Abstract
Introduction
Caregivers of women with breast cancer in low-and-middle-income countries experience significant physical and economic burdens. The review aimed to map the evidence of studies that had reported on the experiences of family caregivers of women diagnosed with breast cancer.
Methods
A systematic literature search was conducted in CINAHL, PubMed, PsycINFO, Scopus, and Web of Science databases using a combination of key search terms and medical subject heading terms such as “family caregiver,” “breast cancer,” “home care,” “low-and-middle-income countries,” “experience,” “effect,” and “coping mechanism.” A total of 1781 articles were retrieved and screened. Nineteen studies addressing caregiving experiences were included in the final review based on the inclusion and exclusion criteria.
Results
The systematic review yielded 19 studies that focused on caregivers’ motivation, needs of caregivers, intervention for caregivers, and consequences of caregiving. The most significant correlates of the quality of life among caregivers were disease severity, functional status of patients, and family income. The challenges encountered by caregivers were mostly psychosocial.
Conclusions
Caregivers play a crucial role in the management of women with breast cancer. However, they are faced with increasing challenges in their caregiving roles. Understanding the nature and extent of the burden experienced by family caregivers in developing countries will facilitate the development of appropriate interventions that can help improve caregivers’ quality of life. Gaps in recent studies were identified, and suggestions for future research were also addressed in this review.
Systematic review registration
PROSPERO CRD42019118391
Keywords: Breast cancer, Family caregiver, Low- and middle-income countries, Experiences
Introduction
The increasing incidence and mortality rate of breast cancer has produced challenges in caring for women with breast cancer, especially in low- and middle-income countries (LMICs) [1, 2]. This challenge has implications for relatives and friends who become family caregivers [3]. Breast cancer treatment is now shifting from an inpatient setting to a more outpatient setting due to contextual barriers to oncology services that exist in LMICs, such as limited availability of treatment facilities, lack of cancer specialists [4], and limited geographical access to oncology care [5]. This shift has resulted in the role of family caregivers as significant members of the cancer care system who are expected to provide physical, emotional, financial, and psychosocial support to women diagnosed with breast cancer in the home setting [6–9]. However, according to Khanjari et al. [10], the current declining socioeconomic trends in LMICs potentially alter the capacity of caregivers to meet the growing demand for home care support for women with breast cancer.
The burden of breast cancer caregiving includes emotional distress, financial burden, physical stress, and fear of uncertainty among caregivers [11–13]. Furthermore, the advanced stage disease presentation, a hallmark of this disease in LMICs, can result in increased psychosocial morbidity, poor physical health, and overall poor quality of life among caregivers [6, 10, 11, 14]. Hashemi-Ghasemabadi et al. [6] have indicated that caregivers who deliver care to women with breast cancer in LMICs experience unique challenges due to under-resourced and limited cancer support systems. For instance, few West African studies focusing on this phenomenon have highlighted that challenges encountered by caregivers include loss of job, difficulty in balancing multiple roles, a decline in physical health, lack of access to healthcare funding, emotional trauma, and lack of information in managing breast cancer-related symptoms such as wound and lymphedema [4, 15]. A recent Ghanaian study reporting on the motivation and caregiving experiences of family caregivers of advanced breast cancer patients showed that sociocultural obligation and reciprocity were the main reasons for assuming the caregiving role [4]. Further, the study also highlighted that caregivers provided multi-dimensional forms of support such as physical, psychosocial, emotional, financial, symptom management, and spiritual support for women living with advanced breast cancer. Financial burden through the provision of out-of-pocket money for treatment costs and other related non-medical costs were the main challenge reported by participants in this study [4]. The study recommended home-based support programs and direct governmental social intervention programs to assist caregivers in their caring role.
However, to date, no systematic review of family caregiving in breast cancer that is specific to LMICs has been conducted to fully understand the experiences and challenges faced by this group of caregivers. Exploring the experiences of family caregivers is critical in providing potential interventions that can aid in addressing the needs of family caregivers in LMICs. Hence, the rationale of this systematic review was to summarize and appraise existing evidence on studies that had reported on:
Home care experiences of caregivers of women diagnosed with breast cancer in LMICs.
Effects of caregiving on the family caregivers in LMICs.
Coping mechanisms utilized by family caregivers of women living with breast cancer in LMICs.
