Abstract
Introduction:
The integration of point-of-care ultrasound (POCUS) in preclerkship medical education is currently popular and based on the notion that POCUS may improve diagnostic and procedural skills in medical students. However, empirical evidence demonstrating that POCUS can enhance clinical skills in preclerkship students has been lacking. We sought to evaluate anatomical sonographic knowledge and ultrasound generation capabilities associated with the implementation of a 3-h echocardiography training camp led by 2 emergency physicians and using a flipped classroom design.
Methods:
Preclerkship students from the University of Ottawa (n = 32) were recruited to participate. A flipped classroom model was adopted, providing students with a 3-chaptered peer-designed, expert validated ultrasound manual before the workshop, to maximize scanning times (2 h of reading). A pretest Likert-type design was used to assess student perception of the ultrasound tool. Similarly, a pretest/post-test model was used to assess sonographic anatomical identification. In addition, a subsequent Objective Structured Clinical Examination (OSCE) test was done 3 weeks after the hands-on session, to evaluate image generation (4 cardiac views: parasternal long, parasternal short, subxiphoid, and apical 4 chambers), understanding of knobology and structural labeling.
Results:
For the sonographic anatomy, there was a statistically significant increase (P < .001) between pretest (average = 12.12) and post-test (average = 18.85). The OSCE, which also ascertained knowledge retention, found that 81% of students were able to generate all 4 cardiac views perfectly, 6% were able to obtain 3 views, 10% obtained 2 views and 3% successfully generated a single view. The most challenging scan to generate was the apical 4-chamber view.
Conclusion:
The positive outcomes stemming from this study reinforces the notion that formal curricular integration of POCUS at the preclerkship level has tangible benefits for medical students.
Keywords: pre-clerkships, ultrasound, medical education, flipped classroom, clinical transferability
Introduction
The dynamic nature of clinical medicine and the limited resources of a public system continuously challenge graduating physicians. It is thus imperative to equip future health care professionals with tools that will enhance their diagnostic capabilities.1 With its increasing portability and affordability, point-of-care ultrasound (POCUS) is allowing clinicians from a wide array of fields to use it at the bedside.2 This versatility permits real-time bedside imaging of anatomic and pathologic structures, with minimal risks to the patient.3 As such, POCUS has become an inextricable part of critical care and emergency medicine.4,5 Another example of POCUS’ extensive use can be seen in cardiology, where echocardiography is the most frequently employed diagnostic tool and the most resource sparring imaging method.6
Point-of-care ultrasound’s clinical advantages are multifaceted as it reduces costs associated with advanced imaging,7 improves patient care and patient safety8 and reinforces the doctor-patient relationship by increasing face-to-face interactions. Point-of-care ultrasound has also been shown to have tangible pedagogical advantages as it can enhance the teaching of anatomy,9-13 physiology,14-17 and procedural skills.18-22 In the anticipation that POCUS will be used by future physicians as an extension of their physical examination, just like the stethoscope has historically been used, medical educators have started implementing ultrasound curricula in medical schools around the world.1,23-27 In Canada, the University of British Columbia, the University of Calgary, and the Northern Ontario School of Medicine have some form of undergraduate POCUS teaching.28 However, at the time of this study, the University of Ottawa was lacking a formal preclerkship POCUS curriculum.
Most studies reporting on point-of-care cardiac ultrasound (PCCU) have solely concentrated on the training of staff and residents.29 Conversely, studies focusing on PCCU undergraduate training are scarce.29 As preclerkship is a period during which fundamental clinical skills are learned, the introduction of PCCU during this early stage may be very effective for the consolidation and enhancement of the physical exam. Thus, this pilot study sought to evaluate anatomical sonographic knowledge and ultrasound generation capabilities associated with the implementation of a 3-h PCCU training camp led by 2 emergency physicians, using a flipped classroom design. Furthermore, student perceptions about POCUS were explored.
Methods
Written and informed consent was obtained from all participants prior to completion of the pretest/post-test questionnaires, workshop and Objective Structured Clinical Examination (OSCE). Approval was granted from our institutional Office of Research Ethics and Integrity (#H-08-18-941). Participants were not told that the study had a pretest/post-test format as they may have focused more intently on discovering the answers to the questions on the pretest, and this could have inflated post-test scores. Pre- and post-tests were written and reviewed by faculty members with extensive experience in question design for validity.
