Abstract
Background
Evidence supporting clinical relevance and persistence of disinhibited social engagement behavior (DSEB) pertains mostly to children reared in institutions and foster care. This study examined the course of DSEB in clinically referred home‐reared children from early into middle childhood, and associations with neglect/emotional maltreatment, effortful control, Attention Deficit/Hyperactivity Disorder, Oppositional Defiant Disorder, and Autism Spectrum Disorder.
Methods
Disinhibited social engagement behavior was examined in 124 children (82% boys, M = 4.06 years, SD = 0.89), referred for treatment of emotional and behavioral problems, by use of the Disturbances of Attachment Interview (DAI) with biological parents. Neglect and emotional maltreatment were assessed from case records and effortful control by use of the Child Behavior Questionnaire. At follow‐up, on average 4 years later, DSEB was examined by use of DAI as well as two observational ratings: the Stranger at the Door procedure (SatD) and a structured home observation of stranger approach. Psychiatric disorders were assessed by means of the Kiddie‐Schedule for Affective Disorders and Schizophrenia.
Results
Persistence of parent‐reported DSEB was found in 57% (n = 27) of the children with DSEB at baseline (n = 47). Parent‐reported DSEB at follow‐up was significantly related to DSEB observed in the SatD (r pb = .31, p = .001) and to observed stranger approach (r s = .41, p < .001), but only stranger approach was associated with baseline DSEB. The course of DSEB was not related to neglect/emotional maltreatment, nor to the level of effortful control. There was no association between DSEB and Autism Spectrum Disorder, but course of DSEB was associated with Attention Deficit/Hyperactivity Disorder/Oppositional Defiant Disorder at follow‐up (χ2 = 13.08, p = .004).
Conclusions
Although explanations for the onset and course of DSEB in home‐reared children remain elusive, findings suggest that DSEB is part of a complex of clinically significant problem behaviors in referred home‐reared preschool children.
Keywords: Disinhibited social engagement, attachment, preschool, longitudinal, home‐reared
Introduction
Aberrant social behavior in the form of lack of reticence with unfamiliar adults was first reported in children who were raised in institutions under conditions of serious insufficient care and neglect (Tizard & Rees, 1975). Since then, this type of behavior has been designated by terms as indiscriminate social behavior, indiscriminate friendliness, disinhibited attachment, and disinhibited social engagement behavior (DSEB) (Zeanah, Chesher, & Boris, 2016). The criteria for Disinhibited Social Engagement Disorder (DSED) in the fifth edition of the Diagnostic and Statistical Manual of mental disorders (DSM‐5) include a pattern of behavior with at least two of the following: reduced reticence in interacting with unfamiliar adults, overly familiar verbal or physical behavior, a failure to maintain proximity to the primary caregiver in unfamiliar settings, and willingness to go off with strangers (American Psychiatric Association, 2013). For a DSED classification, the manual requires extremes of insufficient care, described as social neglect or deprivation, repeated changes of primary caregivers, or rearing in unusual settings. Therefore, most research on DSED and its behavioral phenotype has included children exposed to institutional child‐rearing (Bruce, Tarullo, & Gunnar, 2009; Rutter et al., 2007; Zeanah & Gleason, 2015). Focusing on the full set or subsets of behaviors qualifying for DSED, disinhibited social engagement behavior (DSEB) has also been found in children growing up with their biological parents, where extremes of insufficient care are less prevalent and more difficult to assess (Minnis et al., 2013; Pears, Bruce, Fisher, & Kim, 2010; Scheper et al., 2016). Much less is known about the course and manifestation of DSEB in home‐reared children, and its clinical relevance.
Findings on the relation between DSEB and maltreatment in noninstitutionalized children have been equivocal. DSED (assessed through triangulation of parent, teacher, and observer reports of DSEB) was not associated with maltreatment histories, but was found more common in children adopted between 7 and 24 months compared to outplacement at birth (Kay, Green, & Sharma, 2016). In home‐reared infants, who had not been exposed to out‐of‐home placement or severe physical abuse, observed socially indiscriminate behavior was associated with a history of maltreatment and/or psychiatric hospitalization of mothers (Lyons‐Ruth, Bureau, Riley, & Atlas‐Corbett, 2009). Lyons‐Ruth et al. suggested that socially indiscriminate behavior is not specifically associated with physical abuse or hostility but more with neglect and emotional maltreatment. Higher levels of indiscriminate behavior were reported by caregivers of maltreated preschool‐aged foster children than by caregivers of a low‐income community control group of non‐maltreated home‐reared children (Pears et al., 2010). However, Pears et al. also reported moderate to high levels of indiscriminate behavior in 19% of the non‐maltreated home‐reared children. In children referred for treatment of emotional‐ and behavioral problems, we previously reported that DSEB (assessed by caregiver interview) was as common in home‐reared children as in foster care children, but not associated with maltreatment histories (Scheper et al., 2016). Whether DSEB persists in home‐reared children and whether neglect or emotional maltreatment is related to the course of DSEB in home‐reared children is yet unknown.
Disinhibited social engagement behavior in institutionalized, post‐institutionalized, and adopted children indicate relative persistence of this behavior (Chisholm, 1998; Gleason et al., 2011; Guyon‐Harris, Humphreys, Fox, Nelson, & Zeanah, 2018; Lawler, Koss, Doyle, & Gunnar, 2016; Rutter et al., 2007; Smyke et al., 2012), unless children received early and stable family placement (Guyon‐Harris et al., 2018; Smyke et al., 2012). Continuation of institutional rearing with social deprivation after the age of 6 months was found to predict persistence of DSEB in post‐institutionalized children (Rutter et al., 2007). In a study in adopted children, using a longitudinal design, difficulties in inhibitory control mediated the relation between early deprivation and persistent DSEB (Gorter, Helder, Oh, & Gunnoe, 2017).
Low effortful control in child temperament, including attentional and inhibitory control, has been linked to DSEB in several studies (Bruce et al., 2009; Gleason et al., 2011; Pears et al., 2010). While low effortful control may be an indicator of early exposure to insufficient care due to biological programming, effortful control may also influence children's response to insufficient care (Bakermans‐Kranenburg et al., 2011; Zeanah & Fox, 2004).
Problems in effortful control also have been suggested to underlie the relation between DSEB and externalizing problems (Gleason et al., 2011; Zeanah et al., 2016). Attention Deficit/Hyperactivity Disorder (ADHD), Oppositional Defiant Disorder (ODD), and Conduct Disorder (CD) are psychiatric disorders characterized by externalizing problem behavior (American Psychiatric Association, 2013). The DSM‐5 criteria for DSED requires that the behaviors are not limited to impulsivity, as in ADHD, but should include disinhibited social behavior. This leaves open the possibility that DSED may be comorbid with ADHD. DSED and ADHD showed comorbidity in post‐institutionalized children and in general population children (Gleason et al., 2011; Pritchett, Pritchett, Marshall, Davidson, & Minnis, 2013). In previous studies, DSED symptoms were phenotypically distinguished from ADHD and conduct problems, supporting the clinical relevance of DSEB (Gleason et al., 2011; Minnis et al., 2007). Longitudinal research has shown an association between DSED and later symptoms of ADHD in post‐institutionalized children (Gleason et al., 2011). Socially indiscriminate behavior in 18‐month‐old home‐reared children predicted hostile and hyperactive behavior at the age of five (Lyons‐Ruth et al., 2009). In previously institution‐reared children, DSEB was associated not only with inattention/hyperactivity and conduct problems, but also with autism‐like behavior and problems in peer interaction (Rutter et al., 2007). Clinically, the differentiation between DSED and Autism Spectrum Disorder (ASD) is of interest given that both disorders entail problematic social behaviors (Davidson et al., 2015). It was shown that while symptoms of DSED and ASD co‐occurred in some children, manifestation of DSEB was independent from symptoms of ASD in children with mild intellectual disability, who were referred for psychiatric evaluation (Giltaij, Sterkenburg, & Schuengel, 2015). It is unclear to what extent this finding generalizes to other clinical populations.
