Background:
Parenting stress after preterm birth (PTB) has negative long-term effects on parenting. Research about parental experiences after PTB and on parenting stress in early childhood has focused on mothers.
Purpose:
To compare parenting stress between mothers and fathers 2 to 3 years after PTB and full-term birth (FTB) and to explore their memories about their stress experience, especially after PTB.
Methods:
Fifty-four mothers and fathers in Switzerland whose children were PTB and 65 parents of FTB completed the Parenting Stress Index 2 to 3 years after birth. We compared scores between PTB and FTB and between mothers and fathers. A random subset of parents took part in semistructured interviews that began with photo-elicitation. We analyzed the data thematically. We cross-validated and corroborated qualitative and quantitative findings about parenting stress 2 to 3 years after birth.
Results:
Preterm birth is stressful for parents who cannot take a child's health for granted, but stress experiences after FTB and PTB equalize within 2 to 3 years. Mothers were the primary caregivers and suffered more stress than fathers. For parents with PTB, positive communications from healthcare workers strengthened parental coping in neonatal intensive care unit and after discharge, but parents perceived discharges as early and inconsistent.
Implications for Practice and Research:
Interventions and new models of care improving communication with healthcare professionals, involving parents in infant care as early as possible, increasing staff support to help parents cope better, and optimizing the management of discharge need to be implemented into practice. Their impact on parenting stress on the long term needs to be investigated.
Keywords: fathers, mixed methods, mothers, parenting stress, preterm birth, transition to parenthood
BACKGROUND AND SIGNIFICANCE
Parenthood transforms the family system, affecting parents, the infant–parent relationship, and child development.1 Parent–child relationships begin to develop during pregnancy and strengthen with the first physical contact after birth. In a child's first year, parents must meet the challenges of physical and psychological exhaustion and adaptation, develop their parental roles, and withstand the changes this makes in their relationship.2 Parental role development includes the skills and knowledge parents need to ensure their child survives, cognitive development, and emotional and social growth.3 Belsky4 describes 3 domains of determinants that affect parenting: personal psychological resources; children's characteristics; and contextual sources of stress and support. Parenting stress is understood as the discrepancy between situational demands and personal resources.5
Transition to parenthood is more difficult when a child is premature. Preterm birth (PTB) interrupts mother–child bonding, causing emotional stress in the postpartum period.6 Mothers report guilt over failure to carry infants to term, sadness, helplessness, and worry over the possible loss of their child.7–9 Parents with children admitted to the neonatal intensive care unit (NICU) must cope with many stressors: unfamiliar surroundings; highly technical atmosphere; parental role alterations; the infant's appearance and behaviors; and complete dependence on healthcare providers.10–16 Some studies show that parental stress increases before discharge, persists after and reduces parenting competence and interaction with their child, and negatively influences the child's developmental outcomes.17–24
In addition to the acute stress during hospitalization, PTB can lead to chronic stress in parents, because of their long-term concerns about their child's health and development.23,25–28 However, studies on parental stress 1 to 3 years after birth show contradictory results. Although Treyvaud and Howe et al did not show any differences in the parenting stress between mothers of prematurely born children and term born children at the age of 2 years, Asaka and Takada described significant higher parenting stress in mothers of infants born preterm than in term born children aged 1 to 2 years.29–31 In a longitudinal study, Singer et al23 reported persisting high parenting stress in mothers of high-risk preterm born children at the age of 2 years but similar levels of parenting stress between mothers of low-risk preterm born children and the term control group. Some studies describe factors increasing parental stress after hospital discharge: very low birth weight, low gestational age (GA), higher neonatal medical risk, and lower parental education level.13,23,32,33 Economic insecurity and child outcomes such as lower cognitive test scores, attention deficit/hyperactivity disorder, and psychiatric disorders can further increase parental stress throughout childhood.33–39 Later behavioral and developmental problems were reported because of prolonged parental stress.28,38,40 Huhtala et al28,40 conducted a longitudinal study to discover the association between parental well-being, including parenting stress, and the social, behavioral, and cognitive development of children born preterm. Children whose parents suffered from increased parental stress showed emotional and behavioral problems at the age of 3 and 5 years.28,40 In addition, the longitudinal study by Huhtala et al28,40 shows the impact of fathers' parenting stress on the child's development. Although paternal stress can have a significant influence on the preterm child's development, there is still limited research done with fathers experiencing parenting stress in comparison with mothers after PTB. Some sparse literature shows that mothers and fathers cope and adjust differently after PTB.6,41–43 Understanding both parents' stress experiences after PTB and full-term birth (FTB) could help us identify families' needs and the vulnerable phases where adequate family-centered transitional care interventions to positively influence parenting stress can be provided.
The aim of this study is to compare mothers' and fathers' experience of stress 2 to 3 years after PTB and FTB with focus on parents after PTB. We set out to qualitatively describe and compare stress experiences of mothers and fathers after PTB and FTB, throughout the transition to parenthood, up to 2 to 3 years after birth. Based on theoretical considerations, we explored whether gender and PTB affect stress experience.
What This Study Adds
Explores stress experience among mothers and fathers after preterm birth in comparison with parent's experience after full-term birth during children's first 2 to 3 years.
Identifies ways that help or hinder parents recovering from the stress experiences after preterm birth.
Opens discussion about the implementation and evaluation of new models to optimize transitional care after preterm birth.
METHODS
Design
We used a concurrent confirmatory mixed-methods design with a dominant qualitative component and a less dominant quantitative component. We collected qualitative and quantitative data in semistructured interviews based on photo-elicitation and self-reported questionnaires.44,45 We analyzed data sets separately and cross-validated and confirmed our interpretations of qualitative with quantitative findings on parents' experiences of stress 2 to 3 years after birth.
Sample
In 2009, for the quantitative segment of the study, we recruited a convenience sample of families (mother and father) with FTB and families with PTB from 3 Swiss cantons (federal states of the Swiss confederation). Like a previous study that used the Parenting Stress Index (PSI), we determined adequate sample size with a power analysis.46 If we recruited 63 families in each group (parents after PTB and FTB), this would give us a statistical power of 0.80 (α= .05; one tailed). Inclusion criteria were as follows: (a) children born between January and December 2009 in one of the three Swiss Cantons; (b) parents understood, spoke, and wrote in German; (c) children's GA was ≥370/7 weeks for FTB and between 240/7 and 320/7 weeks for PTB; and (d) parents gave informed consent. For the qualitative segment, we selected a purposive subsample of parents in each group to ensure diversity in age, income, and multiple versus single births, and included parents whose children were hospitalized for at least 2 days after birth, could provide photographs of the child in their first days of life, and who gave informed consent. We excluded parents whose child died after birth. Each of the 3 Swiss cantons granted us ethical approval.
We collected data between September 2011 and February 2012. Consenting mothers and fathers were mailed PSI and family demographic questionnaires and asked to complete them separately. Then, a trained student or the first or last author interviewed parents separately in their homes.
Photographs of the newborn were used to elicit discussion in semistructured interviews. Photo-elicitation interviewing is widely used in sociological and anthropological research. This approach is based on integrating a photograph into a research interview. The difference to an interview using questions only is that images trigger deeper elements of human consciousness, lead to a different kind of information, and induce emotions and memories during interviews. Photo-elicitation may connect an individual to experiences in the past.45 Interviews lasted between 35 and 108 minutes and focused on birth, hospitalization, and transition to parenthood, guided by open-ended questions. The interview started with the question: “Can you tell me how you experienced the time around the birth of your child?” Example questions were as follows: “What happened at birth?” “How did you experience your child in the first years of his life?” “What behaviors pleased you about your child?” “What behaviors about your child did you experience as challenging?”
