses should be a particular focus. An example is the provision of welfare advice in healthcare settings (Woodhead et al., 2017). However, as therapeutic pessimism may deter people from seeking mental health treatment in the first place, social responses independent of health care should also be considered (de Vries & Horstman, 2016). We suggest qualitative methods would be suitable to further explore the socioeconomic influences on stigma outcomes and that better understanding of these influences should inform responses to both mental health problems and stigma in lower socioeconomic groups. Without such exploration an interpretation of survey results that people in lower socioeconomic groups are simply more stigmatising seems itself a stigmatising response towards this group of people.
Ethical standards
The manuscript does not contain clinical studies or patient data.
Ethical statement
The manuscript does not contain clinical studies or patient data. The King’s College London Psychiatry, Nursing and Midwifery Research Ethics Subcommittee exempted this study as secondary analysis of anonymised data.
CRediT authorship contribution statement
Laura C. Potts: Conceptualization, Methodology, Software, Validation, Formal analysis, Resources, Data curation, Writing - original draft, Writing - review & editing, Visualization. Claire Henderson: Conceptualization, Writing - original draft, Writing - review & editing, Supervision, Funding acquisition.
Declaration of competing interest
CH has received an honorarium from Lundbeck for consultancy on an anti-stigma programme and an honorarium from Janssen for teaching on stigma to mental health professionals. LP declares that she has no conflict of interests.
Acknowledgments
The Time to Change evaluation was funded by the UK Government Department of Health, Comic Relief and Big Lottery Fund. CH was supported by these grants during phases 1–3 of TTC and LP during phase 3. The funding sources had no involvement in the study design, data, or report writing. We thank Sue Baker, Maggie Gibbons, and Paul Farmer, Mind; Paul Corry and Mark Davies, Rethink Mental Illness, for their collaboration. Claire Henderson is supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South London at South London and Maudsley NHS Foundation Trust. The views expressed are those of the author and not necessarily those of the NHS, the NIHR or the Department of Health.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2020.100611.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Al Ramiah A., Hewstone M. Intergroup contact as a tool for reducing, resolving, and preventing intergroup conflict evidence. Limitations, and Potential. 2013;68:527–542. doi: 10.1037/a0032603. [DOI] [PubMed] [Google Scholar]
- Bhavsar V. Regional differences in mental health stigma-Analysis of nationally representative data from the Health Survey for England. PloS One. 2014;14(1) doi: 10.1371/journal.pone.0210834. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cechnicki A., Angermeyer M.C., Bielańska A. Anticipated and experienced stigma among people with schizophrenia: Its nature and correlates. Social Psychiatry and Psychiatric Epidemiology. 2011;46(7):643–650. doi: 10.1007/s00127-010-0230-2. [DOI] [PubMed] [Google Scholar]
- Clement S. Messages to use in population-level campaigns to reduce mental health-related stigma: Consensus development study. Epidemiologica e Psichiatria Sociale. 2010;19:72–79. doi: 10.1017/s1121189x00001627. [DOI] [PubMed] [Google Scholar]
- Clement S. Disability hate crime and targeted violence and hostility: A mental health and discrimination perspective. Journal of Mental Health. 2011;20(3):219–225. doi: 10.3109/09638237.2011.579645. [DOI] [PubMed] [Google Scholar]
- Cohen A. Socioeconomic status and anxiety as predictors of antidepressant treatment response and suicidal ideation in older adults. Social Psychiatry and Psychiatric Epidemiology. 2008;44(4):272. doi: 10.1007/s00127-008-0436-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan P.W., Watson A.C. The stigma of psychiatric disorders and the gender, ethnicity, and education of the perceiver. Community Mental Health Journal. 2007;43(5):439–458. doi: 10.1007/s10597-007-9084-9. [DOI] [PubMed] [Google Scholar]
- Evans-Lacko S. Development and psychometric properties of the mental health knowledge Schedule. Canadian Journal of Psychiatry. 2010;55(7):440–448. doi: 10.1177/070674371005500707. [DOI] [PubMed] [Google Scholar]
- Evans-Lacko S. Development and psychometric properties of the reported and intended behaviour scale (RIBS): A stigma-related behaviour measure. Epidemiology and Psychiatric Sciences. 2011;20(3):263–271. doi: 10.1017/s2045796011000308. [DOI] [PubMed] [Google Scholar]
- Evans-Lacko S. Influence of Time to Change's social marketing interventions on stigma in England 2009-2011. British Journal of Psychiatry. 2013;202(s55):s77–s88. doi: 10.1192/bjp.bp.113.126672. [DOI] [PubMed] [Google Scholar]
- Evans-Lacko S., Henderson C., Thornicroft G. Public knowledge, attitudes and behaviour regarding people with mental illness in England 2009-2012. British Journal of Psychiatry - Supplement. 2013;55:s51–s57. doi: 10.1192/bjp.bp.112.112979. [DOI] [PubMed] [Google Scholar]
- Finegan M. Associations between socioeconomic status and psychological therapy outcomes: A systematic review and meta-analysis. Depression and Anxiety. 2018;35(6):560–573. doi: 10.1002/da.22765. [DOI] [PubMed] [Google Scholar]
- Foundation, W.H.O.a.C.G. WHO; Geneva: 2014. Social determinants of mental health. [Google Scholar]