The present study aimed to examine the course of DSEB in home‐reared children, after referral for treatment of emotional and behavioral problems at preschool age (1.5–6 years), as DSEB may be included in those problems. The course of parent‐reported DSEB was examined from referral in early childhood until on average 4 years later. Associations between parent report and observational assessments of DSEB were tested. The course of DSEB was examined in relation to neglect/emotional maltreatment and effortful control. Effortful control was also examined as a moderator of the relation between neglect/emotional maltreatment and DSEB. Finally, DSEB in early childhood, as well as the course of DSEB, was examined in relation to ADHD, ODD, CD, and ASD in middle childhood.
Methods
Participants and procedure
Parents were asked to participate in research on child psychopathology between 2009 and 2014, after their children were referred for outpatient treatment to MOC ‘t Kabouterhuis (Amsterdam, the Netherlands), a health center for young children with developmental and behavioral problems. The center offers diagnostic and treatment trajectories in an urban area, where approximately 100,000 young children (0–7 years old) are registered. Children had been referred by general practitioners, medical specialists, and child workers of (public) health care centers or child protection services. At the start of treatment (baseline), primary caregivers were invited for questionnaires and an interview at home. Inclusion criteria for this study were: preschool age (0–6 years), referral for treatment of social‐, emotional and/or behavioral problems, living with biological parents, and available information on DSEB at the start of treatment. All parents of the 317 eligible participants were contacted between 2015 and 2016, and asked to participate in a follow‐up study on the course of mental health problems after intervention in early childhood. When parents agreed to participate, an appointment was made for a home visit to obtain interviews and observations. From the 317 families, four moved abroad, four children were placed out of home, five could not participate because of language problems, nine had not given permission to be approached again for follow‐up, 72 did not want to participate at follow‐up, and of 99 either we had no valid contact details or the subjects did not respond to contact attempts, resulting in 124 participants for this study. There were eight children who were not present at the home visit and therefore could not be observed.
The 124 participants at follow‐up did not significantly differ from the 193 children who did not participate at follow‐up with regard to age (t = 0.89; p = .37), gender (χ2 = 0.19; p = .67), mean levels of DSEB continuous scores (Mann‐Whitney U = 11,005.0, p = .21), and scoring above cut‐off DSEB (χ2 = 0.75; p = .39) at baseline. Parents of children who participated did not report more or less financial problems than parents of children who did not participate at follow‐up (χ2 = 1.26; p = .26). Prevalence of legal protection measures was similar in children who participated (n = 4, 3.2%) to those not participating at follow‐up (n = 6, 3.1%). However, the children differed on reports of neglect/emotional maltreatment (χ2 = 6.07; p = .01). Children who participated had less often reported neglect/emotional maltreatment (25%) compared to the nonparticipating children (38%). There were more children reared in a single‐parent household not participating (26%) compared to children participating at follow‐up (15%; χ2 = 5.81; p = .02) . Also, children of non‐Western origin were less likely than children of western origin (χ2 = 8.19; p = .004) to be retained at follow‐up.
Characteristics at baseline and follow‐up are listed in Table 1. The mean age at first measurement was 4.06 years (SD = 0.89; range 1.92–5.92) and at follow‐up 7.87 years (SD = 1.51; range 5.17–11.58). The mean time from start of treatment until the follow‐up measurement was 3.9 years (SD = 1.11; range 2.3–6.7). No children were diagnosed with neither Williams syndrome nor fetal alcohol syndrome, for which indiscriminate social behavior is a frequent phenotype (Jones et al., 2000). All children had a developmental age of at least 9 months. There were 19 children with intellectual disability (IQ < 70), who neither significantly differed from the other children in mean levels of DSEB continuous scores (Mann‐Whitney U = 842.5, p = .27) nor in scoring above cut‐off (χ2 = 0.17; p = .68) at start of treatment.
Table 1.
Characteristics of the sample and descriptive statistics of main study variables (N = 124)
| Baseline | Follow‐up | |
|---|---|---|
| Age, mean (SD) | 4.06 (0.89) | 7.87 (1.51) |
| Gender, boy n (%) | 102 (82.3) | |
| Ethnicity, non‐Western n (%)[Link] | 36 (29) | |
| IQ, n = 103, mean (SD) | 93.44 (18.55) | |
| Neglect/emotional maltreatment, n (%) | 31 (25) | |
| Effortful control, n = 104, mean (SD) | 4.21 (0.68) | |
| DSEB, DAI mean (SD) | 1.65 (1.79) | 1.48 (1.68) |
| DSEB, DAI cut‐off, n (%) | 47 (37.9) | 43 (34.7) |
| Stranger Approach, n = 116, mean (SD) | 1.16 (1.06) | |
| SatD, n = 103, n (%) | 50 (48.5) | |
| Psychiatric disorders (present); n = 123 | ||
| ADHD, n (%) | 42 (34.1) | |
| ODD, n (%) | 11 (8.9) | |
| ASD, n (%) | 58 (47.2) | |
| Depression or Anxiety disorder, n (%) | 10 (8.1) | |
| Trauma disorder, n (%) | 4 (3.3) | |
DSEB, disinhibited social engagement behavior; DAI, disturbances of attachment interview; SatD, stranger at the door procedure; ADHD, attention deficit/hyperactivity disorder; ODD, oppositional defiant disorder; ASD, autism spectrum disorder.
Non‐Western origin was defined as: child and/or one or more biological parents born in Africa, Turkey, Latin America or Asia, excluding Indonesia and Japan, conform the criteria of Statistics Netherlands.
Of the 124 participants, 60 children were referred for treatment of behavioral problems, 32 children for treatment of social‐emotional problems, and 32 children for treatment of both social‐emotional and behavioral problems. Additionally, 73 children (59%) were referred with comorbid speech and/or language problems. None of the children were specifically referred for treatment of DSEB. Children and families were offered multimodal treatment. A family worker and a psychologist addressed the developmental needs and specific social‐emotional and behavioral problems of the children by means of parenting support and parent training. In order to practice social, behavioral, and other developmental skills, 74% of the children followed additional group‐treatment. If the therapeutic workers identified discrete disinhibited behaviors as problematic, these were included in the treatment plan. Some children had speech therapy, physiotherapy, or (parent‐) child psychotherapy to address specific parent‐child relation problems or trauma. Parents signed informed consent for use of the collected data for scientific research. The study was approved by the VU University Medical Center Medical Ethical Review Board (protocol 2013.358). A subsample of the children in this study was also reported on for a cross‐sectional study on disordered attachment behavior in referred home‐reared children (Scheper et al., 2016).