Materials and methods
The protocol of this review is duly registered (CRD42019118391) in the PROSPERO international prospective register of systematic reviews. Studies that explored the experiences of caregivers living with breast cancer patients in LMICs were searched.
Inclusion and exclusion criteria
All studies (quantitative studies, qualitative studies, and mixed-method studies) were conducted in diverse settings such as hospitals or communities published from January 2000 to March 2020. Other criteria for inclusion were (1) family caregivers of breast cancer patients aged 18 years and above, (2) providing non-paid caregiving services to breast cancer patients, (3) full-text published articles from LMICs (low-and-middle-income country was operationalized in this study as low-, lower-middle, and upper-middle-income economy based on the January 2020 World Bank list of analytical income classification of economies) [16], (4) reporting on family caregivers experiences, and (5) articles published in the English language.
Exclusion criteria
Studies were excluded from this review based on the following criteria: (1) focused on paid and formal caregivers such as healthcare professionals; (2) not published in the English language (due to limited availability of translation service to the authors); and lastly, (3) systematic reviews, abstracts, editorial reports, letters, conference articles, and gray literatures with no full-text published articles were excluded because they were not considered as scientific published articles.
Search strategy
A systematic review was conducted according to the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P). We conducted a comprehensive search of qualitative, quantitative, and mixed-methods literature that was published from January 2000 to March 2020 in the electronic databases, i.e., PubMed, CINAHL, Scopus, Web of Science, and PsycINFO, to retrieve all English language literature that contained information on family caregivers of breast cancer patients in low- and middle-income countries. As previously defined, studies were defined into “low-income,” “lower-middle-income,” and “upper-middle-income” countries as categorized by the World Bank [16]. Primary concepts such as “family caregiver,” “breast cancer,” “home care,” “low-and-middle-income-countries,” “experience,” “effect,” and “coping” and their Medical Subject Headings (MESH) were used for the search (Additional file 1: Table S1). The subject search and text word search were performed separately in all the databases and then combined with Boolean operators “OR” and “AND.” Combined terms used, for example, were (“Caregiv*(MESH)” OR “Family caregiv (MESH)*”) AND (“Breast cancer (MESH)” OR “Breast neoplasm*(MESH)”) AND (“low-income countr*[tw]” OR “lower-middle-income countr*[tw]”). Additional articles were searched from other sources such as Google Scholar as well as hand-searching the references of all included studies. This produced three additional articles from Google Scholar [17–19].
Literature screening
Following the literature search, citations were imported into Mendeley Desktop (version 1.19.4) reference manager for storage and screening of articles as well as the removal of duplicates. The remaining articles were then screened independently by titles and abstracts. Two reviewers (GK and KBM) screened all the citations that were identified from the search using standard systematic review procedures (inclusion and exclusion criteria). Any disagreement was resolved by discussion and consensus or by consulting a third reviewer (ABBM) where needed.
Quality appraisal or assessment tool
The quality of the selected studies was assessed independently by GK and KBM using the Mixed Methods Appraisal Tool (MMAT) version 2018 [20]. This tool has been developed to evaluate qualitative, quantitative, and mixed-method studies using two screening questions and four methodological criteria. The tool assesses the appropriateness of the aim of the study, adequacy and methodology, study design, participant recruitment, data collection, data analysis, presentation of findings, authors’ discussions, and conclusions [21]. Each question carries three possible responses: “yes,” “no,” or” can’t tell.” A star is assigned (four stars maximum possible score) to each yes response and is converted to percentages (from one star = 25% to four stars = 100%) [20]. Using the aforementioned domains, score from 0–25% is regarded as weak, 50% is regarded as moderate, 75% is regarded as moderate-strong, and 100% is regarded as strong [20].
The interrater reliability for each MMAT dimension for quality ratings of the included studies was evaluated using Cohen’s kappa statistic [22]. This was done to assess the level of agreement of quality ratings between the two independent authors (GK and KBM) who performed the quality assessment for the included studies. The interrater reliability of each MMAT dimension was assessed and reported as Cohen’s kappa coefficient and 95% confidence interval (95% CI) with two-sided p value. Acceptable kappa values 0.80–0.90, > 0.90, and 1.0 represent strong, almost perfect, and excellent levels of agreement between raters [22].