Instruments
We collected the following Family Demographic Information about parents via questionnaire: sex, age, marital status, nationality, native language, occupation, educational level, yearly family income, number, and age of children. For children born in 2009, we requested their sex, GA at birth, date of birth, mode of delivery, single or multiple birth, birth weight, birth length, and length of hospitalization.
Parenting Stress Index47 assesses parental stress perceptions with 101 items rated from 1 to 5 on a Likert scale (1 = strongly disagree to 5 = strongly agree). The parent domain measures 7 dimensions: attachment, depression, role restriction, health, sense of competence, social isolation, and spousal/partner support. The Child Domain has 6 dimensions: adaptability, acceptability, distractibility–hyperactivity, mood, demandingness, and “reinforces parent.” Higher scores indicate greater parenting stress. Total score and scores in the 2 domains ≥ 85th percentiles are considered clinically significant. Parenting Stress Index was standardized for parents whose children were 1 month to 12 years of age and validated with parents who had PTB. The PSI is written at a fifth-grade reading level and takes 20 minutes to complete. We used the German version of Hofecker Fallahpour et al.48 Internal consistency for total parenting stress score had a Cronbach α coefficient of 0.92.
Statistical Analysis and Procedures
Qualitative Data
Interviews were audio-recorded and transcribed verbatim. Transcriptions were anonymized and checked for errors. We analyzed the interviews semantically by using an inductive approach of thematic analysis described by Braun and Clarke.49 Thematic analysis is a flexible method and identifies repeated patterns strongly linked to the data itself. First, we familiarized ourselves with topics and patterns by reading the transcript repeatedly and noting first ideas. Second, we extracted descriptions of experiences and patterns referring to the research questions and created our first codes. Third, we sorted these codes into themes, rechecked the themes against the extracts we coded, and generated a thematic map. A peer group of nursing scientists consisted of the first and last authors, a qualitative expert senior researcher, and 2 students in nursing science. The group engaged in an iterative process of content analysis, code, and theme generation. Each interview was coded by 2 group members independently. At the end of the analysis process, we performed short (30 minutes) member checking interviews with a random sample of 3 parents after PTB (2 mothers, 1 father) to reach participant agreement and confirm credibility of the results. We distributed a summary of the themes emerged during analysis to the 3 participants of the member checking, discussed the themes, and incorporated comments into the final analysis.
Quantitative Data
Double-entry procedures produced less than 0.5% error rates. Descriptive statistics, including mean, standard deviation, frequencies, and cross tabulations, described all variables and uncovered data anomalies (eg, outliers, extreme values, influential cases, nonrandom missing data patterns, and parametric method invalidating nonstandard conditions) that influenced the inferential statistics. Q-Q-Plots verified normal data distribution. We used computed hierarchical linear models to test differences in gender and PTB in total PSI, the 7-dimension parent domain, and the 6-dimension child domain. Hierarchical linear models helped us account for the clustering effect of parents of the same child by defining the variable “family” as random effect and including explanatory binary variables “group” (preterm or full-term) and “sex” (mother or father) as fixed effects. Statistical significance was set at P < .05 for all analyses.
RESULTS
Of 65 families (63 mothers, 45 fathers) recruited for the PTB group, 54 (83%) returned the questionnaire; of 76 families (76 mothers, 59 fathers) recruited for the FTB group, 65 (86 %) returned the questionnaire. The total sample for final quantitative analysis was N = 190 (113 mothers; 77 fathers). We excluded parents after consent for (a) no response (n = 43), (b) no time (n = 6), (c) no interest (n = 2), and (d) language problems (n = 2). We compare sample characteristics of the groups in Table 1.
TABLE 1. Sample Characteristics of the Total Sample of Parents With Preterm and Full-Term Childrena.
| Characteristics | Preterm Group | Full-Term Group | ||||
|---|---|---|---|---|---|---|
| n (%) | M (SD) | Range | n (%) | M (SD) | Range | |
| Parent sex | 85 | 105 | ||||
| Mothers | 52 (61.2) | 61 (58.1) | ||||
| Fathers | 33 (38.8) | 44 (41.9) | ||||
| Age of mothers, yb | 52 | 34.58 (5.20) | 25-47 | 61 | 36.67 (5.10) | 24-48 |
| Age of fathers, y | 33 | 38.06 (8.00) | 27-57 | 44 | 38.86 (5.86) | 28-56 |
| Total number of children | 54 | 2.07 (1.06) | 1-5 | 65 | 1.87 (0.95) | 1-6 |
| Gestational age at birth, wkb | 53 | 29.26 (1.80) | 25-32 | 63 | 40.04 (1.23) | 37-42 |
| Birth weight, gb | 54 | 1249.26 (390.42) | 580-2080 | 61 | 3462.2 (435.11) | 2100-4300 |
| Birth length, cmb | 54 | 37.94 (4.16) | 30-47 | 61 | 50.16 (2.08) | 44-56 |
| Hospital stay, db | 54 | 56.44 (23.16) | 14-110 | 60 | 3.72 (1.98) | 0-8 |
| Child's sex | 52 | 65 | ||||
| Female | 30 (57.7) | 33 (50.8) | ||||
| Male | 22 (42.3) | 32 (49.2) | ||||
| Marital status | 54 | 64 | ||||
| Married/living together | 51 (94.4) | 63 (98.4) | ||||
| Separated/divorced | 3 (5.6) | 1 (1.6) | ||||
| Yearly family income | 48 | 64 | ||||
| <80 000 Swiss francsc | 18 (37.5) | 12 (18.8) | ||||
| >80 000 Swiss francsc | 30 (62.5) | 52 (81.3) | ||||
| Single/multiple birthb | 54 | 65 | ||||
| Single birth | 42 (77.8) | 65 (100.0) | ||||
| Multiple birth | 12 (22.3) | 0 (0.0) | ||||
| Method of deliveryb | 54 | 64 | ||||
| Planned cesarean delivery | 8 (14.8) | 9 (14.1) | ||||
| Unplanned cesarean delivery | 42 (77.8) | 7 (10.9) | ||||
| Vaginal delivery | 4 (7.4) | 48 (75.0) | ||||
| Mothersb, n (%) | Fathersb, n (%) | Mothersb, n (%) | Fathersb, n (%) | |||
| Highest degree of education | ||||||
| Elementary school | 1 (1.9) | 2 (6.1) | 0 (0.0) | 0 (0.0) | ||
| High school | 1 (1.9) | 1 (3.0) | 3 (4.9) | 1 (2.3) | ||
| Apprenticeship | 28 (53.8) | 8 (24.2) | 13 (21.3) | 4 (9.1) | ||
| Higher technical school | 13 (25.0) | 16 (48.5) | 15 (24.6) | 9 (20.5) | ||
| University | 9 (17.3) | 6 (18.2) | 30 (49.2) | 30 (68.2) | ||
| Mothersb, n (%) | Fathers, n (%) | Mothersb, n (%) | Fathers, n (%) | |||
| Employment status | ||||||
| Full time | 3 (5.8) | 22 (66.7) | 6 (9.8) | 27 (61.4) | ||
| Part time | 31 (59.6) | 11 (33.3) | 47 (77.0) | 17 (38.6) | ||
| Not employed | 18 (34.6) | 0 (0.0) | 8 (13.1) | 0 (0.0) | ||
aTable with sample characteristics from the total sample of parents with preterm and full-term children. n varies because of missing values. Percentage may not add to 100% because of rounding. Superscript letter (b) appears only in items for which significant differences were observed between preterm and term groups.
bP < .05 (univariate analysis or χ2 test).
cUS$ = 0.97 Swiss francs (exchange rate at the time of study).
