Abstract
Cell-proliferation potency is limited, as cells cannot proceed through the cell cycle continually. Instead, they eventually show an irreversible arrest of proliferation, commonly referred to as cellular senescence. Following the initial discovery of this phenomenon by Hayflick et al., studies have indicated that cells are also destined to undergo aging. In addition to the irreversible termination of proliferation, senescent cells are characterized by a flattened and enlarged morphology. Senescent cells become pro-inflammatory and contribute to the initiation and maintenance of sustained chronic sterile inflammation. Aging is associated with the accumulation of senescent cells in the cardiovascular system, and in general these cells are considered to be pathogenic because they mediate vascular remodeling. Recently, genetic and pharmacological approaches have enabled researchers to eliminate senescent cells both in vitro and in vivo. The term “senolysis” is now used to refer to the depletion of senescent cells, and evidence indicates that senolysis contributes to the reversal of age-related pathogenic phenotypes without the risk of tumorigenesis. The concept of senolysis has opened new avenues in research on aging, and senolysis may be a promising therapeutic approach for combating age-related disorders, including arterial diseases.
Keywords: Cellular senescence, Arterial diseases, Senolysis
INTRODUCTION
Aging predisposes animals to age-related disorders,1,2 which include heart failure, systemic metabolic disorders, and arterial diseases.3,4,5 Aging itself is not pathogenic, but rather a physiological and biological process that has links with several undesirable diseases.2 To some extent, the mechanisms of aging share similarities with those of age-related diseases.2,6,7 For this reason, it remains crucial to understand the pathologies involved in chronological aging and age-related diseases.2,8 In an elegant article, López-Otín et al.2 reviewed chronological aging and linked this process with alterations in intercellular communication, instability of the genome, telomere shortening, alterations in epigenetics, deregulated nutrient sensing, loss of proteostasis, mitochondrial dysfunction, stem cell exhaustion, and cellular senescence.2 All these processes disturb homeostasis in organs and at the cellular level, and contribute to reduced physiological activity, making organisms prone to death.2 The mechanisms underlying aging and age-related disorders are complex; however, studies have shown that cellular senescence plays pathogenic roles in these conditions.6,9,10,11,12,13,14,15,16 Cellular senescence was originally defined as cells showing an irreversible termination of proliferation.17 These cells show flat morphology, in association with an altered genetic expression profile.18 They become positive for p53 or p16Ink4a, and contribute to the initiation and maintenance of sustained chronic sterile inflammation.2,6,8,12,14,19 Cells positive for these senescence markers accumulate in organs affected by aging and age-related disorders.7,19 Co-culture of young fibroblasts with senescent fibroblasts increased the levels of markers of DNA damage in young cells, indicating that senescence has a contagious aspect, which was first described as the “bystander effect”.20 In general, senescent cells are considered to promote tissue remodeling.6,8 It was recently shown that a process referred to as “senolysis” that involves the pharmacological or genetic depletion of senescent cells yields beneficial effects in chronological and age-related disease models.21,22,23 Compounds that mediate cell death only in senescent cells are referred to as “senolytics,” and studies have suggested that the use of senolytics is promising for combating age-related disorders.9,23,24
CELLULAR SENESCENCE AND SENESCENCE-RELATED MOLECULES IN ARTERIAL DISEASES
The number of senescent cells in arteries is reported to increase significantly with age.7,25,26,27 Aging is associated with higher expression of cyclin-dependent kinase inhibitors (p16 and p21), phosphorylated p38, double-stranded DNA breaks, and senescence-associated beta-galactosidase (SA-β-gal) activity in the vessels of humans and rodents.28,29,30,31 The expression of p53, a tumor suppressor gene, and p21 was found to be increased in the arteries of an aged population.27 This was associated with the breakdown of telomere structures, described as “telomere uncapping”.27 A study analyzing single-nucleotide polymorphisms concluded that elongated telomere length is associated with reduced risks of coronary heart disease and abdominal aortic aneurysm (AAA).32 Additional studies have indicated that cellular senescence, mediated by senescence molecules, plays a role in the pathogenesis of arterial diseases, including aortic aneurysm, coronary artery disease, and peripheral artery disease (PAD), all of which are discussed below.25,33
1. Aortic aneurysm
Thoracic aortic aneurysms and AAAs are life-threatening aortic diseases, the risk of which is known to increase with age. Endothelial cells (ECs) and vascular smooth muscle cells (VSMCs) from AAA patients show telomere attrition and oxidative DNA damage.25 Human VSMCs from AAA patients exhibited high levels of phosphorylated histone H2AX (γH2AX), but no correlation was found with patients' chronological age.33 Sirtuins are protein deacetylases that are known to inhibit aging and contribute to longevity.34 Suppression of vascular cell senescence by the activation of sirtuin 1 (SIRT1) prevented AAA formation, but AAA formation was augmented by promoting cell senescence in these cells.35 It is well known that calorie restriction (CR) can extend the lifespan in organisms ranging from Caenorhabditis elegans to mammals.36,37 CR can reduce the incidence of AAA formation induced by the peptide hormone angiotensin II (AngII) in mice.38 Systemic genetic depletion of p53 also contributed to the suppression of AAA formation.39 Patients with thoracic aortic aneurysm/dissection exhibited elevated numbers of p53-, p21-, and p19-positive cells in the vessel wall, along with increased SA-β-gal activity.40 These results indicate that cellular senescence plays a pathogenic role in aortic aneurysm.38,39,40
2. Coronary artery diseases
