Abstract
Introduction
Proximal tibial fractures are common with an incidence of 10.2/100.000. Those displaced and involving the articular surface will often require surgical treatment. However, no consensus exists on whether to allow the patient early weight bearing or not. We developed a technique using structural bone chips, highly impacted under the articular surface, to permit immediate weight bearing after surgery.
Patient
The patient was a 44-year old male who suffered a lateral tibial plateau fracture (AO type 41B2).
Intervention
We used an anterolateral approach with an S-shaped incision. A small window in the tibia was made using an awl, and the articular surface was reduced under radiographic imaging. The bone allograft was prepared by splitting the frozen femoral head in quarters and then taking large pieces of bone with a bone rongeur forceps avoiding the cartilage. The large pieces of bone were gathered in a small tray and thereafter compressed into the drill guide insert. The drill guide filled with bone graft was then inserted into the tibia window and directed in the appropriate position guided by radiography. Hereafter, the bone graft was impacted under the articular surface with force using the appropriate trocar and a hammer, and the fracture was finally reduced. Finally, the fracture was fixated utilizing an angular stable plate.
Outcome
The patient was followed up one year postoperatively and allowed immediate weight bearing after surgery. No subsequent articular collapse occurred.
Discussion
In this case, we present a proximal tibial fracture with articular depression, which was surgically treated with a highly impacted bone allograft of large pieces and a locking plate. The patient was allowed immediate weight bearing and no subsequent articular collapse occurred.
Keywords: Tibial plateau fracture, Weight bearing, Bone grafting, Case reports, Early mobilization
Introduction
Proximal tibial fractures are common with an incidence of 10.2/100.000 [1]. Those displaced will require surgical treatment to reduce the risk of malalignment, post-traumatic osteoarthritis, and reduced functional outcome. Surgical treatment involves reduction of the fracture, management of subchondral bone defects with a bone substitute, and fixation of the fracture with an angular stable plate [2].
No consensus exists on whether to allow weight bearing or not after the osteosynthesis of a proximal tibial fracture, regardless of fracture type. The concern of early weight bearing in proximal tibial fractures is the risk of subsequent articular collapse. The AO foundation recommends no weight bearing for 10–12 weeks after surgery for an articular proximal tibial fracture (surgeryreference.aofoundation.org). However, small observational studies have reported early weight bearing after osteosynthesis of a proximal tibial fracture without an increased risk of subsequent articular collapse [[3], [4], [5], [6]]. The surgical technique was not, though, formally described in these studies. Early weight bearing may be crucial for rehabilitation and good functional outcome and critical for the elderly since non-weight bearing is four times as demanding when walking [7]. A demand the older patients most often cannot honor and therefore need support.
We developed a technique using structural bone chips from a frozen allograft, which was highly impacted under the articular surface to allow immediate weight bearing after surgery and for the final reposition of the articular surface. The purpose of this article is to present a case using this surgical technique.
Patient information
The patient was a 44-year old male who was kicked by a horse in the head and suffered a concussion and a facial injury that needed plastic surgery. Plastic surgery was performed the day after the trauma, and afterward the patient complained of left knee pain, and the following radiography revealed a proximal lateral tibial fracture. He could not describe the actual mechanism of injury to the knee.
The patient presented no skin lesions on the left knee and was otherwise healthy. We performed the surgery nine days after the trauma.
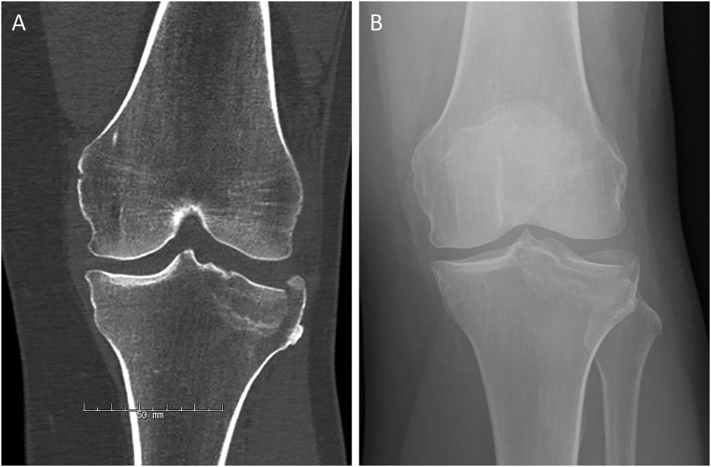
A preoperative CT scan of the left knee was performed, which showed a displaced lateral tibial plateau fracture with a fracture line beyond the eminentia intercondylaris (AO type 41B2) (Fig. 1).