Data extraction and analysis
Two reviewers (GK and KBM) independently extracted key characteristics from the included articles: bibliographic information (authors’ name, year of publication, country, and address). Others included the methodology (study aim, design, setting, and sample size), caregivers’ characteristics, and major findings on caregivers’ experiences, conclusions, and limitations of the study as described in Table 1. There was significant heterogeneity in the measurement of the outcomes of the eligible studies, making it impossible to pool data in a meta-analysis. Therefore, a narrative analysis or strategy was employed to synthesize the evidence.
Table 1.
Summary of study characteristics and findings
| Author/year | Country | Aim/research questions | Study design | Caregivers | Findings | Conclusion | Limitation |
|---|---|---|---|---|---|---|---|
| Vahidi et al. (2016) [3] | Iran | Determine factors associated with caregiver burden among primary caregivers of women with breast cancer | Descriptive correlation study | 150 primary caregivers; caregivers mean age 39.60 years; 77 (51.3%) were males | Caregivers assisted with activities of daily living, administering medication, symptom management, and financial support. Higher caregiver burden was associated with increasing assistance with activities of daily living, low educational level, gender, and poor financial status | Caregivers must be provided with comprehensive care needs support. Primary caregivers need to be supported financially by relevant organizations, such as government agencies and charities. Other factors such as dedicating a place for caregivers in the clinic to receive care skills training from expert nurses can be effective | Cross-sectional studies do not show the difference in burden in response to cancer progression in the patient; therefore, longitudinal studies are recommended |
| Gabriel, Aluko and Okeme (2019) [15] | Nigeria | Impact of caregiving burden on the informal caregivers of women with breast cancer | Descriptive study | 118 caregivers; mean age = 41.9 years. Most were child (77.1%), spouse (14.4%), and others (8.5%) | Determinants of high caregiver burden were payment type for treatment, family income, relationship to the patient, social support, and self-efficacy | Strategies to improve self-efficacy such as additional training, follow-up, peer education, and support groups for caregivers might decrease the caregiver burden | Use of convenience sampling making it difficult to identify causal relationships |
| Zhu et al. (2014) [31] | China | To assess the quality of life in male spouse caregivers | Cross-sectional study | 243 spouse caregivers. Mean age = 49.5 years | Decreasing patient functional status was significantly associated with poor quality of life among caregivers. High family income and longer sleeping time increased the quality of life among caregivers | Attention should be paid to male spouse caregivers as a separate group. Nurses can understand the status of caregiver burden and QOL by assessing both patients and spouses. The mental health of spouse caregivers was disrupted more seriously than the physical health | The study focused on spouse caregivers and hence cannot be generalized for other non-spousal caregivers |
| Hashemi-Ghasemabadi et al. (2016) [6] | Iran | Transition to the new role of caregiving for families of women with breast cancer diagnosis | Qualitative descriptive exploratory study | 23 caregivers. Mean age = 37.5 years. 69.6% were females and 30.4% men |
Emerged themes: •“Grasping a new situation without preparation” •“Perceived inefficiency” •“Infinite absence” •“Abandoned in the role” Caregivers cited that they were unprepared for their new role and did not have the necessary skills and knowledge to manage breast cancer and its related symptoms. Caregiving was also described as a time-consuming role which competed with other family roles and responsibilities. |
By understanding their experiences in the transition to the new role, it is possible to provide detailed information for designing evidence-based healthcare interventions and comprehensive family-centered care program. Also, interventions can be tailored to the objectives and resource limitations, for the support and resolution of the challenges of caregivers to decrease the negative consequences of caregiving | Study could not be generalized because it is a qualitative study. Provided limited information on coping strategies |
| Sahadevan et al. (2019) [26] | India | Identify the determinants of depression among caregivers of patients with breast cancer | Cross-sectional survey | 384 caregivers. Mean age = 47.25 years. 163 (42.4%) were males | Higher financial responsibilities, being a spousal caregiver are important determinants of depression among caregivers | Cancer specialists in treatment team need to be aware of the need for psychological assessment of principal caregivers. They should be trained to pick up depressive symptoms and its associated risk factors at the earliest and should be offered services to the needful. This approach ultimately improves the outcome of cancer treatment | This cross-sectional survey was a hospital-based study and may not be generalizable to all caregivers in India |
