Abstract
Deciding whether to pursue elective surgery is a complex process for older adults. Comprehensive geriatric assessment (CGA) can help refine estimates of benefits and risks, at times leading to a delay of surgery to optimize surgical readiness. We describe a cohort of geriatric patients who were evaluated in anticipation of elective abdominal surgery and whose procedures were delayed for any reason. Themes behind the reasons for delay are described, and a holistic framework to guide preoperative discussion is suggested.
Consideration of elective abdominal surgery is a process that ideally takes into account medical, physical, cognitive, psychological, logistical, financial, and social factors.1 For older adults, these decisions become more difficult partly because they are less likely to ask questions about surgery.2 Preoperative comprehensive geriatric assessment (CGA) can refine estimates of benefits and risks for older patients and identify opportunities for optimization.3 Guidelines published in 2012 from the American Geriatrics Society and American College of Surgeons National Surgical Quality Improvement Program recommend preoperative evaluation of not only an older adult’s cardiopulmonary health,but also cognition, psychosocial factors, function, and frailty, and discussion of goals and expectations.4 Evidence suggests that CGA leads to specific interventions to optimize health and reduce postoperative complications.5
The advent of preoperative CGA led to the development at Duke University and the Durham Veterans Affairs Health Care System (DVHCS) of the Perioperative Optimization of Senior Health (POSH) program,6 a multidisciplinary program promoting perioperative comanagement between surgery, geriatrics, and anesthesiology. POSH empowers patients to discuss options and form realistic expectations. Moreover, CGA may uncover problems that change the risk–benefit assessment, leading to an intentional delay to optimize surgical readiness.
Little evidence exists to guide decision making surrounding surgery postponement in older adults considering elective abdominal surgery. We present a description of veterans who were evaluated before elective abdominal surgery in the POSH program at the Durham Veterans Affairs Medical Center (DVAMC) (VA-POSH) whose procedures were delayed.
METHODS
Setting, Patients, and Recruitment
The study was reviewed and deemed exempt as non-research by the VA Institutional Review Board, and as such, the requirement for written informed consent was waived. VA-POSH is a model of care built on the interdisciplinary expertise of surgery, anesthesiology, geriatrics, nursing, physical and occupational therapy, chaplaincy, neuropsychiatry, and nutrition. All participants undergo cognitive evaluation using the Saint Louis University Mental Status (SLUMS) examination and depression screening using the Patient Health Questionnaire-9 (PHQ-9) depression scale. The SLUMS is a 30-point, clinician-administered screening for dementia, with a score of 21–26 suggestive of mild neurocognitive disorder, and 1–20 suggestive of dementia; 1 point is added to the patient’s score if they have less than a high school education.7 The PHQ-9 is a 9-item depression questionnaire diagnosing major depression if ≥5 of the 9 depressive symptom criteria have been present “more than half the days” in the past 2 weeks, and one of the symptoms is depressed mood or anhedonia.8 Physical function measures include 30-second chair stands and gait speed. Veterans complete a questionnaire to assess functional status, based on the Older Adults Resources and Services (OARS) Multidimensional Functional Assessment Questionnaire.9 The modified OARS questionnaire used in POSH includes questions about patients’ ability to independently use the telephone, get to places out of walking distance, go shopping, prepare meals, do housework, take medicine, handle finances, eat, groom, bathe, and ambulate. Patients undergo comprehensive preoperative assessment by an interprofessional team. The team reviews expectations and goals, functional status, psychosocial issues, comorbidities, medications, potential need for rehabilitation, and advance directives. A consensus is reached on recommendations for referrals or evaluations before surgery. Perioperatively, geriatricians continue to follow patients in a consultative role, with goals of reducing complications and easing transitions.
For this retrospective case series, we reviewed the records of patients referred to VA-POSH from its inception in July 2015, through July 2017. Because most initial referrals to VA-POSH were for elective abdominal surgery, only these cases were reviewed for this series, although the program has since expanded. Surgeons referred patients over the age of 65 years who they considered to be at risk for a poor outcome for any reason. Referral criteria include >85 years of age, or patients >65 years of age with cognitive impairment (suspected or formally diagnosed), weight loss, multimorbidity, and anticipation of elective surgery.