As expected, given our definitions of prematurity and FTB, preterm infants had lower GAs at birth than FTB infants, weighed less, were shorter in length, had longer initial hospital stays, and were likelier to be multiple births. Mothers with PTB were significantly younger and had fewer vaginal deliveries. Of 65 eligible parents who gave consent to participate in the interviews, a subsample of n = 18 in the FTB group (9 mothers; 9 fathers) and n = 20 parents in the PTB group (10 fathers; 10 mothers) participated in semistructured interviews. With a total subsample of n = 38, data saturation was achieved: data showed redundancy or repetition. Demographic characteristics of the interview subsample were the same as for the total sample (see Table 2). Although the FTB group included only singleton births, the PTB group included 1 quadruplet, 1 triplet, 2 twins, and 6 singleton births.
TABLE 2. Sample Characteristics of the Qualitative Subsample of Parents With Preterm and Full-Term Childrena.
| Characteristics | Preterm Group | Full-Term Group | ||||||
|---|---|---|---|---|---|---|---|---|
| n (%) | M | SD | Range | n (%) | M | SD | Range | |
| Age of mothers, y | 10 | 36.1 | 6.350 | 28-47 | 9 | 37.56 | 6.521 | 30-47 |
| Age of fathers, y | 10 | 34.9 | 9.049 | 27-52 | 9 | 40.22 | 7.446 | 32-50 |
| Total number of childrenb | 17 | 2.1 | 1.197 | 1-4 | 9 | 2.09 | 1.483 | 1-6 |
| Gestational age at birth, wkb | 17 | 28.77 | 2.127 | 25-31 | 9 | 40.05 | 1.225 | 38-42 |
| Birth weight, gb | 17 | 1150 | 333.766 | 700-1650 | 9 | 3421 | 556.524 | 2515-4270 |
| Hospital stay, db | 17 | 61.1 | 26.15 | 30-110 | 9 | 3.11 | 1.691 | 1-5 |
| Marital status | 10 | 9 | ||||||
| Married/living together | 9 (90) | 9 (100) | ||||||
| Separated/divorced | 1 (10) | 0 (0) | ||||||
aComparison of the sample characteristics of the qualitative subsample between parents with preterm and full-term children.
bItems for which significant differences were observed between preterm and term groups. P < .05 (univariate analysis or χ2 test).
Parental Experiences Within Their Child's First 2 to 3 Years
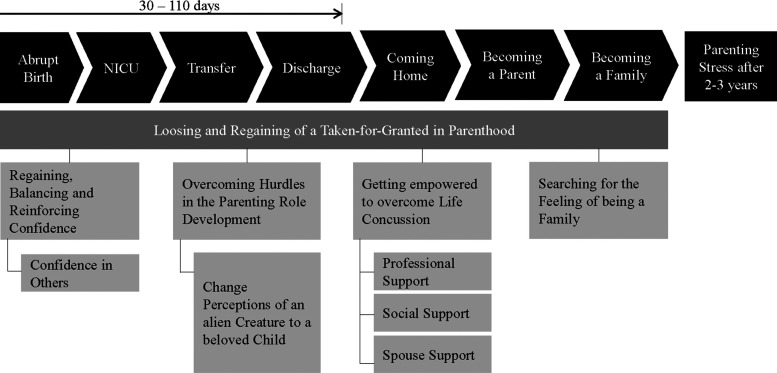
Parents of preterm and full-term infants described their transition to parenthood differently. We compared the groups, but our analysis focused on the perceptions of parents in the PTB group, who described periods of vulnerability to stress, including the abrupt birth, NICU and transfers to other wards, discharge, and first months at home. During this time, they suffered serious strain and emotional work (see Figure 1). One experience predominated: the loss and recovery of taking for granted that they were handling a healthy child. We defined taking for granted as the unselfconscious presumption that a child is healthy.
FIGURE 1.
Vulnerable phases and emotional work done by parents after preterm birth. NICU indicates neonatal intensive care unit.
Loss and Recovery of Taking for Granted in Parenthood
Most parents in the PTB group described birth as unexpected and said that it destabilized their personal and family systems. They were alienated from the intimate world, from the child, and the expected role as parent—a loss of taking for granted a child's health. Mothers described loss of control and distance from their child during the hectic and overwhelming birth event: “Everything went extremely fast .... Despite suddenly becoming mother of my second child, I didn't have this child—that was the worst.” Fathers felt abandoned—some could not be present, arrived late at birth, or were forgotten somewhere between the ward and the operating room—and thrust into a situation that did not seem real. After their preterm infant was born and had been stabilized, most fathers saw the infant alone: “I was the only one allowed to see my child ... alone in this room, surrounded by all these children. What a dramatic beginning experience.” These fathers felt isolated and helpless in alienation. Even when parents of healthy full-term infants found themselves in unexpected situations during birth (eg, instrument-assisted vaginal delivery), they expected healthy infants. They said that they were included in decision making, not separated from their child, and could take for granted their transition to parenthood.
Regaining, Balancing, and Reinforcing Confidence
After PTB and their infant's hospitalization at NICU, parents faced a period of uncertainty; conditions might worsen, or they might lose their child. Referrals to other wards or hospitals challenged most parents in the PTB group. Adapting to hospital conditions and relying on others' judgment and competence to protect their child's well-being damaged their confidence; it was fragile and needed reinforcement. For parents after PTB, this time after birth through transition to parenthood was characterized by growing confidence. Some parents in the PTB group felt mistrust at leaving their child alone in the hospital. Their ability to rebuild their confidence depended on their personalities and preexisting confidence in others. A basic sense of trust—believing everything happening for a reason—helped parents (especially mothers) maintain optimism and overcome uncertainty.
Parents in the PTB group described discharge as another major challenge; most felt that it was disorganized and too soon. They reported feeling overwhelmed, afraid, and unprepared to assume upcoming responsibilities but also felt happiness and relief at finally going home, where their first weeks were characterized by constant child monitoring and insecurity.
Confidence in Others
Growing confidence included confidence in the child's strength and desire to survive, professionals who provided care, and medical advances or the setting. Parents who trusted their child's strength and willingness to survive had greater hope of their child's survival. Parents of 2 extremely low birth-weight infants said that this proved invaluable to their decision-making process when offered lifesaving interventions. The child's survival reinforced each parent's confidence in his or her child's strength during the transition from hospital to home. These 2 parents were much less worried about the child's health at home:
We felt that he [the child] wanted to live. He is a fighter, and we have to give him this chance... and he proved he wanted to live. We were convinced our son wouldn't have fought for the last three months in the hospital if now he comes home and something negative would happen.
When a child was in NICU, parents were bound to the medical environment and care from health professionals. Most mothers were distressed by the lack of privacy at NICU, but as they adapted, and their confidence rebound, these concerns decreased for some. Fathers focused mainly on the technical environment and were concerned through monitor alarms. Seeing their child in the incubator surrounded by technical devices frightened, and fathers felt insecure and overstrained.
Overcoming Hurdles in Parenting Role Development
Parental role development is a process of attachment during which parents learn to recognize and satisfy a child's needs. After FTB, parents, supported by healthcare professionals learned to care for their child within a week and took full responsible for their child from the beginning. After PTB, the parenting role developed intermittently at NICU and after discharge. In NICU, some mothers felt like their child belonged to the healthcare professionals, with whom they shared care duties. Being involved in caretaking helped them overcome those feelings. Most parents took more responsibility for childcare after their infant left the incubator. Postdischarge, parents in the PTB group were most challenged by their child's nutritional problems and sleep patterns and their own physical and psychological exhaustion. One father developed abdominal disorders after the child's discharge; others described intense tiredness or negative feelings during the child's hospitalization. One father said that it was “like being in a bob run ... there was no way back, it just went down.” (Bob run is an icy track to run with a special sleigh). They describe bottle-feeding as time-consuming and parents felt pressured to ensure that their underweight child got enough to eat.