Fig. 1.
A: Radiography of the left knee. B: CT scan of the left knee.
Intervention
The intervention was based on existing techniques using a bone allograft to support the articular surface and a locking plate to fixate the fracture [5,8,9]. The last author, TB, further developed this technique as described below. No approval from the Ethics Committee was needed (study id: SJ-634).
The goal of the procedure was to perform a stable osteosynthesis in which a solid bone graft would support the articular surface of the tibia after reduction. This would allow the patient early mobilization with immediate weight bearing after surgery. To achieve this, we aimed to create a bone graft that would be more solid than morselized bone graft previously described [8] and to impact the bone graft sufficiently similar to earlier studies on hip revision surgery [10].
The patient was positioned in a supine position with the leg rested on a wedge. The surgery was performed without the use of a tourniquet. The patient was given preoperative antibiotics of 1500 mg cefuroxime.
The bone allograft was a frozen femoral head. The second author (EB) performed the surgery at Slagelse Hospital, Region Zealand, Denmark.
We used an anterolateral approach with an S-shaped incision. A small window was made in the anterolateral cortex of the tibia using an awl, and the articular surface was reduced under radiographic imaging. The bone graft was prepared by splitting the frozen femoral head in quarters and then taking large pieces of bone with a bone rongeur forceps avoiding the cartilage. The large pieces of bone were gathered in a small tray and thereafter compressed into the drill guide insert (Fig. 2). The drill guide filled with bone graft was then inserted into the window in the tibia and directed in the appropriate position guided by radiography. Hereafter, the bone graft was impacted under the articular surface with force using the appropriate trocar and a hammer (Fig. 3), and the fracture was finally reduced. Finally, the fracture was fixated utilizing an angular stable plate (Fig. 4).
Fig. 2.
A: The femoral head is divided in quarters allowing for easier grasp with the bone rongeur forceps. B: Bone chips up to 10 mm are gathered in a metal tray (C). D: The bone chips are stomped into the drill guide.
Fig. 3.
A: The drill guide is placed under the articulate surface guided by radiography. B: The bone allograft is impacted with force through the drill guide.
Fig. 4.
A: Postoperative radiography, B: 1-year follow-up radiography.
Follow-up and outcomes
The patient was followed up after 2 and 6 weeks, 3 and 12 months postoperatively and was allowed immediate weight bearing after surgery. There was no secondary collapse of the articular surface or widening of the tibial plateau. The range of motion was 10 to 80 degrees at the 2-week follow-up, 0–125 degrees at the 6-week follow-up, and 0–140 degrees (full range of motion) at 12 months. The patient performed 15 rises in the 30-second chair-stand-test at the 2-week follow-up and 29 rises at the 1-year follow-up. The patient returned to work three months after surgery.
Discussion
This study describes an operative technique for the osteosynthesis of a proximal tibial fracture with articular depression using a highly impacted bone allograft of large pieces and a locking plate. The patient was allowed immediate weight bearing, and no subsequent articular collapse occurred.
The study was reported accordingly to the SCARE guidelines [11] and TIDieR [12], which allow this procedure to be replicated by others. No other studies have described a similar technique or at the same level of detail.
The nature of the study limits the study since only a single case is presented. Thus, even though successful in this patient, we do not know if this would apply for all patients with a proximal tibial fracture with articular depression. We are currently performing an observational study (ClinicalTrials.gov identifier: NCT03314623) to support the continued use of the technique and subsequent immediate weight bearing. Until this study is reported, orthopedic surgeons may replicate the technique and make their own decision whether to allow immediate weight bearing or not.