Studies have suggested a close connection between cellular senescence and coronary artery disease.7,41 In patients with ischemic heart disease, the number of senescent cells was higher in the coronary arteries than in the internal mammary arteries.7 A large amount of evidence now indicates that telomere length and telomerase activity in peripheral leukocytes and circulating progenitor cells are involved in human cardiovascular diseases.42,43 It has been reported that endothelial progenitor cells from coronary heart disease patients exhibited telomere attrition and reduced telomerase activity.41 In addition, leukocyte telomere length showed an inverse association with the risk of coronary heart disease independent of conventional vascular risk factors.44 MicroRNA (miRNA) is a type of small non-coding RNA, and studies have indicated that some subsets of miRNA play a role in either maintaining or disturbing systemic homeostasis.45,46 Expression of miR-23a has been shown to be higher in peripheral blood mononuclear cells in patients with coronary artery disease than in controls.47 Telomeric repeat binding factor-2 (TRF-2) plays a critical role in telomere maintenance, and miR-23a has been shown to reduce the levels of TRF-2.47 The level of miR-23a was higher in coronary artery disease patients than in controls, suggesting that it affects the progression of coronary atherosclerosis via downregulation of TRF-2.47 Nutrients and oxygen are delivered via capillaries, and the formation of the capillary network is critical for maintaining organ function.11,48 Vascular endothelial growth factor-A (VEGF-A), an angiogenic molecule, has been extensively studied, and suppression of VEGF-A has been reported to result in a lack of tissue remodeling.11,48 Several splice variants or isoforms of VEGF-A exist, all of which are generally recognized to elicit a pro-angiogenic response; however, some isoforms have been reported to become anti-angiogenic molecules.49,50 For example, under metabolic stress, it has been shown that levels of VEGFA165b increased and became pathogenic by reducing angiogenesis in a murine ischemic limb model.50 Senescent human aortic ECs (HAECs) express a high level of VEGFA165b, and interestingly, the transcript Vegfa165b is present at higher levels in patients with coronary heart disease.51 These results indicate that dysregulation of the splicing of VEGF-A into its various isoforms may be a key feature of EC senescence involved in the pathogenesis of coronary heart disease.51
3. PADs
The ankle-brachial index (ABI) is defined as the ratio of ankle systolic blood pressure to that of the arm. A decline in the ABI is known to be indicative of PAD.52 As the ABI decreases with age, this index has traditionally been considered to be independent of traditional risk factors for PAD.53 The prevalence of PAD, and in particular pathological PAD, increases with age.54 It was reported that aging caused a drop in perfusion in a hind limb ischemia model.55 Furthermore, aging was shown to exacerbate injuries mediated by ischemia-reperfusion in skeletal muscle.56 In one study, hind limb ischemia was generated in young, old, and very old mice administered a telomerase activator.57 Blood flow recovery was suppressed in the ischemic limbs of old mice compared to young mice, and recovery in old mice improved in response to administration of a telomerase activator, TA-65.57 The expression of hypoxia inducible factor 1α, VEGF-A, and peroxisome proliferator-activated receptor gamma coactivator 1-alpha was reduced in old mice, but increased following TA-65 administration.57 Expression of senescence markers—including p53, p21, and p16—increased in ischemic limbs on day 3 in old mice, although the expression of these senescence markers was ameliorated in old mice given TA-65.57 This indicates that telomerase activation is a potential therapeutic agent for ischemic tissues in aged individuals.57 Serum from PAD patients showed acceleration in the aging phenotype of HAECs.58 This was suppressed by administering sulodexide (a mixture of glycosaminoglycans).58 The results of that study indicate that serum from PAD patients contains pro-senescent molecules that accelerate arteriosclerosis.58 However, to date, few studies have investigated the role of cellular senescence in PAD or the role of senescence processes in VSMCs specifically.57
ROLE OF SENESCENCE AND SENESCENCE-RELATED MOLECULES IN VSMCs
It is well known that VSMCs, ECs, and immune cells play crucial roles in maintaining vascular homeostasis.59,60 These cells are involved in complex cell-cell interactions, but no investigative techniques currently exist for thoroughly determining the role these cells play in vascular structure, function, and remodeling.60 Studies have indicated, though, that senescence processes play a pivotal role in the involvement of these cells in arterial diseases.7,25,61
1. VSMCs
With aging, VSMCs undergo transformation from a “contractile” to a “synthetic” phenotype, show enhanced inducible nitric oxide synthase activity, and exhibit high expression of intercellular adhesion molecule-1 (ICAM-1) and angiotensinogen in response to stress.3,62 Senescent VSMCs have been reported to accumulate in atherosclerotic plaques of patients with ischemic heart disease, AAA, and PAD.7,25 Approximately 20% of the VSMCs in a carotid artery plaque stained positive for p16, p21, and SA-β-gal.61
In cell culture conditions, VSMCs from the fibrous cap of an atheroma exhibited telomere attrition compared to those from normal media.61 Furthermore, VSMCs with short telomeres were found to be positive for SA-β-gal activity, in addition to their increased levels of p16 and p21.61 Oxidative stress induced DNA damage in VSMCs, which was associated with a reduction in telomerase activity, telomere attrition, and cellular senescence.61 In atherosclerotic plaques, VSMCs become senescent, and the levels of TRF-2 are reduced in these cells.63 TRF-2 is known to be localized in telomeres, where it mediates their protective activity.64 In vitro studies have demonstrated that increased expression of TRF-2 reduces DNA damage, accelerates DNA repair, and suppresses the process of senescence.65 Inhibition of TRF-2 resulted in the opposite phenotype.65 Finally, VSMC-specific TRF-2 suppression led to the progression of atherosclerosis in vivo in mice, which was ameliorated in VSMC-specific TRF-2 overexpression in vivo in mice.65 The peptide hormone AngII is involved in vasoconstriction, ultimately resulting in increased blood pressure.66 It was previously reported that AngII induced senescence in VSMCs in Apoe−/− mice.67 Smooth muscle 22α, an actin-binding protein, was recently shown to promote AngII-induced senescence by the suppression of E3 ubiquitin ligase (Mdm2)-induced p53 degradation in mice.68 Senescent VSMCs in carotid plaques stained positive for interleukin-6, suggesting that senescent VSMCs contribute to vascular remodeling by acquiring the senescence-associated secretory phenotype.69 Dysregulation of the production of growth factors and modifiers of the extracellular matrix results in senescent VSMCs, further accelerating the remodeling process in vessels.69 Suppression of SIRT1 in VSMCs increased vascular cell senescence, upregulated p21 expression, enhanced vascular inflammation, and ultimately promoted pathologies associated with AAA.35 In contrast, specific SIRT1 overexpression inhibited AngII-induced AAA formation and progression in Apoe−/− mice.35