- González-Sanguino C. Time to change's social marketing campaign for a new target population: Results from 2017 to 2019. BMC Psychiatry. 2019;19(1):417. doi: 10.1186/s12888-019-2415-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansson L., Stjernswärd S., Svensson B. Changes in attitudes, intended behaviour, and mental health literacy in the Swedish population 2009–2014: An evaluation of a national antistigma programme. Acta Psychiatrica Scandinavica. 2016;134:71–79. doi: 10.1111/acps.12609. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler M.L., Phelan J.C., Link B.G. Stigma as a fundamental cause of population health inequalities. American Journal of Public Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson C. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry. 2014;1(6):467–482. doi: 10.1016/S2215-0366(14)00023-6. [DOI] [PubMed] [Google Scholar]
- Henderson C. Public knowledge, attitudes, social distance and reported contact regarding people with mental illness 2009-2015. Acta Psychiatrica Scandinavica. 2016;134(Suppl 446):23–33. doi: 10.1111/acps.12607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson C., Potts L., Robinson E. Mental illness stigma after a decade of Time to Change England: Inequalities as targets for further improvement. European Journal of Public Health. 2020 doi: 10.1093/eurpub/ckaa013. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson C., Robinson E. Department of Health Survey Evaluation Report (2008-2017); 2017. [Google Scholar]
- Ilic N H.H., Henderson C., Evans-Lacko S., Thornicroft G. Attitudes towards mental illness. In: Craig R., Fuller E., Mindell J., editors. Health survey for England 2014: Health, social care and lifestyles. Health and Social Care Information Centre; London: 2016. [Google Scholar]
- Jakubovski E., Bloch M.H. Prognostic subgroups for citalopram response in the STAR*D trial. Journal of Clinical Psychiatry. 2014;75(7):738–747. doi: 10.4088/JCP.13m08727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorm A.F. Attitudes towards people with a mental disorder: A survey of the Australian public and health professionals. Australian and New Zealand Journal of Psychiatry. 1999;33(1):77–83. doi: 10.1046/j.1440-1614.1999.00513.x. [DOI] [PubMed] [Google Scholar]
- Knaak S., Mantler E., Szeto A. Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. Healthcare Management Forum. 2017;30(2):111–116. doi: 10.1177/0840470416679413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauber C. What about psychiatrists' attitude to mentally ill people? European Psychiatry. 2004;19(7):423–427. doi: 10.1016/j.eurpsy.2004.06.019. [DOI] [PubMed] [Google Scholar]
- Laursen T.M. Increased mortality among patients admitted with major psychiatric disorders: A register-based study comparing mortality in unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia. Journal of Clinical Psychiatry. 2007;68(6):899–907. doi: 10.4088/jcp.v68n0612. [DOI] [PubMed] [Google Scholar]
- Link B.G., Phelan J.C. Conceptualizing stigma. Annual Review of Sociology. 2001;27(1):363–385. [Google Scholar]
- Mai Q. Mental illness related disparities in diabetes prevalence, quality of care and outcomes: A population-based longitudinal study. BMC Medicine. 2011;9:118. doi: 10.1186/1741-7015-9-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McManus S., Bebbington P.E., Jenkins R., Brugha T., editors. Mental health and wellbeing in England: Adult psychiatric morbidity survey 2014. NHS Digital; Leeds: 2016. [Google Scholar]
- Mehta N. Evidence for effective interventions to reduce mental health-related stigma and discrimination in the medium and long term: Systematic review. British Journal of Psychiatry. 2015;207(5):377–384. doi: 10.1192/bjp.bp.114.151944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettigrew T.F., Tropp L.R. How does intergroup contact reduce prejudice? Meta‐analytic tests of three mediators. European Journal of Social Psychology. 2008;38(6):922–934. [Google Scholar]
- Robinson E.J., Henderson C. Public knowledge, attitudes, social distance and reporting contact with people with mental illness 2009-2017. Psychol Med. 2018:1–10. doi: 10.1017/S0033291718003677. [DOI] [PubMed] [Google Scholar]
- Ronalds C. Outcome of anxiety and depressive disorders in primary care. British Journal of Psychiatry. 2018;171(5):427–433. doi: 10.1192/bjp.171.5.427. [DOI] [PubMed] [Google Scholar]
- Star S.A. National Opinion Research Center; 1952. What the public thinks about mental health and mental illness: A paper. [Google Scholar]
- Taylor S.M., Dear M.J. Scaling community attitudes toward the mentally ill. Schizophrenia Bulletin. 1981;7(2):225–240. doi: 10.1093/schbul/7.2.225. [DOI] [PubMed] [Google Scholar]
- TNS BMRB . Time to Change; 2015. Attitudes to mental illness 2014 research report.https://www.time-to-change.org.uk/sites/default/files/Attitudes_to_mental_illness_2014_report_final_0.pdf [cited 2019 03/01/2019]; Available from: [Google Scholar]
- Unit S.E. Office of the Deputy Prime Minister; London: 2004. Mental health and social exclusion. [Google Scholar]
- de Vries M., Horstman K. Bianca in the neighborhood: Moving beyond the ‘reach paradigm’ in public mental health AU - knibbe, mare. Critical Public Health. 2016;26(4):434–445. [Google Scholar]
- Wang J. Gender specific correlates of stigma toward depression in a Canadian general population sample. Journal of Affective Disorders. 2007;103(1):91–97. doi: 10.1016/j.jad.2007.01.010. [DOI] [PubMed] [Google Scholar]
- Woodhead C. Impact of co-located welfare advice in healthcare settings: Prospective quasi-experimental controlled study. British Journal of Psychiatry. 2017;211(6):388–395. doi: 10.1192/bjp.bp.117.202713. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.