Recruitment
Thirty-two preclerkship students (23 first years and 9 second years) were recruited via email from the University of Ottawa’s Faculty of Medicine during January 2019. To ensure a basic knowledge of cardiac anatomy and physiology, recruitment was done after the 2 first introductory weeks of the preclerkship first-year cardiac bloc. Inclusion criteria included students at the preclerkship level. Students were excluded (n = 3) if they had any pre-existing ultrasound workshop exposure. As an extracurricular learning experience, no compensation or academic recognition was provided to participants. However, 5 h toward the POCUS Interest Group was offered.
POCUS manual, intervention #1
A peer-written, evidence-based and expert validated POCUS manual was sent to the participants 1 week prior to the workshop, to maximize hands-on scanning during the session. Students were instructed to spend 2 h reading the manual, which included 3 chapters addressing ultrasound fundamentals/knobology, artifacts, and PCCU.
Workshop, intervention #2
Subsequently, students attended a 3-h workshop that focused on the image acquisition of 4 cardiac windows (see Figure 1). The workshop commenced with a 20-min presentation recapping relevant theory. Following this, students were divided into 8 groups of 4, each with their respective ultrasound machine, simulated patient and exam table. Two Emergency department physicians circulated between groups, instructing participants on proper sonographic technique and optimizing the students’ image accuracy and quality. A peer mentoring model was adopted, with a leader having done extracurricular POCUS training being assigned to each group. This allowed for the mobilization of a large group of students with few staff members, who have a scarcity of time.
Figure 1.
Cardiac views that students learned.
Perception pretest
A 5-point Likert-type scale pretest (completely agree, agree, neutral, disagree, completely disagree) with 8 questions (see Table 1) was filled out by students 2 weeks before the workshop on SurveyMonkey (SurveyMonkey, San Mateo, CA, U.S.A.; http://www.surveymonkey.com). The questionnaire was used to assess student perceptions of the ultrasound tool, with subjects pertaining to its clinical usefulness and its perceived role in undergraduate medical education.
Table 1.
Pretest perception questionnaire.
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
|---|---|---|---|---|---|
| 1. I would like to have extracurricular training in ultrasound during my preclinical (year 1-2) years (workshops) | |||||
| Pretest | 0% (0/41) | 0% (0/41) | 0% (0/41) | 19.5% (8/41) | 80.5% (33/41) |
| 2. I would like to see a formal integration of an ultrasound curriculum during my preclinical (year 1-2) years | |||||
| Pretest | 0% (0/41) | 0% (0/41) | 0% (0/41) | 26.8% (11/41) | 73.2% (30/41) |
| 3. My development of ultrasound skills will help my preclinical (year 1-2) education in various fields (physiology, diagnostic capacities, physical exam, etc.) | |||||
| Pretest | 0% (0/41) | 0% (0/41) | 0% (0/41) | 26.8% (11/41) | 73.2% (30/41) |
| 4. My development of ultrasound skills during my preclinical year will further prepare me for my clinical years (year 3-4) | |||||
| Pretest | 2.5% (1/41) | 0% (0/41) | 0% (0/41) | 25.0% (0/41) | 67.5% (0/41) |
| 5. I would benefit from a longitudinal ultrasound training (years 1,2,3,4) regardless of what residency I end up choosing | |||||
| Pretest | 0% (0/41) | 0% (0/41) | 9.8% (0/41) | 24.4% (0/41) | 65.9% (0/41) |
| 6. Having ultrasound training will increase my confidence when attempting to diagnose patients | |||||
| Pretest | 0% (0/41) | 0% (0/41) | 0% (0/41) | 26.8% (11/41) | 73.2% (30/41) |
| 7. Being able to use ultrasound during anatomy sessions will improve my knowledge of anatomical structure identification and spatial orientation | |||||
| Pretest | 0% (0/41) | 0% (0/41) | 7.3% (3/41) | 39.0% (16/41) | 53.7% (22/41) |
| 8. I see ultrasound as an essential part of the PSD classes | |||||
| Pretest | 2.4% (1/41) | 0% (0/41) | 0% (0/41) | 34.2% (14/41) | 63.41% (0/41) |
Abbreviation: PSD, Physician Skills Development.
Sonographic anatomy pretest/post-test
Identical pretests and post-tests comprised of 4 sections containing a total of 21 questions (multiple-choice, short answer, and identification) were used to assess sonographic anatomical identification (See Figure 2 for example). The pretest was administered right before the workshop began, while the post-test was given at the end of the workshop.
Figure 2.