No consensus exists on whether to allow immediate weight bearing after osteosynthesis of a proximal tibial fracture or not. Recent observational studies have shown no increased risk of subsequent articular collapse after immediate weight bearing regardless of fracture type [13,14], suggesting immediate weight as safe post-operative management. The post-operative management in our department is in line with these studies though most surgeons lean towards a non-weight bearing regime, the more complex and comminuted the fracture is. However, Callary et al. argue that more plates allow for immediate weight bearing even in Schatzker type 5 and 6 fracture [13].
The use of bone allografts to support the articular surface after reduction is debatable. In tibial plateau fractures with subsequent loss of bone in the subchondral space, the use of a bone graft substitute is used to support the successful elevation of a depressed tibial plateau fragment. No consensus exists on which type of bone graft substitute is superior. Cancellous autograft from the iliac crest has been the “gold standard” but has lately been abandoned because of numerous complications and prolonged surgical time [15] and might not provide the same mechanical stability needed to support the articular surface. A systematic review [16] found that synthetic bone substitutes were superior to biological substitutes for preventing secondary articular collapse. However, these studies were small and did not include any comparable randomized studies, and only one study included the use of bone allograft from a frozen femoral head and only in 6 patients. Furthermore, not only the type of bone graft substitute must be considered but also the surgical technique of its implementation. Veitch et al. suggested a compaction morselized bone grafting technique [8] for better support, especially in the elderly osteoporotic patient, but did not allow early weight bearing. We believe the use of large fragments of bone allograft, which afterward is highly compacted, is the best way to provide mechanical stability.
Even though the technique described is new compared to existing literature, the differences in surgical techniques are still small. We do not know how or if these small differences may affect the patient in the long-term outcome (pain and function) or risk of osteoarthritis. Large scale randomized studies are needed for this, but the feasibility of these studies is difficult and might not even be possible [17,18].
In this case, we presented a proximal tibial fracture with articular depression, which was surgically treated with a highly impacted bone allograft and a locking plate. The patient was allowed immediate weight bearing, and no subsequent articular collapse occurred in one year. We believe the technique is a viable method to permit early weight bearing with a positive impact on rehabilitation and return to work.
Informed consent
All figures in this paper are presented with the acceptance of the patient involved.
Declaration of competing interest
None.
Acknowledgments
The research is supported by Naestved, Slagelse and Ringsted Hospitals' Research Fund.
References
- 1.Elsoe R., Larsen P., Nielsen N.P.H., Swenne J., Rasmussen S., Ostgaard S.E. Population-based epidemiology of tibial plateau fractures. Orthopedics. 2015;38:e780–e786. doi: 10.3928/01477447-20150902-55. [DOI] [PubMed] [Google Scholar]
- 2.Raschke M.J., Kitt C., Domnick C. Partial proximal tibia fractures. EFORT Open Rev. 2017;2:241–249. doi: 10.1302/2058-5241.2.160067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haak K.T., Palm H., Holck K., Krasheninnikoff M., Gebuhr P., Troelsen A. Immediate weight-bearing after osteosynthesis of proximal tibial fractures may be allowed. Dan. Med. J. 2012;59 [PubMed] [Google Scholar]
- 4.Thewlis D., Fraysse F., Callary S.A., Verghese V.D., Jones C.F., Findlay D.M., Atkins G.J., Rickman M., Solomon L.B. Postoperative weight bearing and patient reported outcomes at one year following tibial plateau fractures. Injury. 2017;48:1650–1656. doi: 10.1016/j.injury.2017.05.024. [DOI] [PubMed] [Google Scholar]