It is well known that CR can prolong the lifespan.70 Interestingly, CR has also been shown to contribute to vascular health, as CR inhibited AAA formation in AngII-infused Apoe−/− mice.38 Furthermore, in an AAA mice model, CR led to an increase in SIRT1 expression in VSMCs, and genetic depletion of Sirt1 in VSMCs abolished the protective role of CR.38 Nicotinamide phosphoribosyltransferase (NAMPT) is a rate-limiting enzyme that initiates nicotinamide adenine dinucleotide (NAD+) production.71 Reduced NAD+ levels are associated with aging and age-associated diseases and contribute to the progression of pathologies in these disorders.71 In ascending dilated aortas from patients with aortopathy, an inverse relationship was found between NAMPT in VSMCs and aortic diameter.72 Depletion of Nampt in VSMCs led to dilatation of the aorta in association with a 43% reduction in NAD+ in the media.72 Infusion of AngII in a VSMC-Nampt knockout mouse model led to aortic medial hemorrhage and dissection or tearing.72 In addition, VSMCs showed high levels of p16 and SA-β-gal activity, indicating that they were senescent, not apoptotic.72 These results suggest that suppression of VSMC senescence contributes to the inhibition of pathologies associated with atherosclerotic diseases.38,71,72
2. ECs
It is well known that ECs play a role in the maintenance of vascular homeostasis, and that EC dysfunction is associated with a pro-inflammatory phenotype, an altered angiogenic response, and pro-oxidant and pro-thrombotic states.15,16,73 The proliferation and migration capacity of aged ECs is diminished, which is associated with reduced nitric oxide production.74 Studies have suggested that EC dysfunction plays a causal role in alterations of blood pressure, systemic metabolism, and the coagulation system, and may play a pivotal role in cellular senescence.75 In a murine left ventricular pressure overload model, the expression of p53 was increased, leading to overexpression of ICAM-1 in these cells, which promoted cardiac inflammation.16 Levels of p53 in ECs also increased under metabolic stress, ultimately resulting in diminished endothelium-dependent vasodilatation and ischemia-induced angiogenesis.15 In addition, elevated levels of p53 in ECs induced systemic metabolic dysfunction.75 Senescent ECs have been shown to exist in atherosclerotic plaques in coronary arteries.7 In contrast, the expression of these senescent cells was low in the internal mammary arteries.7 In the coronary arteries, SA-β-gal activity was high in cells located on the luminal surface, indicating that ECs in the coronary arteries contain SA-β-gal.7 Disturbance of flow in the ascending aorta and aortic arch was shown to promote EC senescence in atherosclerotic mice.76 Oxidized low density lipoprotein (LDL) is a well-established atherogenic lipoprotein.77 The most electronegative subfraction of LDL is L5, which was recently demonstrated to promote EC senescence.63 Furthermore, L5 administration increased levels of γH2AX and SA-β-gal activity in the aortic endothelium of mice.63 A high-caloric diet increased L5 levels in circulation, which also promoted a senescent-like phenotype in the aortic endothelium of Syrian hamsters.63 Regarding cellular pathways, an in vitro study showed that L5 induced EC senescence via activation of the ATM/Chk2/p53 pathway.63 Long non-coding RNA H19 (lncRNA H19), has been shown to be downregulated in the endothelium of aged mice.78 The loss of lncRNA H19 led to increased p16 and p21 levels in vitro.78 In addition, lncRNA H19 depletion increased expression of signal transducer and activator of transcription 3 (STAT3), while suppression of lncRNA H19 reduced STAT3.78 Additional studies have reported that increased H19 levels contributed to an inhibition of STAT3-mediated cell senescence.78 Several molecules and methods have been reported to inhibit senescence in ECs.79,80 Polyphenol suppressed reactive oxygen species (ROS) production, reduced endothelial p53 levels, and increased nitric oxide levels in the aorta, contributing to an inhibition of endothelial dysfunction.79 Both L-citrulline and L-arginine supplementation reduced SA-β-gal activity and p16 levels, and increased telomerase activity in human umbilical vein ECs maintained in a high-glucose medium.80 Administration of these amino acids also led to a reduction of SA-β-gal activity in the abdominal aorta of Zucker diabetic fatty rats with diabetes.80 Omega-3 fatty acids (eicosapentaenoic acid and docosahexaenoic acid) suppressed a hydrogen peroxide-induced increase in SA-β-gal activity in HAECs.81 Aging increased levels of the senescence marker p19 in arteries, and this was suppressed by dietary rapamycin administration, resulting in enhanced endothelium-dependent dilatation in carotid arteries.82 In humans and rodents, it is well known that physical activity improves vascular structure and function.83 The bioavailability of nitric oxide decreases with age, which is associated with high ROS levels and reduced physical activity.84,85,86,87 Compared to sedentary older individuals, older individuals who regularly exercised had lower levels of p53, p21, and p16 in ECs from the brachial artery and antecubital vein.88 This indicates that physical activity inhibits cellular senescence in human vessels.88
3. Immune cells