| Jaafar et al. (2014) [24] | Malaysia | To examine the rates of clinical depressive disorders in caregivers during breast cancer treatment | Cross-sectional study | 130 caregivers comprising of spouses (46.9%), children (40.0%), and siblings (13.1%) | Depressive disorders were related to low educational status of caregivers and high duration of caregiving | This finding gives clues to intervening depression among the caregivers by providing support in the form of respite care to the caregivers and improving engagement of the caregivers by the health care providers. The results should increase the health care providers’ awareness of the vulnerability of this population and discard a patient-centric approach of treatment | Data on coping mechanism were missing in this study. The study was conducted in a single facility which might limit generalizability to similar population |
| Gabriel and Mayers (2019) [27] | Nigeria | To assess the effectiveness of a psychosocial intervention in reducing caregiver burden among caregivers | Quasi-experimental study | 108 caregivers; intervention group (54); control group (54). Caregivers were primarily spouse (30.6%), parent (15.7%), sibling (17.6%), child (21.3%), and friend (14.8%) | Primary caregivers who received the psychosocial intervention reported significant decrease in burden at 6 weeks and 12 weeks. Further, the psychosocial intervention also improved the overall quality of life of caregivers | The need for effective advocacy on the issue of caregiver burden is vital. Relevant stakeholders in the healthcare sector, especially in palliative care, should conduct advocacy campaigns to promote the culture of caring and support for the person with cancer and the caregiver | Non-randomized deign was used to recruit participants. Psychosocial intervention did not address the subjective aspect of the caregiver burden |
| Giray and Akyuz (2019) [28] | Turkey | To assess relationships between caregiver burden, quality of life, arm disability, grip strength, and lymphedema symptoms in patients with postmastectomy lymphedema | Prospective cross-sectional study | 52 caregivers. Mean age = 48.46 years. 14 (26.9%) were females and 38 (73.1%) were males | Caregiver burden was associated with arm disability and quality of life of these patients. Arm disability affects caregiver burden and quality of life in these patients. Arm disability was higher in patients at stage 3 lymphedema than patients at milder stages | Arm disability should be diagnosed and treated to improve caregiver burden and quality of life | This was an observational study using a convenience sample. Comparison of caregiver burden before and after lymphedema development and treatment can more enlighten the importance of caregiver burden in the management of patients with postmastectomy lymphedema |
| Moreno-Gonzalez et al. (2019) [29] | Mexico | To describe the experience of family care of women with breast cancer during treatment from the perspective of caregivers | Qualitative study | Seven caregivers (3 men and 4 women) | Male caregivers stated that the absence of a breast did not interfere with the perception of their femininity or sexual attractiveness. Caregivers experienced fear and despair for not knowing how to alleviate women symptoms. Also, caregivers experienced fear of the unknown and sometimes anger. They also looked for strategies to maintain their emotional balance. Female caregivers living this experience expressed a greater perception of the risk of suffering from breast cancer, which favored their self-care by knowing about the timely detection | The experience of caregivers of women with breast cancer generated profound changes in them through the discovery of their reach and limitations in difficult situations | The study leaves aside different contexts and events such as rupture between couple and family disintegration that may prevail |
| Wulandari et al. (2017) | Indonesia | Determine the experience of stress and adaptation of breast cancer patient’s family | Qualitative method | 7 male caregivers | Caregivers cited that they experience stressors related to difficulty in managing of the disease and the financial needs of the patient. Caregivers further reported that financial problem became a stressor from the beginning until the end of the breast cancer treatment. Components of caregiver coping mechanism consisted of strategies such as emotional support from health professionals, prayer, and gratitude | The experience of stress and adaptation of the family of breast cancer patients is a continuous stage. Continued coping such as support from professional nurses may be needed to minimize the stress and improve adaptation of family caregivers | Caregivers in this study was small. Study did not explain comprehensively measures that were undertaken to ensure trustworthiness of the study |
| Bahrami and Farzi (2014) [18] | Iran | Determine the effect of a supportive educational program on the caregiving burden and quality of life in the family caregivers of women with breast cancer | Two‑group two‑step before–after clinical trial |
64 family caregivers. Mean age (control group) = 38.97 Mean age (experimental group) |