Data Collection and Analysis
Supplemental Digital Content 1, Figure 1, http://links.lww.com/AA/C882, diagrams how cases were identified. All data were collected from the electronic medical record. Documentation from the surgery clinic appointment, VA-POSH visit, and consultant notes were qualitatively reviewed for content, focusing on the assessment and plan for reasons for surgery delay. After a preliminary reading of the data, 2 independent reviewers (S.P.W., K.M.Z.) developed codes indicating a primary reason for surgical delay, including provider-driven, patient-driven, and logistical reasons. Reviewers then independently coded all cases using this schema. Reviewers agreed on 16 of 18 cases (88.9% simple agreement, κ = 0.78; 95% confidence interval [CI], 0.48–1.00). Disagreements were resolved by consensus after discussion with a third reviewer (S.R.M.). Reviewers then identified themes and subthemes underlying the decision-making process accounting for categories of reasons for delays. Mean or median values were calculated for demographic and clinical variables, and the functional status of patients who underwent delay was compared to those who proceeded for surgery as planned, using the χ2 test for categorical data (SAS, Cary, NC).
RESULTS
During the study period, 428 veterans attended the POSH clinic, 214 of whom were scheduled for elective abdominal surgery. Eighteen (8.4%) of these experienced a delay of surgery. Patient characteristics are shown in Supplemental Digital Content 2, Table 1, http://links.lww.com/AA/C883. Of the delays, 61.1% were provider driven, 22.2% were patient driven, and 16.7% were logistical (Supplemental Digital Content 3, Table 2, http://links.lww.com/ AA/C884). Compared to the patients who proceeded for surgery as planned, patients whose surgery was delayed were approximately the same age (73.5 years for delayed vs 72.2 years for nondelayed) and had a similar SLUMS score (22.9 for delayed vs 23.7 for nondelayed, adjusted for education level). Of note, SLUMS scores were available for all 19 delayed patients but were incomplete or missing for 57 of the nondelayed patients (45%). Differences in impairments in ability to perform activities of daily living (ADLs) or instrumental activities of daily living (IADLs) per the OARS questionnaire were not statistically significant between the 2 groups (64.3% for delayed vs 41.1% for nondelayed, P = .095). The median length of delay, defined as the time between planned surgery date and actual surgery date, was 93 days (interquartile range, 42.3–214.8), and 11 of the 18 patients (61%) returned to VA-POSH for reevaluation. A referral for evaluation of a comorbid condition, or discussion with a specialist already following the patient, occurred in 10 patients (56%).
Qualitative themes explaining the decisions to delay are shown in the Table. Most patients’ delays involved multiple themes. The reasons are heterogeneous, but 6 themes were identified: managing comorbid conditions and frailty, optimizing communication among different parties, addressing psychosocial needs, building decision-making confidence, identifying a preference for nonsurgical management, and working through logistical issues.
Table.