Atherosclerotic lesions develop and progress through excessive levels of lipids and chronic inflammatory responses.60 Evidence indicates that cellular senescence in immune cells plays a causal role in the progression of atherosclerosis.23,89,90,91 Links between immune cell senescence and atherosclerosis have been reported.23,89,90,91Telomere attrition in leukocytes in aged individuals has been linked with a high mortality rate, of which a moderate number of cases are attributable to cardiovascular deaths.23,89,90,91 Monocytes from atherosclerotic patients showed high levels of ROS and pro-inflammatory cytokine production.89 Senescent intimal foam cells have been shown to accumulate in atherosclerotic lesions and become drivers of atheroma formation.23 Another report showed that p16INK4a can induce cellular senescence in macrophages, causing these cells to become pro-inflammatory.91 Evidence indicates that leukocyte senescence can accelerate plaque formation in atherosclerosis.23,91 Inhibition of the senescence process in immune cells is another important concept to be considered in the treatment of atherosclerotic vascular disorders.23,89,91
SENOLYTICS TARGETING ARTERIAL DISEASES
Genetic and pharmacological studies have indicated that specifically eliminating senescent cells may contribute to reversal of the aging phenotype.9,92 A study in INK-ATTAC mice (prematurely aging mice) eliminated p16Ink4a-positive cells by introducing AP20187, thereby reversing the aging phenotype in several organs including white adipose tissue, the heart, and the kidney.9 Elimination of p16Ink4a-positive cells led to a significant reduction in cardiomyocyte cross-sectional area, indicating an increase in cardiomyocyte number.22 Currently, more than 10 compounds have been reported to induce senolysis, the specific depletion of senescent cells.73 Currently, dasatinib and quercetin (D+Q) and ABT263 are the most studied senolytics.24,73,92 In particular, D+Q has been tested in clinical studies targeting chronic kidney diseases or idiopathic pulmonary fibrosis.92 Recently, it was reported that D+Q administration reduced p16INK4a, p21, and SA-β-gal levels in subcutaneous adipose tissue.92 This was associated with the suppression of inflammatory cell infiltration and an increase in the number of adipocyte progenitor cells, indicating that senolytics may be beneficial in humans.92 In vitro studies of ABT263 showed that this compound specifically depleted irradiated fibroblasts, and that administration of ABT263 led to the clearance of p16Ink4a-positive cells in bone marrow.24 Importantly, ABT263 was shown to contribute to the rejuvenation of hematopoietic stem cells during aging.24 In an aged murine model with hypercholesterolemia, D+Q treatment yielded improvements in vasomotor function.93 In 24-month-old mice, D+Q introduction ameliorated systolic cardiac dysfunction and inhibited end-systolic left ventricular dilatation.94 In pharmacological and genetic senolytic models, the depletion of senescent cells in aged mice contributed to the activation of cardiac progenitor cells in the heart, along with an enhanced proliferative capacity of cardiomyocytes.21,95 Evidence indicates that senolytics have the potential to be considered as possible therapies for atherosclerotic vascular disorders.23 In addition, p16Ink4a-3MR (3MR) is another transgenic mouse model generated to study the inducible depletion of p16Ink4a positive cells.23 Specific deletion of p16-positive cells, as analyzed in Ldlr−/−, p16-3MR mice, led to the elimination of macrophages, VSMCs, and ECs expressing p16 in vessels, and reversed atherosclerosis.23 In a hypercholesterolemic mouse model, D+Q administration reduced aortic calcification and osteogenic signaling.93 In an aged murine myocardial infarction model, ABT263 administration improved myocardial remodeling, diastolic function, and overall survival.96 These results suggest that elimination of senescent cells with senolytics should be considered as a next-generation therapy for atherosclerotic disorders.6,24,73,92
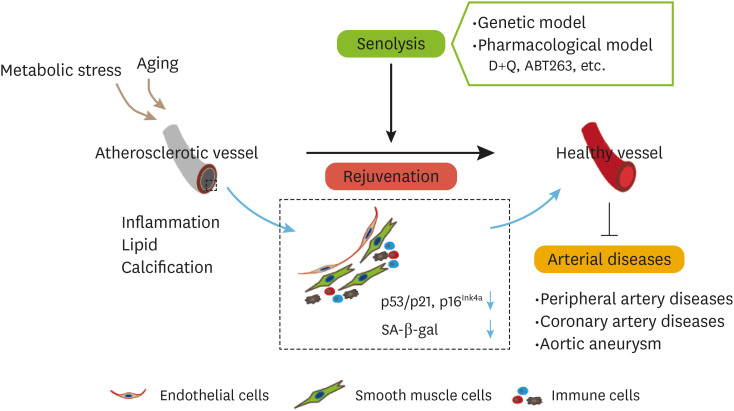
The most fundamental limitation of currently available senolytics is their potential toxicity.97,98 Dasatinib is a tyrosine kinase inhibitor and ABT-263 is a Bcl-2 family inhibitor; it is well known that both were developed as anticancer drugs and therefore come with a risk of toxicity.97,98 Quercetin is polyphenol in the flavonoid group, and may be less toxic; however, it would, in general, need to be taken in combination with dasatinib.73 Discovering new senolytic compounds continues to be an interesting and important research area to combat arterial diseases (Fig. 1).
Fig. 1. The emerging concept underlying therapies targeting arterial diseases with senolysis. The rejuvenation of senescent vascular cells by senolysis contributes to the suppression of senescence markers such as p53/p21, p16Ink4a, and SA-β-gal, and reverses atherosclerosis. In addition to genetic models, senolysis includes pharmacological models such as the D+Q and ABT263 models. These contribute to the suppression of pathologies in arterial diseases, including peripheral artery disease, coronary artery disease, and aortic aneurysm.
D+Q, dasatinib and quercetin; SA-β-gal, senescence-associated beta-galactosidase.
CONCLUSION
In this review article, the role of cellular senescence in arterial diseases was discussed. In combination, the results from many studies show that senescent cells play a pathogenic role in several vascular diseases, including aortic aneurysm, coronary artery disease, and PAD. Genetic and pharmacological senolytic approaches have made considerable contributions to the regression of atherosclerotic plaques in older patients. Findings from more recent studies have indicated that these 2 approaches should be considered as therapeutic possibilities for aging individuals, as they do not appear to promote tumorigenesis. The concept of senolysis has opened a new and very interesting avenue in aging research. In addition to further research investigating the underlying mechanisms contributing to the progression of cellular senescence, it remains critical to find less toxic senolytics in order to establish next-generation therapies for atherosclerotic vascular disorders.
Footnotes
Funding: None.
Conflict of Interest: The authors have no conflicts of interest to declare.
- Conceptualization: Shimizu I.
- Writing - original draft: Shimizu I.
- Writing - review & editing: Minamino T.
References