Measures
Demographic and social‐economic characteristics were examined at baseline. Parents reported on age, gender, and country of birth of the child as well as their own country of birth. A non‐Western origin was defined as: child and/or one or more biological parents born in Africa, Turkey, Latin America or Asia, excluding Indonesia and Japan, consistent with the criteria of Statistics Netherlands (Centraal Bureau voor Statistiek, 2000). Furthermore, parents reported single parenting and whether there had been serious financial problems in the last 6 months. Intelligence quotient (IQ) was examined at follow‐up by combining two subtests of the WISC‐R, vocabulary, and block design with the highest correlation with full‐scale IQ score (0.88) (Silverstein, 1975). For 21 children an IQ could not be assessed using the WISC‐R; eight children were not present at follow‐up and in 13 children no reliable scores could be made (due to noncooperative behavior or recently being tested with the same test). Of these 21 children, there was documentation in patient records during treatment or recent IQ‐testing, which was used to estimate a cut‐off score for intellectual disability with IQ below 70 (10 children) and IQ above 70 (11 children).
The Course of DSEB was assessed at baseline and follow‐up with the Disturbances of Attachment Interview (DAI). The DAI (Smyke & Zeanah, 1999) is a semi‐structured interview with five items assessing inhibited attachment behavior (items 1–5), three items assessing DSEB (items 6, 7, and 8), and four items assessing secure base distortions (items 9, 10, 11, and 12). A full characterization of the sample on DAI items is given in Appendix S1. The following three items were used to assess DSEB: (a) rarely checks back with caregiver after venturing away, especially in unfamiliar settings, (b). rarely exhibits reticence with unfamiliar adults, (c) willing to go off readily with relative strangers. The scores range between 0 (indicating no evidence for symptom behavior), 1 (indicating some evidence), and 2 (indicating definite evidence). Parent‐reported DSEB was analyzed both as a continuous (scale ranging from 0 to 6) and a dichotomous variable (cut‐off score). For the cut‐off score, the criteria described by Gleason et al. (2011) were used, as this was endorsed by principal component analysis in previous research (Scheper et al., 2016): two or more DAI items assessing DSEB with a score 1 or 2 for a positive cut‐off score on DSEB. Coders (FYS, CG) were blind to other case details. The researchers showed high inter‐rater reliability on DSEB: on scale level 0.89–0.91 and on classification level (cut‐off) 0.94–1.0. The Cronbach's α in this sample was .70.
At follow‐up, two observational measures of DSEB were added to the assessment. In order to assess whether the child would go off with a stranger, the ‘Stranger at the Door’ (SatD) procedure (Gleason et al., 2011; Zeanah, Smyke, Koga, & Carlson, 2005) was applied. Before the home visit, parents were carefully briefed about the SatD procedure. They were instructed not to give verbal or nonverbal signals to the child when the experimenter would come at their door at a prearranged time. The child would be allowed to answer the door for the home visitor, unknown to the child, who would say to the child ‘Hello, come with me, I have something to show you.’ If the child actually left with the experimenter, the parent and experimenter together debriefed the child about the prearrangement between the researcher and the parent, encouraging children to refer to the parent if in the future strangers would invite them to step out of the door. The SatD procedure was developed for younger children (54 months), whose response was coded as leaving with the stranger (DSEB) or not leaving with the stranger (no DSEB). As the current follow‐up sample was older, the scoring was elaborated with an additional option. A score of zero was given for not leaving with the stranger, a score of one was given for leaving after making (eye) contact with the parent, and a score of two was given for leaving without (eye) contact with the parent. Observed DSEB with the SatD procedure was scored as present when there was a score 2 and not present when there was a score 0 or 1. There were 21 children in which the SatD procedure could not be completed; eight children were not present at measurement, in 10 children the procedure was not completed (e.g. the child refused to open the door, the setting was unsuitable), and in three children the primary caregiver did not give final consent for this procedure. During the home visit, DSEB was also measured by use of a structured observational schedule developed for reactive attachment disorder (McLaughlin, Espie, & Minnis, 2010; Vervoort, De Schipper, Bosmans, & Verschueren, 2013). For this study, the stranger approach scale was used, which showed a strong association with DSEB in the study of Vervoort et al. (2013). The child's approach to the experimenter during home visit was scored. The scale includes the following items ‘Does the child look at the stranger as if to invite a conversation’, ‘Does the child initiate conversation with the stranger as if previously familiar?’, ‘Does the child move towards and approach the stranger?’, and ‘Does the child display caution or shyness with the stranger?’ (reverse scored). After the home visit, the experimenter scored each item by ‘yes’ (1) or ‘no’ (0) indicating the presence or absence of observed DSEB by stranger approach, leading to a total score from 0 to 4. In eight children the observation schedule could not be completed because the child was not present. Cronbach's alpha for this 4‐item scale was .69 in the study of Vervoort et al. (2013) and in the present study .61.
Neglect/emotional maltreatment was determined utilizing the Maltreatment Classification System, MCS (Barnett, Manly, & Cicchetti, 1993; Manly, 2005). Based on operational criteria, the MCS distinguishes different types of maltreatment (e.g. physical abuse, emotional maltreatment including emotional abuse and neglect, physical neglect with lack of supervision or lack of basic needs). The MCS is designed to code incidents reported in child protection services records on maltreatment and has as such been described as reliable and valid (Cicchetti, Rogosch, & Thibodeau, 2012; English et al., 2005; Manly, 2005). In the current study, the MCS was applied to records containing assessment of safety using parent interview and information on abuse and neglect shared by former health care providers and child protection agencies. Based on the operational criteria of the MCS, only the scores ‘definitely present’ were used in this study. The scores on emotional maltreatment (including emotional abuse and neglect) and physical neglect were combined for analyses on neglect/emotional maltreatment. The average agreement of raters (kappa) was .70. In case of disagreement, coders discussed and consulted with a third researcher to get consensus.
Effortful control was assessed at baseline by use of the ‘Children's Behavior Questionnaire’ (CBQ)‐short form (Putnam & Rothbart, 2006) for children aged 3–7. The Dutch translation of the CBQ‐short form consists of 94 items on temperament and is rated on a scale ranging from 1 (never) to 7 (always), or when the child was not observed in the situation described for the past 2 weeks as ‘not applicable’. The broad dimension of effortful control consists of 26 items, addressing children's self‐regulation of emotional reactivity and behavior (Rothbart, Ahadi, Hershey, & Fisher, 2001). Cronbach's alpha was .74, revealing adequate internal consistency.
Psychiatric disorders were assessed at follow‐up by interviewing the children and their parents with the Kiddie‐Schedule for Affective Disorders and Schizophrenia for School‐Age Children Present and Lifetime Version (K‐SADS‐PL DSM‐5 November 2016). This is a semi‐structured diagnostic interview measuring DSM‐5 disorders (Kaufman et al., 2016). The K‐SADS‐PL 2009, which uses the same questions for externalizing disorders as the K‐SADS‐PL DSM‐5 (November 2016), showed good validity (Jarbin, Andersson, Rastam, & Ivarsson, 2017). Classifications were given if the child met criteria for a current diagnosis. Interviews were conducted by researchers (trained at Curium‐Leiden University Medical Center), under supervision of a child psychiatrist (FYS). Most assessments were conducted at home. The interviewers were instructed not to use prompts that were inappropriate for young children and to take into account whether any symptom was above and beyond of what is expected from the child, according to developmental age. If it was not possible to make a definite classification after the home visit, the interviewer called parents and sometimes teachers to obtain further information. In one case, the interview was not completed and was therefore left out of analyses. Final classifications were discussed by the clinical team (including FS and CG) and made by expert consensus. There were no children meeting criteria for CD at the follow‐up measurement. Therefore, only the classifications of ADHD, ODD, and ASD were used. ADHD and ODD were combined to determine the presence of psychiatric disorders with externalizing behavior. ADHD was also used as a separate category in analyses.
