Abstract
Aims
To identify the key common components of knowledge transfer and exchange in existing models to facilitate practice developments in health services research.
Background
There are over 60 models of knowledge transfer and exchange designed for various areas of health care. Many of them remain untested and lack guidelines for scaling‐up of successful implementation of research findings and of proven models ensuring that patients have access to optimal health care, guided by current research.
Design
A scoping review was conducted in line with PRISMA guidelines. Key components of knowledge transfer and exchange were identified using thematic analysis and frequency counts.
Data Sources
Six electronic databases were searched for papers published before January 2015 containing four key terms/variants: knowledge, transfer, framework, health care.
Review Methods
Double screening, extraction and coding of the data using thematic analysis were employed to ensure rigour. As further validation stakeholders’ consultation of the findings was performed to ensure accessibility.
Results
Of the 4,288 abstracts, 294 full‐text articles were screened, with 79 articles analysed. Six key components emerged: knowledge transfer and exchange message, Stakeholders and Process components often appeared together, while from two contextual components Inner Context and the wider Social, Cultural and Economic Context, with the wider context less frequently considered. Finally, there was little consideration of the Evaluation of knowledge transfer and exchange activities. In addition, specific operational elements of each component were identified.
Conclusions
The six components offer the basis for knowledge transfer and exchange activities, enabling researchers to more effectively share their work. Further research exploring the potential contribution of the interactions of the components is recommended.
Keywords: evidence‐based practice, health services research, nursing, research implementation, systematic scoping review
Abstract
目的
的在于确定已有模式中知识传递和交流的关键通用组分,以促进卫生服务研究的实践发展。
背景为各种医疗保健领域设计了60多种知识转移和交流模式。当中许多吧没有进行测试,也没有指导方针来既扩大研究结果的成功实施,又没有指导方针来扩大已证模型的成功实施,以便于确保患者在当前研究的指导下获得最佳的医疗保健。
设计
根据PRISMA指南进行了范围综述。采用了主题分析和频率计数来确定知识传递和交流的关键组分。
数据来源
在6个电子数据库中搜索了2015年1月之前发表的论文,其中包含四个关键术语/变体:知识、传递、框架、医疗保健。
综述方法
采用了主题分析对数据进行双重筛选,提取和编码,以便确保严谨性。随着进一步确认,利益相关者对调查结果进行了协商,以确保可访问性。
结果
在4288篇摘要中,筛选了294篇全文文章,分析了79篇文章。出现了6个关键组分:知识传递和交流信息、利益相关者和流程组件经常一起出现、而出现于两个上下文组件——内部语境和更广阔的社会,文化和经济语境、不太经常考虑更广阔的语境。最后,很少考虑对知识传递和交流活动的评估。此外,还确定了每个组分的具体操作要素。
结论
这六个组分为知识传递和交流活动提供了基础,使研究人员能够更有效地共享其工作。建议进一步研究探讨组件交互的潜在贡献。
Why is this research or review needed?
There is lack of studies that inform the application of knowledge transfer and exchange strategies across various healthcare settings to enable evidence‐based practice.
Analysis and synthesis of existing knowledge transfer and exchange frameworks would identify their commonalities and core concepts.
What are the key findings?
Six key components emerged from analysis of 79 articles; the knowledge transfer and exchange Message, Stakeholders and Process, Inner Context, Social, Cultural and Economic Context and Evaluation. Their prevalence varied, especially in relation to the Evaluation of KTE activities.
In addition, specific operational elements of each key component were identified.
How should the findings be used to influence policy/practice/research/education?
The components and the specific operational elements offer guidance for knowledge transfer and exchange activities in applied setting and can serve as a framework within which to evaluate their impact.
1. INTRODUCTION
While the ultimate aim of health research is to inform practice and policy, research findings can only change population health outcomes if adopted and embedded by healthcare systems, organizations and clinicians (Grimshaw, Ward, & Eccles, 2006). Therefore, it is important to explore the most effective ways of implementing existing evidence into practice (Kutner2011). Applying research findings to practice is especially difficult due to the broad, holistic and elements of complex interventions offered in various practice settings (Evans, Snooks, Howson, & Davies,2013). Several frameworks or models have been developed to provide guidance for the process of implementing research evidence into practice, including the Promoting Action on Research Implementation in Health Services framework (PARiHS; Rycroft‐Malone, 2004) and the Consolidated Framework for Implementation Research (CFIR, Damschroder et al.,2009). This review was performed with the focus on a specific aspect of implementation—the concept of knowledge transfer and exchange (KTE), which is often noted but not explicated in existing models in the area of implementation. Discussing the impact of implementation research in mental health services (Proctor et al.,2009) considers KTE in this wider context, noting the movement of research into practice settings as the basis for implementation. They also cite work by the NIH and the CDC, which defines implementation as requiring the generation of knowledge, the dissemination (transfer, our addition) of this knowledge, followed by active efforts to support the implementation of this knowledge.
1.1. Background
There are many terms used to refer to KTE related activity, including dissemination, knowledge transfer and knowledge mobilization. A review by (Pentland et al.,2011) highlighted the variation in this area, stressing the challenge that this can create in providing guidance to researchers and practitioners. However, to frame the current research, it is important to be explicit about the definition of KTE that underpins this work. For this study, we adopted the following definition of KTE, as one which is routinely cited in research and reflects the views of the authors:
“an interactive interchange of knowledge between research users and researcher producers (Kiefer et al.,2005). [Its purpose is] to increase the likelihood that research evidence will be used in policy and practice decisions and to enable researchers to identify practice and policy‐relevant research questions” (cited in Mitton, Adair, McKenzie, Patten, & Perry,2007.729).
KTE is a complex, dynamic and iterative social process, (Kiefer et al.,2005; Ward, House, & Hamer,2009a, 2009b; Ward, Smith, Foy, House, & Hamer,2010) which does not necessarily contribute directly to implementation but instead to an increased chance that evidence can and will be implemented. Consequently, KTE presents an early challenge to implementation of evidence‐based health care. To be rigorous and effective, it has been recommended that KTE activities are guided by a model that clearly shows how the process works and how it can help knowledge producers and users plan and evaluate KTE activities (Anderson, Allen, Peckham, & Goodwin,2008; Armstrong, Waters, Roberts, Oliver, & Popay,2006; Estabrooks, Squires, Cummings, Birdsell, & Norton,2009; Graham, Tetroe, & Grp,2007; McKibbon et al.,2013; Straus, Tetroe, & Graham,2009; Ward, House, & Hamer,2009a; Ward, Smith, House, & Hamer,2012; Wilson, Petticrew, Calnan, & Nazareth,2010). Yet, KTE as a key aspect of implementation has rarely been explicitly operationalized in existing models of implementation.
2. THE REVIEW
2.1. Aim
The aim of this study was to review, analyse and synthesize the key components of KTE as evidenced in published health services research. Apart from the prevalence of the individual components of the components we will also capture the operational elements of these components and their interactions. To contextualize the components and their interactions, the findings will be presented in a form of a model.
2.2. Design
A scoping approach was adopted, following a detailed protocol (Prihodova, Guerin, & Kernohan,2015). The review was guided the methodological framework proposed by Arksey and O'Malley (Arksey & O'Malley,2005), with additional amendments based on (Levac, Colquhoun, and O'Brien,2010; Levac et al.,2010). While the protocol for this review set out as one of the aims as appraisal of the relevance and suitability of these components for providers, settings and dimensions of palliative care, this study will report the general components of KTE in any healthcare setting identified by the review and their appraisal for palliative care will be addressed in a subsequent publication. In addition, in the absence of reporting guidelines for scoping reviews, the six‐stage process (Table 1) was benchmarked against the PRISMA guidelines (Moher, Liberati, Tetzlaff, Altman, & Grp,2009) to ensure rigour.
Table 1.