- 1.Chien KR, Karsenty G. Longevity and lineages: toward the integrative biology of degenerative diseases in heart, muscle, and bone. Cell. 2005;120:533–544. doi: 10.1016/j.cell.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 2.López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153:1194–1217. doi: 10.1016/j.cell.2013.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lakatta EG. So! What's aging? Is cardiovascular aging a disease? J Mol Cell Cardiol. 2015;83:1–13. doi: 10.1016/j.yjmcc.2015.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Triposkiadis F, Xanthopoulos A, Butler J. Cardiovascular aging and heart failure: JACC review topic of the week. J Am Coll Cardiol. 2019;74:804–813. doi: 10.1016/j.jacc.2019.06.053. [DOI] [PubMed] [Google Scholar]
- 5.Yoshii M, Horinaka S, Yabe A, Mori Y, Nakano S, Ishimura K, et al. The relationship between coronary artery disease and parameters of arteriosclerosis in patients with ischemic heart disease. J Hypertens. 2006;24:214–215. [Google Scholar]
- 6.Childs BG, Durik M, Baker DJ, van Deursen JM. Cellular senescence in aging and age-related disease: from mechanisms to therapy. Nat Med. 2015;21:1424–1435. doi: 10.1038/nm.4000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Minamino T, Miyauchi H, Yoshida T, Ishida Y, Yoshida H, Komuro I. Endothelial cell senescence in human atherosclerosis: role of telomere in endothelial dysfunction. Circulation. 2002;105:1541–1544. doi: 10.1161/01.cir.0000013836.85741.17. [DOI] [PubMed] [Google Scholar]
- 8.Shimizu I, Yoshida Y, Suda M, Minamino T. DNA damage response and metabolic disease. Cell Metab. 2014;20:967–977. doi: 10.1016/j.cmet.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 9.Baker DJ, Wijshake T, Tchkonia T, LeBrasseur NK, Childs BG, van de Sluis B, et al. Clearance of p16Ink4a-positive senescent cells delays ageing-associated disorders. Nature. 2011;479:232–236. doi: 10.1038/nature10600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karakasilioti I, Kamileri I, Chatzinikolaou G, Kosteas T, Vergadi E, Robinson AR, et al. DNA damage triggers a chronic autoinflammatory response, leading to fat depletion in NER progeria. Cell Metab. 2013;18:403–415. doi: 10.1016/j.cmet.2013.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sano M, Minamino T, Toko H, Miyauchi H, Orimo M, Qin Y, et al. p53-induced inhibition of Hif-1 causes cardiac dysfunction during pressure overload. Nature. 2007;446:444–448. doi: 10.1038/nature05602. [DOI] [PubMed] [Google Scholar]
- 12.Shimizu I, Yoshida Y, Katsuno T, Tateno K, Okada S, Moriya J, et al. p53-induced adipose tissue inflammation is critically involved in the development of insulin resistance in heart failure. Cell Metab. 2012;15:787. doi: 10.1016/j.cmet.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 13.Shimizu I, Yoshida Y, Moriya J, Nojima A, Uemura A, Kobayashi Y, et al. Semaphorin3E-induced inflammation contributes to insulin resistance in dietary obesity. Cell Metab. 2013;18:491–504. doi: 10.1016/j.cmet.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Tchkonia T, Zhu Y, van Deursen J, Campisi J, Kirkland JL. Cellular senescence and the senescent secretory phenotype: therapeutic opportunities. J Clin Invest. 2013;123:966–972. doi: 10.1172/JCI64098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yokoyama M, Shimizu I, Nagasawa A, Yoshida Y, Katsuumi G, Wakasugi T, et al. p53 plays a crucial role in endothelial dysfunction associated with hyperglycemia and ischemia. J Mol Cell Cardiol. 2019;129:105–117. doi: 10.1016/j.yjmcc.2019.02.010. [DOI] [PubMed] [Google Scholar]
- 16.Yoshida Y, Shimizu I, Katsuumi G, Jiao S, Suda M, Hayashi Y, et al. p53-induced inflammation exacerbates cardiac dysfunction during pressure overload. J Mol Cell Cardiol. 2015;85:183–198. doi: 10.1016/j.yjmcc.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 17.Hayflick L, Moorhead PS. The serial cultivation of human diploid cell strains. Exp Cell Res. 1961;25:585–621. doi: 10.1016/0014-4827(61)90192-6. [DOI] [PubMed] [Google Scholar]
- 18.Shimizu I, Minamino T. Cellular senescence in cardiac diseases. J Cardiol. 2019;74:313–319. doi: 10.1016/j.jjcc.2019.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Minamino T, Orimo M, Shimizu I, Kunieda T, Yokoyama M, Ito T, et al. A crucial role for adipose tissue p53 in the regulation of insulin resistance. Nat Med. 2009;15:1082–1087. doi: 10.1038/nm.2014. [DOI] [PubMed] [Google Scholar]
- 20.Nelson G, Wordsworth J, Wang C, Jurk D, Lawless C, Martin-Ruiz C, et al. A senescent cell bystander effect: senescence-induced senescence. Aging Cell. 2012;11:345–349. doi: 10.1111/j.1474-9726.2012.00795.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson R, Lagnado A, Maggiorani D, Walaszczyk A, Dookun E, Chapman J, et al. Length-independent telomere damage drives post-mitotic cardiomyocyte senescence. EMBO J. 2019;38:e100492. doi: 10.15252/embj.2018100492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baker DJ, Childs BG, Durik M, Wijers ME, Sieben CJ, Zhong J, et al. Naturally occurring p16(Ink4a)-positive cells shorten healthy lifespan. Nature. 2016;530:184–189. doi: 10.1038/nature16932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Childs BG, Baker DJ, Wijshake T, Conover CA, Campisi J, van Deursen JM. Senescent intimal foam cells are deleterious at all stages of atherosclerosis. Science. 2016;354:472–477. doi: 10.1126/science.aaf6659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chang J, Wang Y, Shao L, Laberge RM, Demaria M, Campisi J, et al. Clearance of senescent cells by ABT263 rejuvenates aged hematopoietic stem cells in mice. Nat Med. 2016;22:78–83. doi: 10.1038/nm.4010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cafueri G, Parodi F, Pistorio A, Bertolotto M, Ventura F, Gambini C, et al. Endothelial and smooth muscle cells from abdominal aortic aneurysm have increased oxidative stress and telomere attrition. PLoS One. 2012;7:e35312. doi: 10.1371/journal.pone.0035312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marchand A, Atassi F, Gaaya A, Leprince P, Le Feuvre C, Soubrier F, et al. The Wnt/beta-catenin pathway is activated during advanced arterial aging in humans. Aging Cell. 2011;10:220–232. doi: 10.1111/j.1474-9726.2010.00661.x. [DOI] [PubMed] [Google Scholar]
- 27.Morgan RG, Ives SJ, Lesniewski LA, Cawthon RM, Andtbacka RH, Noyes RD, et al. Age-related telomere uncapping is associated with cellular senescence and inflammation independent of telomere shortening in human arteries. Am J Physiol Heart Circ Physiol. 2013;305:H251–H258. doi: 10.1152/ajpheart.00197.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lin JR, Shen WL, Yan C, Gao PJ. Downregulation of dynamin-related protein 1 contributes to impaired autophagic flux and angiogenic function in senescent endothelial cells. Arterioscler Thromb Vasc Biol. 2015;35:1413–1422. doi: 10.1161/ATVBAHA.115.305706. [DOI] [PubMed] [Google Scholar]