The study implemented a supportive educational program to a group of caregivers. After the intervention has been implemented, the results showed that in the experimental group, the mean score of physical, mental, spiritual, and environmental domains and overall quality of life in the family caregivers was significantly increased compared to the control group. Further, in the experimental group, the mean score of caring burden among the caregivers was significantly decreased compared to the control group | The findings of the study suggested that supportive educational program can improve physical, psychological, spiritual, and environmental domains and overall quality of life. It can also decrease the caring burden in the family caregivers of women with breast cancer | Small sample size was used |
| Mahadevan et al. (2013) [32] | Malaysia | To determine the proportion of stress among the caregivers of breast cancer patients receiving oncologic treatment at Kuala Lumpur Hospital and to determine the predictors of stress among the caregivers | A cross-sectional study | 130 caregivers with mean age of 42.8 ± 14.5 years | Generally, caregivers had higher levels of stress. Approximately 16% of caregivers felt emotionally strained and 26% acknowledge that taking care of the patient is hard on them emotionally. In addition, caregivers felt less in control of their lives. Caregivers who looked after older patients were less likely to be stressed | There should be awareness among medical personnel about the high likelihood of stress among the family caregivers of breast cancer patients and a heightened sensitivity to the caregivers’ emotional condition. Caregivers should have easy access to mental health services. There should be respite care facilities in order to relieve the caregivers from constant caregiving burden and stress | The study was cross-sectional in design, whereby being conducted at one point of time; no causal relationship can be inferred between the outcomes and the variables. The application of non-random sampling method within a convenience samples frame could create sampling bias, resulting in over- or under-representation of certain members of the study population |
| Yeung et al. (2018) [30] | China | This study aimed to examine the experience of guilt and its correlates among Chinese husbands of women with breast cancer | A cross-sectional survey | 176 husbands caregivers with mean age of 50.22 years | Lower endorsement of the “masculinity strength” gender-role norm, and higher caregiving burden and social support seeking were associated with higher caregiving guilt. Unexpectedly, higher marital satisfaction and less protective buffering were associated with higher caregiving guilt. Younger husband caregivers in our sample were more likely to report higher guilt. Also, caregiving burden was associated with caregiver guilt. Also, protective buffering and caregiver guilt was conditional to caregiver’s level of marital satisfaction | The new findings and complex interplay between caregivers’ characteristics (including endorsement of male gender-role norms and marital satisfaction) and coping strategies (protective buffering and seeking social support) in predicting guilt imply that individual and cultural characteristics may change the effectiveness of specific coping strategies in cancer caregivers’ well-being | Caregivers were recruited from two hospitals. Hence, sample may not be representative of the total population of caregivers of breast cancer patients |
| Heidari Gorji et al. (2012) | Iran | To examine the correlates of depression in relation to quality of life among breast cancer caregivers | A cross-sectional descriptive design | Findings were demonstrated that high percent of caregivers were afflicted by mild and moderate depression. The results showed that 42 and 11% reported moderate and low quality of life, respectively. The study demonstrate that psychological issues have a significant impact on quality of life | The study demonstrate that psychological issues have a significant impact on quality of life. Additionally, help and attention to caregivers would be beneficial in improving quality of life of all family of patients | This is a cross-sectional study; hence, results may not be generalizable to all caregivers in Iran | |
| Yuanyuan An et al. (2019) | China | To identify the influence of family caregiver’s burden on breast cancer patient’s QoL and possible mediators | A cross-sectional design | 382 caregivers | Higher level of family caregiver’s burden was associated with higher levels of patient’s anxiety and depression | Given the important role of family caregiver’s burden, it should be targeted by the intervention aiming to improve breast cancer patients’ QoL and well-being | The data were cross-sectional, which precludes conclusions regarding causation and the direction of relationship among variables. Second, the findings are only generalizable to the population studied |
| Nejad et al. (2016) | Iran | Determine and compare the caregiver strain index scores of breast cancer informal caregivers, before and after a patient-caregiver educational and telephone follow-up program | Experimental study design |
60 caregivers Mean age > 30 (28.3 years) 30–50 (43.3 years) < 50 (28.3 years) |