Stages of systematic review applied
| 1. Identify research question | What are the core components of KTE frameworks? |
| 2. Identify relevant studies | Search conducted of MEDLINE, EMBASE, CINAHL Plus, PsycINFO, Social Services Abstracts, ASSIA.Additional review of reference sections of selected papers. |
| 3. Select studies | Search terms, inclusion and exclusion see (Prihodova et al.,2015). Abstracts and full text screened by two members of the team, with disagreements adjudicated by third member |
| 4. Appraise quality & extract data | Appraisal based on (Dixon‐Woods et al.,2006. Data extracted by one researcher (see Prihodova et al.,2015), validation conducted with 20% of studies. |
| 5. Collate & summarize findings | Thematic analysis based on (Braun and Clarke,2006) with additional frequency and statistical analysis. |
| 6. Disseminate | Dissemination included presentations to researchers in health, publication of review protocol and conference presentations. |
2.3. Search strategy
The search strategy included four search terms and their variations (knowledge (evidence, research, information, data), transfer (exchange, generation, translation, uptake, mobilization, dissemination, implementation), framework (model, concept) and health care (health system, health service, healthcare provider)) and was designed to be as extensive as possible. The search was performed across six main electronic databases (MEDLINE, EMBASE (Elsevier), CINAHL Plus (EBSCO), PsycINFO (ProQuest), Social Services Abstracts, Applied Social Sciences Index and Abstracts (ASSIA)). Only studies that sufficiently described an original (or adapted) explicit framework, model or concept of KTE applied in healthcare setting were included.
To be included, articles had to provide a description of an original (or adapted) model or framework (noting that these terms are often used interchangeably) that considered the implementation of research knowledge and its application. This included articles which presented a specific model of KTE and articles that used KTE models or model elements to inform the implementation of research into practice. Limiting searches to health services settings was intended to ensure a practical focus of the work and the potential to synthesize the operational elements of the KTE process rather than just the theoretical.
2.4. Search outcomes
The initial database search identified 7,544 abstracts with none identified elsewhere (Figure 1). After the removal of duplicates (N = 2,672; 35%), a further 7.7% of abstracts were removed due to following exclusion criteria: not research articles (N = 356; book/book chapter/conference proceedings, etc.); low quality (N = 158; no abstract, published in non‐peer reviewed journals); were not involving humans (N = 70). The remaining abstracts (N = 4,288; 57%) were screened independently by two authors (92% agreement rate on inclusion/exclusion), resulting in 298 (3.9%) articles identified for full‐text screening.
Figure 1.
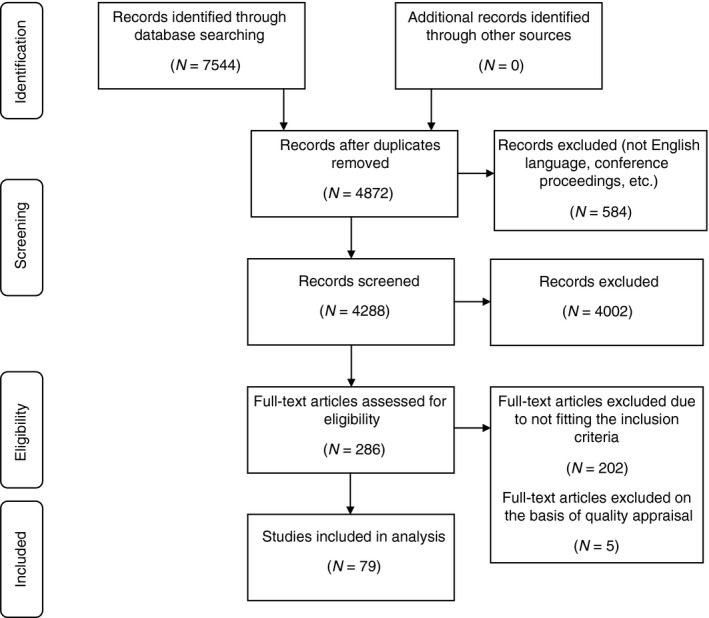
Flow diagram of the systematic review (modified from Moher et al.,2009)
From the identified abstracts, we were unable to source 12 full‐texts and therefore 286 full‐texts were reviewed independently by two reviewers, with 75% agreement on inclusion/exclusion. A further 202 articles (71%) articles were removed at the full‐text review as they were found to not fit the inclusion criteria, with the final number 84 (29%) of articles included in data extraction. At the data extraction phase, the articles underwent a criteria appraisal (Table 3) and five more articles were removed following an in‐depth analysis due to very vague description of the model or its application. The final number of articles included in data analysis was 79 (28%). The summary details of these articles are included in Table 2.
Table 2.
Studies identified by systematic review and included in the final analysis grouped by model used
| Framework | N of studies | Outer context | Evidence/message | Process/strategy | People/audience | Inner context | Efficacy/outcome | Total components | Total operational factors | Reference |
|---|---|---|---|---|---|---|---|---|---|---|
| The Consolidated Framework for Implementation Research (CFIR) | 3 | 3 | 5 | 3 | 3 | 6 | 0 | 15 | 20 | (Hartzler, Lash, and Roll,2012; Ilott, Gerrish, Booth, and Field,2013; Ruffolo and Capobianco,2012) |
| Iowa model | 2 | 4 | 4 | 2 | 3 | 1 | 7 | 14 | (Mark, Latimer, and Hardy,2010; Tschannen et al.,2011 | |
| Knowledge‐to‐Action Framework (KTA) | 5 | 8 | 5 | 4 | 2 | 12 | 19 | (Douglas et al.,2013; Hemmelgarn et al.,2012; Heyland et al.,2013; Kastner and Straus,2012; Petzold, Korner‐Bitensky, and Menon,2010) | ||
| Ottawa Model of Research Use (OMRU) | 3 | 6 | 3 | 3 | 4 | 2 | 12 | 18 | (Logan and Graham,1998; Logan et al.,1999; Santesso and Tugwell,2006 | |
| Other | 46 | 8 | 82 | 66 | 87 | 57 | 10 | 147 | 310 | (Aguilar‐Gaxiola et al.,2002c; Alvaro et al.,2010; Ammentorp and Kofoed,2011; Anderson, Cosby, Swan, Moore, and Broekhoven,1999b; Atchan, Davis, and Foureur,2014; Borbas, Morris, McLaughlin, Asinger, and Gobel,2000; D'Andreta, Scarbrough, and Evans,2013; Dobbins, Ciliska, Cockerill, Barnsley, and DiCenso,2002; Donaldson, Rutledge, and Ashley,2004; Doran and Sidani,2007; Dufault,2004; Elliott et al.,2003; Florin et al.,2012; Gabbay, le May, and McCaughan,2005; Glasgow,2013; Greenhalgh, Robert, MacFarlane, Bate, and Kyriakidou,2004; Hartling et al.,2007; Haynes, Hayward, and Lomas,1995; Herr, English, and Brown,2003; Ho et al.,2004; Jack and Tonmyr,2008; Jacobson, Butterill, and Goering,2005; Kahn et al.,2014; Kitson et al.,2013; Krishnan, Nongkynrih, Kapoor, and Pandav,2009; McNeill and Kelley,2005; Mende, Meredith, Schoenbaum, Sherbourne, and Wells,2008; Moore,1999; Nakata, Kuriyama, Mitsuyasu, Morimoto, and Tomioka,1989; Orlandi,1987; Palmer and Kramlich,2011; Pronovost et al.,2008; Rogers,2009; Russell‐Babin and Miley,2013; Rubenstein et al.,2010; Sakala and Mayberry,2006; Silva, Morel, and de Moraes,2014; Sterling and Weisner,2006; Stetler,2003; Tavernier,2014; Thomson‐O'Brien and Moreland,1998; Tugwell, Robinson, Grimshaw, and Santesso,2006; Unützer, Powers, Katon, and Langston,2005; Urquhart, Porter, and Grunfeld,2011; Wallace, Brown, and Hilton,2014; Wilkins et al.,2013) |
| Promoting Action on Research Implementation in Health Services (PARIHS) framework | 16 | 1 | 24 | 23 | 9 | 32 | 2 | 49 | 91 | (Alkema and Frey,2006; Blackwood,2003; Brown and McCormack,2005; Capasso et al.,2009; Ellis, Howard, Larson, and Robertson,2005; Helfrich et al.,2010; Kavanagh, Watt‐Watson, and Stevens,2007; Kristensen, Borg, and Hounsgaard,2011; Milner, Estabrooks, and Myrick,2006; Obrecht, Van Hulle Vincent, and Ryan,2014; Rycroft‐Malone et al.,2002, 2013; Tilson and Mickan,2014; Urquhart, Sargeant, and Grunfeld,2013; Ullrich, Sahay, and Stetler,2014; Wright, McCormack, Coffey, and McCarthy,2007) |
| The Practical, Robust Implementation and Sustainability Model (PRISM) | 2 | 2 | 0 | 2 | 3 | 2 | 1 | 9 | 10 | (Beck, Bergman, Rahm, Dearing, and Glasgow,2009; Feldstein and Glasgow,2008) |
| Reach‐Efficacy‐Adoption ‐ Implementation – Maintenance (RE‐AIM) | 2 | 0 | 2 | 0 | 0 | 1 | 0 | 3 | 3 | (Boratgis et al.,2007; Dzewaltowski, Glasgow, Klesges, Estabrooks, and Brock,2004) |
| Total | 79 | 14 | 131 | 106 | 111 | 105 | 18 | 254 | 485 |
2.5. Quality appraisal
In line with scoping reviews, limited application of quality appraisal criteria was undertaken; and aggregated quality assessments of the dataset are presented rather than study level assessments (Table 3).