- 29.Melk A, Schmidt BM, Takeuchi O, Sawitzki B, Rayner DC, Halloran PF. Expression of p16INK4a and other cell cycle regulator and senescence associated genes in aging human kidney. Kidney Int. 2004;65:510–520. doi: 10.1111/j.1523-1755.2004.00438.x. [DOI] [PubMed] [Google Scholar]
- 30.Rajapakse AG, Yepuri G, Carvas JM, Stein S, Matter CM, Scerri I, et al. Hyperactive S6K1 mediates oxidative stress and endothelial dysfunction in aging: inhibition by resveratrol. PLoS One. 2011;6:e19237. doi: 10.1371/journal.pone.0019237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang D, McCrann DJ, Nguyen H, St Hilaire C, DePinho RA, Jones MR, et al. Increased polyploidy in aortic vascular smooth muscle cells during aging is marked by cellular senescence. Aging Cell. 2007;6:257–260. doi: 10.1111/j.1474-9726.2007.00274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Telomeres Mendelian Randomization Collaboration. Haycock PC, Burgess S, Nounu A, Zheng J, Okoli GN, et al. Association between telomere length and risk of cancer and non-neoplastic diseases: a mendelian randomization study. JAMA Oncol. 2017;3:636–651. doi: 10.1001/jamaoncol.2016.5945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Riches K, Clark E, Helliwell RJ, Angelini TG, Hemmings KE, Bailey MA, et al. Progressive development of aberrant smooth muscle cell phenotype in abdominal aortic aneurysm disease. J Vasc Res. 2018;55:35–46. doi: 10.1159/000484088. [DOI] [PubMed] [Google Scholar]
- 34.Imai SI, Guarente L. It takes two to tango: NAD+ and sirtuins in aging/longevity control. NPJ Aging Mech Dis. 2016;2:16017. doi: 10.1038/npjamd.2016.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen HZ, Wang F, Gao P, Pei JF, Liu Y, Xu TT, et al. Age-associated sirtuin 1 reduction in vascular smooth muscle links vascular senescence and inflammation to abdominal aortic aneurysm. Circ Res. 2016;119:1076–1088. doi: 10.1161/CIRCRESAHA.116.308895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bordone L, Guarente L. Calorie restriction, SIRT1 and metabolism: understanding longevity. Nat Rev Mol Cell Biol. 2005;6:298–305. doi: 10.1038/nrm1616. [DOI] [PubMed] [Google Scholar]
- 37.Guarente L, Picard F. Calorie restriction--the SIR2 connection. Cell. 2005;120:473–482. doi: 10.1016/j.cell.2005.01.029. [DOI] [PubMed] [Google Scholar]
- 38.Liu Y, Wang TT, Zhang R, Fu WY, Wang X, Wang F, et al. Calorie restriction protects against experimental abdominal aortic aneurysms in mice. J Exp Med. 2016;213:2473–2488. doi: 10.1084/jem.20151794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gao P, Zhang H, Zhang Q, Fang X, Wu H, Wang M, et al. Caloric restriction exacerbates angiotensin II-induced abdominal aortic aneurysm in the absence of p53. Hypertension. 2019;73:547–560. doi: 10.1161/HYPERTENSIONAHA.118.12086. [DOI] [PubMed] [Google Scholar]
- 40.Zhang WM, Liu Y, Li TT, Piao CM, Liu O, Liu JL, et al. Sustained activation of ADP/P2ry12 signaling induces SMC senescence contributing to thoracic aortic aneurysm/dissection. J Mol Cell Cardiol. 2016;99:76–86. doi: 10.1016/j.yjmcc.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 41.Satoh M, Ishikawa Y, Takahashi Y, Itoh T, Minami Y, Nakamura M. Association between oxidative DNA damage and telomere shortening in circulating endothelial progenitor cells obtained from metabolic syndrome patients with coronary artery disease. Atherosclerosis. 2008;198:347–353. doi: 10.1016/j.atherosclerosis.2007.09.040. [DOI] [PubMed] [Google Scholar]
- 42.Hammadah M, Al Mheid I, Wilmot K, Ramadan R, Abdelhadi N, Alkhoder A, et al. Telomere shortening, regenerative capacity, and cardiovascular outcomes. Circ Res. 2017;120:1130–1138. doi: 10.1161/CIRCRESAHA.116.309421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Salpea KD, Humphries SE. Telomere length in atherosclerosis and diabetes. Atherosclerosis. 2010;209:35–38. doi: 10.1016/j.atherosclerosis.2009.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Haycock PC, Heydon EE, Kaptoge S, Butterworth AS, Thompson A, Willeit P. Leucocyte telomere length and risk of cardiovascular disease: systematic review and meta-analysis. BMJ. 2014;349:g4227. doi: 10.1136/bmj.g4227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mori MA, Ludwig RG, Garcia-Martin R, Brandão BB, Kahn CR. Extracellular miRNAs: from biomarkers to mediators of physiology and disease. Cell Metab. 2019;30:656–673. doi: 10.1016/j.cmet.2019.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Salem ES, Vonberg AD, Borra VJ, Gill RK, Nakamura T. RNAs and RNA-binding proteins in immuno-metabolic homeostasis and diseases. Front Cardiovasc Med. 2019;6:106. doi: 10.3389/fcvm.2019.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nasu T, Satoh M, Takahashi Y, Takahashi K, Hitomi S, Morino Y, et al. Expression of miR-23a induces leukocyte telomere shortening and is associated with poor clinical outcomes in patients with coronary artery disease. Eur Heart J. 2017;38:ehx501.P838. doi: 10.1042/CS20170242. [DOI] [PubMed] [Google Scholar]
- 48.Shimizu I, Aprahamian T, Kikuchi R, Shimizu A, Papanicolaou KN, MacLauchlan S, et al. Vascular rarefaction mediates whitening of brown fat in obesity. J Clin Invest. 2014;124:2099–2112. doi: 10.1172/JCI71643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harper SJ, Bates DO. VEGF-A splicing: the key to anti-angiogenic therapeutics? Nat Rev Cancer. 2008;8:880–887. doi: 10.1038/nrc2505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kikuchi R, Nakamura K, MacLauchlan S, Ngo DT, Shimizu I, Fuster JJ, et al. An antiangiogenic isoform of VEGF-A contributes to impaired vascularization in peripheral artery disease. Nat Med. 2014;20:1464–1471. doi: 10.1038/nm.3703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Latorre E, Pilling LC, Lee BP, Bandinelli S, Melzer D, Ferrucci L, et al. The VEGFA156b isoform is dysregulated in senescent endothelial cells and may be associated with prevalent and incident coronary heart disease. Clin Sci (Lond) 2018;132:313–325. doi: 10.1042/CS20171556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Guirguis-Blake JM, Evans CV, Redmond N, Lin JS. Screening for peripheral artery disease using the ankle-brachial index: updated evidence report and systematic review for the US preventive services task force. JAMA. 2018;320:184–196. doi: 10.1001/jama.2018.4250. [DOI] [PubMed] [Google Scholar]