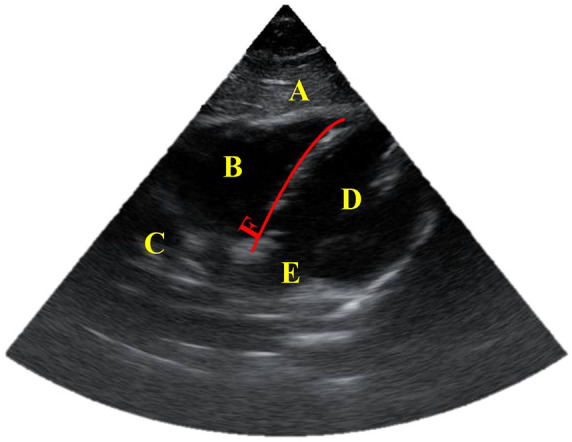
Example of a section of the pretest/post-test of the sonographic anatomy identification.
Window: Subxiphoid.
A: liver, B: right ventricle, C: right atrium, D: left ventricle, E: left atrium, F: septum.
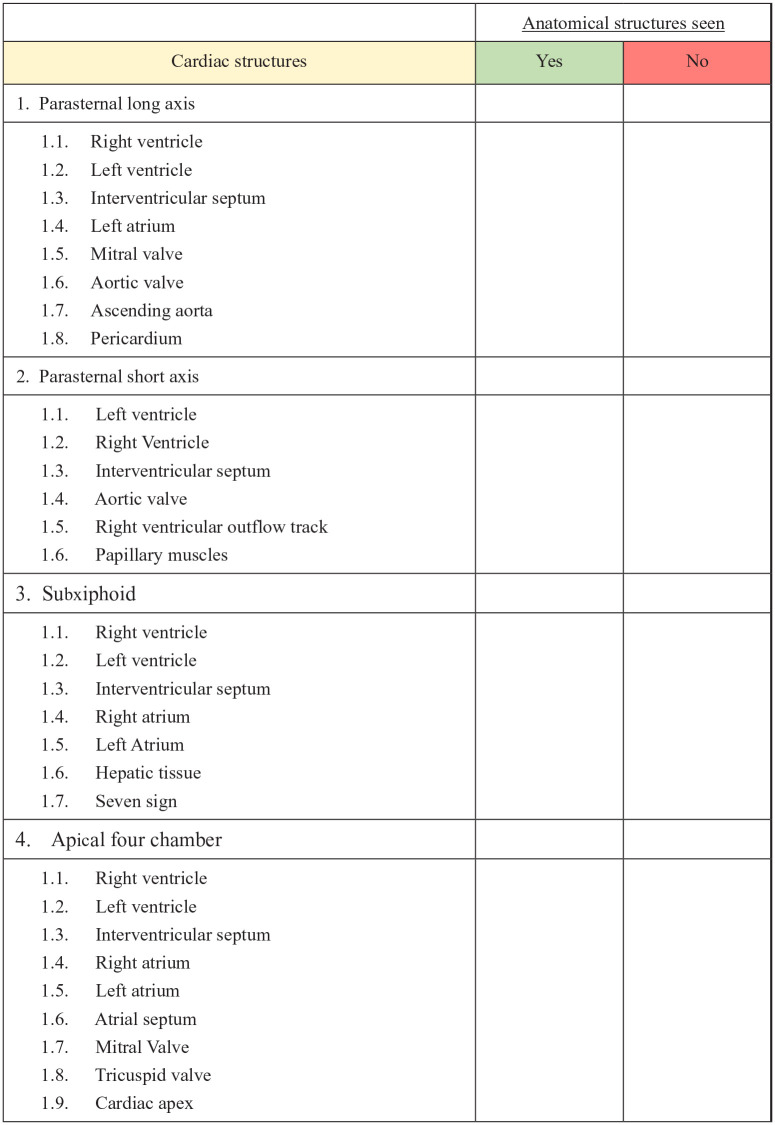
Objective structured clinical examination long-term post-test
To assess the retention of POCUS skills over time, an OSCE was done 3 weeks after the workshop to evaluate the participant’s image generation of all 4 cardiac views, and structural labeling. Each cardiac view was ascertained using a detailed grid outlining specific sonographic structures that had to be visualized to have a successful scan (See Figure 3). A binominal model was used (pass/fail) for each cardiac view. A view was considered successful only if it filled all its respective criteria outlined in Figure 3. The simulated patient was scanned by an emergency physician ahead of time to establish the gold standard for all four cardiac views.
Figure 3.
Objective structured clinical examination checklist.
Data analysis
Collected numerical variables from pre- and post-tests were compared using a t-test and reported as percentages and ratios. A p value < .05 was considered statistically significant. Calculations were carried out using SPSS, version 25. Internal consistency for the Likert-type perception questionnaire was calculated using Cronbach’s alpha.
Results
Perception pretest
A total of 41 students answered the perception pretest (see Table 1). The perception questionnaire was handed out as a pretest (before intervention #2, workshop) to assess ultrasound-naive student perceptions around POCUS and PCCU. Cronbach’s alpha revealed a value of 0.76.