Data analysis
Descriptive statistics using cut‐off scores for parent‐reported DSEB at baseline and follow‐up were used to construct groups with different patterns in course of DSEB: persisters (DSEB at baseline and follow‐up), desisters (DSEB at baseline, but not at follow‐up), de novo manifestations of DSEB (only DSEB at follow‐up), and children remaining below cut‐off levels of DSEB at both measurements (no DSEB).
Associations between the study variables were determined using Spearman's correlation, point‐biserial correlation, and Χ2 tests. Associations between parent‐reported DSEB and observational assessments of DSEB were also examined by use of regression analyses to account for possible confounding by ASD. The additive value of the two observational assessments was evaluated in relation to the parent‐reported DSEB variable at follow‐up by use of logistic regression analysis. With (cut‐off) parent‐reported DSEB as the dependent variable, stranger approach and SatD were entered as independent variables. Parent‐reported DSEB at follow‐up was triangulated with the two observational measures by counting an above cut‐off score on the disinhibited items of the DAI only as positive if either the SatD was positive, or stranger approach scored 2 or higher. The cut‐off variable of substantiated parent‐reported DSEB was examined in relation with neglect/emotional maltreatment, effortful control, and psychiatric disorders.
In order to examine moderation, logistic regression analysis was used with parent‐reported DSEB at baseline as the dependent variable. Neglect/emotional maltreatment was entered first, then effortful control was entered as independent variable, and finally an interaction term was added. The same analysis was applied with parent‐reported DSEB at follow‐up as dependent variable, and also with substantiated parent‐reported DSEB. These analyses controlled for age, gender, ethnicity, and IQ. Furthermore, the four different groups with different patterns in course of DSEB were investigated in relation to neglect/emotional maltreatment in early childhood by using a Χ2 test, and on differences in the level of effortful control by use of a one‐way ANOVA.
A logistic regression analysis tested prediction by baseline parent‐reported DSEB of ADHD/ODD and ADHD without ODD at follow‐up, controlling for age, gender, ethnicity, IQ, and ASD. Furthermore, the four different groups with different patterns in course of DSEB were examined in relation to ADHD/ODD, as well as to ADHD without ODD, and ASD, by use of Χ2 tests.
Results
Course of DSEB
There was a significant positive correlation between the level of parent‐reported DSEB (continuous) at baseline and follow‐up (Table 2). At baseline, parents reported DSEB above cut‐off level in 47 children (38%). At follow‐up, parents reported DSEB above cut‐off level in 43 children (35%). Observation during the SatD procedure identified 50 children (48% of n = 104) who left with a stranger, resulting in a positive coding of DSEB on the SatD (Table 1). Persisting DSEB was found in 22% of the 124 children (Figure 1). Of the children with parent‐reported DSEB above cut‐off level at baseline (n = 47), 27 (57%) persisted in DSEB above cut‐off level (persisters). Of the children without parent‐reported DSEB above cut‐off level at baseline (n = 77), 61 children (79%) remained negative for DSEB (no DSEB) and 16 children (21%) were reported with de novo DSEB at follow‐up assessment (Figure 1). Descriptive results on main characteristics and study variables of the four groups (persisters, desisters, de novo DSEB, and no DSEB) are presented in Table 3.
Table 2.
Associations of main study variables
| 1. | 2. | 3. | 4. | 5. | 6. | |
|---|---|---|---|---|---|---|
| 1. Baseline DSEB continuous, n = 124 | ||||||
| 2. Follow‐up DSEB continuous, n = 124 | r s = .51*** | |||||
| 3. Stranger Approach, n = 116 | r s = .35*** |
r s = .41*** βASD = .46*** |
||||
| 4. SatD, n = 103 | r pb = .08 |
r pb = .31** βASD = .31** |
r pb = .23* | |||
| 5. Neglect/emotional maltreatment, n = 124 | r pb = .04 | r pb = .01 | r pb = −.06 | Χ2 = 0.54 | ||
| 6. Effortful control, n = 104 | r s = −.13 | r s = −.03 | r s = −.16 | r pb = −.06 | r pb = −.04 | |
| 7. ADHD/ODD, n = 123 | r pb = .25** | r pb = .37*** | r pb = .13 | Χ2 = 0.05 | Χ2 = 1.31 | r pb = −.05 |
| 8. ASD, n = 123 | r pb = .04 | r pb = .11 | r pb = .01 | Χ2 = 0.08 | Χ2 = 5.46* | r pb = .12 |
DSEB, disinhibited social engagement behavior; SatD, stranger at the door procedure; ADHD, attention deficit/hyperactivity disorder; ODD, oppositional defiant disorder; ASD, autism spectrum disorder.
*<.05, **<.01, ***<.001; r s = Spearman's correlation, r pb = Point‐Biserial correlation; βASD = regression coefficient with correction for ASD.
Figure 1.
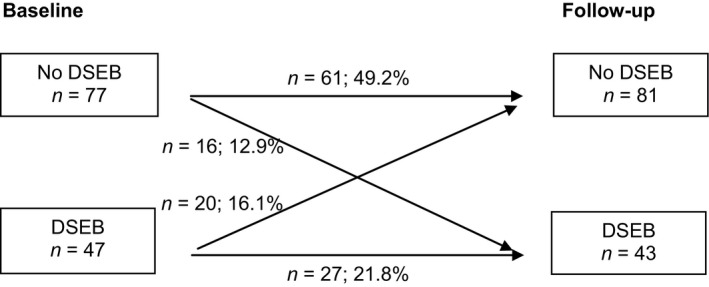
Course of parent‐reported disinhibited social engagement behavior (DSEB) in referred home‐reared children, percentages of n = 124
Table 3.
Descriptive statistics of four groups with a different course in parent‐reported DSEB
|
Persisting DSEB (n = 27) |
Desisting DSEB (n = 20) |
De Novo DSEB (n = 16) |
No DSEB (n = 61) |
|
|---|---|---|---|---|
| Age, M (SD) | 4.31 (0.92) | 3.98 (0.88) | 4.33 (0.88) | 3.91 (0.87) |
| Boy, n (%) | 20 (74) | 16 (80) | 15 (94) | 51 (84) |
| Non‐Western ethnicity, n (%) | 6 (22.2) | 4 (20) | 4 (25) | 22 (36.1) |
| IQ, M (SD) | 99.5 (18.0) | 90.8 (17.6) | 85.3 (21.4) | 94.86 (17.7) |
| Neglect/emotional maltreatment, n (%) | 8 (29.6) | 5 (25.0) | 3 (18.8) | 15 (24.6) |
| Effortful control, M (SD) |
(n = 21) 4.26 (0.63) |
(n = 16) 4.06 (1.04) |
(n = 15) 4.36 (0.33) |
(n = 52) 4.19 (0.64) |
| SatD, n (%) |
(n = 23) 14 (61) |
(n = 18) 8 (44) |
(n = 15) 12 (80) |
(n = 47) 16 (34) |
| Stranger approach, M (SD) |
(n = 25) 1.8 (1.08) |
(n = 18) 1.17 (0.92) |
(n = 15) 1.83 (1.22) |
(n = 58) 0.72 (0.83) |
| ADHD/ODD, n (%) |
(n = 27) 16 (59) |
(n = 20) 8 (40) |
(n = 16) 8 (50) |
(n = 60) 13 (21.7) |
| ADHD without ODD, n (%) | 12 (44) | 4 (20) | 8 (50) | 10 (17) |
| ASD, n (%) | 11 (41) | 11 (55) | 10 (63) | 26 (43) |
DSEB, disinhibited social engagement behavior; SatD, stranger at the door procedure; ADHD, attention deficit/hyperactivity disorder; ODD, oppositional defiant disorder; ASD, autism spectrum disorder.