The mean caregiver strain score of the intervention group was 8.3 ± 2, and it dropped to 4.8 ± 2.3 post-intervention | Caregiver burden decreased significantly in the intervention group after the patient-caregiver education and follow-up program (P < 0.001) | The intervention period was relatively short, thus limiting the generalizability of the results |
| Din et al. (2017) [25] | Malaysia | To determine the anxiety disorders specifically focusing on the family caregivers of breast cancer patients | A cross-sectional study | 130 caregiver-patient dyads |
The study found that more than a 10th (11.5%, n = 15) of the family members who were primarily involved in caring for breast cancer patients had anxiety disorders. Specifically, 8 caregivers (6.1%) had generalized anxiety disorder, 6 were (4.6%) diagnosed to have panic disorder, and one (0.8%) had social phobia associated with both the patients’ type of treatment and non-shared caregiving |
A multidisciplinary management approach should be extended to those at risk which would directly and inadvertently optimize the treatment care for patients with breast cancer | It was cross-sectional in design that the direction of the factors and the risk factors of anxiety disorders could not be established. The small sample size limited the power of the study to detect any other factors particularly involving the caregiving process such as duration of care that could have significance to the anxiety disorders |
| Khanjari et al. (2014) [35] | Iran | To explore how family caregivers of women with breast cancer in Iran describe the areas in life which are important to their quality of life (QoL) and to determine which areas in life that are influenced by having a family member with breast cancer | Descriptive and prospective cross-sectional study | 88 family caregivers consisted of 29 (33%) men and 59 (67%) women with mean (SD) 41.1 (13.9). | A majority of family caregivers reported a high psychological impact described as experiences of shock and stress, feeling sadness and depressed, fear and anxiety, and having disturbed sleep. Furthermore, family caregivers stated other aspects which may have a negative impact on mental and emotional well-being but not covered, namely, descriptions of fear of recurrence, uncertainty of outcome, and worry about future and death. Many family caregivers reported a change in their relationship with their sick relative and that the disease tended to amplify existing problems. Religious aspects such as feeling a stronger connection to God as well as optimism and hope were expressed to be enhanced for some of the family caregivers | Family caregivers need support in dealing with the psychological strain related to the situation by acquiring information about cancer and its treatment and in how to communicate about their own concerns with their relative with cancer. Moreover, education and interventions from health care professionals would be beneficial in improving QoL for the families of patients | Sample size of the family caregivers is a limitation to the study. The use of semi-structured interviews may not be as adequate to capture a phenomenon as more in-depth interviews |
| Kusi et al. (2020) [4] | Ghana | To explore the caregiving motivations and experiences of family caregivers of patients living with advanced breast cancer | Exploratory descriptive phenomenological approach | 15 caregivers. 7 were males while 8 were females with age range from 25 to 73 years. | Caregivers were involved in bathing, grooming, and cooking for patients. Their experiences further include symptom management such as the management of pain, lymphedema, wound, and evaluation of symptoms. Caregivers were the main providers of emotional support by offering patients with words of encouragement. They also experience financial burden by providing out-of-pocket money for treatment costs and other related non-medical costs | There is the need for home-based support programs to assist caregivers in their caring role especially in the area of symptom management and direct governmental social intervention programs (e.g., transportation to treatment facilities and drugs for patients) to resource-limited caregiving families of women with advanced breast cancer. The National Health Insurance Scheme should be expanded to fully cover breast cancer treatment to women and their family caregivers | The findings cannot be generalized based on the sample selection (caregivers of only advanced breast cancer patients). The study was limited to a single site |
Results
Literature search results
Only articles that had reported on family caregivers of breast cancer patients in low- and middle-income countries were included. The initial search returned 1781 records. A total of 430 duplicates were removed using the Mendeley Desktop (version 1.19.4). The remaining 1351 records were screened for titles and abstracts by the two independent reviewers (GK and KBM). We then excluded 1225 articles, and a full-text screening was done on the remaining 126 articles. Following the full-text screening, 107 were excluded because they did not meet the inclusion criteria as detailed in the PRISMA flow diagram. At the end of the screening procedure, 19 peer-reviewed citations remained for final inclusion in the review [3, 4, 6, 10, 15, 17–19, 23–33].
A schema illustrating the screening process is shown in Fig. 1.
Fig. 1.