When asked about their desire to see more time allotted to POCUS education in a longitudinal fashion (4 years of undergraduate medical education), 68% reported that they completely agreed, 24% reported that they agreed and 7% were neutral. Conversely, when students were asked about their perceptions toward non-formal extracurricular preclerkship POCUS training, 80% strongly agreed and 10% agreed.
When asked about POCUS’s ability to enhance their performance in clerkship, 67.5% of students completely agreed, 25 % agreed and 2.5% completely disagreed. Finally, when students were asked whether POCUS should be integrated into the Physician Skills Development (PSD) portion of their training, 63% completely agreed, 34% agreed and only 2% disagreed.
Sonographic anatomy pretest/post-test
All 32 first- and second-year medical students demonstrated improvements in their sonographic anatomy interpretation ability after the workshop (intervention #2). There was a statistically significant improvement for the overall score with a mean result of 12.12 for the pretest and 18.85 for the post-test (P < .001). Furthermore, each question had a statistically significant improvement from pretest to post-test scores (see Table 2).
Table 2.
Pretest and post-test mean results for sonographic anatomy.
| Pretest |
Post-test |
|||
|---|---|---|---|---|
| M | SD | M | SD | |
| Section 1 (7 questions) | 3.42 | 2.46 | 6.67 | 0.816 |
| Section 2 (5 questions) | 2.85 | 2.02 | 4.24 | 1.52 |
| Section 3 (4 questions) | 3 | 1.09 | 3.7 | 0.73 |
| Section 4 (5 questions) | 2.88 | 1.96 | 4.38 | 0.94 |
| Total (out of 21) | 12.12 | 5.8 | 18.85 | 3.35 |
OSCE long-term post-test
The OSCE follow-up revealed that 26 students scored 100% (26/32; 81.3%), 2 scored 75% (2/32; 6.3%), 3 scored 50% (3/32; 9.4%), and 1 scored 25% (1/32; 3.1%).
Discussion
Flipped classroom and peer-teaching
A flipped classroom, employing a peer-written, expert validated POCUS manual was used in our study to maximize hands-on learning during the workshop. Furthermore, as students had acquired basic knowledge in knobology, ultrasound artifacts, and PCCU image acquisition/interpretation, minimal faculty members (n = 2) were needed. Moreover, a flipped classroom allowed the experts to concentrate their time on coaching students and refining image generation techniques in lieu of teaching the basics. A flipped classroom in POCUS education has shown to be superior to conventional face-to-face teaching for both immediate and 2 month follow-up results.30 Interestingly, our follow-up OSCE results, with 26 out of 32 students having scored 100%, might be indicative that the flipped classroom played an important role in the student’s knowledge retention.
Our decision to use a peer for the conception of the pedagogic manual and peer-tutors for the workshop revolved around the notion that peer-tutors can more appropriately frame the complexity of their teachings around students’ degree of knowledge when compared to conventional teachers.31-34 The peers were the founders of the University of Ottawa’s POCUS Interest Group and had consequently amassed extensive training from local POCUS experts, conferences, and residents. This approach thus fostered a more comfortable and collaborative environment while efficaciously transmitting information. To our knowledge, the use of a peer-designed manual for a flipped classroom model has not been described for POCUS education.
A flipped classroom offers several advantages when compared to traditional teaching methods. First, this teaching didactic increases accessibility, allowing students to view the relevant theory regardless of location. Second, updating the information as ultrasound technology evolves is relatively simple and can be done in real time. Finally, a flipped classroom standardizes the educational content given to students.35
Perceptions
We decided to evaluate student perceptions exclusively in a pretest manner as we wanted to assess current views on the technology in a POCUS-naïve subset of preclerks. Overall, students reported positive perceptions toward the formal and informal implementation of curricular and extracurricular POCUS training. Similarly, Dinh et al36 evaluated student perceptions using the same Likert-type scale as our study (1, strongly disagree to 5, strongly agree) and found a mean score of 4.6 for POCUS’ perceived importance in medical education and a mean score of 4.44 for POCUS curricular integration into first year of medical school. Likewise, another study showed that students positively viewed POCUS as an enhancement tool in preclerkship years (mean 4.45) while favoring a longitudinal (4 year) approach (mean 4.39).37 As various emergent teaching modalities such as digital resources, e-learning and the flipped classroom model have redefined medical education,37 POCUS has great potential to enhance the preclerkship curriculum, especially when backed by student support and enthusiasm.