Relations between parent report and observational assessments of DSEB
Parent‐reported DSEB at baseline (continuous) was positively associated with observed stranger approach, but did not significantly predict leaving with a stranger during the SatD procedure (Table 2). Parent‐reported DSEB at follow‐up (continuous) was positively associated with stranger approach as well as with leaving with a stranger during the SatD procedure, also after controlling for ASD (Table 2). Consistent with the continuous scores, children with parent‐reported DSEB above cut‐off level at follow‐up were observed to go off with a stranger significantly more often (68%; χ2(1, n = 103) = 9.53, p = .002) during the SatD procedure than children without parent‐reported DSEB (37%). Also, parent‐reported DSEB above cut‐off level at follow‐up was associated with stranger approach (r pb = .43, p < .001). Stranger approach and the SatD procedure showed both unique association with parent‐reported DSEB at follow‐up (resp. OR 2.35, p = .001, [95% Cl: 1.42–3.88]; OR 2.92, p = .03, 95% Cl [1.13–7.05]).
Because there were 16 children with de novo DSEB reported by parents in middle childhood, the four groups were compared in relation to observational measures of DSEB. A Kruskall‐Wallis test showed a difference between the four groups on level of stranger approach (χ2(3, n = 116) = 25.54, p < .001). Post hoc analysis with Mann‐Whitney tests showed that children with persisting DSEB as well as children with de novo DSEB displayed more stranger approach than the children without DSEB (resp. U = 298.5, p < .001 and U = 222.5, p = .002). The groups also differed on the outcome of the SatD procedure (χ2(3, n = 103) = 11.42, p = .01). Children with persisting DSEB more often left with a stranger during the SatD procedure (61%) than children without DSEB (34%; χ2(1, n = 70) = 4.54, p = .03). Also, children with de novo DSEB left with a stranger more often than children without DSEB (χ2(1, n = 62) = 9.70, p = .002).
Relation with neglect/emotional maltreatment and child temperament
Maltreatment, including physical abuse/neglect and emotional abuse/neglect, was found in 29% (n = 36). Neglect and/or emotional maltreatment was found in 31 children (25%; Table 1).
Neglect/emotional maltreatment was not significantly associated with DSEB, based on continuous scores on parent‐reported DSEB and observational measures of DSEB (Table 2). Furthermore, children with and without substantiated parent‐reported DSEB at follow‐up did not differ in neglect/emotional (χ2(1, n = 116) = 0.70, p = .40). Also, neglect/emotional maltreatment in the four groups (Table 3) did not differ in prevalence (χ2(3, n = 124) = 0.65, p = .89).
Regarding child temperament, parent‐reported DSEB (continuous) at baseline and follow‐up was not significantly associated with the level of effortful control in current follow‐up sample (Table 2). There was no difference between children with and without an above cut‐off score on substantiated parent‐reported DSEB in mean levels of effortful control (t(98) = −0.48, p = .63). In addition, the interaction between effortful control and neglect/emotional maltreatment was not significantly associated with parent‐reported DSEB. Interaction terms were not significant for parent‐reported DSEB at baseline (OR 1.2, p = .83, 95% CI [0.31–4.33]), parent‐reported DSEB at follow‐up (OR 1.2, p = .94, 95% CI [0.25–4.55]), nor for substantiated parent‐reported DSEB (OR 0.39, p = .24, 95% CI [0.08–1.86). Finally, there was no difference between the four groups (persisters, desisters, de novo DSEB, and no DSEB) in mean levels of effortful control (F(3, 100) = 0.55, p = .65).
Relation with psychiatric disorders: ADHD, ODD, and ASD
There were 88 children (72%) meeting DSM‐classification criteria for psychiatric disorders at follow‐up, listed in Table 1. The most prevalent disorder was ASD (n = 58, 47%). There were 45 children with ADHD and/or ODD, of which 34 children had only ADHD, three children had only ODD, and eight children had comorbid ADHD and ODD. There were no children with CD (Table 1).
At baseline and follow‐up, a higher score on parent‐reported DSEB (continuous) was significantly associated with a classification of ADHD/ODD (Table 2). Also after controlling for ASD, a higher score on parent‐reported DSEB (continuous) at baseline was significantly associated with ADHD/ODD 4 years later (OR 1.34, p = .017, 95% CI [1.05–1.70]). Also, parent‐reported DSEB above cut‐off level predicted ADHD/ODD 4 years later, with the odds at follow‐up being 3.05 times larger for children with above cut‐off parent‐reported DSEB than for children below cut‐off at baseline (Table 4). For children who did not meet criteria for ODD, parent‐reported DSEB at baseline (continuous and above cut‐off level) was not significantly associated with ADHD (resp. r pb = .11, p = .23 and χ2 (1, n = 123) = 3.22, p = .07). Parent‐reported DSEB at follow‐up (continuous and above cut‐off level) was significantly associated with ADHD alone (resp. r pb = .49, p < .001 and χ2 (1, n = 123) = 12.4, p < .001). Children with substantiated parent‐reported DSEB at follow‐up were more often classified with ADHD/ODD (χ2(1, n = 115) = 3.84, p = .05), as well as classified with ADHD without ODD (χ2(1, n = 115) = 5.58, p = .02) than children without substantiated parent‐reported DSEB.
Table 4.
Multiple logistic regression analysis predicting ADHD/ODD, with correction for age, ethnicity, gender, and IQ (n = 123)
| B | SE | Significance (p) | OR | 95% CI | |
|---|---|---|---|---|---|
| Parent‐reported DSEB baseline, cut‐off | 1.12 | 0.43 | .01 | 3.05 | 1.31–7.10 |
| ASD | −0.21 | 0.43 | .63 | 0.810 | 0.35–1.89 |
| R 2 = .218 |
ADHD, attention deficit/hyperactivity disorder; ODD, oppositional defiant disorder; DSEB, disinhibited social engagement behavior; ASD, autism spectrum disorder.
At baseline and at follow‐up, parent‐reported DSEB (continuous) was not associated with ASD (Table 2). Consistent with the continuous scores, parent‐reported DSEB above cut‐off level was not associated with ASD (at baseline χ2(1, n = 123) = 0.004, p = .95, and at follow‐up χ2(1, n = 123) = 0.08, p = .78). Neither a positive score on the SatD procedure nor the level of stranger approach were associated with ASD (Table 2). Also, substantiated parent‐reported DSEB at follow‐up was not associated with ASD (χ2(1, n = 115) = 0.02, p = .89).