Table 3.
Quality appraisal of articles included in the scoping review
| Quality appraisal criterion | Yes | No |
|---|---|---|
| Are the aims and objectives of the research clearly stated? | 79 (100%) | |
| Is the framework described sufficiently | 60 (76%) | 19 (24%) |
| Is the research design clearly specified and appropriate for the aims and objectives of the research? | 73 (92.4%) | 6 (7.6%) |
| Do the researchers display enough data to support their interpretations and conclusions? | 32 (40.5%) | 47 (59.5%) |
| Do the researchers provide a clear account of the process by which their findings were produced? | 53 (67%) | 26 (32%) |
| Is the method of analysis appropriate and adequately explicated? | 51 (64.6%) | 28 (35.4%) |
2.6. Data abstraction and synthesis
Analysis of extracted data was conducted at two levels: descriptive and explorative. Level 1 (descriptive analysis) involved tabulation of basic information such as study design, participant samples and the named models. Level 2 (explorative analysis) involved thematic analysis of narrative data, of the descriptions of identified models and of their visual representations. We used thematic analysis (Braun & Clarke,2006) wherein initial coding and the development of candidate themes were conducted independently by two authors, who then met to agree the final thematic map of the findings. Once the themes were agreed, two authors coded the data, while a third author conducted an independent coding check of 10% of the articles. The agreement for the credibility check of the independently coded themes was 83%. Frequency analysis provided the occurrence of each theme across the identified articles, as a reflection of the salience of the theme in the data.
As a validity check, stakeholder consultation was performed by presenting the findings at a national workshop for researchers, policy makers and patient/carer representatives in health services research. A stenographer recorded the workshop and feedback was gathered from attendees to allow reflection on the discussions. No significant changes were made to the components; however, the discussion highlighted the need for some clarity regarding the operational elements and the nature of the interaction between components. This led to some changes in the naming of components and operational elements and more clarity on structure. A visualization, incorporating the revisions from this process is presented in this paper.
3. RESULTS
3.1. Overview of articles and models
Of the 79 articles included in this scoping review, the majority were published in medical (53%) and nursing (25%) journals, followed by behavioural/psychological journals (7.6%), journals on medical training (6.3%), health services research (5%) and miscellaneous (2.1%). The earliest studies were published in 1985, with 2014 being the latest year included in the search; 70 articles (89%) were published after 2001 and over a third of all articles (35%) were published after 2010. This suggests a relatively recent increase in interest in the issue of knowledge transfer in health research.
In the 79 articles were references to 88 models or frameworks (including multiple occurrences across articles), with 49 unique models/frameworks named and 13 models not explicitly named. Five models were mentioned in multiple articles, with PARiHS being the most frequently cited (Rycroft‐Malone,2004). When it came to the theoretical background of the framework, 19 (24%) articles provided no information, while 24 (30%) referred to previous publications. From the remaining articles, 25 (32%) referred to multiple other models/frameworks or theories and 11 (14%) to a single framework. Over half of the articles indicated the target audience for the KTE (N = 43, 54%), with the majority proposing the use of the model in multiple stakeholder groups (N = 32, 41%).
Our quality appraisal focused on fatal flaws, as outlined by Dixon‐Woods et al. (Dixon‐Woods et al.,2006). We also rated the level of detail in the description of the framework or its application. The findings highlight several limitations (see Table 3). All articles had clear statements of the aims and objectives, a majority (>90%) had a clearly described research design (where appropriate) and a significant proportion (76%) provided sufficient detail to analyse the framework. However, fewer articles (67%) provided a clear account of data analysis and findings or presented data to support their interpretations (40%), which may highlight the need for more critical evaluation of dissemination activities and limitations in the quality of this research.
3.2. Identifying the core components and operational elements of knowledge transfer and exchange
From the thematic analysis, six key themes were identified to represent the core components of KTE.
The first component of KTE—the Message reflects the information to be shared. Within this component, the most common operational element was the idea that the message is needs‐driven. This often‐presented research as a clinical or practical problem, while multiple studies applying the PARiHS framework referred to the research as needs‐ or problem‐based (Kristensen, Borg, & Hounsgaard,2011; Rycroft‐Malone,2004; Tilson & Mickan,2014). The operational elements or attributes of the message as credible and actionable occurred with equal frequency. Research findings being actionable related to its use or application in practice and were particularly evident in articles considering the Ottawa Model of Research Use (Logan & Graham,1998; Logan, Harrison, Graham, Dunn, & Bissonnette,1999; Pronovost, Berenholtz, & Needham,2008). The credibility of the message referred to the use of outcomes that are considered valid (Pronovost et al.,2008). Jack and Tonmyr (Jack & Tonmyr,2008) applied Lavis’ model of KTE and referred to the importance of messages containing credible information. Occurring slightly less frequently was the operational element of the message as accessible, which was represented in as translating the knowledge or tailoring it for key stakeholders (Kitson et al.,2013; Tugwell, O'Connor, et al.,2006). The final operational element noted was that multiple types of message are important, which reflected the use of different research methods to generate messages and the potential for research to have different messages to transfer. For example, the revised PARiHS Framework (Rycroft‐Malone et al.,2002) noted that different types of research evidence are required to answer different questions relevant to practice.
The Process component represented the activities intended to implement the transfer of knowledge. This was often identified as a collaborative aspect of KTE, reflecting the “push‐pull” dynamic exchange of information. Taking the operational element of KTE as an interactive exchange, the Research Practice Integration model (Sterling & Weisner,2006) referred to the bidirectional relationship between stakeholders in treatment and research. KTE was described as requiring skilled facilitation, with multiple articles referring to PARiHS model that highlights the importance of this. The KTE processes were also expected to be targeted and timely, stressing the need to target key groups such as policy makers (Aguilar‐Gaxiola et al.,2002b), recognizing the importance of activities taking place at the right time (Haynes, Hayward, & Lomas,1995).
The Process component also included the operational element of marketing the message, reflecting the need for the communicators (typically the researchers) to communicate in a way that effectively pitched information to their target audience. Herr et al. (Borbas, Morris, McLaughlin, Asinger, & Gobel,2000; Herr, English, & Brown,2003) drew on the Knowledge Development and Application model, discussing the need to ‘get the message out’ through dissemination activities. The KTE process was also recognized to require the support or endorsement of opinion leaders/champions, for example the article by Borbas et al. (Borbas et al.,2000) reported on their Healthcare Education and Research Foundation process, which uses clinical opinion leaders to support research implementation, while the Translating Research into Practice model reported by Tschannen et al. (Tschannen, Talsma, Gombert, & Mowry,2011) also highlights the use of opinion leaders in the process. The final operational element reflected the need for KTE to draw on diverse activities, for example Aguilar‐Gaxiola et al. described multiple multifaceted activities as part of research on mental health care for Mexican Americans (Aguilar‐Gaxiola et al.,2002a, 2002b).
The Stakeholders represent the people involved on either side of the exchange process. This was operationalized into four operational elements: knowledge users, knowledge beneficiaries and multiple stakeholders. The knowledge producers refer predominantly to the researchers themselves (Dufault,2004; Ho et al.,2004; Sterling & Weisner,2006); while knowledge users, sometimes referred to as knowledge consumers (Ho et al.,2004) represent the most common stakeholders—practitioners and policy makers, positioning them in the context of communities of professional practice, e.g., primary care practitioners (McCaughan,2005). The knowledge beneficiaries represent the wider group of patients and families who benefit from the implementation (Hemmelgarn et al.,2012; Jack & Tonmyr,2008). Finally, several papers emphasized that those involved in KTE have multiple stakeholders to consider including patients’ families and the general public (Anderson, Cosby, et al.,1999b; Ho et al.,2004; Orlandi,1987).