Students in our study also perceived POCUS skills as important for their residency and clerkship years. Similarly, a study surveying preclerkship medical students found that 95% of students considered POCUS a valuable teaching tool.15 Also, a recent study reported that 88% of their preclerk controls felt POCUS would be useful to their future careers2 while another study reported that 96% of their preclerk participants expected to learn and use it in their future clinical practice.38 In parallel, a recent national survey has shown an increase in POCUS utilization and training among doctors.39
Image interpretation
Our study showed that preclerkship students were able to significantly improve their PCCU image interpretation abilities after our minimally time-intensive educational interventions. Despite the scarcity in the literature surrounding ultrasound image interpretation evaluation for preclerkship medical students, previous studies, have shown that short amounts of targeted teaching result in the ability of medical trainees to acquire and interpret ultrasound imaging.18,40-43
We decided to initially teach and assess student’s ability at understanding the normal sonographic anatomy. As they we’re all POCUS naïve, this was crucial first step before the challenge of pathological identification. A study evaluating pathological cardiac ultrasound interpretation for first year medical students showed either modest or no improvement after an educational intervention.29 This was probably due to a lack of fundamental knowledge surrounding conventional cardiac anatomy and subsequently sonographic cardiac anatomy,29 reinforcing the notion of the importance of a stepwise approach to PCCU learning.
Image generation
Despite the ongoing debate over POCUS’s scope of use, there is little dispute over its ability to enhance the physical exam.44 The cardiac exam is routinely performed, regardless of the patient’s chief complaint, as it provides clinicians with baseline cardiovascular status of the individual. When indicated, POCUS can therefore provide a more in depth look of the heart in a timely manner, complementing the physical exam. As clinical examination skills are learned and refined during undergraduate medical education, precocious POCUS training in preclerkship may therefore have the most significant impact.
In our study, we demonstrated that preclerkship medical students were able to generate 4 PCCU views after practicing hands-on scans during a 3 h workshop. The use of a peer-leader in every group helped alleviate the need to have several faculty members present. Interestingly, a recent study using a 4-h PCCU lecture coupled with a 4-h hands-on session revealed that peer instructors were superior to staff instructors (cardiologists or diagnostic medical sonographers) at teaching the scanning techniques.45
Another study evaluating the ability of first year medical students to generate 7 cardiac views after an educational intervention showed that they only acquired limited scanning skills. The educational intervention involved 16 hours of training over 8 weeks. This discordance in results might be explained by the fact that our study only required students to generate 4 views. However, the use of a flipped classroom design with a mandatory learning manual in our study might have played a role in increasing our cohort’s ability to focus on scanning techniques when attending the workshop. In line with this, a recent meta-analysis compiling 28 comparative studies revealed that a flipped classroom design was superior to the traditional classroom in health education.46
Studies conducted on preclerkship students have also shown promising results relating to POCUS’ cardiac imaging capabilities in novice hands. For instance, briefly trained preclerks showed an acceptable diagnostic threshold when performing a PCCU, and this when compared with a formal cardiac ultrasound conducted by a cardiologist.47 It has been also shown that the exactness of preclerks students using a handheld ultrasound device after brief echocardiographic training to detect valvular disease, left ventricular dysfunction and hypertrophy was superior to that of seasoned cardiologists performing the physical exam.48 Thus, PCCU teaching during the preclerkship years has been shown to have clinical transferability, reinforcing the notion of curricular integration.
Limitations
Our study had several limitations. Due to the use of a flipped classroom and thus self-directed learning model, the time spent by each student might have differed despite our efforts to standardize invested time by instructing students to spend 2 h studying the manual. While this variation is inherent with the self-directed approach, we did not collect any data quantifying the hours spent reading the manual. As our study involved extracurricular participation, examination results might have been skewed to higher scores due to the participation of a motivated, self-selected group with an interest in POCUS. As such, if the program was part of the formal curriculum, we might have seen relatively lower results as the student body at large might have invested less time and effort studying. The OSCE follow-up demonstrated good 3-week POCUS skills retention but we did not have longer-term follow-up to assess knowledge retention beyond this period. As the medical school preclerkship curriculum is already saturated with content, it would be important to assess the ability of students to retain what they have learned from succinct training. Finally, students were trained and tested on their ability to ascertain normal sonographic anatomy. Even though this stepwise approach is important, an ability to interpret and recognize pathology provides more valuable clinical utility.
The introduction of PCCU for image acquisition and interpretation is feasible at the preclerkship level. Furthermore, PCCU can be taught effectively and succinctly using a flipped classroom model. These positive outcomes reinforce the notion that formal curricular ultrasound education should be integrated from an early stage in medical training.