Changing Perceptions: From an Alien Creature to a Beloved Child
Parents in the PTB group experienced attachment differently than parents in the FTB group. The FTB parents cuddled their infants and shared joy with their partner, but PTB parents were separated from their infant for hours, which could make them feel alienated. One mother said, “She was under a plastic sheet and I could barely see her. I didn't feel this was my child. It was just a child in an incubator.” Seeing this tiny infant, who sometimes looked strange to them, overwhelmed fathers. For all parents, beginning skin-to-skin care was a turning point. A mother said, “On the fourth day we started skin-to-skin care. This was an extremely emotional experience. At this moment, for the first time I felt, this is my child. This was just beyond words.” Most mothers and fathers described skin-to-skin care as the only way to feel close to an infant in the incubator. The attachment process advanced when the child left the incubator and parents gained more opportunities for care. All parents felt that it was important to make time to build a relationship with their child. Some parents found daily visits to NICU after PTB taxing, especially if they had other children. All mothers spent several hours a day with their child. After FTB, fathers planned time off from work. Since Switzerland has no paternity leave laws, fathers balanced work and NICU post-PTB, a situation that exhausted them. After their child came home, they took days off to help them adapt to having the infant at home and deepen father–child relationships. Parents in the FTB group described their attachment to their child as deepening relationship over time. One mother said, “I realized the relationship to my child grew over the last 3 years.” The PTB parents perceived the process as interrupted and initially challenging but by the time the child reached 2–3 years, their descriptions of the relationship matched those of parents after FTB. The father of preterm twins spoke of his growing love: “...although sometimes they were difficult, today I can say I deeply love these two boys.”
Overcoming Life's Jolts Through Self-Empowerment
Although both groups described supportive elements in transition to parenthood, parents after PTB more often described elements that hindered them. The demeanor of professionals (eg, nurses, midwives, physicians, pastoral carers, breastfeeding consultants) or social attitudes (eg, families, close friends, other acquaintances, and partner/spouse) could be positive or negative.
Professional Support
Parents after PTB often talked about the ways professionals communicated and involved them in their child's care during hospitalization. They needed healthcare providers to explain their child's condition honestly, but they felt that most communication emphasized risks and dangers. The mother of a child born at 25 weeks' GA, “Although everything went well with my son, they [...] told us: don't be too optimistic. [...] There could still be a [...] crisis. But crisis never came.”
All parents wanted to visit their children freely and help care for them. Mothers were eager to assume care responsibilities while fathers waited for an invitation. As parents became better at assessing infant needs, they craved affirmation from healthcare providers. Most parents with a primary nurse felt that it gave them an advantage to be able to deepen that relationship over time. Pastoral carers and breastfeeding consultants could also be helpful. No parent accepted psychological support, even when it was offered during their child's hospitalization, but 2 fathers mentioned that they now thought they needed it.
All parents had lengthy discharge conversations with physicians and nurses; most expressed uncertainty and concerns about discharge and taking sole responsibility for their child. The first days at home exhausted them. One father said, “Somebody looked after you for the past three months and suddenly you are alone .... It was especially challenging, when (she) ... was asleep. I couldn't sleep anymore, because I had to check her all the time.” Most parents in the PTB group were supported by a midwife or breastfeeding consultant for the first 2 weeks at home and found it helpful. Parents were told to contact the community family health nurse or their pediatrician if problems arose and they described their pediatrician as especially supportive. Checkups that focused on their child's deficits rather than their own needs frustrated them, while focusing on the child's developmental improvements empowered them. A mother said, “I felt follow-up examinations were about their interests instead of supporting us parents. [...] The physician emphasized only my son's inability to lift his head for a certain time.”
Social Support
Family and friends get involved after a child's birth. After FTB, parents proudly announced the birth and introduced the newcomer, while parents after PTB witnessed that friends and family also go through the cycle of loss and recovery, the feeling of taking a child's health for granted. The process included shock at the early birth, inability to see the infant, child development concerns, and concern for the parents' physical and mental health as they adapted to normal life over time. Mothers and fathers were exhausted by the responsibility of informing and comforting network members while needing comfort and hope themselves.
Partner Support
Partner support during transition to parenthood was described as essential after all births. Mothers more often explained how they got support, while fathers explained how they helped. Most parents reported that a stable and respectful relationship helped them better understand each other after the birth. Almost all fathers took several weeks off when mother and child were discharged after FTB. They did household chores, cared for older children, and helped care for the newborn. After PTB, parents said that their ability to discuss concerns and feelings and make necessary decisions (eg, withdrawing therapies, breastfeeding versus nonbreastfeeding, or whether they want to show pictures of their preterm infant to friends) during the child's hospitalization was paramount. After discharge, most PTB fathers supported partners by responsibilities equally. Almost all parents of preterm children described their partner relationship as deeper and more faithful after transition to parenthood.
Searching for the Feeling of Being a Family
All parents of full-term children described the unique moment of happiness and the feeling of being a family immediately after birth when they held their newborn. Parents with preterm children did not have this feeling and described it as an eternal loss: “We never got this unique happiness after birth .... This moment will always lack in our lives.” After PTB, most parents did not feel like a family until the child's discharge. Parents with older children tried to integrate them during NICU hospitalization, but meeting children's different needs proved challenging. All parents described becoming a family as an adaptation process in which every member finds his or her new role.
Parenting Stress 2 to 3 Years After Birth
Despite a difficult transition, parents in the PTB group and parents in the FBT group described similar challenges 2 to 3 years later. The child became integral to the family and enriched his or her parents' lives. Parents were most stressed by the toddler's demanding behaviors and by balancing work and family. When both parents worked, they had to keep strict schedules, including meeting responsibilities to children, household, and family time. Although most mothers worked part-time and spent more time with their children, fathers were involved as much as possible, which was important for them to maintain a strong bond but challenging. Working mothers described their life as a balance between work and family.
Comparison of Parenting Stress Scores
The total sample to compare Parenting Stress Scores was N = 190 (113 mothers; 77 fathers). Mean Total Parenting Stress scores, parent and child domain scores, and scores of all dimensions are presented in Table 3. Fixed effects of Total Parenting Stress Scores, scores in the 2 domains, and the significant differences of scores in dimensions are shown in Table 4. Mean Total Parenting Stress scores were the same for the PTB and FTB groups (F1,101.32 = 0.63; P = .430) and for mothers and fathers (F1,71.43 = 0.62; P = .435). In the parent domain, mean scores did not differ between the PTB and FTB groups (F1,102.46 = 0.28; P = .598), but for mothers in both groups scores averaged 4.66 higher than for fathers (F1,73.74 = 4.21, P = .044); mean scores in the child domain did not differ between groups (F1,101.73 = 0.77; P = .384) or between mothers and fathers (F1,74.58 = 0.93; P = .337). In 13 dimensions, we found no differences between parents with PTB and FTB. In 3 dimensions of the parent domain (depression, health, and spousal/partner support), mean scores differed between mothers and fathers; fathers had 2.2 lower averaged scores than mothers for depression (F1,83.76 = 11.52; P = .001), 0.62 lower averaged scores for health (F1,89.67 = 4.14; P = .045), and 1.57 lower averaged score for spousal/partner support (F1,72.72 = 10.34; P = .002). In the child domain, acceptability differed between fathers and mothers: fathers had 0.91 higher averaged scores than mothers (F1,83.86 = 7.64; P = .007).