The course of parent‐reported DSEB was not significantly associated with ASD (χ 2 (3, n = 123) = 2.80, p = .42), but was significantly related to psychiatric disorders with externalizing behavior (ADHD/ODD). Prevalence of these disorders differed between the four groups (χ2 (3, n = 123) = 13.08, p = .004). Post hoc analysis showed a higher prevalence of ADHD/ODD (59%) in children with persisting DSEB than in children without DSEB (22%). The prevalence of ADHD without ODD also differed between the four groups (χ2 (3, n = 123) = 12.01, p = .007). Post hoc analysis showed a higher prevalence of ADHD (without ODD) in children with persisting DSEB (44%) and in children with de novo DSEB (50%) than in children without DSEB (17%). Of the 16 children with de novo DSEB, 12 children met criteria for ADHD or ASD, and none of these children had reports of neglect/emotional maltreatment. Six children met criteria for concurrent classifications of ADHD and ASD, four children were classified with ASD alone, two children with ADHD alone, and no children had ODD.
Discussion
According to this follow‐up study in clinically referred home‐reared children, findings showed that more than half of the children with DSEB in early childhood persisted in this behavior in middle childhood, when measured by parent interview on average 4 years after treatment of emotional and behavioral problems at preschool age. While parent report may be subject to various forms of bias that may partly explain these results, the significant associations between parent report and observation of DSEB support validity of parent report, lending credibility to the longitudinal findings. Parent‐reported DSEB at preschool age was related to ADHD/ODD in middle childhood. This study adds important longitudinal findings to what is already known about DSEB in children raised by biological parents.
Desistence of DSEB was found in 43% (n = 20) and could be explained by parents interpreting social aberrant behaviors differently over time, leading to a decline in parent‐reported DSEB (Rutter et al., 2007). But it is also possible that children learned to adjust in social behavior due to experiences and early intervention. As DSEB was not the main focus in treatment in this sample and there was no control group of children without treatment, the impact of early intervention on DSEB was unknown. Guyon‐Harris et al. (2018) found that placement of children in stable families at early age after institutionalized care was related to a decrease in DSEB, suggesting that DSEB may be modified by early improvements in the child‐rearing situation.
Persistence of parent‐reported DSEB was found in earlier research, but mainly in institutionalized and post‐insititutionalized children (Zeanah et al., 2016). The finding that 57% of the children with parent‐reported DSEB at baseline persisted in this behavior at follow‐up, is in line with the rate of persistence found in (post) institutionalized children (54%) (Rutter et al., 2007). However, it is much higher than in a group of adopted children (6.5%) without institutional rearing (Rutter et al., 2007).
Reported neglect or emotional maltreatment was found in 25% of the children in the current study. However, we found no association between (the course of) DSEB and neglect/emotional maltreatment of the children. It is possible that neglect or emotional maltreatment in early years of life was not identified in the clinical records of some of the children with DSEB. Although the direct association between early neglect/emotional maltreatment and DSEB was not significant, the high percentage of inadequate care underlines the high level of risk in the sample. It should be noted that the emotional‐ and behavioral problems at preschool age that were grounds for referral may indicate the presence of risk factors that might also predispose to DSEB. An avenue for further research is to broaden the set of possible adverse childhood experiences related to DSEB. In an earlier study, socially indiscriminate attachment behavior in home‐reared infants was associated with maternal disorientation in disruptive affective communication (Lyons‐Ruth et al., 2009). These disruptive emotional interactions between a primary caregiver and child, which could influence the behavior of the child, are not always captured within the concept of child maltreatment/neglect. As we reported earlier, more DSEB was associated with more parenting stress in treatment referred home‐reared and foster care children (Scheper et al., 2016). It might well be possible that higher parenting stress concurs with disruptive emotional interactions between parent and child that could underlie DSEB in home‐reared children.
Prior research also raises questions about neurodevelopmental problems in children with DSEB, possibly due to interplay between biological and environmental factors. In earlier studies, DSEB has been associated with problems in self‐regulation, including low attentional and inhibitory control as measured by laboratory assessments (Bruce et al., 2009; Gleason et al., 2011; Pears et al., 2010). Findings in current study showed no association between (the course) DSEB and the level of effortful control, as reported by parents. In addition, effortful control did not moderate the association between neglect/emotional maltreatment and parent‐reported DSEB.
Results of the current study did show that children with persisting DSEB, as well as children with de novo DSEB, had a higher prevalence of ADHD than children without DSEB. This is consistent with evidence for comorbidity of DSED and ADHD (Gleason et al., 2011; Pritchett et al., 2013). However, there is also a possibility that parent‐reported DSEB was miss‐classified in some of the children with ADHD, because ADHD/ODD was not associated with the observational measures for DSEB. Parent‐reported DSEB in early childhood was associated with ADHD/ODD but not with ADHD alone (without ODD) at follow‐up, suggesting that parent‐reported DSEB in early childhood is associated with mixed externalizing behaviors only. DSEB and ASD were not associated at follow‐up from intervention, which is in line with a previous study showing no association between DSEB and symptoms of ASD (Giltaij et al., 2015). These findings suggest that the aberrant social behaviors of DSEB and ASD can be reliably discriminated when standardized assessment procedures are used and that DSEB can be comorbid with ASD.
Unexpectedly, parents reported de novo manifestations of DSEB at follow‐up for 16 children (13%). Three of these children had reports of neglect or emotional maltreatment in their clinical records. Twelve children met criteria for ADHD or ASD without reports of neglect or emotional maltreatment. De novo manifestations were so scarce in an earlier follow‐up study of DSEB in post‐institutionalized and adopted children (4%–5%), that it was not presumed to be relevant (Rutter et al., 2007). The children with de novo DSEB in current study not only scored above cut‐off level on parent reports, but also left more often with a stranger during the SatD procedure and scored more stranger approach during observation than children without parent‐reported DSEB. De novo DSEB might have occurred because at intake, other problems overshadowed the perception of parents of DSEB. Findings underscore the importance of using multiple assessments and informants on these behaviors (Giltaij, Sterkenburg, & Schuengel, 2017; Zeanah et al., 2016).
Findings should be interpreted in light of study limitations. In the current study, no full diagnostic clinical assessment of DSED was undertaken, which would have required information from multiple informants and observation sessions at the two measurement occasions. Because we only used parent reports on DSEB at baseline, we cannot report on the course of observed DSEB. Also, the sample sizes in the DSEB course subgroups were small. There is a dearth of validity evidence for measurement of DSEB in middle childhood and beyond (Vervoort et al., 2013). The SatD procedure was adapted to suit the age range of the study sample. However, 34% of the children without parent‐reported DSEB at both time measurements did leave with a stranger without checking back with the caregiver. Also, the outcome on the SatD was not related to early emerging DSEB (r pb = .08). The validity of this test for middle childhood awaits additional research with other informants and observations. The results with the observational scale stranger approach should be viewed with caution as internal consistency bordered on a low value. However, the stranger approach did indicate prediction from baseline DSEB (r s = .35) and differentiation of the four change groups. Further work is needed in different kinds of samples, but initial results indicate good concurrent and predictive validity in relation to parent report in this age range. Given the importance of multimethod assessment of DSEB, further work to establish clinically relevant cut points for the stranger approach assessment is warranted. It is important to be able to distinguish between high levels of non‐impairing sociability and impairing disinhibited behavior.
The lack of relations between DSEB and neglect/emotional maltreatment, as well as effortful control, in the current study may be due to limitations in measurement. The MCS was designed for child protection services records and not designed for coding clinical records. In the current study, the MCS was applied to records containing assessment of safety using parent interview and information on abuse and neglect shared by former health care providers and child protection agencies, but child protection service records itself could not be accessed. It is possible that neglect or emotional maltreatment in early years of life were missed in children with DSEB. Also, there was very limited information on parent‐child separations and quality of care in the first 2 years of life, the period when prior research has found that DSED first appears. An important limitation regarding measurement of effortful control is that only parent reports were used. In other studies laboratory assessments were used (Bruce et al., 2009; Gleason et al., 2011; Pears et al., 2010) or a different parent questionnaire (Gorter et al., 2017). The use of several different instruments examining effortful control hampers comparison between studies.