The context for KTE was reported at two important levels: local and wider social, economic and cultural. The Local Context, addressing the immediate, often organizational environments, where the transfer would occur, included four operational elements. The most prevalent of these was organizational influence, with organizations and their leaders/managers identified as key influencers in the KTE process. Senior colleagues in organizations were reported as instrumental in the adoption of research knowledge to implement change, (Dobbins, Ciliska, Cockerill, Burnsley, & DiCenso,2002) or support evidence‐based practice (Stetler,2003). Closely linked to this was the operational element of organizational culture, which may be expressed as the attitudes, knowledge and values expressed in the organization. Multiple articles implementing the PARIHS Framework (Helfrich et al.,2010) or the Translating Research into Practice model highlighted the importance of organizational culture and the importance of setting organizational standards (Tschannen et al.,2011).
Our findings highlighted the need for dedicated resources for KTE activities. For example, the Multisystem Model of Knowledge Integration and Translation, referred to resourcing effective implementation (Palmer & Kramlich,2011), while the Conservation of Resources Theory, recognized the range of resources required and noted that these may differ at different stages of the process (Alvaro et al.,2010). The final operational element in this section was readiness for knowledge. One application of PARIHS emphasized receptivity of the context—a factor which is common in many of the articles applying or using this KTE model (Helfrich et al.,2011).
The inclusion of the Social, Cultural & Economic Context component recognized the influence of wider environmental factors influencing research and practice. While this was the least frequent theme it was evident in the Evidence‐based Information Circle, designed to help practitioners engage with evidence‐based practice (Thomson‐O'Brien & Moreland,1998). This component included an outer context representing factors that may have an impact on decision making, with specific reference to aspects of the social, cultural and economic context. In the Practical, Robust Implementation and Sustainability Model the external environment was considered to have an influence on the implementation of research (Feldstein & Glasgow,2008) while in the CFIR model, the outer setting incorporating wider cultural, political and economic factors was explicitly referenced (Damschroder & Hagedorn,2011).
The final component of KTE highlighted the importance of evaluation in the model, with the concept of Evaluating Efficacy expressing the need for a mechanism for evaluation of the success of the knowledge transfer activity. It is interesting to note that, alongside the theme of Social, Cultural and Economic context, this component was least prevalent in the coding of data extracted. The Ottawa Model of Research Use (Logan & Graham,1998; Logan et al.,1999) highlighted the importance of evaluating the outcomes of KTE and implementation work, while others referred to the importance of examining the effectiveness of transfer activities (Anderson, Caplan, et al.,1999a) and the importance of both outcome and process evaluation (Sakala & Mayberry,2006).
3.3. Reflections on the structure of the components
Informed by the discussions at the stakeholder workshop, a visualization incorporating these components is presented in Figure 2. Also included are the operational elements identified as part of the analysis and the frequency of occurrence of each component and operational element.
Figure 2.
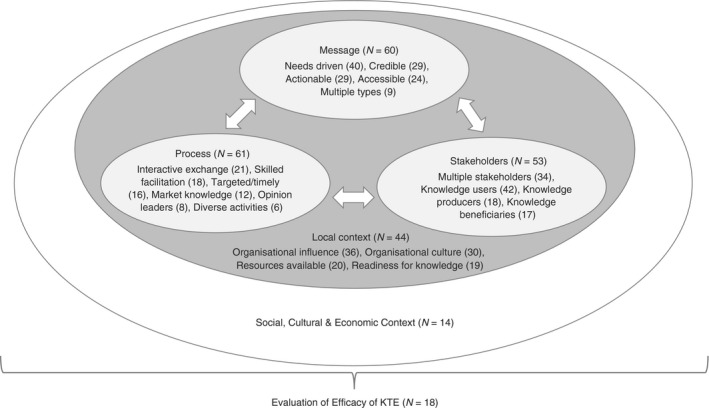
Key components of knowledge transfer identified through thematic analysis (with frequencies reported)
Taking the components together the starting point of KTE activity is the knowledge to be transferred (the Message). The message is influenced by the Stakeholders, recognizing that there may be multiple groups who may influence the way the message needs to be communicated). Based on the message and the stakeholders the knowledge producer should identify the Processes to be used to ensure the message can be delivered to the stakeholders effectively. Also important is allowing for feedback to come back though the same channels. These interacting components sit in two identified layers, the Local Context and the wider Social, Cultural and Economic Context and highlight the need for researchers to consider how these contexts may have an impact on the Message, Stakeholders and Processes.
4. DISCUSSION
The aim of this review was to identify key components and related operational elements of KTE, intended to guide researchers’ actions in relation to KTE, in the broader context of implementation. The search identified 79 articles which included an explicit model related to transferring research findings in health settings. These articles were drawn from a range of disciplines, although medicine and nursing were the most common. The publication date range highlights a recent increase in research and dissemination activity in this area. This review identified almost 50 individual models or frameworks, with PARiHS the most frequent. Quality appraisal of the articles highlighted several limitations to the quality of the research; however, few articles were excluded on the basis of a lack of information on the model itself.
The thematic analysis identified six core components of KTE, three of which were commonly present in the articles. The messages to be transferred, the stakeholders and the specific processes by which transfer was achieved were considered in detail. However, the key practical finding lies in the operational elements in these components, which provide more specific and practical guidance for researchers intending to maximize the potential impact of their research. Recognizing that multiple types of message are important highlights the need to be aware of different processes when communicating with different stakeholders. Echoing this, the use of diverse activities as part of the KTE process was rarely evident in articles, perhaps due to the dominance of traditional methods that focus on academic dissemination. Another key finding is the importance of targeted and timely KTE activities. Rather than planning for dissemination at the end of the research process, the evidence presented in this review stresses the need for KTE to be an ongoing activity across the lifetime of the project. While transfer processes were frequently considered in previous studies, few considered multiple processes for a single study, suggesting a simplistic, linear approach to knowledge transfer. This does not reflect the complex non‐linear process of KTE evident across the findings of this review.
Recognizing the context where KTE is to take place is another key finding. While the immediate or local context was considered in more than half of the articles, the issue of the wider social, cultural and economic context was considered in less detail, with no evidence of specific operational elements to guide the researcher when considering the influence of this wider context. The need to consider not just the local but the wider context represents a possible shift in KTE activities. However, given that change in the health sector is often influenced by these wider factors (for example the impact of an economic recession), it is perhaps surprising that these aspects of the context are poorly expressed in existing models. Given the lack of representation of this component in the existing literature we would argue there is a need to increase awareness of its role in KTE and the possible activities that would operationalize this level of the process.
A novel finding is the lack of evidence that process and outcomes of KTE activity is being evaluated by those engaged in the process. In addition, the presence of methodological issues in the studies, such as lack of grounding in data and or detail on analysis and process, further highlights the need for rigorous evaluation of KTE activities. If researchers apply the key principles of evidence‐based practice to their KTE activities, then evaluating the effectiveness of these KTE activities becomes necessary. The focus on audit of practice evident in other areas of the health services (Ivers et al.,2012) could and should be extended to KTE, with researchers recognizing the importance of assessing how effective their KTE activities have been in reaching key stakeholders, beyond more traditional metrics such as article citation counts and journal impacts.
It is important to reflect on the methodological quality of this review before final conclusions can be drawn. While the presented findings are based on evidence pre‐2015, there was an exponential rise in the number of studies published since 2015; re‐running the search terms employed in this review yielded over 4000 results, highlighting the urgency in understanding KTE and implementation. While in‐depth analysis of the search terms is beyond the scope of this review, many of the recent studies were based on refining of existing models and clarifying the ways of using them in the process of implementation, e.g., (Harvey & Kitson,2016). There have been significant developments in the conduct and use of systematic reviews in intervention and health research, which allowed for clear guidance in the development of this review. The method of review used was mapped onto the PRISMA procedure as the agreed process for systematic reviews and validity checks such as phases of independent review were included in the screening of articles and in the extraction and analysis of data. In addition, the methodology of the review was peer reviewed and published in advance of the completion of the study. However, there are limitations, not least the lack of engagement with unpublished and policy‐related literature and the timeframe of the search (papers published before January 2015). Despite these limitations we are confident that the rigour evident in the search and analysis provides a basis for confidence in the findings.
5. CONCLUSION
The components identified represent both established and emerging aspects of KTE, with a clear focus on effective ways of transferring research knowledge to care providers and stakeholders and could be used in applied settings and to inform future research. Specific operational elements in these components can directly guide the researcher to maximize the activities in relation to these components. The synthesis of the components and operational elements identified potentially provides a functional model of KTE that could offer researchers the tools to ensure their KTE activities are appropriate and a framework within which to evaluate their actions. Given the process of identification undertaken in this study the authors are tentatively proposing the structure presented in Figure 2 as an Evidence‐based model for the Transfer and Exchange of Research Knowledge (EMTReK).