Footnotes
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project received 5000$ of funding from the Affaires Francophones (Faculty of Medicine, University of Ottawa, Ottawa, Ontario, Canada) in the context of a summer studentship program.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: MK: Contributed significantly to the design, implementation, analysis, interpretation and to the writing of the manuscript.
SF: Contributed significantly to the design, implementation, analysis, interpretation and to the writing of the manuscript.
AJ: Contributed significantly to the design, implementation, analysis, interpretation and to the writing of the manuscript.
NC: Contributed significantly to the design, implementation, and to the writing of the manuscript.
SM: Contributed significantly to the design, implementation, and to the writing of the manuscript.
NY: Contributed significantly to the design, implementation, analysis, interpretation and to the writing of the manuscript.
Ethical Approval: Institutional Review Board approval was obtained for the following study
ORCID iDs: Michel Khoury  https://orcid.org/0000-0003-2062-7428
https://orcid.org/0000-0003-2062-7428
Alireza Jalali  https://orcid.org/0000-0002-0709-9088
https://orcid.org/0000-0002-0709-9088
References
- 1. Afonso N, Amponsah D, Yang J, et al. Adding new tools to the black bag—introduction of ultrasound into the physical diagnosis course. J Gen Intern Med. 2010;25:1248-1252. doi: 10.1007/s11606-010-1451-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. DesJardin JT, Ricceri SK, Brown SD, et al. A Near-Peer Point-of-Care Ultrasound Elective; 2017. https://journals-scholarsportal-info.proxy.bib.uottawa.ca/pdf/10766332/v24i0006/772_anpuefauassl.xml. Accessed July 9, 2019.
- 3. Shankar H, Pagel PS. Potential adverse ultrasound-related biological effects: a critical review. Anesthesiology. 2011;115:1109-1124. doi: 10.1097/ALN.0b013e31822fd1f1. [DOI] [PubMed] [Google Scholar]
- 4. Peterson D, Arntfield RT. Critical care ultrasonography. Emerg Med Clin North Am. 2014;32:907-926. doi: 10.1016/j.emc.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 5. Royse CF, Canty DJ, Faris J, Haji DL, Veltman M, Royse A. Core review: physician-performed ultrasound: the time has come for routine use in acute care medicine. Anesth Analg. 2012;115:1007-1028. doi: 10.1213/ANE.0b013e31826a79c1. [DOI] [PubMed] [Google Scholar]
- 6. Point-of-care ultrasound in medical education—stop listening and look. NEJM. http://www.nejm.org/doi/10.1056/NEJMp1311944. Accessed July 9, 2019. [DOI] [PubMed]
- 7. Van Schaik GWW, Van Schaik KD, Murphy MC. Point-of-care ultrasonography (POCUS) in a community emergency department: an analysis of decision making and cost savings associated with POCUS. J Ultrasound Med. 2019;38:2133-2140. doi: 10.1002/jum.14910. [DOI] [PubMed] [Google Scholar]
- 8. Smallwood N, Dachsel M. Point-of-care ultrasound (POCUS): unnecessary gadgetry or evidence-based medicine? Clin Med. 2018;18:219-224. doi: 10.7861/clinmedicine.18-3-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jurjus RA, Dimorier K, Brown K, et al. Can anatomists teach living anatomy using ultrasound as a teaching tool. Anat Sci Educ. 2014;7:340-349. doi: 10.1002/ase.1417. [DOI] [PubMed] [Google Scholar]
- 10. Stringer MD, Duncan LJ, Samalia L. Using real-time ultrasound to teach living anatomy: an alternative model for large classes. N Z Med J. 2012;125:37-45. [PubMed] [Google Scholar]
- 11. Brown B, Adhikari S, Marx J, Lander L, Todd GL. Introduction of ultrasound into gross anatomy curriculum: perceptions of medical students. J Emerg Med. 2012;43:1098-1102. doi: 10.1016/j.jemermed.2012.01.041. [DOI] [PubMed] [Google Scholar]
- 12. Griksaitis MJ, Sawdon MA, Finn GM. Ultrasound and cadaveric prosections as methods for teaching cardiac anatomy: a comparative study. Anat Sci Educ. 2012;5:20-26. doi: 10.1002/ase.259. [DOI] [PubMed] [Google Scholar]
- 13. Finn GM, Sawdon M, Griksaitis M. The additive effect of teaching undergraduate cardiac anatomy using cadavers and ultrasound echocardiography. Eur J Anat. 2012;16:199-205. [Google Scholar]