Themes and Subthemes Around Medical and Surgical Decisión Making
| Management of comorbidities (n = 11, 61.1%) | Multimorbidity/frailty |
| Delays were implemented to improve nutritional status or physical conditioning. | |
| Identification of appropriate referrals | |
| Delays provided an opportunity to consult with a specialist for management of a comorbidity. | |
| Communication (n = 6, 33.3%) | Communication with patients and families |
| Several patients expressed significant anxiety before surgery, requesting delays on short notice. | |
| Communication between providers | |
| In some cases, a provider identified an issue that needed further evaluation and communicated concerns to the other providers, necessitating a delay of surgery. | |
| In 4 cases, providers communicated with a patient’s preexisting specialist. | |
| Psychosocial needs (n = 3, 16.7%) | Social stressors |
| In some cases, a social issue (such as an ill family member) caused the delay of surgery. | |
| Family support | |
| Patients often rely on family members for transportation, emotional support, and helping with ADLs and IADLs as they recover. Delays were needed for some patients to secure this support. | |
| Confidence (n = 4, 22.2%) | Confidence for providers and patients |
| Sometimes reevaluation either with imaging or another diagnostic procedure triggered a delay, but provided valuable information contributing to a full risk–benefit profile. | |
| Preference for nonsurgical management (n = 3, 16.7%) | Desire to trial nonsurgical management |
| Three patients preferred to try medical management, either because their symptoms subsided, they had anxiety about surgery, or other events in their lives took priority over having surgery at that particular point in time. | |
| Logistical issue (n = 3, 16.7%) | Need for specialized equipment |
| Two patients had their surgeries delayed so that their care could be transferred to another facility with appropriate equipment. | |
| Transportation | |
| One patient’s surgery was delayed in part due to a lack of transportation to the hospital on the day of surgery. |
Abbreviations: ADL, activities of daily living; IADL, instrumental activities of daily living.
DISCUSSION
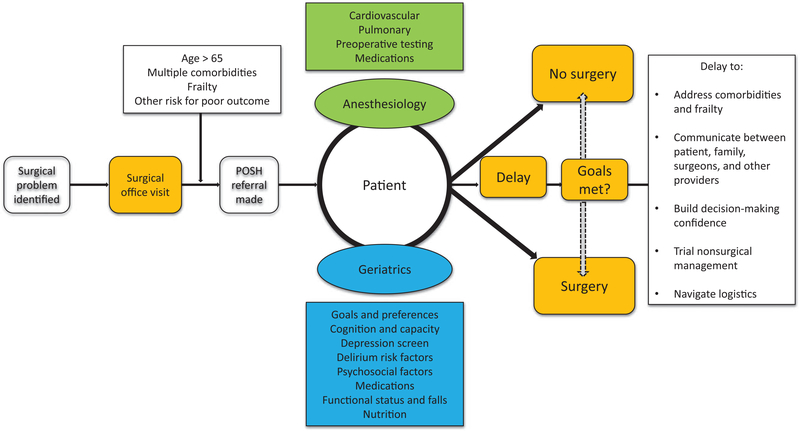
We have described a cohort of 19 veterans assessed in VA-POSH whose surgeries were delayed, with a brief comparison to the cohort of veterans who proceeded to surgery as planned. To our knowledge, this is the first qualitative characterization of older patients, whose surgeries were delayed for preoperative optimization. Although traditional preoperative assessments may have resulted in delay of some of our cohort, we posit that CGA expands discussion beyond usual risk factors. By exploring values and psychosocial factors, the VA-POSH process identified patients requiring further preoperative optimization. Our findings highlight an opportunity to improve the standard of preoperative evaluation, which focuses on formulaic risk assessments. While these remain important, we suggest a holistic perioperative care system, building on our identified themes. A process that provides the opportunity to empower patients to engage in decision making could improve outcomes and better ensure that patients are prepared for surgery. The Figure illustrates the VA-POSH model, including the factors of CGA and themes for delay. This model could be used to guide thought processes, discussion topics, and evaluation of older adults who are contemplating elective surgery.
Figure.
This model describes the framework within which the patients in VA-POSH are evaluated, showing the many issues that may impact a patient’s decision to pursue surgery. It includes the discrete aspects of comprehensive geriatric assessment, as well as the specific themes identified in this case series. POSH indicates perioperative optimization of senior health; VA, Veterans Affairs.
As a next step, we plan to prospectively examine the long-term patient experience with perioperative care, through surveys or structured interviews, with an established postoperative long-term followup period. It would be helpful to compare patients whose surgeries were delayed with patients who went to surgery as planned or whose surgeries were canceled. Comparisons of differences in patient characteristics, factors involved in decision making, and outcomes after surgery could identify opportunities for improvements in risk assessment and optimization. With more structured, objective data, the decision-making factors around surgical delay can be more thoroughly explored.