While requiring further research, EMTReK could act as a resource for researchers planning KTE activities, with this review establishing an initial evidence‐base for the components and the operational evidence. We are conscious that the components and operational elements presented are not new, with each one less or more evident in the articles reviewed. The real potential for contribution lies in its focus on operational elements that may serve as a practical guide for researchers. To conduct an initial exploration of the model we have conducted a series of case studies where healthcare researchers applied the model to their own KTE activities. Initial findings are positive and highlight the need to develop a process guide to complement the description of the model presented in this article. This could be particularly important if there is increased interest in routine evaluation of KTE activities. However, there is a need for further evaluation of the EMTReK model (including the operational elements) before a definitive statement can be made about its contribution.
We recommend that researchers consider EMTReK as a possible functional model of KTE in health services research to ensure that research is conducted with knowledge transfer in mind from the earliest phases of the process. We also recommend that researchers develop evaluation strategies to both assess their activities and to provide feedback on the potential contribution of this model.
6. DECLARATIONS
Ethics approval and consent to participate—Approval was not required given the documentary nature of the study and the lack of human participants (see www.ucd.i.e/researchethics).
Availability of data and material—The datasets used and/or analysed during the current study (namely the database of articles and extracted data) are available from the corresponding author on reasonable request.
Authors’ contributions: LP, SG and GWK designed the study and conducted the review. SG and CT conducted the analysis of model components, LP conducted credibility checks. LP and SG drafted the article. All authors reviewed multiple drafts of the article.
7. REGISTRATION
As a scoping review the study was not registered, though the protocol of the review was published (PMID: 25739936; https://doi.org/10.1111/jan.12642).
8. IMPACT STATEMENT
Through rigorous synthesis of evidence from a range of disciplines, this review identified key components and related operational elements of knowledge transfer and exchange (KTE) that may guide researchers’ actions in KTE in the broader context of implementation.
The components represent established and emerging aspects of KTE and the specific operational elements are positioned to guide the KTE activities in applied settings.
As a result, we propose that these components may represent a functional model of KTE—the Evidence‐based model for the Transfer and Exchange of Research Knowledge (EMTReK), highlighting the elements for consideration to ensure KTE activities are appropriate and as a framework where to evaluate their impact.
CONFLICT OF INTEREST
No conflict of interest has been declared by the authors.
AUTHOR CONTRIBUTIONS
All authors have agreed on the final version and meet at least one of the following criteria [recommended by the ICMJE (http://www.icmje.org/recommendations/)]:
substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data;
drafting the article or revising it critically for important intellectual content.
Supporting information
ACKNOWLEDGEMENTS
The authors thank the All Ireland Institute of Hospice & Palliative Care who funded the research, Geraldine Boland who supported the data extraction and reliability checks, and Mary Jane Brown and Cathy Payne who provided comments on the research.
Prihodova L, Guerin S, Tunney C, Kernohan WG. Key components of knowledge transfer and exchange in health services research: Findings from a systematic scoping review. J Adv Nurs. 2019;75:313–326. 10.1111/jan.13836
Funding information
This research was funded by the All Ireland Institute of Hospice & Palliative Care. The funding body reviewed and commented on the proposal for the research but were not involved in any aspect of the collection, analysis, and interpretation of data
REFERENCES
- Aguilar‐Gaxiola, S. A. , Zelezny, L. , Garcia, B. , Edmondson, C. , Alejo‐Garcia, C. , & Vega, W. A. (2002a). Translating research into action: Reducing disparities in mental health care for Mexican Americans. Psychiatric Services, 53(12), 1563–1568. 10.1176/appi.ps.53.12.1563 [DOI] [PubMed] [Google Scholar]
- Aguilar‐Gaxiola, S. A. , Zelezny, L. , Garcia, B. , Edmondson, C. , Alejo‐Garcia, C. , & Vega, W. A. (2002b). Mental health care for Latinos: Translating research into action: Reducing disparities in mental health care for Mexican Americans. Psychiatric Services, 53(12), 1563–1568. 10.1176/appi.ps.53.12.1563 [DOI] [PubMed] [Google Scholar]
- Aguilar‐Gaxiola, S. A. , Zelezny, L. , Garcia, B. , Edmondson, C. , Alejo‐Garcia, C. , & Vega, W. A. (2002c) Translating research into action: Reducing disparities in mental health care for Mexican Americans. Psychiatric Services (Washington, D.C.), 53(12), 1563–1568. 10.1176/appi.ps.53.12.1563 [DOI] [PubMed] [Google Scholar]
- Alkema, G. E. , & Frey, D. (2006). Implications of translating research into practice: A medication management intervention. Home Health Care Services Quarterly, 25(1–2), 33–54. [DOI] [PubMed] [Google Scholar]
- Alvaro, C. , Lyons, R. F. , Warner, G. , Hobfoll, S. E. , Martens, P. J. , Labonte, R. , & Brown, R. E. (2010). Conservation of resources theory and research use in health systems. Implementation Science, 5, 79 10.1186/1748-5908-5-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammentorp, J. , & Kofoed, P. E. (2011). Research in communication skills training translated into practice in a large organization: A proactive use of the RE‐AIM framework. Patient Education and Counseling, 82, 482–487. [DOI] [PubMed] [Google Scholar]
- Anderson, S. , Allen, P. , Peckham, S. , & Goodwin, N. (2008). Asking the right questions: Scoping studies in the commissioning of research on the organisation and delivery of health services. Health Res Policy Syst, 6, 7 10.1186/1478-4505-6-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson, L. A. , Caplan, L. S. , Buist, D. S. , Newton, K. M. , Curry, S. J. , Scholes, D. , & LaCroix, A. Z. (1999a) Perceived barriers and recommendations concerning hormone replacement therapy counseling among primary care providers. Menopause (New York, N.Y.), 6(2), 161–166. 10.1097/00042192-199906020-00014 [DOI] [PubMed] [Google Scholar]
- Anderson, M. , Cosby, J. , Swan, B. , Moore, H. , & Broekhoven, M. (1999b). The use of research in local health service agencies. Social Science & Medicine, 49, 1007–1019. 10.1016/S0277-9536(99)00179-3 [DOI] [PubMed] [Google Scholar]
- Arksey, H. , & O'Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Armstrong, R. , Waters, E. , Roberts, H. , Oliver, S. , & Popay, J. (2006). The role and theoretical evolution of knowledge translation and exchange in public health. Journal of Public Health, 28(4), 384–389. 10.1093/pubmed/fdl072 [DOI] [PubMed] [Google Scholar]
- Atchan, M. , Davis, D. , & Foureur, M. (2014). Applying a knowledge translation model to the uptake of the Baby Friendly Health Initiative in the Australian health care system. Women and Birth, 27, 79–85. [DOI] [PubMed] [Google Scholar]
- Beck, A. , Bergman, D. A. , Rahm, A. K. , Dearing, J. W. , & Glasgow, R. E. (2009). Using implementation and dissemination concepts to spread 21st‐century well‐child care at a health maintenance organization. Permanente Journal, 13(3), 10–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackwood, B. (2003). Can protocolised‐weaning developed in the United States transfer to the United Kingdom context: A discussion. Intensive and Critical Care Nursing, 19(4), 215–225. [DOI] [PubMed] [Google Scholar]
- Boratgis, G. , Broderick, S. , Callahan, M. , Combes, J. , Lannon, C. , Mebane‐Sims, I. , … Watt, A. (2007). Disseminating QI interventions… quality improvement. Joint Commission Journal on Quality and Patient Safety, 33(12), 48–65. [DOI] [PubMed] [Google Scholar]
- Borbas, C. , Morris, N. , McLaughlin, B. , Asinger, R. , & Gobel, F. (2000). The role of clinical opinion leaders in guideline implementation and quality improvement. Chest, 118(2 Suppl), 24S–32S. 10.1378/chest.118.2_suppl.24S [DOI] [PubMed] [Google Scholar]