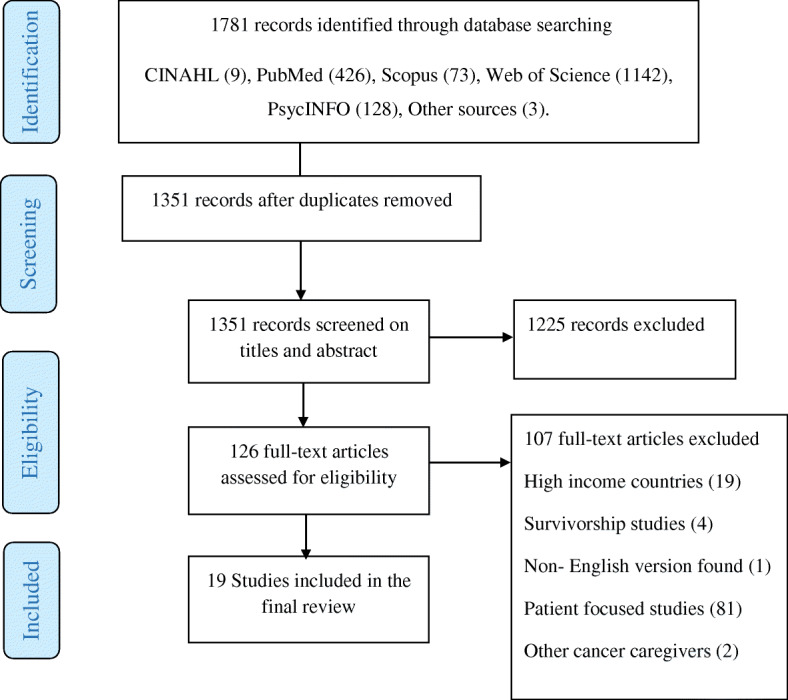
PRISMA flow diagram showing the systematic screening process
Methodological characteristics of included studies
The majority of the included studies (n = 15) used quantitative approaches [3, 10, 15, 18, 19, 23–28, 30–33] and the remaining (n = 4) were qualitative studies [4, 6, 17, 29]. Studies were conducted in the following countries: Nigeria (n = 2), Malaysia (n = 3), Ghana (n = 1), China (n = 3), Iran (n = 6), Turkey (n = 1), Mexico (n = 1), Indonesia (n = 1), and India (n = 1).
A total of 2330 family caregivers were included in the studies. The sample sizes within the included studies ranged from 7 caregivers [17, 29] to 384 caregivers [26]. The disease severity of the patients being cared for by the caregivers was only stated in 10 studies [4, 15, 24, 26, 28–32, 34].
Table 1 shows the summary of the included studies on caregivers’ experiences of women diagnosed with breast cancer.
Quality appraisal or assessment of included studies
Quality appraisal of the included works of literature using MMAT ranged from moderate (50%) to strong quality (100%). Two studies were rated as strong quality [4, 6]. Fifteen studies were scored as moderate-strong quality [15, 18, 19, 23–33, 35], and the remaining two studies [3, 17] were scored as moderate. None of the included studies was excluded based on their quality assessment score. The level of agreement of quality ratings between the two independent raters ranged from strong [kappa 0.79; 95% (0.4–1.2); p = 0.001] to excellent agreement [kappa 1.0; 95% (0.9–1.0); p =0.001]. Table 2 shows the quality assessment of the included studies.
Table 2.
Quality appraisal of included papers and their Mixed Methods Appraisal Tool (MMAT) score
| Qualitative | Quantitative | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Author, year | Sources relevant to address research question | Analysis Process relevant to address research question | Findings adequately derived from data | Interpretation of results sufficiently substantiated by data | Sampling strategy reduce selection bias | Measuring appropriate for intervention /outcome | Sample representativeness | Acceptable response rate | Total points | Score | Quality |
| Vahidi et al. (2016) [3] | 0 | 0 | 1 | 1 | (2/4) | 50 | Moderate | ||||
| Gabriel, Aluko, and Okeme (2019) [15] | 0 | 1 | 1 | 1 | (3/4) | 75 | Moderate-strong | ||||
| Zhu et al. (2014) [31] | 0 | 1 | 1 | 1 | (3/4) | 75 | Moderate-strong | ||||
| Sahadevan et al. (2019) [26] | 0 | 1 | 1 | 1 | (3/4) | 75 | Moderate-strong | ||||
| Jaafar et al. (2014) [24] | 0 | 1 | 1 | 1 | (3/4) | 75 | Moderate-strong | ||||
| Gabriel and Mayers. (2019) [27] | 0 | 1 | 1 | 1 | (3/4) | 75 | Moderate -strong | ||||
| Giray and Akyuz (2019) [28] | 0 | 1 | 1 | 1 | (3/4) | 75 | Moderate-strong | ||||
| Moreno-Gonzalez et al. (2019) [29] | 0 | 1 | 1 | 1 | (3/4) | 75 | Moderate-strong | ||||
| Hashemi-Ghasemabadi et al. (2016) [6] | 1 | 1 | 1 | 1 | (4/4) | 100 | Strong | ||||
| Mahadevan et al. (2013) [32] | 0 | 1 | 1 | 1 | (3/4) | 75 | Moderate-strong | ||||
| Bahrami and Farzi (2014) [18] | 1 | 1 | 0 | 1 | (3/4) | 75 | Moderate-strong | ||||
| Wulandari et al. (2017) | 0 | 1 | 0 | 1 | (2/4) | 50 | Moderate | ||||
| Yeung et al. (2018) [30] | 0 | 1 | 1 | 1 | (3/4) | 75 | Moderate-strong | ||||
| Heidari Gorji et al. (2012) | 0 | 1 | 1 | 1 | (3/4) | 75 | Moderate-strong | ||||