- 5.Van De Pol G.J., Iselin L.D., Callary S.A., Thewlis D., Jones C.F., Atkins G.J., Solomon L.B. Impaction bone grafting has potential as an adjunct to the surgical stabilisation of osteoporotic tibial plateau fractures: early results of a case series. Injury. 2015;46:1089–1096. doi: 10.1016/j.injury.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 6.Solomon L.B., Callary S.A., Stevenson A.W., McGee M.A., Chehade M.J., Howie D.W. Weight-bearing-induced displacement and migration over time of fracture fragments following split depression fractures of the lateral tibial plateau: a case series with radiostereometric analysis. J. Bone Jt. Surg Br. 2011;93-B:817–823. doi: 10.1302/0301-620X.93B6.26122. [DOI] [PubMed] [Google Scholar]
- 7.Westerman R.W., Hull P., Hendry R.G., Cooper J. The physiological cost of restricted weight bearing. Injury. 2008;39:725–727. doi: 10.1016/j.injury.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 8.Veitch S.W., Stroud R.M., Toms A.D. Compaction bone grafting in tibial plateau fracture fixation. J. Trauma. 2010;68:980–983. doi: 10.1097/TA.0b013e3181b16e3d. [DOI] [PubMed] [Google Scholar]
- 9.Segur J.M., Torner P., Garc S., Combal A., Suso S., Ramón R. Use of bone allograft in tibial plateau fractures. Arch. Orthop. Trauma Surg. 1998;117:357–359. doi: 10.1007/s004020050265. [DOI] [PubMed] [Google Scholar]
- 10.Ullmark G., Orthop A., Surg T. Bigger size and defatting of bone chips will increase cup stability. Arch. Orthop. Trauma Surg. 2000;120:445–447. doi: 10.1007/s004029900122. http://www.ncbi.nlm.nih.gov/pubmed/10968536 [DOI] [PubMed] [Google Scholar]
- 11.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A.J., Orgill D.P., Zhu H., Alsawadi A., Noureldin A., Rao A., Enam A., Thoma A., Bashashati M., Vasudevan B., Beamish A., Challacombe B., De Wilde R.L., Machado-Aranda D., Laskin D., Muzumdar D., D’cruz A., Manning T., Healy D., Pagano D., Goel P., Ranganathan P., Pai P.S., Raja S., Ather M.H., kadioäžlu H., Nixon I., Mukherjee I., Gómez Rivas J., Raveendran K., Derbyshire L., Valmasoni M., Chalkoo M., Raison N., Muensterer O., Bradley P., Roberto C., Afifi R., Rosin D., Klappenbach R., Wynn R., Giordano S., Basu S., Surani S., Suman P., Thorat M., Kasi V. The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 12.Hoffmann T.C., Glasziou P.P., Boutron I., Milne R., Perera R., Moher D., Altman D.G., Barbour V., Macdonald H., Johnston M., Kadoorie S.E.L., Dixon-Woods M., McCulloch P., Wyatt J.C., Phelan A.W.C., Michie S. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348 doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- 13.Callary S.A., Jones C.F., Kantar K., Du Toit H., Baker M.P., Thewlis D., Atkins G.J., Solomon L.B. A new approach to surgical management of tibial plateau fractures. J. Clin. Med. 2020;9:626. doi: 10.3390/jcm9030626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williamson M., Iliopoulos E., Jain A., Ebied W., Trompeter A. Immediate weight bearing after plate fixation of fractures of the tibial plateau. Injury. 2018;49:1886–1890. doi: 10.1016/j.injury.2018.06.039. [DOI] [PubMed] [Google Scholar]
- 15.Myeroff C., Archdeacon M. Autogenous bone graft: donor sites and techniques. J. Bone Jt. Surg. Ser. A. 2011;93:2227–2236. doi: 10.2106/JBJS.J.01513. [DOI] [PubMed] [Google Scholar]
- 16.Goff T., Kanakaris N.K., Giannoudis P.V. Use of bone graft substitutes in the management of tibial plateau fractures. Injury. 2013;44 doi: 10.1016/S0020-1383(13)70019-6. [DOI] [PubMed] [Google Scholar]
- 17.Hare K.B., Lohmander L.S., Roos E.M. The challenge of recruiting patients into a placebo-controlled surgical trial. Trials. 2014;15:1–5. doi: 10.1186/1745-6215-15-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCulloch P., Taylor I., Sasako M., Lovett B., Griffin D. Randomised trials in surgery: problems and possible solutions. Br. Med. J. 2002;324:1448–1451. doi: 10.1136/bmj.324.7351.1448. [DOI] [PMC free article] [PubMed] [Google Scholar]