- Braun, V. , & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Brown, D. , & McCormack, B. (2005). Developing postoperative pain management: Utilising the promoting action on research implementation in health services (PARIHS) framework. Worldviews on Evidence‐Based Nursing, 2, 131–141. [DOI] [PubMed] [Google Scholar]
- Capasso, V. , Collins, J. , Griffith, C. , Lasala, C. A. , Kilroy, S. , Martin, A. T. , … Wood, S. L. (2009). Outcomes of a clinical nurse specialist‐initiated wound care education program using the Promoting Action on Research Implementation in Health Services Framework. Clinical Nurse Specialist, 23, 252–257. [DOI] [PubMed] [Google Scholar]
- Damschroder, L. J. , Aron, D. C. , Keith, R. E. , Kirsh, S. R. , Alexander, J. A. , & Lowery, J. C. (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science, 4, 15 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damschroder, L. J. , & Hagedorn, H. J. (2011). A guiding framework and approach for implementation research in substance use disorders treatment. Psychology of Addictive Behaviors, 25, 194–205. 10.1037/a0022284 [DOI] [PubMed] [Google Scholar]
- D'Andreta, D. , Scarbrough, H. , & Evans, S. (2013). The enactment of knowledge translation: A study of the Collaborations for Leadership in Applied Health Research and Care initiative within the English National Health Service. Journal of Health Services Research and Policy, 18(3), 40–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon‐Woods, M. , Cavers, D. , Agarwal, S. , Annandale, E. , Arthur, A. , Harvey, J. , … Sutton, A. J. (2006). Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Medical Research Methodology, 6, 35 10.1186/1471-2288-6-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobbins, M. , Ciliska, D. , Cockerill, R. , Burnsley, J. , & DiCenso, A. (2002). A framework for the dissemination and utilization of research for health‐care policy and practice. Online Journal of Knowledge Synthesis for Nursing, 9(7), 12. [PubMed] [Google Scholar]
- Donaldson, N. E. , Rutledge, D. N. , & Ashley, J. (2004). Outcomes of adoption: Measuring evidence uptake by individuals and organizations. Worldviews on Evidence‐Based Nursing, 1, s41–s51. [DOI] [PubMed] [Google Scholar]
- Doran, D. M. , & Sidani, S. (2007). Outcomes‐focused knowledge translation: A framework for knowledge translation and patient outcomes improvement. Worldviews on Evidence‐Based Nursing, 4, 3–13. [DOI] [PubMed] [Google Scholar]
- Douglas, M. L. , McGhan, S. L. , Tougas, D. , Fenton, N. , Sarin, C. , Latycheva, O. , & Befus, A. D. (2013). Asthma education program for First Nations children: An exemplar of the Knowledge‐to‐Action Framework. Canadian Respiratory Journal, 20, 295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dufault, M. (2004). Testing a collaborative research utilization model to translate best practices in pain management. Worldviews on Evidence‐Based Nursing, 1, S26–S32. 10.1111/j.1524-475X.2004.04049.x [DOI] [PubMed] [Google Scholar]
- Dzewaltowski, D. A. , Glasgow, R. G. , Klesges, L. M. , Estabrooks, P. A. , & Brock, E. (2004). RE‐AIM: Evidence‐based standards and a web resource to improve translation of research into practice. Annals of Behavioral Medicine, 28(2), 75–80. [DOI] [PubMed] [Google Scholar]
- Elliott, S. J. , O'Loughlin, J. , Robinson, K. , Eyles, J. , Cameron, R. , Harvey, D. , … Gelskey, D. (2003). Conceptualizing dissemination research and activity: The case of the Canadian Heart Health Initiative. Health Education and Behaviour, 30(3), 267–282, 283–286. [DOI] [PubMed] [Google Scholar]
- Ellis, I. , Howard, P. , Larson, A. , & Robertson, J. (2005). From workshop to work practice: An exploration of context and facilitation in the development of evidence‐based practice. Worldviews on Evidence‐Based Nursing, 2, 84–93. [DOI] [PubMed] [Google Scholar]
- Estabrooks, C. A. , Squires, J. E. , Cummings, G. G. , Birdsell, J. M. , & Norton, P. G. (2009). Development and assessment of the Alberta Context Tool. Bmc Health Services Research, 9, 234 10.1186/1472-6963-9-234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans, B. A. , Snooks, H. , Howson, H. , & Davies, M. (2013). How hard can it be to include research evidence and evaluation in local health policy implementation? Results from a mixed methods study. Implementation Science, 8, 17 10.1186/1748-5908-8-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldstein, A. C. , & Glasgow, R. E. (2008). A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Joint Commission Journal on Quality and Patient Safety/Joint Commission Resources, 34(4), 228–243. 10.1016/S1553-7250(08)34030-6 [DOI] [PubMed] [Google Scholar]
- Florin, P. , Friend, K. B. , Buka, S. , Egan, C. , Barovier, L. , & Amodei, B. (2012). The Interactive Systems Framework Applied to the Strategic Prevention Framework: The Rhode Island Experience. American Journal of Community Psychology, 50(3–4), 402–414. [DOI] [PubMed] [Google Scholar]
- Gabbay, J. , le May, A. , & McCaughan, D. (2005). Primary care practitioners based everyday practice on internalised tacit guidelines derived through social interactions with trusted colleagues. Evidence Based Nursing, 8(3), 94. [DOI] [PubMed] [Google Scholar]
- Glasgow, R. E. (2013). What does it mean to be pragmatic? Pragmatic methods, measures, and models to facilitate research translation. Health Education and Behavior, 40, 257–265. [DOI] [PubMed] [Google Scholar]
- Graham, I. D. , Tetroe, J. , & Grp, K. T. T. R. (2007). Some theoretical underpinnings of knowledge translation. Academic Emergency Medicine, 14(11), 936–941. 10.1197/j.aem.2007.07.004 [DOI] [PubMed] [Google Scholar]
- Greenhalgh, T. , Robert, G. , MacFarlane, F. , Bate, P. , & Kyriakidou, O. (2004). Diffusion of innovations in service organizations: Systematic review and recommendations. Milbank Quarterly, 82(4), 581–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimshaw, J. , Ward, J. , & Eccles, M. (2006). Getting research into practice In Oxford handbook of public health practice (pp. 480–48). Oxford, UK: Oxford University Press. [Google Scholar]
- Hartling, L. , Scott‐Findlay, S. , Johnson, D. , Osmond, M. , Plint, A. , Grimshaw, J. , Klassen, T. P. , & CIHRTPEM (2007). Bridging the gap between clinical research and knowledge translation in pediatric emergency medicine. Academic Emergency Medicine, 14, 968–977. [DOI] [PubMed] [Google Scholar]
- Hartzler, B. , Lash, S. J. , & Roll, J. M. (2012). Contingency management in substance abuse treatment: A structured review of the evidence for its transportability. Drug and Alcohol Dependence, 122, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey, G. , & Kitson, A. (2016). PARIHS revisited: From heuristic to integrated framework for the successful implementation of knowledge into practice. Implementation Science, 11, 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynes, R. B. , Hayward, R. S. , & Lomas, J. (1995). Bridges between health care research evidence and clinical practice. Journal of the American Medical Informatics Association : JAMIA, 2(6), 342–350. 10.1136/jamia.1995.96157827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helfrich, C. D. , Blevins, D. , Smith, J. L. , Kelly, P. A. , Hogan, T. P. , Hagedorn, H. , … Sales, A. E. (2011). Predicting implementation from organizational readiness for change: A study protocol. Implementation Science, 6, 76 10.1186/1748-5908-6-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helfrich, C. D. , Damschroder, L. J. , Hagedorn, H. J. , Daggett, G. S. , Sahay, A. , Ritchie, M. , … Stetler, C. B. (2010). A critical synthesis of literature on the promoting action on research implementation in health services (PARIHS) framework. Implementation Science, 5, 82 10.1186/1748-5908-5-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemmelgarn, B. R. , Manns, B. J. , Straus, S. , Naugler, C. , Holroyd‐Leduc, J. , Braun, T. C. , … Tonelli, M. (2012). Knowledge translation for nephrologists: Strategies for improving the identification of patients with proteinuria. Journal of Nephrology, 25, 933–943. 10.5301/jn.5000226 [DOI] [PubMed] [Google Scholar]
- Herr, E. C. M. , English, M. J. , & Brown, N. B. (2003). Translating mental health services research into practice: A perspective from staff at the US substance abuse and mental health services administration. Alzheimer's Care Quarterly, 4(3), 241–253. [Google Scholar]