Furthermore, ascertainment bias occurred as not all parents agreed to participate. Differential attrition occurred as children participating at follow‐up had less often a history of emotional neglect/maltreatment, were less often reared in a single‐parent household and were less likely of non‐Western origin than children who did not participate at follow‐up. This may have affected the strength of the associations at follow‐up, especially with externalizing disorders. Boys formed the majority in the study sample, who are more likely to exhibit externalizing behaviors. The stability and comorbidity patterns for girls with DSEB may differ and need to be explored further. DSEB was assessed among children referred for a variety of other behavioral and emotional disorders, including ADHD, ODD, and ASD. This difference in sample characteristics leaves open the question of whether DSEB among home‐reared children, in the context of other diagnoses, represents something different than the behavior in children with DSED that appears early in life among post‐institutionalized children. Kay et al. (2016) reported that the lack of a direct association between DSEB and maltreatment in a noninstitutionalized group suggests a complex developmental pathway to DSED. Longitudinal studies comparing young home‐reared and post‐institutionally reared children are needed, including assessment of comorbid psychiatric diagnoses, quasi‐autistic behaviors that were previously associated with DSEB, effortful control, as well as assessments on parent‐child interaction and information on previous separations and quality of care in the first 2 years of life. Future studies may not only aid in understanding of the factors that are involved in the onset and course of DSEB but also offer treatment perspectives for home‐reared children.
In conclusion, the longitudinal findings of current study suggest clinical relevance of DSEB in home‐reared children referred for mental health care. Future research should focus on advancing clinical understanding of DSEB in home‐reared children. Regarding clinical implications, DSEB could be overshadowed by comorbid ADHD symptoms and lead to selective treatment of ADHD symptoms in children without focus on parent‐child relation and social interaction, as has been discussed by Pritchett et al. (2013). On the other hand, a lack of understanding of etiology of DSEB in clinically referred children asks for cautious interpretation of DSEB in home‐reared children. DSEB should not be used as an indicator for maltreatment, as was also noted for disorganized attachment (Granqvist et al., 2017). When DSEB is reported in early childhood, maltreatment should be carefully investigated as well as the quality of the parent‐child relationship, parenting behavior, and observation of child behavior. Research on treatment of DSEB is scarce, but it has been suggested that intervention focused on behavior regarding social boundaries and self‐control might be effective in children with DSEB (Zeanah & Gleason, 2015). A recent case‐report shows support for an attachment based parent‐focused behavior management treatment (Dickmann & Allen, 2017). We therefore propose that DSEB should be considered in assessment and treatment procedures in referred young children, using information from parents about the behaviors as well as parent‐child observation and interaction with relative strangers.
Key point.
Disinhibited social engagement behavior (DSEB) without evidence for extremes of inadequate caregiving does not qualify for a clinical diagnosis of disorder.
More than half of the parents who reported notable DSEB in clinically referred home‐reared preschoolers did so again four years later.
Disinhibited social engagement behavior showed moderate consistency across caregiver report, independent home observation, and response to the Stranger‐at‐the‐Door test.
Disinhibited social engagement behavior was not found related to emotional maltreatment/neglect, but parent‐reported DSEB was associated with externalizing problems.
Despite unclear etiology, DSEB in home‐reared children has a place in diagnostic case formulation.
Supporting information
Appendix S1. Full characterization at baseline on items from the Disturbances of Attachment Interview.
Acknowledgements
The authors are grateful to the caregivers and children who participated in this study, the staff of MOC ‘t Kabouterhuis, research students, Stichting Villa Johanna, and Netwerk Effectieve Jeugdhulp Amsterdam (NEJA). The authors have declared that they have no competing or potential conflicts of interest.
Conflict of interest statement: No conflicts declared.
References
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders‐ fifth edition (DSM‐5). Washington DC: Author. [Google Scholar]
- Bakermans‐Kranenburg, M.J. , Steele, H. , Zeanah, C.H. , Muhamedrahimov, R.J. , Vorria, P. , Dobrova‐Krol, N.A. , … & Gunnar, M.R. (2011). Attachment and emotional development in institutional care: Characteristics and catch‐up. Monographs of the Society for Research in Child Development, 76, 62–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett, D. , Manly, J.T. , & Cicchetti, D. (1993). Defining child maltreatment: The interface between policy and research, Vol. 8 Norwood, NJ: Ablex. [Google Scholar]
- Bruce, J. , Tarullo, A.R. , & Gunnar, M.R. (2009). Disinhibited social behavior among internationally adopted children. Development and Psychopathology, 21, 157–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centraal Bureau voor Statistiek . (2000, 2012). Standaarddefinitie Allochtonen.
- Chisholm, K. (1998). A three year follow‐up of attachment and indiscriminate friendliness in children adopted from Romanian orphanages. Child Development, 69, 1092–1106. [PubMed] [Google Scholar]
- Cicchetti, D. , Rogosch, F.A. , & Thibodeau, E.L. (2012). The effects of child maltreatment on early signs of antisocial behavior: Genetic moderation by tryptophan hydroxylase, serotonin transporter, and monoamine oxidase A genes. Development and Psychopathology, 24, 907–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson, C. , O'Hare, A. , Mactaggart, F. , Green, J. , Young, D. , Gillberg, C. , & Minnis, H. (2015). Social relationship difficulties in autism and reactive attachment disorder: improving diagnostic validity through structured assessment. Research in Developmental Disability, 40, 63–72. [DOI] [PubMed] [Google Scholar]
- Dickmann, C.R. , & Allen, B. (2017). Parent–child interaction therapy for the treatment of disinhibited social engagement disorder: A case report. Evidence‐Based Practice in Child and Adolescent Mental Health, 2, 19–29. [Google Scholar]
- English, D.J. , Upadhyaya, M.P. , Litrownik, A.J. , Marshall, J.M. , Runyan, D.K. , Graham, J.C. , & Dubowitz, H. (2005). Maltreatment's wake: The relationship of maltreatment dimensions to child outcomes. Child Abuse and Neglect, 29, 597–619. [DOI] [PubMed] [Google Scholar]
- Giltaij, H.P. , Sterkenburg, P.S. , & Schuengel, C. (2015). Psychiatric diagnostic screening of social maladaptive behaviour in children with mild intellectual disability: Differentiating disordered attachment and pervasive developmental disorder behaviour. Journal of Intellectual Disability Research, 59, 138–149. [DOI] [PubMed] [Google Scholar]
- Giltaij, H.P. , Sterkenburg, P.S. , & Schuengel, C. (2017). Convergence between observations and interviews in clinical diagnosis of reactive attachment disorder and disinhibited social engagement disorder. Clinical Child Psychology and Psychiatry, 22, 603–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gleason, M.M. , Fox, N.A. , Drury, S. , Smyke, A. , Egger, H.L. , Nelson, C.A., III , … & Zeanah, C.H. (2011). Validity of evidence‐derived criteria for reactive attachment disorder: Indiscriminately social/disinhibited and emotionally withdrawn/inhibited types. Journal of the American Academy of Child and Adolescent Psychiatry, 50, 216–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorter, B. , Helder, E.J. , Oh, Y.I. , & Gunnoe, M.L. (2017). Are disinhibited social behaviors among internationally adopted children mediated by the attachment environment or by children's difficulties with inhibitory control? Adoption Quarterly, 20, 291–308. 10.1080/10926755.2017.1349699. [DOI] [Google Scholar]
- Granqvist, P. , Sroufe, L.A. , Dozier, M. , Hesse, E. , Steele, M. , van Ijzendoorn, M. , … & Duschinsky, R. (2017). Disorganized attachment in infancy: A review of the phenomenon and its implications for clinicians and policy‐makers. Attachment and Human Development, 19, 534–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyon‐Harris, K.L. , Humphreys, K.L. , Fox, N.A. , Nelson, C.A. , & Zeanah, C.H. (2018). Course of disinhibited social engagement disorder from early childhood to early adolescence. Journal of the American Academy of Child and Adolescent Psychiatry, 57, 329–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarbin, H. , Andersson, M. , Rastam, M. , & Ivarsson, T. (2017). Predictive validity of the K‐SADS‐PL 2009 version in school‐aged and adolescent outpatients. Nordic Journal of Psychiatry, 71, 270–276. [DOI] [PubMed] [Google Scholar]
- Jones, W. , Bellugi, U. , Lai, Z. , Chiles, M. , Reilly, J. , Lincoln, A. , & Adolphs, R. (2000). Hypersociability in Williams Syndrome. Journal of Cognitive Neuroscience, 12(Suppl 1), 30–46. [DOI] [PubMed] [Google Scholar]
- Kaufman, J. , Birmaher, B. , Axelson, D. , Perepletchikova, F. , Brent, B. , & Ryan, N. (2016). K‐SADS DSM‐5 November 2016. Yale University Child and Adolescent Research and Education (CARE) Western Psychiatric Institute and Clinic: Advanced Center for Intervention and Services Research (ACISR) for Early Onset Mood and Anxiety Disorders.