- 53.Oberdier MT, Morrell CH, Lakatta EG, Ferrucci L, AlGhatrif M. Subclinical longitudinal change in ankle-brachial index with aging in a community-dwelling population is associated with central arterial stiffening. J Am Heart Assoc. 2019;8:e011650. doi: 10.1161/JAHA.118.011650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Olinic DM, Spinu M, Olinic M, Homorodean C, Tataru DA, Liew A, et al. Epidemiology of peripheral artery disease in Europe: VAS educational paper. Int Angiol. 2018;37:327–334. doi: 10.23736/S0392-9590.18.03996-2. [DOI] [PubMed] [Google Scholar]
- 55.Faber JE, Zhang H, Lassance-Soares RM, Prabhakar P, Najafi AH, Burnett MS, et al. Aging causes collateral rarefaction and increased severity of ischemic injury in multiple tissues. Arterioscler Thromb Vasc Biol. 2011;31:1748–1756. doi: 10.1161/ATVBAHA.111.227314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Paradis S, Charles AL, Georg I, Goupilleau F, Meyer A, Kindo M, et al. Aging exacerbates ischemia-reperfusion-induced mitochondrial respiration impairment in skeletal muscle. Antioxidants (Basel) 2019;8:E168. doi: 10.3390/antiox8060168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kokubun T, Saitoh SI, Miura S, Ishida T, Takeishi Y. Telomerase plays a pivotal role in collateral growth under ischemia by suppressing age-induced oxidative stress, expression of p53, and pro-apoptotic proteins. Int Heart J. 2019;60:736–745. doi: 10.1536/ihj.18-564. [DOI] [PubMed] [Google Scholar]
- 58.Sosińska-Zawierucha P, Maćkowiak B, Staniszewski R, Sumińska-Jasińska K, Maj M, Krasiński Z, et al. Sulodexide slows down the senescence of aortic endothelial cells exposed to serum from patients with peripheral artery diseases. Cell Physiol Biochem. 2018;45:2225–2232. doi: 10.1159/000488167. [DOI] [PubMed] [Google Scholar]
- 59.Hansson GK, Libby P. The immune response in atherosclerosis: a double-edged sword. Nat Rev Immunol. 2006;6:508–519. doi: 10.1038/nri1882. [DOI] [PubMed] [Google Scholar]
- 60.Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473:317–325. doi: 10.1038/nature10146. [DOI] [PubMed] [Google Scholar]
- 61.Matthews C, Gorenne I, Scott S, Figg N, Kirkpatrick P, Ritchie A, et al. Vascular smooth muscle cells undergo telomere-based senescence in human atherosclerosis: effects of telomerase and oxidative stress. Circ Res. 2006;99:156–164. doi: 10.1161/01.RES.0000233315.38086.bc. [DOI] [PubMed] [Google Scholar]
- 62.Faggiotto A, Ross R, Harker L. Studies of hypercholesterolemia in the nonhuman primate. I. Changes that lead to fatty streak formation. Arteriosclerosis. 1984;4:323–340. doi: 10.1161/01.atv.4.4.323. [DOI] [PubMed] [Google Scholar]
- 63.Wang YC, Lee AS, Lu LS, Ke LY, Chen WY, Dong JW, et al. Human electronegative LDL induces mitochondrial dysfunction and premature senescence of vascular cells in vivo . Aging Cell. 2018;17:e12792. doi: 10.1111/acel.12792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.de Lange T. Protection of mammalian telomeres. Oncogene. 2002;21:532–540. doi: 10.1038/sj.onc.1205080. [DOI] [PubMed] [Google Scholar]
- 65.Wang J, Uryga AK, Reinhold J, Figg N, Baker L, Finigan A, et al. Vascular smooth muscle cell senescence promotes atherosclerosis and features of plaque vulnerability. Circulation. 2015;132:1909–1919. doi: 10.1161/CIRCULATIONAHA.115.016457. [DOI] [PubMed] [Google Scholar]
- 66.Reaux A, Fournie-Zaluski MC, Llorens-Cortes C. Angiotensin III: a central regulator of vasopressin release and blood pressure. Trends Endocrinol Metab. 2001;12:157–162. doi: 10.1016/s1043-2760(01)00381-2. [DOI] [PubMed] [Google Scholar]
- 67.Kunieda T, Minamino T, Nishi J, Tateno K, Oyama T, Katsuno T, et al. Angiotensin II induces premature senescence of vascular smooth muscle cells and accelerates the development of atherosclerosis via a p21-dependent pathway. Circulation. 2006;114:953–960. doi: 10.1161/CIRCULATIONAHA.106.626606. [DOI] [PubMed] [Google Scholar]
- 68.Miao SB, Xie XL, Yin YJ, Zhao LL, Zhang F, Shu YN, et al. Accumulation of smooth muscle 22α protein accelerates senescence of vascular smooth muscle cells via stabilization of p53 in vitro and in vivo . Arterioscler Thromb Vasc Biol. 2017;37:1849–1859. doi: 10.1161/ATVBAHA.117.309378. [DOI] [PubMed] [Google Scholar]
- 69.Gardner SE, Humphry M, Bennett MR, Clarke MCH. Senescent vascular smooth muscle cells drive inflammation through an interleukin-1α-dependent senescence-associated secretory phenotype. Atherosclerosis. 2016;244:E5. doi: 10.1161/ATVBAHA.115.305896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Colman RJ, Anderson RM, Johnson SC, Kastman EK, Kosmatka KJ, Beasley TM, et al. Caloric restriction delays disease onset and mortality in rhesus monkeys. Science. 2009;325:201–204. doi: 10.1126/science.1173635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yoshino J, Baur JA, Imai SI. NAD+ intermediates: the biology and therapeutic potential of NMN and NR. Cell Metab. 2018;27:513–528. doi: 10.1016/j.cmet.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Watson A, Nong Z, Yin H, O'Neil C, Fox S, Balint B, et al. Nicotinamide phosphoribosyltransferase in smooth muscle cells maintains genome integrity, resists aortic medial degeneration, and is suppressed in human thoracic aortic aneurysm disease. Circ Res. 2017;120:1889–1902. doi: 10.1161/CIRCRESAHA.116.310022. [DOI] [PubMed] [Google Scholar]
- 73.Katsuumi G, Shimizu I, Yoshida Y, Minamino T. Vascular senescence in cardiovascular and metabolic diseases. Front Cardiovasc Med. 2018;5:18. doi: 10.3389/fcvm.2018.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Torella D, Leosco D, Indolfi C, Curcio A, Coppola C, Ellison GM, et al. Aging exacerbates negative remodeling and impairs endothelial regeneration after balloon injury. Am J Physiol Heart Circ Physiol. 2004;287:H2850–H2860. doi: 10.1152/ajpheart.01119.2003. [DOI] [PubMed] [Google Scholar]
- 75.Yokoyama M, Okada S, Nakagomi A, Moriya J, Shimizu I, Nojima A, et al. Inhibition of endothelial p53 improves metabolic abnormalities related to dietary obesity. Cell Reports. 2014;7:1691–1703. doi: 10.1016/j.celrep.2014.04.046. [DOI] [PubMed] [Google Scholar]
- 76.Warboys CM, de Luca A, Amini N, Luong L, Duckles H, Hsiao S, et al. Disturbed flow promotes endothelial senescence via a p53-dependent pathway. Arterioscler Thromb Vasc Biol. 2014;34:985–995. doi: 10.1161/ATVBAHA.114.303415. [DOI] [PubMed] [Google Scholar]