- Heyland, D. K. , Dhaliwal, R. , Cahill, N. E. , Carli, F. , Flum, D. , Ko, C. , … McClave, S. A. (2013). Driving perioperative nutrition quality improvement processes forward! Journal of Parenteral and Enteral Nutrition, 37(5 Suppl), 83S–98S. [DOI] [PubMed] [Google Scholar]
- Ho, K. , Bloch, R. , Gondocz, T. , Laprise, R. , Perrier, L. , Ryan, D. , … Wenghofer, E. (2004). Technology‐enabled knowledge translation: Frameworks to promote research and practice. The Journal of Continuing Education in the Health Professions, 24(2), 90–99. 10.1002/chp.1340240206 [DOI] [PubMed] [Google Scholar]
- Ilott, I. , Gerrish, K. , Booth, A. , & Field, B. (2013). Testing the Consolidated Framework for Implementation Research on health care innovations from South Yorkshire. Journal of Evaluation in Clinical Practice, 19, 915–924. [DOI] [PubMed] [Google Scholar]
- Ivers, N. , Jamtvedt, G. , Flottorp, S. , Young, J. M. , Odgaard‐Jensen, J. , French, S. D. , … Oxman, A. D. . (2012). Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews, 6 Art. No.: CD000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack, S. , & Tonmyr, L. (2008). Knowledge Transfer and Exchange: Disseminating Canadian Child Maltreatment Surveillance Findings to Decision Makers. Child Indicators Research, 1, 51–64. 10.1007/s12187-007-9001-3 [DOI] [Google Scholar]
- Jacobson, N. , Butterill, D. , & Goering, P. (2005). Consulting as a strategy for knowledge transfer. Milbank Quarterly, 83, 299–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn, K. L. , Mendel, P. , Leuschner, K. J. , Hiatt, L. , Gall, E. M. , Siegel, S. , & Weinberg, D. A. (2014). The national response for preventing healthcare‐associated infections: Research and adoption of prevention practices. Medical Care, 52(2 Suppl 1), S33–S45. [DOI] [PubMed] [Google Scholar]
- Kastner, M. , & Straus, S. E. (2012). Application of the Knowledge‐to‐Action and Medical Research Council frameworks in the development of an osteoporosis clinical decision support tool. Journal of Clinical Epidemiology, 65, 1163–1170. [DOI] [PubMed] [Google Scholar]
- Kavanagh, T. , Watt‐Watson, J. , & Stevens, B. (2007). An examination of the factors enabling the successful implementation of evidence‐based acute pain practices into pediatric nursing. Children's Health Care, 36(3), 303–321. [Google Scholar]
- Kiefer, L. , Frank, J. , Di Ruggiero, E. , Dobbins, M. , Manuel, D. , Gully, P. R. , & Mowat, D. (2005). Fostering evidence‐based decision‐making in Canada – Examining the Need for a Canadian Population and Public Health Evidence Centre and Research Network. Canadian Journal of Public Health‐Revue Canadienne De Sante Publique, 96(3), I1–I19. [PubMed] [Google Scholar]
- Kitson, A. , Powell, K. , Hoon, E. , Newbury, J. , Wilson, A. , & Beilby, J. (2013). Knowledge translation within a population health study: How do you do it? Implementation Science, 8, 54 10.1186/1748-5908-8-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan, A. , Nongkynrih, B. , Kapoor, S. K. , & Pandav, C. (2009). A role for INDEPTH Asian sites in translating research to action for non‐communicable disease prevention and control: A case study from Ballabgarh, India. Global Health Action, 2, 76–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristensen, H. K. , Borg, T. , & Hounsgaard, L. (2011). Facilitation of research‐based evidence within occupational therapy in stroke rehabilitation. British Journal of Occupational Therapy, 74, 473–483. 10.4276/030802211X13182481841949 [DOI] [PubMed] [Google Scholar]
- Kutner, J. S. (2011). A significant milestone for palliative care: Imperative for dissemination and implementation research. Journal of Palliative Medicine, 14(11), 1194–1195. 10.1089/jpm.2011.9639 [DOI] [PubMed] [Google Scholar]
- Levac, D. , Colquhoun, H. , & O'Brien, K. K. (2010). Scoping studies: Advancing the methodology. Implementation Science, 5, 69 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan, J. , & Graham, I. D. (1998). Toward a comprehensive interdisciplinary model of health care research use. Science Communication, 20, 227–246. 10.1177/1075547098020002004 [DOI] [Google Scholar]
- Logan, J. , Harrison, M. B. , Graham, I. D. , Dunn, K. , & Bissonnette, J. (1999) Evidence‐based pressure‐ulcer practice: The Ottawa model of research use. The Canadian Journal of Nursing Research = Revue Canadienne de Recherche en Sciences Infirmières, 31(1), 37–52. [PubMed] [Google Scholar]
- Mark, D. D. , Latimer, R. W. , & Hardy, M. D. (2010). Stars aligned for evidence‐based practice: A triservice initiative in the pacific. Nursing Research, 59, S48–S57. [DOI] [PubMed] [Google Scholar]
- McCaughan, D. (2005). Primary care practitioners based everyday practice on internalised tacit guidelines derived through social interactions with trusted colleagues. Evidence Based Nursing, 8(3), 94 10.1136/ebn.8.3.94 [DOI] [PubMed] [Google Scholar]
- McKibbon, K. A. , Lokker, C. , Keepanasseril, A. , Colquhoun, H. , Haynes, R. B. , & Wilczynski, N. L. (2013). WhatisKT wiki: A case study of a platform for knowledge translation terms and definitions – descriptive analysis. Implementation Science, 8, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeill, D. , & Kelley, E. (2005). How the National Healthcare Quality and Disparities Reports can catalyze quality improvement. Medical Care, 43, 82–88. [DOI] [PubMed] [Google Scholar]
- Mende, P. L. , Meredith, L. S. , Schoenbaum, M. , Sherbourne, C. D. , & Wells, K. B. (2008). Interventions in organizational and community context: A framework for building evidence on dissemination and implementation in health services research. Administration and Policy in Mental Health and Mental Health Services Research, 35, 21–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milner, M. , Estabrooks, C. A. , & Myrick, F. (2006). Research utilization and clinical nurse educators: A systematic review. Journal of Evaluation in Clinical Practice, 12, 639–655. [DOI] [PubMed] [Google Scholar]
- Mitton, C. , Adair, C. E. , McKenzie, E. , Patten, S. B. , & Perry, B. W. (2007). Knowledge transfer and exchange: Review and synthesis of the literature. Milbank Quarterly, 85(4), 729–768. 10.1111/j.1468-0009.2007.00506.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , Altman, D. G. , & Grp, P. (2009). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. Journal of Clinical Epidemiology, 62(10), 1006–1012. 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- Moore, M. L. (1999). From randomized trial to community‐focused practice. Journal of Nursing Scholarship, 31(4), 349–354. [DOI] [PubMed] [Google Scholar]
- Nakata, M. , Kuriyama, S. , Mitsuyasu, K. , Morimoto, M. , & Tomioka, K. (1989). Transfer of innovation for advancement in dentistry: A case study on pit and fissure sealants’ use in Japan. International Dental Journal, 39(4), 263–268. [PubMed] [Google Scholar]
- Obrecht, J. A. , Van Hulle Vincent, C. , & Ryan, C. S. (2014). Implementation of evidence‐based practice for a pediatric pain assessment instrument. Clinical Nurse Specialist, 28(2), 97–104. [DOI] [PubMed] [Google Scholar]
- Orlandi, M. A. (1987). Promoting health and preventing disease in health care settings: An analysis of barriers. Preventive Medicine, 16(1), 119–130. 10.1016/0091-7435(87)90011-9 [DOI] [PubMed] [Google Scholar]
- Palmer, D. , & Kramlich, D. (2011). An introduction to the multisystem model of knowledge integration and translation. Advances in Nursing Science, 34, 29–38. 10.1097/ANS.0b013e318209439f [DOI] [PubMed] [Google Scholar]
- Pentland, D. , Forsyth, K. , Maciver, D. , Walsh, M. , Murray, R. , Irvine, L. , & Sikora, S. (2011). Key characteristics of knowledge transfer and exchange in healthcare: Integrative literature review. Journal of Advanced Nursing, 67(7), 1408–1425. 10.1111/j.1365-2648.2011.05631.x [DOI] [PubMed] [Google Scholar]
- Petzold, A. , Korner‐Bitensky, N. , & Menon, A. (2010). Using the knowledge to action process model to incite clinical change. Journal of Continuing Education in Health Professions, 30(3), 167–171. [DOI] [PubMed] [Google Scholar]
- Prihodova, L. , Guerin, S. , & Kernohan, W. G. (2015). Knowledge transfer and exchange frameworks in health and their applicability to palliative care: Scoping review protocol. Journal of Advanced Nursing, 71(7), 1717–1725. 10.1111/jan.12642 [DOI] [PubMed] [Google Scholar]