TABLE 3. Mean Parenting Stress Scores of Mothers and Fathers of Preterm and Full-Term Childrena.
| PSI Variables | Preterm Group | Term Group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mothers (n = 50) | Fathers (n = 32) | Mothers (n = 60) | Fathers (n = 43) | |||||||||
| M | SD | Range | M | SD | Range | M | SD | Range | M | SD | Range | |
| Total PSI | 226.86 | 38.43 | 139-340 | 214.94 | 27.43 | 162-260 | 220.65 | 35.49 | 141-304 | 219.3 | 32.95 | 146-277 |
| Parent domainb | 132.28 | 23.40 | 73-200 | 123 | 16.55 | 93-163 | 130.17 | 19.85 | 80-179 | 125.81 | 18.07 | 86-159 |
| Child domainc | 94.00 | 18.69 | 66-147 | 91.94 | 14.41 | 67-123 | 90.44 | 17.89 | 61-131 | 93.49 | 18.24 | 60-137 |
| Distractibility/hyperactivity | 24.34 | 5.02 | 15-35 | 23.34 | 4.10 | 13-32 | 23.43 | 4.97 | 13-37 | 23.42 | 4.76 | 14-34 |
| Adaptability | 22.32 | 5.63 | 14-39 | 21.53 | 3.84 | 14-30 | 21.13 | 5.08 | 12-35 | 22.21 | 4.99 | 13-34 |
| Reinforces parent | 11.48 | 1.97 | 8-16 | 11.44 | 1.56 | 9-15 | 11.33 | 1.74 | 6-16 | 11.44 | 2.00 | 8-16 |
| Demandingness | 17.56 | 5.26 | 9-34 | 16.47 | 3.32 | 10-23 | 16.42 | 5.09 | 9-31 | 16.56 | 5.18 | 9-32 |
| Mood | 8.72 | 2.92 | 5-18 | 8.84 | 2.58 | 5-14 | 8.72 | 2.81 | 5-17 | 8.91 | 2.76 | 5-18 |
| Acceptabilityb | 10.16 | 3.05 | 7-18 | 10.31 | 3.30 | 7-18 | 9.45 | 2.84 | 7-17 | 10.95 | 3.39 | 7-23 |
| Competence | 36.02 | 4.88 | 22-50 | 34.13 | 3.50 | 27-43 | 35.50 | 4.40 | 27-47 | 35.67 | 4.59 | 26-43 |
| Isolation | 14.28 | 3.12 | 9-21 | 14.63 | 2.67 | 10-20 | 14.35 | 3.45 | 6-23 | 14.79 | 3.14 | 9-22 |
| Attachment | 13.98 | 2.83 | 7-22 | 14.44 | 2.72 | 10-20 | 13.25 | 2.52 | 7-21 | 13.91 | 2.56 | 7-21 |
| Healthb | 14.16 | 2.17 | 9-23 | 13.25 | 2.11 | 9-19 | 14.17 | 2.21 | 9-19 | 13.77 | 1.66 | 10-17 |
| Role restriction | 17.46 | 6.26 | 7-33 | 16.25 | 4.91 | 7-28 | 17.42 | 4.64 | 8-29 | 15.95 | 3.77 | 9-24 |
| Depressionb | 18.14 | 5.76 | 9-30 | 14.72 | 4.48 | 9-26 | 17.47 | 5.42 | 9-35 | 15.6 | 4.84 | 9-28 |
| Spouseb | 18.24 | 5.49 | 7-30 | 15.59 | 3.57 | 7-24 | 18.02 | 4.74 | 7-28 | 16.12 | 3.97 | 8-25 |
Abbreviation: PSI, Parenting Stress Index.
aComparison of parenting stress scores between mothers and fathers of preterm and full-term children.
bItems for which significant differences were observed between mothers and fathers in preterm and full-term groups.
cn = 52, n = 61, respectively.
TABLE 4. Fixed-Effects Parenting Stress Scores: Total Parenting Stress Index, Domains, and Significant Dimensionsa.
| Outcome Variable | Parameter | b | SEb | df | t | P | 95% CI |
|---|---|---|---|---|---|---|---|
| Total Parenting Stress Scores | Intercept | 223.85 | 6.72 | 146.39 | 33.32 | .000 | 210.57-237.13 |
| Preterm | 4.80 | 6.05 | 101.32 | 0.79 | .430 | −7.20 to 16.79 | |
| Sex: Father | −3.03 | 3.86 | 71.43 | −0.79 | .435 | −10.72 to 4.66 | |
| Score Parent Domain | Intercept | 134.64 | 3.92 | 144.75 | 34.34 | .000 | 126.89-142.39 |
| Preterm | 1.83 | 3.46 | 102.46 | 0.53 | .598 | −5.04 to 8.70 | |
| Sex: Father | −4.66 | 2.27 | 73.74 | −2.05 | .044b | −9.19 to −0.14 | |
| Score Child Domain | Intercept | 88.91 | 3.40 | 150.28 | 26.16 | .000 | 82.19-95.62 |
| Preterm | 2.66 | 3.04 | 101.73 | 0.88 | .38 | −3.36 to 8.68 | |
| Sex: Father | 1.89 | 1.96 | 74.58 | 0.97 | .34 | −2.01 to 5.79 | |
| Score Dimension Health | Intercept | 14.87 | 0.47 | 119.23 | 31.37 | .000 | 13.93-15.81 |
| Preterm | −0.21 | 0.31 | 93.01 | −0.68 | .50 | −0.83 to 0.41 | |
| Sex: Father | −0.62 | 0.30 | 89.67 | −2.03 | .045b | −1.22 to −0.01 | |
| Score Dimension Depression | Intercept | 19.73 | 1.08 | 138.94 | 18.31 | .000 | 17.60-21.86 |
| Preterm | 0.47 | 0.87 | 106.26 | 0.54 | .59 | −1.27 to 2.20 | |
| Sex: Father | −2.20 | 0.65 | 83.76 | −3.39 | .001b | −3.49 to −0.91 | |
| Score Dimension Spouse | Intercept | 19.53 | 0.87 | 154.57 | 22.45 | .000 | 17.81-21.25 |
| Preterm | 0.15 | 0.82 | 105.29 | 0.181 | .86 | −1.47 to 1.77 | |
| Sex: Father | −1.57 | 0.49 | 72.72 | −3.216 | .002b | −2.54 to −0.60 | |
| Score Dimension Acceptability | Intercept | 8.72 | 0.58 | 159.53 | 15.01 | .000 | 7.57-9.87 |
| Preterm | 0.41 | 0.53 | 112.43 | 0.77 | .44 | −0.64 to 1.46 | |
| Sex: Father | 0.91 | 0.33 | 83.86 | 2.76 | .007b | 0.26-1.57 |
Abbreviation: CI, confidence interval.
aFixed effects of total parenting stress scores, scores in domains, and significant scores in dimensions.
bItems for which significant differences were observed.
DISCUSSION
Becoming a parent after PTB is a stressful event accompanied by loss of taking for granted a child's health. Lasiuk et al50 describe this process as a “disruption in the parents' meaning system, followed by uncertainty and lack of agency.”