- 14. Brunner M, Moeslinger T, Spieckermann PG. Echocardiography for teaching cardiac physiology in practical student courses. Am J Physiol. 1995;268:S2-9. doi: 10.1152/advances.1995.268.6.S2. [DOI] [PubMed] [Google Scholar]
- 15. Bell FE, 3rd, Wilson LB, Hoppmann RA. Using ultrasound to teach medical students cardiac physiology. Adv Physiol Educ. 2015;39:392-396. doi: 10.1152/advan.00123.2015. [DOI] [PubMed] [Google Scholar]
- 16. Paganini M, Rubini A. Chest ultrasound integrated teaching of respiratory system physiology to medical students: a first experience. Adv Physiol Educ. 2015;39:129-130. doi: 10.1152/advan.00084.2014. [DOI] [PubMed] [Google Scholar]
- 17. Paganini M, Rubini A. Ultrasound-based lectures on cardiovascular physiology and reflexes for medical students. Adv Physiol Educ. 2016;40:243-247. doi: 10.1152/advan.00010.2016. [DOI] [PubMed] [Google Scholar]
- 18. Amini R, Stolz LA, Breshears E, et al. Assessment of ultrasound-guided procedures in preclinical years. Intern Emerg Med. 2017;12:1025-1031. doi: 10.1007/s11739-016-1525-4. [DOI] [PubMed] [Google Scholar]
- 19. Brascher A-K, Blunk JA, Bauer K, Feldmann R, Jr, Benrath J. Comprehensive curriculum for phantom-based training of ultrasound-guided intercostal nerve and stellate ganglion blocks. Pain Med. 2014;15:1647-1656. doi: 10.1111/pme.12365. [DOI] [PubMed] [Google Scholar]
- 20. Dunlap PM, Holmberg JM, Whitney SL. Vestibular rehabilitation: advances in peripheral and central vestibular disorders. Curr Opin Neurol. 2019;32:137-144. doi: 10.1097/WCO.0000000000000632. [DOI] [PubMed] [Google Scholar]
- 21. Griswold-Theodorson S, Hannan H, Handly N, et al. Improving patient safety with ultrasonography guidance during internal jugular central venous catheter placement by novice practitioners. Simul Healthc. 2009;4:212-216. doi: 10.1097/SIH.0b013e3181b1b837. [DOI] [PubMed] [Google Scholar]
- 22. Miller R, Ho H, Ng V, et al. Introducing a fresh cadaver model for ultrasound-guided central venous access training in undergraduate medical education. West J Emerg Med. 2016;17:362-366. doi: 10.5811/westjem.2016.3.30069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ivanusic J, Cowie B, Barrington M. Undergraduate student perceptions of the use of ultrasonography in the study of “living anatomy.” Anat Sci Educ. 2010;3:318-322. doi: 10.1002/ase.180. [DOI] [PubMed] [Google Scholar]
- 24. Wicke W, Brugger PC, Firbas W. Teaching ultrasound of the abdomen and the pelvic organs in the medicine curriculum in Vienna. Med Educ. 2003;37:476. [DOI] [PubMed] [Google Scholar]
- 25. Cheng W-C, Lin X-Z, Chen C-Y. Using modern teaching strategies to teach upper abdominal sonography to medical students. J Chin Med Assoc. 2013;76:395-400. doi: 10.1016/j.jcma.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 26. Teichgräber UK, Meyer JM, Poulsen Nautrup C, von Rautenfeld DB. Ultrasound anatomy: a practical teaching system in human gross anatomy. Med Educ. 1996;30:296-298. [DOI] [PubMed] [Google Scholar]
- 27. Hammoudi N, Arangalage D, Boubrit L, et al. Ultrasound-based teaching of cardiac anatomy and physiology to undergraduate medical students. Arch Cardiovasc Dis. 2013;106:487-491. doi: 10.1016/j.acvd.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 28. Steinmetz P, Oleskevich S, Lewis J. Acquisition and long-term retention of bedside ultrasound skills in first-year medical students. J Ultrasound Med. 2016;35:1967-1975. doi: 10.7863/ultra.15.09088. [DOI] [PubMed] [Google Scholar]
- 29. Cawthorn TR, Nickel C, O’Reilly M, et al. Development and evaluation of methodologies for teaching focused cardiac ultrasound skills to medical students. J Am Soc Echocardiogr. 2014;27:302-309. doi: 10.1016/j.echo.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 30. Bashir MDK, Azad MDA, Farook MDKS, et al. Research: emergency medicine residents’ acquisition of point-of-care ultrasound knowledge and their satisfaction with the flipped classroom andragogy. POCUS. 2018;3:2-5. doi: 10.24908/pocus.v3i1.13301. [DOI] [Google Scholar]