There are several limitations to this report. First, it was retrospective and utilized the medical record to describe mostly qualitative subject matter. Most clinical documentation provided detailed descriptions of reasons for delay. Some charts, however, had less detail and, as a result, provided an incomplete picture of the thought processes behind the decision for delay. Also, data for key factors like multimorbidity and formal frailty score were unavailable. The VA-POSH assessment workflow should be adjusted to include these critical data in future research. Last, due to the heterogeneity of the patient group, no standard of optimization was possible.
In conclusion, elective surgeries for geriatric patients are postponed for myriad reasons after CGA. We identified 6 themes that explain delays in our cohort, including those that capture physical, social, emotional, and logistical needs. Open communication between transdisciplinary, interprofessional teams, and patients is key. An important focus for future research will be investigating the physical, functional, and psychosocial outcomes of patients who opt to delay surgery.
Supplementary Material
ACKNOWLEDGMENTS
The authors are grateful to Richard Sloane, MPH, (Duke University Medical Center for Aging) and Susan Korucubasi, BSN, MHM, (Durham VA Medical Center) for support with data collection and statistical analysis.
Funding: This study received the Specialty Care Education Center of Excellence Grant from the Office of Academic Affiliations of the US Veterans Health Administration.
GLOSSARY
- ADL
activities of daily living
- CGA
comprehensive geriatric assessment
- DVAMC
Durham Veterans Affairs Medical Center
- DVHCS
Durham Veterans Affairs Health Care System
- IADL
instrumental activities of daily living
- OARS
Older Adults Resources and Services
- PHQ-9
Patient Health Questionnaire-9
- POSH
Perioperative Optimization of Senior Health
- SLUMS
Saint Louis University Mental Status Examination
- VA
Veterans Affairs
Footnotes
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (www.anesthesia-analgesia.org).
Reprints will not be available from the authors.
REFERENCES
- 1.Leeds IL, Efron DT, Lehmann LS. Surgical gatekeeping -modifiable risk factors and ethical decision making.N Engl J Med. 2018;379:389–394. [DOI] [PubMed] [Google Scholar]
- 2.Steffens NM, Tucholka JL, Nabozny MJ, Schmick AE, Brasel KJ, Schwarze ML. Engaging patients, health care professionals, and community members to improve preoperative decision making for older adults facing High-Risk surgery. JAMA Surg. 2016;151:938–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bettelli G. Preoperative evaluation of the elderly surgical patient and anesthesia challenges in the XXI century. Aging Clin Exp Res. 2018;30:229–235. [DOI] [PubMed] [Google Scholar]
- 4.Chow WB, Rosenthal RA, Merkow RP, Ko CY, Esnaola NF; American College of Surgeons National Surgical Quality Improvement Program; American Geriatrics Society. Optimal preoperative assessment of the geriatric surgical patient: a best practices guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society. J Am Coll Surg 2012;215:453–466. [DOI] [PubMed] [Google Scholar]
- 5.Partridge JS, Harari D, Martin FC, Dhesi JK. The impact of pre-operative comprehensive geriatric assessment on postoperative outcomes in older patients undergoing scheduled surgery: a systematic review. Anaesthesia 2014;69(suppl 1:8–16. [DOI] [PubMed] [Google Scholar]
- 6.McDonald SR, Heflin MT, Whitson HE, et al. Association of integrated care coordination with postsurgical outcomes in High-Risk older adults: the Perioperative Optimization of Senior Health (POSH) Initiative. JAMA Surg 2018;153:454–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tariq SH, Tumosa N, Chibnall JT, Perry MH 3rd, Morley JE. Comparison of the Saint Louis University mental status examination and the mini-mental state examination for detecting dementia and mild neurocognitive dis-order–a pilot study. Am J Geriatr Psychiatry 2006;14: 900–910. [DOI] [PubMed] [Google Scholar]
- 8.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fillenbaum GG. Screening the elderly. A brief instrumental activities of daily living measure. J Am Geriatr Soc. 1985;33:698–706. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.