Mothers and fathers of preterm infants coped with added stress from the moment of sudden birth through hospitalization and transition home. Our finding aligns with earlier studies that reported greater parenting stress 1 year after PTB and greater concerns about the child in the first 2 years.23,25,37 We were surprised to find that stress experiences equalized 2 to 3 years after PTB and FTB, perhaps because parents in this study received more support associated with their middle-class background. Longitudinal studies of socioeconomically disadvantaged parents may return different results.14
After 2 to 3 years, mothers experienced more stress than fathers in the PSI's parent domain. Gender is a factor in psychosocial stress and, like our study, the literature consistently shows that women report higher levels of stress than men.10,15,51–53 Most mothers in our sample took the role of primary caregiver and were exposed to daily stressful circumstances. They had symptoms of depression, poorer spousal support, and poorer perceived health. Fathers, entitled to only 3 days paid leave by Swiss law, adopted the traditional role of breadwinner, spent less time with their children, and were less accepting of their child, consistent with the findings of earlier studies.54–56 Few studies have examined the influence of paternal paid leave on the family system: it can increase fathers' involvement in their infant's care and strengthen the parent–infant relationship. Despite these facts, Switzerland is one of the very few European countries with policies supporting only short paid paternal leave, similarly to the United States.57 Mothers and fathers also coped differently with NICU: mothers used active participation in childcare as coping mechanism43,58,59; fathers who wished to be involved waited for an invitation. Mothers felt loss of control, of privacy, and loss of closeness to their child in NICU, while fathers felt isolated and were distressed by the technical surroundings and their child's appearance. The distraction of work and more absence/distance may explain why PTB fathers were less stressed than mothers.60 In 2 earlier studies, going back to work emerged to be a coping strategy for fathers.58,61 Two fathers retrospectively felt that they needed psychological support. The studies by Pohlman61 and Arockiasamy et al58 also highlight fathers denying their emotional needs. Studies advocating healthcare provider awareness of fathers' individual situation and needs suggest to react carefully and sensitively to fathers emotional feelings, to provide information tailored to fathers, and to actively engage them in the care of their preterm infant.62,63 Lindberg et al64 showed that care acts play an instrumental role in helping fathers develop strong bonds with their infants. Both parents bonded with their child when they were able to provide skin-to-skin care in the NICU.64–67
Positive communication between healthcare professionals and parents reinforced parents' optimism, hope, and trust during hospitalization and after discharge, but parents thought that communication that focused on problems of their child's development impeded coping.6,7 Transfer of a child to another ward or hospital was associated with loss of trust in healthcare providers and parental confidence. Parents needed continued support from the same group of professionals during referrals and a well-planned transfer.
Our study associated hospital discharge and the first week at home after a PTB with feelings of insecurity, anxiety, and need for additional support, consistent with previous research.8,42,43 Discharge was perceived as coming too soon and it was inconsistently managed. Parents and healthcare providers may disagree on readiness for discharge; this implies that readiness must carefully be assessed and include the infant, the family and home environment, and community and healthcare system readiness.68,69
Implications for Practice
Parents would benefit from interventions that help them cope with NICU.70 Our results suggest that both mothers and fathers want to care for their infants. Intervention programs, such as “Creating Opportunities for Parent Empowerment” or “Mother–Infant Transaction Program,” which are designed to enhance parental confidence while including parents as partners into the care for their infants should be further assessed for implementation and effectiveness.25,71 Challenges in transitional care such as suboptimal parent–professional communication, poor coordination of postdischarge services, and parental need for support after discharge are addressed in Naylor's Transitional Care Model, who developed a nurse-led multidisciplinary model including physicians, nurses, social workers, and discharge planners to improve elder health outcomes and manage care while reducing healthcare costs.72 An advanced practice neonatal nurse-led version could help improve health outcomes, including parenting stress for parents and their children after PTB. Hospitals in Germany have already implemented transitional care models based on multidisciplinary teams of professionals (“Bunter Kreis,” “FamilieNetz,” and “Elternberatung Frühstart”), and these might be further assessed by healthcare professionals and researchers for implementation in other countries and settings.73–75
Strengths and Limitations of the Study
Our findings are not generalizable to all parents after FTB and PTB; our participants were volunteers from 2-parent heterosexual families, well-educated, middle-class, with relatively healthy children. More burdened families may have been less likely to volunteer. We assume that more burdened families would experience more stress. Without discounting the possible significance of multiple births as a factor in parenting stress, our study placed nonsingleton birth outside its scope as an independent variable and instead regarded it as part of a matrix of correlating influences within both multiple birth and PTB rates. Although we did not monitor parenting stress over the long term, we confirmed qualitative with quantitative findings 2 to 3 years after birth to show changes in perceived stress over time after PTB, which is a strength of this study. Our retrospective qualitative study used photo-elicitation to help parents vividly recall their birth events, bringing back deep memories and emotions. By including fathers and interviewing mothers and fathers could identify gender differences in stress perceptions and examine factors associated with these differences.
Implications for Further Research
We need more longitudinal data on parenting stress after PTB and FTB and research that focuses on families with preterm children who suffer from developmental difficulties. Researchers should assess existing intervention programs designed to reduce parental stress and determine their effectiveness, along with developing new models of care that help reduce parental stress after PTB.
Summary of Recommendations for Practice and Research.
| What we know: |
|
| What needs to be studied: |
|
| What can we do today that would guide caregivers in the practice setting considering use of this evidence for guiding practice: |
|
CONCLUSIONS
Although PTB created considerable physical and emotional strain for parents, perceived parenting stress leveled off 2 to 3 years later. The transition to parenthood was different after PTB than FTB. Factors such as good communication with healthcare professionals, both parents' involvement in infant care at NICU, staff support enhancing parents' coping and self-confidence, and optimized discharge management need to be translated into important interventions with long-term effects on parenting stress and family well-being.
Footnotes
The authors disclose any potential financial or ethical conflicts of interest regarding the contents of the submission.