- 31. Yu T-C, Wilson NC, Singh PP, Lemanu DP, Hawken SJ, Hill AG. Medical students-as-teachers: a systematic review of peer-assisted teaching during medical school. Adv Med Educ Pract. 2011;2:157-172. doi: 10.2147/AMEP.S14383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tayler N, Hall S, Carr NJ, Stephens JR, Border S. Near peer teaching in medical curricula: integrating student teachers in pathology tutorials. Med Educ Online. 2015;20:27921. doi: 10.3402/meo.v20.27921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hall S, Stephens J, Andrade T, Davids J, Powell M, Border S. Perceptions of junior doctors and undergraduate medical students as anatomy teachers: investigating distance along the near-peer teaching spectrum. Anat Sci Educ. 2014;7:242-247. doi: 10.1002/ase.1419. [DOI] [PubMed] [Google Scholar]
- 34. Nelson AJ, Nelson SV, Linn AMJ, Raw LE, Kildea HB, Tonkin AL. Tomorrow’s educators . . . today? Implementing near-peer teaching for medical students. Med Teach. 2013;35:156-159. doi: 10.3109/0142159X.2012.737961. [DOI] [PubMed] [Google Scholar]
- 35. Heiberg J, Hansen L, Wemmelund K, et al. Point-of-care clinical ultrasound for medical students. Ultrasound Int Open. 2015;1:E58-E66. doi: 10.1055/s-0035-1565173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Dinh VA, Frederick J, Bartos R, Shankel TM, Werner L. Effects of ultrasound implementation on physical examination learning and teaching during the first year of medical education. J Ultrasound Med. 2015;34:43-50. doi: 10.7863/ultra.34.1.43. [DOI] [PubMed] [Google Scholar]
- 37. Rempell JS, Saldana F, DiSalvo D, et al. Pilot point-of-care ultrasound curriculum at Harvard Medical School: early experience. West J Emerg Med. 2016;17:734-740. doi: 10.5811/westjem.2016.8.31387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Larese S, Gorman E, Snyder A, Syverud S. A pilot study: exposing novice medical and nursing students to point-of-care sonography skills. J Diagn Med Sonog. 2012;28:91-94. doi: 10.1177/8756479311434827. [DOI] [Google Scholar]
- 39. Leschyna M, Hatam E, Britton S, et al. Current state of point-of-care ultrasound usage in Canadian emergency departments. Cureus. 2019;11:e4246. doi: 10.7759/cureus.4246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Barsky M, Kushner L, Ansbro M, et al. A feasibility study to determine if minimally trained medical students can identify markers of chronic parasitic infection using bedside ultrasound in rural Tanzania. World J Emerg Med. 2015;6:293-298. doi: 10.5847/wjem.j.1920-8642.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Miner B, Purdy A, Curtis L, et al. Feasibility study of first-year medical students identifying cardiac anatomy using ultrasound in rural Panama. World J Emerg Med. 2015;6:191-195. doi: 10.5847/wjem.j.1920-8642.2015.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wright SA, Bell AL. Enhancement of undergraduate rheumatology teaching through the use of musculoskeletal ultrasound. Rheumatology (Oxford). 2008;47:1564-1566. doi: 10.1093/rheumatology/ken324. [DOI] [PubMed] [Google Scholar]
- 43. García de Casasola Sánchez G, Torres Macho J, Casas Rojo JM, et al. Abdominal ultrasound and medical education. Rev Clin Esp (Barc). 2014;214:131-136. doi: 10.1016/j.rce.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 44. Kimura BJ. Point-of-care cardiac ultrasound techniques in the physical examination: better at the bedside. Heart. 2017;103:987-994. doi: 10.1136/heartjnl-2016-309915. [DOI] [PubMed] [Google Scholar]
- 45. Ben-Sasson A, Lior Y, Krispel J, et al. Peer-teaching cardiac ultrasound among medical students: a real option. PLoS ONE. 2019;14:e0212794. doi: 10.1371/journal.pone.0212794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hew KF, Lo CK. Flipped classroom improves student learning in health professions education: a meta-analysis. BMC Med Educ. 2018;18:1-12. doi: 10.1186/s12909-018-1144-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Filipiak-Strzecka D, John B, Kasprzak J, Michalski B, Lipiec P. Pocket-size echocardiograph: a valuable tool for non-experts or just a portable device for echocardiographers. Adv Med Sci. 2013;58:67-72. doi: 10.2478/v10039-012-0054-2. [DOI] [PubMed] [Google Scholar]
- 48. Kobal SL, Trento L, Baharami S, et al. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. 2005;96:1002-1006. doi: 10.1016/j.amjcard.2005.05.060. [DOI] [PubMed] [Google Scholar]