- Kay, C. , Green, J. , & Sharma, K. (2016). Disinhibited attachment disorder in UK adopted children during middle childhood: Prevalence, validity and possible developmental origin. Journal of Abnormal Child Psychology, 44, 1375–1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawler, J.M. , Koss, K.J. , Doyle, C.M. , & Gunnar, M.R. (2016). The course of early disinhibited social engagement among post‐institutionalized adopted children. Journal of Child Psychology and Psychiatry, 57, 1126–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons‐Ruth, K. , Bureau, J.F. , Riley, C.D. , & Atlas‐Corbett, A.F. (2009). Socially indiscriminate attachment behavior in the Strange Situation: Convergent and discriminant validity in relation to caregiving risk, later behavior problems, and attachment insecurity. Developmental Psychopathology, 21, 355–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manly, J.T. (2005). Advances in research definitions of child maltreatment. Child Abuse and Neglect, 29, 425–439. [DOI] [PubMed] [Google Scholar]
- McLaughlin, A. , Espie, C. , & Minnis, H. (2010). Development of a brief waiting room observation for behaviours typical of reactive attachment disorder. Child and Adolescent Mental Health, 15, 73–79. [DOI] [PubMed] [Google Scholar]
- Minnis, H. , Macmillan, S. , Pritchett, R. , Young, D. , Wallace, B. , Butcher, J. , … & Gillberg, C. (2013). Prevalence of reactive attachment disorder in a deprived population. The British Journal of Psychiatry, 202, 342–346. [DOI] [PubMed] [Google Scholar]
- Minnis, H. , Reekie, J. , Young, D. , O'Connor, T. , Ronald, A. , Gray, A. , & Plomin, R. (2007). Genetic, environmental and gender influences on attachment disorder behaviours. British Journal of Psychiatry, 190, 490–495. [DOI] [PubMed] [Google Scholar]
- Pears, K.C. , Bruce, J. , Fisher, P.A. , & Kim, H.K. (2010). Indiscriminate friendliness in maltreated foster children. Child Maltreatment, 15, 64–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pritchett, R. , Pritchett, J. , Marshall, E. , Davidson, C. , & Minnis, H. (2013). Reactive attachment disorder in the general population: A hidden ESSENCE disorder. The Scientific World Journal, 2013, 818157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam, S.P. , & Rothbart, M.K. (2006). Development of short and very short forms of the Children's Behavior Questionnaire. Journal of Personality Assessment, 87, 102–112. [DOI] [PubMed] [Google Scholar]
- Rothbart, M.K. , Ahadi, S.A. , Hershey, K.L. , & Fisher, P. (2001). Investigations of temperament at three to seven years: The Children's Behavior Questionnaire. Child Development, 72, 1394–1408. [DOI] [PubMed] [Google Scholar]
- Rutter, M. , Colvert, E. , Kreppner, J. , Beckett, C. , Castle, J. , Groothues, C. , … & Sonuga‐Barke, E.J. (2007). Early adolescent outcomes for institutionally deprived and non deprived adoptees. I: Disinhibited attachment. Journal of Child Psychology and Psychiatry, 48, 17–30. [DOI] [PubMed] [Google Scholar]
- Scheper, F.Y. , Abrahamse, M.E. , Jonkman, C.S. , Schuengel, C. , Lindauer, R.J.L. , Vries, A.L.C. , … & Jansen, L.M.C. (2016). Inhibited attachment behaviour and disinhibited social engagement behaviour as relevant concepts in referred home reared children. Child: Care, Health and Development, 42, 544–552. [DOI] [PubMed] [Google Scholar]
- Silverstein, A.B. (1975). Validity of Wisc‐R short forms. Journal of Clinical Psychology, 31, 696–697. [Google Scholar]
- Smyke, A.T. , & Zeanah, C.H. (1999). The Disturbances of Attachment Interview.
- Smyke, A.T. , Zeanah, C.H. , Gleason, M.M. , Drury, S.S. , Fox, N.A. , Nelson, C.A. , & Guthrie, D. (2012). A randomized controlled trial comparing foster care and institutional care for children with signs of reactive attachment disorder. American Journal of Psychiatry, 169, 508–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tizard, B. , & Rees, J. (1975). The effect of early institutional rearing on the behaviour problems and affectional relationships of four‐year‐old children. Journal of Child Psychology and Psychiatry, 16, 61–73. [DOI] [PubMed] [Google Scholar]
- Vervoort, E. , De Schipper, J.C. , Bosmans, G. , & Verschueren, K. (2013). Screening symptoms of reactive attachment disorder: Evidence for measurement invariance and convergent validity. International Journal of Methods in Psychiatric Research, 22, 256–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeanah, C.H. , Chesher, T. , & Boris, N.W. (2016). Practice parameter for the assessment and treatment of children and adolescents with reactive attachment disorder and disinhibited social engagement disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 55, 990–1003. [DOI] [PubMed] [Google Scholar]
- Zeanah, C.H. , & Fox, N.A. (2004). Temperament and attachment disorders. Journal of Clinical Child and Adolescent Psychology, 33, 32–41. [DOI] [PubMed] [Google Scholar]
- Zeanah, C.H. , & Gleason, M.M. (2015). Annual Research Review: Attachment disorders in early childhood ‐ clinical presentation, causes, correlates, and treatment. Journal of Child Psychology and Psychiatry, 56, 207–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeanah, C.H. , Smyke, A.T. , Koga, S.F. , & Carlson, E. (2005). Attachment in institutionalized and community children in Romania. Child Development, 76, 1015–1028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Full characterization at baseline on items from the Disturbances of Attachment Interview.