References
- 1.Cowan CP, Cowan PA. Interventions to ease the transition to parenthood: why they are needed and what they can do. Fam Relat. 1995;44(4):412–423. [Google Scholar]
- 2.Gloger-Tippelt G. Schwangerschaft und erste Geburt (Pregnancy and First Birth). Stuttgart, Germany: Kohlhammer; 1988. [Google Scholar]
- 3.Bryanton J, Beck CT. Postnatal parental education for optimizing infant general health and parent-infant relationships. Cochrane Database Syst Rev. 2013;11:CD004068. [DOI] [PubMed] [Google Scholar]
- 4.Belsky J. The determinants of parenting: a process model. Child Dev. 1984;55:83–96. [DOI] [PubMed] [Google Scholar]
- 5.Ostberg M, Hagekull B. A structural modeling approach to the understanding of parenting stress. J Clin Child Psychol. 2000;29(4):615–625. [DOI] [PubMed] [Google Scholar]
- 6.Fegran L, Helseth S, Fagermoen MS. A comparison of mothers' and fathers' experiences of the attachment process in a neonatal intensive care unit. J Clin Nurs. 2008;17(6):810–816. [DOI] [PubMed] [Google Scholar]
- 7.Holditch-Davis D, Miles MS. Mothers' stories about their experiences in the neonatal intensive care unit. Neonatal Netw. 2000; 19(3):13–21. [DOI] [PubMed] [Google Scholar]
- 8.Kantrowitz-Gordon I, Altman MR, Vandermause R. Prolonged distress of parents after early preterm birth. J Obstet Gynecol Neonatal Nurs. 2016;45(2):196–209. [DOI] [PubMed] [Google Scholar]
- 9.Shin H, White-Traut R. The conceptual structure of transition to motherhood in the neonatal intensive care unit. J Adv Nurs. 2007;58(1):90–98. [DOI] [PubMed] [Google Scholar]
- 10.Baia I, Amorim M, Silva S, Kelly-Irving M, De Freitas C, Alves E. Parenting very preterm infants and stress in neonatal intensive care units. Early Hum Dev. 2016;101:3–9. [DOI] [PubMed] [Google Scholar]
- 11.Dudek-Shriber L. Parent stress in the neonatal intensive care unit and the influence of parent and infant characteristics. Am J Occup Ther 2004;58(5):509–520. [DOI] [PubMed] [Google Scholar]
- 12.Greene MM, Rossman B, Patra K, Kratovil A, Khan S, Meier PP. Maternal psychological distress and visitation to the neonatal intensive care unit. Acta Paediatr. 2015;104(7):e306–e313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holditch-Davis D, Miles MS, Weaver MA, et al. Patterns of distress in African-American mothers of preterm infants. J Dev Behav Pediatr. 2009;30(3):193–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holditch-Davis D, Santos H, Levy J, et al. Patterns of psychological distress in mothers of preterm infants. Infant Behav Dev. 2015;41:154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ionio C, Colombo C, Brazzoduro V, et al. Mothers and fathers in NICU: the impact of preterm birth on parental distress. Eur J Psychol. 2016;12(4):604–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spear ML, Leef K, Epps S, Locke R. Family reactions during infants' hospitalization in the neonatal intensive care unit. Am J Perinatol. 2002;19(4):205–213. [DOI] [PubMed] [Google Scholar]
- 17.Thomas J, Feeley N, Grier P. The perceived parenting self-efficacy of first-time fathers caring for very-low-birth-weight infants. Issues Compr Pediatr Nurs. 2009;32(4):180–199. [DOI] [PubMed] [Google Scholar]
- 18.Forcada-Guex M, Borghini A, Pierrehumbert B, Ansermet F, Muller-Nix C. Prematurity, maternal posttraumatic stress and consequences on the mother-infant relationship. Early Hum Dev. 2011;87(1):21–26. [DOI] [PubMed] [Google Scholar]
- 19.Coletti MF, Caravale B, Gasparini C, Franco F, Campi F, Dotta A. One-year neurodevelopmental outcome of very and late preterm infants: risk factors and correlation with maternal stress. Infant Behav Dev. 2015;39:11–20. [DOI] [PubMed] [Google Scholar]
- 20.Davis L, Edwards H, Mohay H, Wollin J. The impact of very premature birth on the psychological health of mothers. Early Hum Dev. 2003;73(1-2):61–70. [DOI] [PubMed] [Google Scholar]
- 21.Raines DA. Mothers' stressor as the day of discharge from the NICU approaches. Adv Neonatal Care. 2013;13(3):181–187. [DOI] [PubMed] [Google Scholar]
- 22.Rowe J, Jones L. Discharge and beyond. A longitudinal study comparing stress and coping in parents of preterm infants. J Neonatal Nurs. 2010;16(6):258–266. [Google Scholar]
- 23.Singer LT, Salvator A, Guo S, Collin M, Lilien L, Baley J. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. JAMA. 1999;281(9):799–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garfield CF, Lee Y, Kim HN. Paternal and maternal concerns for their very low-birth-weight infants transitioning from the NICU to home. J Perinat Neonatal Nurs. 2014;28(4):305–312. [DOI] [PubMed] [Google Scholar]
- 25.Kaaresen PI, Ronning JA, Ulvund SE, Dahl LB. A randomized, controlled trial of the effectiveness of an early-intervention program in reducing parenting stress after preterm birth. Pediatrics. 2006;118(1):e9–e19. [DOI] [PubMed] [Google Scholar]
- 26.Suttora C, Spinelli M, Monzani D. From prematurity to parenting stress: the mediating role of perinatal post-traumatic stress disorder. Eur J Dev Psychol. 2014;11(4):478–493. [Google Scholar]
- 27.Gray PH, Edwards DM, Gibbons K. Parenting stress trajectories in mothers of very preterm infants to 2 years. Arch Dis Child. 2018;103(1):F43–F48. [DOI] [PubMed] [Google Scholar]
- 28.Huhtala M, Korja R, Lehtonen L, Haataja L, Lapinleimu H, Rautava P. Associations between parental psychological well-being and socio-emotional development in 5-year-old preterm children. Early Hum Dev. 2014;90(3):119–124. [DOI] [PubMed] [Google Scholar]
- 29.Treyvaud K. Parent and family outcomes following very preterm or very low birth weight birth: a review. Semin Fetal Neonatal Med. 2014;19(2):131–135. [DOI] [PubMed] [Google Scholar]
- 30.Howe TH, Sheu CF, Wang TN, Hsu YW. Parenting stress in families with very low birth weight preterm infants in early infancy. Res Dev Disabil. 2014;35(7):1748–1756. [DOI] [PubMed] [Google Scholar]
- 31.Asaka Y, Takada S. Relation between sleep status of preterm infants aged 1-2 years and mothers' parenting stress. Pediatr Int. 2013;55(4):416–421. [DOI] [PubMed] [Google Scholar]
- 32.Neri E, Agostini F, Baldoni F, Facondini E, Biasini A, Monti F. Preterm infant development, maternal distress and sensitivity: the influence of severity of birth weight. Early Hum Dev. 2017;106-107:19–24. [DOI] [PubMed] [Google Scholar]
- 33.Taylor HG, Klein N, Minich NM, Hack M. Long-term family outcomes for children with very low birth weights. Arch Pediatr Adolescent Med. 2001;155(2):155–161. [DOI] [PubMed] [Google Scholar]
- 34.Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;371(9608):261–269. [DOI] [PubMed] [Google Scholar]
- 35.Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJ. Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. JAMA. 2002;288(6):728–737. [DOI] [PubMed] [Google Scholar]
- 36.Reijneveld SA, De Kleine MJ, Van Baar AL, et al. Behavioural and emotional problems in very preterm and very low birthweight infants at age 5 years. Arch Dis Child Fetal Neonatal Ed. 2006;91(6):F423–F428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brummelte S, Grunau RE, Synnes AR, Whitfield MF, Petrie-Thomas J. Declining cognitive development from 8 to 18 months in preterm children predicts persisting higher parenting stress. Early Hum Dev. 2011;87(4):273–280. [DOI] [PubMed] [Google Scholar]
- 38.Miceli PJ, Goeke-Morey MC, Whitman TL, Kolberg KS, Miller-Loncar C, White RD. Brief report: birth status, medical complications, and social environment: individual differences in development of preterm, very low birth weight infants. J Pediatr Psychol. 2000;25(5):353–358. [DOI] [PubMed] [Google Scholar]
- 39.Singer LT, Fulton S, Kirchner HL, et al. Parenting very low birth weight children at school age: maternal stress and coping. J Pediatr. 2007;151(5):463–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huhtala M, Korja R, Lehtonen L, et al. Parental psychological well-being and behavioral outcome of very low birth weight infants at 3 years. Pediatrics. 2012;129(4):e937–e944. [DOI] [PubMed] [Google Scholar]