- Proctor, E. K. , Landsverk, J. , Aarons, G. , Chambers, D. , Glisson, C. , & Mittman, B. (2009). Implementation research in mental health services: An emerging science with conceptual, methodological and training challenges. Administration and Policy in Mental Health and Mental Health Services Research, 36(1), 24–34. 10.1007/s10488-008-0197-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronovost, P. , Berenholtz, S. , & Needham, D. (2008). Translating evidence into practice: A model for large scale knowledge translation. British Medical Journal, 337, a1714 10.1136/bmj.a1714 [DOI] [PubMed] [Google Scholar]
- Rogers, J. L. (2009). Transferring research into practice an integrative review. Clinical Nurse Specialist, i, 192–199. [Google Scholar]
- Rubenstein, L. V. E. , Chaney, F. , Ober, S. , Felker, B. , Sherman, S. E. , Lanto, A. , & Vivell, S. (2010). Using evidence‐based quality improvement methods for translating depression collaborative care research into practice. Families Systems and Health, 28(2), 91–113. [DOI] [PubMed] [Google Scholar]
- Ruffolo, M. C. , & Capobianco, J. (2012). Moving an evidence‐based intervention into routine mental health care: A multifaceted case example. Social Work in Health Care, 51, 77–87. [DOI] [PubMed] [Google Scholar]
- Russell‐Babin, K. A. , & Miley, H. (2013). Implementing the best available evidence in early delirium identification in elderly hip surgery patients. International Journal of Evidence‐Based Healthcare, 11(1), 39–45. [DOI] [PubMed] [Google Scholar]
- Rycroft‐Malone, J. (2004). The PARIHS framework – A framework for guiding the implementation of evidence‐based practice. Journal of Nursing Care Quality, 19(4), 297–304. 10.1097/00001786-200410000-00002 [DOI] [PubMed] [Google Scholar]
- Rycroft‐Malone, J. , Kitson, A. , Harvey, G. , McCormack, B. , Seers, K. , Titchen, A. , & Estabrooks, C. (2002). Ingredients for change: Revisiting a conceptual framework. Quality & Safety in Health Care, 11, 174–180. 10.1136/qhc.11.2.174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rycroft‐Malone, J. , Seers, K. , Chandler, J. , Hawkes, C. A. , Crichton, N. , Allen, C. , … Strunin, L. (2013). The role of evidence, context, and facilitation in an implementation trial: Implications for the development of the PARIHS framework. Implementation Science, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakala, C. , & Mayberry, L. J. (2006). Vaginal or cesarean birth? Application of an advocacy organization‐driven research translation model. Nursing Research, 55, S68–S74. 10.1097/00006199-200603001-00011 [DOI] [PubMed] [Google Scholar]
- Santesso, N. , & Tugwell, P. (2006). Knowledge translation in developing countries. Journal of Continuing Education in Health Professions, 26(1), 87–96. [DOI] [PubMed] [Google Scholar]
- Silva, A. B. , Morel, C. M. , & de Moraes, I. H. S. (2014). Proposal for a telehealth concept in the translational research model. Revista de saúde pública, 48(2), 347–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterling, S. , & Weisner, C. (2006). Translating research findings into practice ‐ Example of treatment services for adolescents in managed care. Alcohol Research & Health, 29, 11–18. [PMC free article] [PubMed] [Google Scholar]
- Stetler, C. B. (2003). Role of the organization in translating research into evidence‐based practice. Outcomes Management, 7(3), 97–103. [PubMed] [Google Scholar]
- Straus, S. E. , Tetroe, J. , & Graham, I. (2009). Defining knowledge translation. Canadian Medical Association Journal, 181(3–4), 165–168. 10.1503/cmaj.081229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavernier, S. S. (2014). Translating research on the distress thermometer into practice. Clinical Journal of Oncology Nursing, 18, 26–30. [DOI] [PubMed] [Google Scholar]
- Thomson‐O'Brien, M. A. , & Moreland, J. (1998). Evidence‐based practice information circle… adapted from a presentation at the 1996 Canadian Physiotherapy Association Congress in Victoria, British Columbia. Physiotherapy Canada, 50(3), 184. [Google Scholar]
- Tilson, J. K. , & Mickan, S. (2014). Promoting physical therapists’ of research evidence to inform clinical practice: Part 1‐theoretical foundation, evidence and description of the PEAK program. Bmc Medical Education, 14, 125 10.1186/1472-6920-14-125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tschannen, D. , Talsma, A. , Gombert, J. , & Mowry, J. L. (2011). Using the TRIP model to disseminate an IT‐based pressure ulcer intervention. Western Journal of Nursing Research, 33, 427–442. 10.1177/0193945910379436 [DOI] [PubMed] [Google Scholar]
- Tugwell, P. , O'Connor, A. , Andersson, N. , Mhatre, S. , Kristjansson, E. , Jacobsen, M. J. , … Losos, J. (2006). Reduction of inequalities in health: Assessing evidence‐based tools. International Journal for Equity in Health, 5, 11 10.1186/1475-9276-5-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tugwell, P. , Robinson, V. , Grimshaw, J. , & Santesso, N. (2006). Systematic reviews and knowledge translation. Bulletin of the World Health Organization, 84, 643–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullrich, P. M. , Sahay, A. , & Stetler, C. B. (2014). Use of implementation theory: A focus on PARIHS. Worldviews on Evidence‐Based Nursing, 11, 26–34. [DOI] [PubMed] [Google Scholar]
- Unützer, J. , Powers, D. , Katon, W. , & Langston, C. (2005). From establishing an evidence‐based practice to implementation in real‐world settings: IMPACT as a case study. Psychiatric Clinics of North America, 28(4), 1079–1092. [DOI] [PubMed] [Google Scholar]
- Urquhart, R. , Porter, G. A. , & Grunfeld, E. (2011). Reflections on knowledge brokering within a multidisciplinary research team. Journal of Continuing Education in the Health Professions, 31, 283–290. [DOI] [PubMed] [Google Scholar]
- Urquhart, R. , Sargeant, J. , & Grunfeld, E. (2013). Exploring the usefulness of two conceptual frameworks for understanding how organizational factors influence innovation implementation in cancer care. Journal of Continuing Education in the Health Professions, 33, 48–58. [DOI] [PubMed] [Google Scholar]
- Wallace, L. M. , Brown, K. E. , & Hilton, S. (2014). Planning for, implementing and assessing the impact of health promotion and behaviour change interventions: A way forward for health psychologists. Health Psychology Review, 8, 8–33. [DOI] [PubMed] [Google Scholar]
- Ward, V. , House, A. , & Hamer, S. (2009a). Developing a framework for transferring knowledge into action: A thematic analysis of the literature. Journal of Health Services Research & Policy, 14(3), 156–164. 10.1258/jhsrp.2009.008120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward, V. L. , House, A. O. , & Hamer, S. (2009b). Knowledge brokering: Exploring the process of transferring knowledge into action. BMC Health Services Research, 9(1), 12 10.1186/1472-6963-9-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward, V. , Smith, S. , Foy, R. , House, A. , & Hamer, S. (2010). Planning for knowledge translation: A researcher's guide. Evidence & Policy: A Journal of Research, Debate and Practice, 6, 527–541. 10.1332/174426410X535882 [DOI] [Google Scholar]
- Ward, V. , Smith, S. , House, A. , & Hamer, S. (2012). Exploring knowledge exchange: A useful framework for practice and policy. Social Science & Medicine, 74(3), 297–304. 10.1016/j.socscimed.2011.09.021 [DOI] [PubMed] [Google Scholar]
- Wilkins, N. , Thigpen, S. , Lockman, J. , Mackin, J. , Madden, M. , Perkins, T. , … Donovan, J. (2013). Putting program evaluation to work: A framework for creating actionable knowledge for suicide prevention practice. Translational Behavioral Medicine, 3(2), 149–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson, P. M. , Petticrew, M. , Calnan, M. W. , & Nazareth, I. (2010). Disseminating research findings: What should researchers do? A systematic scoping review of conceptual frameworks. Implementation Science, 5, 91 10.1186/1748-5908-5-91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, J. , McCormack, B. , Coffey, A. , & McCarthy, G. (2007). Evaluating the context within which continence care is provided in rehabilitation units for older people. International Journal of Older People Nursing, 2(1), 9–19. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