- 77.Steinberg D. Clinical trials of antioxidants in atherosclerosis: are we doing the right thing? Lancet. 1995;346:36–38. doi: 10.1016/s0140-6736(95)92657-7. [DOI] [PubMed] [Google Scholar]
- 78.Hofmann P, Sommer J, Theodorou K, Kirchhof L, Fischer A, Li Y, et al. Long non-coding RNA H19 regulates endothelial cell aging via inhibition of STAT3 signalling. Cardiovasc Res. 2019;115:230–242. doi: 10.1093/cvr/cvy206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Furuuchi R, Shimizu I, Yoshida Y, Hayashi Y, Ikegami R, Suda M, et al. Boysenberry polyphenol inhibits endothelial dysfunction and improves vascular health. PLoS One. 2018;13:e0202051. doi: 10.1371/journal.pone.0202051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tsuboi T, Maeda M, Hayashi T. Administration of L-arginine plus L-citrulline or L-citrulline alone successfully retarded endothelial senescence. PLoS One. 2018;13:e0192252. doi: 10.1371/journal.pone.0192252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sakai C, Ishida M, Ohba H, Yamashita H, Uchida H, Yoshizumi M, et al. Fish oil omega-3 polyunsaturated fatty acids attenuate oxidative stress-induced DNA damage in vascular endothelial cells. PLoS One. 2017;12:e0187934. doi: 10.1371/journal.pone.0187934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lesniewski LA, Seals DR, Walker AE, Henson GD, Blimline MW, Trott DW, et al. Dietary rapamycin supplementation reverses age-related vascular dysfunction and oxidative stress, while modulating nutrient-sensing, cell cycle, and senescence pathways. Aging Cell. 2017;16:17–26. doi: 10.1111/acel.12524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sjøberg KA, Frøsig C, Kjøbsted R, Sylow L, Kleinert M, Betik AC, et al. Exercise increases human skeletal muscle insulin sensitivity via coordinated increases in microvascular perfusion and molecular signaling. Diabetes. 2017;66:1501–1510. doi: 10.2337/db16-1327. [DOI] [PubMed] [Google Scholar]
- 84.Ji LL. Redox signaling in skeletal muscle: role of aging and exercise. Adv Physiol Educ. 2015;39:352–359. doi: 10.1152/advan.00106.2014. [DOI] [PubMed] [Google Scholar]
- 85.Nyberg M, Blackwell JR, Damsgaard R, Jones AM, Hellsten Y, Mortensen SP. Lifelong physical activity prevents an age-related reduction in arterial and skeletal muscle nitric oxide bioavailability in humans. J Physiol. 2012;590:5361–5370. doi: 10.1113/jphysiol.2012.239053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Reid MB, Durham WJ. Generation of reactive oxygen and nitrogen species in contracting skeletal muscle: potential impact on aging. Ann N Y Acad Sci. 2002;959:108–116. doi: 10.1111/j.1749-6632.2002.tb02087.x. [DOI] [PubMed] [Google Scholar]
- 87.Sindler AL, Reyes R, Chen B, Ghosh P, Gurovich AN, Kang LS, et al. Age and exercise training alter signaling through reactive oxygen species in the endothelium of skeletal muscle arterioles. J Appl Physiol (1985) 2013;114:681–693. doi: 10.1152/japplphysiol.00341.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rossman MJ, Kaplon RE, Hill SD, McNamara MN, Santos-Parker JR, Pierce GL, et al. Endothelial cell senescence with aging in healthy humans: prevention by habitual exercise and relation to vascular endothelial function. Am J Physiol Heart Circ Physiol. 2017;313:H890–H895. doi: 10.1152/ajpheart.00416.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Calvert PA, Liew TV, Gorenne I, Clarke M, Costopoulos C, Obaid DR, et al. Leukocyte telomere length is associated with high-risk plaques on virtual histology intravascular ultrasound and increased proinflammatory activity. Arterioscler Thromb Vasc Biol. 2011;31:2157–2164. doi: 10.1161/ATVBAHA.111.229237. [DOI] [PubMed] [Google Scholar]
- 90.Cawthon RM, Smith KR, O'Brien E, Sivatchenko A, Kerber RA. Association between telomere length in blood and mortality in people aged 60 years or older. Lancet. 2003;361:393–395. doi: 10.1016/S0140-6736(03)12384-7. [DOI] [PubMed] [Google Scholar]
- 91.Cudejko C, Wouters K, Fuentes L, Hannou SA, Paquet C, Bantubungi K, et al. p16INK4a deficiency promotes IL-4-induced polarization and inhibits proinflammatory signaling in macrophages. Blood. 2011;118:2556–2566. doi: 10.1182/blood-2010-10-313106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hickson LJ, Langhi Prata LG, Bobart SA, Evans TK, Giorgadze N, Hashmi SK, et al. Senolytics decrease senescent cells in humans: preliminary report from a clinical trial of Dasatinib plus Quercetin in individuals with diabetic kidney disease. EBioMedicine. 2019;47:446–456. doi: 10.1016/j.ebiom.2019.08.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Roos CM, Zhang B, Palmer AK, Ogrodnik MB, Pirtskhalava T, Thalji NM, et al. Chronic senolytic treatment alleviates established vasomotor dysfunction in aged or atherosclerotic mice. Aging Cell. 2016;15:973–977. doi: 10.1111/acel.12458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhu Y, Tchkonia T, Pirtskhalava T, Gower AC, Ding H, Giorgadze N, et al. The Achilles' heel of senescent cells: from transcriptome to senolytic drugs. Aging Cell. 2015;14:644–658. doi: 10.1111/acel.12344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lewis-McDougall FC, Ruchaya PJ, Domenjo-Vila E, Shin Teoh T, Prata L, Cottle BJ, et al. Aged-senescent cells contribute to impaired heart regeneration. Aging Cell. 2019;18:e12931. doi: 10.1111/acel.12931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Walaszczyk A, Dookun E, Redgrave R, Tual-Chalot S, Victorelli S, Spyridopoulos I, et al. Pharmacological clearance of senescent cells improves survival and recovery in aged mice following acute myocardial infarction. Aging Cell. 2019;18:e12945. doi: 10.1111/acel.12945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hartmann JT, Haap M, Kopp HG, Lipp HP. Tyrosine kinase inhibitors - a review on pharmacology, metabolism and side effects. Curr Drug Metab. 2009;10:470–481. doi: 10.2174/138920009788897975. [DOI] [PubMed] [Google Scholar]
- 98.Wilson WH, O'Connor OA, Czuczman MS, LaCasce AS, Gerecitano JF, Leonard JP, et al. Navitoclax, a targeted high-affinity inhibitor of BCL-2, in lymphoid malignancies: a phase 1 dose-escalation study of safety, pharmacokinetics, pharmacodynamics, and antitumour activity. Lancet Oncol. 2010;11:1149–1159. doi: 10.1016/S1470-2045(10)70261-8. [DOI] [PMC free article] [PubMed] [Google Scholar]