- 41.Hagen IH, Iversen VC, Svindseth MF. Differences and similarities between mothers and fathers of premature children: a qualitative study of parents' coping experiences in a neonatal intensive care unit. BMC Pediatr. 2016;16:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mundy CA. Assessment of family needs in neonatal intensive care units. Am J Crit Care. 2010;19(2):156–163. [DOI] [PubMed] [Google Scholar]
- 43.Jackson K, Ternestedt BM, Schollin J. From alienation to familiarity: experiences of mothers and fathers of preterm infants. J Adv Nurs. 2003;43(2):120–129. [DOI] [PubMed] [Google Scholar]
- 44.Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. 2nd ed. Los Angeles, London, New Delhi, Singapore, Washington DC: SAGE Publications Inc; 2011. [Google Scholar]
- 45.Harper D. Talking about pictures: a case for photo elicitation. Vis Stud. 2002;17(1):13–26. [Google Scholar]
- 46.Grunau RE, Whitfield MF, Petrie-Thomas J, et al. Neonatal pain, parenting stress and interaction, in relation to cognitive and motor development at 8 and 18 months in preterm infants. Pain. 2009;143(1-2):138–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abidin RR. Parenting Stress Index. Professional Manual. 3rd ed. Odessa, FL: Psychological Assessment Resources, Inc; 1995. [Google Scholar]
- 48.Hofecker Fallahpour M, Benkert TN, Riecher-Rössler A, Stieglitz RD. Parenthood and parenting stress: psychometric testing of the Parenting Stress Index (PSI) in a German sample. Psychother Psychosom Med Psychol. 2009;59(6):224–233. [DOI] [PubMed] [Google Scholar]
- 49.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 50.Lasiuk GC, Comeau T, Newburn-Cook C. Unexpected: an interpretive description of parental traumas' associated with preterm birth. BMC Pregnancy Childbirth. 2013;13(suppl 1):S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Aftyka A, Rybojad B, Rozalska-Walaszek I, Rzonca P, Humeniuk E. Post-traumatic stress disorder in parents of children hospitalized in the neonatal intensive care unit (NICU): medical and demographic risk factors. Psychiatr Danub. 2014;26(4):347–352. [PubMed] [Google Scholar]
- 52.Ghorbani M, Dolatian M, Shams J, Alavi-Majd H, Tavakolian S. Factors associated with posttraumatic stress disorder and its coping styles in parents of preterm and full-term infants. Glob J Health Sci. 2014; 6(3):65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vismara L, Rolle L, Agostini F, et al. Perinatal parenting stress, anxiety, and depression outcomes in first-time mothers and fathers: a 3- to 6-months postpartum follow-up study. Front Psychol. 2016;7:938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ahn YH, Kim NH. Parental perception of neonates, parental stress and education for NICU parents. Asian Nurs Res (Korean Soc Nurs Sci). 2007;1(3):199–210. [DOI] [PubMed] [Google Scholar]
- 55.Saisto T, Salmela-Aro K, Nurmi JE, Halmesmaki E. Longitudinal study on the predictors of parental stress in mothers and fathers of toddlers. J Psychosom Obstet Gynaecol. 2008;29(3):213–222. [DOI] [PubMed] [Google Scholar]
- 56.Der Bundesrat. 822.11. Bundesgesetz über die Arbeit in Industrie, Gewerbe und Handel, Art. 36 (Federal Law on Labor in Industry, Commerce and Trade, §36). Arbeitnehmer mit Familienpflichten (Jobholders with family responsibilities). In. Bern 2000. Available at https://www.admin.ch/opc/de/classified-compilation/19640049/index.html.
- 57.Heymann J, Sprague AR, Nandi A, et al. Paid parental leave and family wellbeing in the sustainable development era. Public Health Rev. 2017;38:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Arockiasamy V, Holsti L, Albersheim S. Fathers' experiences in the neonatal intensive care unit: a search for control. Pediatrics. 2008;121(2):e215–e222. [DOI] [PubMed] [Google Scholar]
- 59.Sloan K, Row J, Jones L. Stress and coping in fathers following the birth of a preterm infant. J Neonatal Nurs. 2008;14(4):108–115. [Google Scholar]
- 60.Hollywood M, Hollywood E. The lived experiences of fathers of a premature baby on a neonatal intensive care unit. J Neonatal Nurs. 2011;17(1):32–40. [Google Scholar]
- 61.Pohlman S. The primacy of work and fathering preterm infants: findings from an interpretive phenomenological study. Adv Neonatal Care. 2005;5(4):204–216. [DOI] [PubMed] [Google Scholar]
- 62.Martel MJ, Milette I, Bell L, Tribble DS, Payot A. Establishment of the relationship between fathers and premature infants in neonatal units. Adv Neonatal Care. 2016;16(5):390–398. [DOI] [PubMed] [Google Scholar]
- 63.Provenzi L, Santoro E. The lived experience of fathers of preterm infants in the neonatal intensive care unit: a systematic review of qualitative studies. J Clin Nurs. 2015;24(13-14):1784–1794. [DOI] [PubMed] [Google Scholar]
- 64.Lindberg B, Axelsson K, Ohrling K. Adjusting to being a father to an infant born prematurely: experiences from Swedish fathers. Scand J Caring Sci. 2008;22(1):79–85. [DOI] [PubMed] [Google Scholar]
- 65.Baley J. Skin-to-skin care for term and preterm infants in the neonatal ICU. Pediatrics. 2015;136(3):596–599. [DOI] [PubMed] [Google Scholar]
- 66.Conde-Agudelo A, Diaz-Rossello JL. Kangaroo mother care to reduce morbidity and mortality in low birthweight infants. Cochrane Database Syst Rev. 2016;(8):CD002771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Feldman R, Rosenthal Z, Eidelman AI. Maternal-preterm skin-to-skin contact enhances child physiologic organization and cognitive control across the first 10 years of life. Biol Psychiatry. 2014;75(1):56–64. [DOI] [PubMed] [Google Scholar]
- 68.American Academy of Pediatrics Committee on Fetus & Newborn. Hospital discharge of the high-risk neonate. Pediatrics. 2008;122(5):1119–1126. [DOI] [PubMed] [Google Scholar]
- 69.Weiss M, Johnson NL, Malin S, Jerofke T, Lang C, Sherburne E. Readiness for discharge in parents of hospitalized children. J Pediatr Nurs. 2008;23(4):282–295. [DOI] [PubMed] [Google Scholar]
- 70.Benzies KM, Magill-Evans JE, Hayden KA, Ballantyne M. Key components of early intervention programs for preterm infants and their parents: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2013;13(suppl 1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Melnyk BM, Alpert-Gillis L, Feinstein NF, et al. Improving cognitive development of low-birth-weight premature infants with the COPE program: a pilot study of the benefit of early NICU intervention with mothers. Res Nurs Health. 2001;24(5):373–389. [DOI] [PubMed] [Google Scholar]
- 72.Naylor MD, Feldman PH, Keating S, et al. Translating research into practice: transitional care for older adults. J Eval Clin Pract. 2009;15(6):1164–1170. [DOI] [PubMed] [Google Scholar]
- 73.Porz F, Podeswik A. Case Management in der Kinder- und Jugendmedizin. Qualitätsmanagement beim Aufbau und in der Begleitung von Nachsorgeeinrichtungen für schwer und chronisch kranke Kinder und Jugendliche am Beispiel des Bunten Kreises (Case management in paediatrics. Quality management in setting up and accompanying aftercare facilities for severely and chronically ill children and adolescents using the example of Bunter Kreis]. In: Brinkman V, ed. Case Management, Organisationsentwicklung und Change Management im Gesundheits- und Sozialunternehmen (Case Management, Organizational Development and Change Management in Health and Social Organizations). 2nd ed. Wiesbaden, Germany: Gabler Fachverlag GmbH; 2010:337. [Google Scholar]
- 74.Reichert J, Rüdiger M. Psychologisch-sozialmedizinische Versorgung von Eltern Frühgeborener. Stuttgart, Germany: Ligatur; 2012. [Google Scholar]
- 75.Huning BM, Reimann M, Beerenberg U, Stein A, Schmidt A, Felderhoff-Muser U. Establishment of a family-centred care programme with follow-up home visits: implications for clinical care and economic characteristics. Klin Padiatr. 2012;224(7):431–436. [DOI] [PubMed] [Google Scholar]