| Yuanyuan An et al. (2019) | 0 | 1 | 1 | 1 | (3/4) | 75 | Moderate-strong | ||||
| Nejad et al. (2016) | 1 | 1 | 0 | 1 | (3/4) | 75 | Moderate-strong | ||||
| Din et al. (2017) [25] | 0 | 1 | 1 | 1 | (3/4) | 75 | Moderate-strong | ||||
| Khanjari et al. (2014) [35] | 0 | 1 | 1 | 1 | (3/4) | 75 | Moderate-strong | ||||
| Kusi et al. (2020) [4] | 1 | 1 | 1 | 1 | (4/4) | 100 | Strong | ||||
|
k; 0.9 (0.6–1.2) p < 0.05 |
k; 0.8 (0.5–1.1) p < 0.001 |
k; 1.0 (0.9–1.0) p = 0.001 |
k; 0.9 (0.7–1.1) p < 0.05 |
k; 0.79 (0.4–1.2) p < 0.001 |
k; 1.0 (0.9–1.0) p < 0.001 |
k; 1.0 (0.9–1.0) p < 0.001 |
k; 0.8 (0.4–1.2) p = 0.001 |
||||
Indicators: 0 criteria not met, 1 criteria met. Scale 1, 25% (one criterion met); scale 2, 50% (two criteria met); scale 3, 75% (three criteria met); scale 4, 100% (all criteria met)
k; Cohen’s kappa coefficient, 95% CI; 95% Confidence Interval, p; p-value
Findings on the caregivers’ experiences
The synthesis of the included articles showed that caregivers’ experiences fell into 10 main categories, namely, (1) caregivers’ motivation, (2) roles of family caregivers, (3) quality of life among caregivers, (4) physical burden of caregiving, (5) psychological burden of caregiving, (6) disruption in social life, (7) economic burden of caregiving, (8) need for support, (9) interventions for improving caregiver experience, and lastly (10) coping. These findings are described in the ensuing paragraphs.
Caregivers’ motivation
Three studies focused on the caregivers’ motivation for delivering care to women with breast cancer [4, 6, 30]. In the first study, caregivers cited a sense of responsibility and commitment as forms of motivation for their caregiving roles [6]. One Ghanaian study reported that family and sociocultural obligations prompted family members, especially females, to assume the caregiving role for women with breast cancer [4]. However, two studies conducted in Ghana [4] and China [30] reported that family-oriented cultural norms also prompted males such as spouse caregivers to assume the role of primary caregivers.
Roles of family caregivers
Four studies emphasized the role of caregivers in the management of breast cancer [3, 4, 26, 29]. Vahidi et al. [3] and Kusi et al. [4] suggested that caregivers played key roles in assisting patients with activities of daily living and the administration of medications. The studies also showed that caregivers played roles in assisting with treatment decision-making and symptom management [3, 4, 26, 29]. Moreno-González et al. [29] and Kusi et al. [4] also emphasized that caregivers managed specific symptoms such as breast wound and lymphedema, evaluation of symptoms, and management of pain. One study also reported that caregivers were the primary source of psychosocial, spiritual, and financial support for women with breast cancer [4].
Quality of life among caregivers
Seven articles gave an account of the quality of life of caregivers. The reports indicated that caregivers of women diagnosed with breast cancer had low levels of quality of life as compared to the general healthy population [3, 15, 23, 26, 28, 31, 33]. One study reported that the patient correlates of poor quality of life among family caregivers were advanced-stage breast cancer, poor functional status, frequent hospitalization, longer duration of breast cancer [15], lack of transportation [3], and high symptom burdens such as wound [31] and postmastectomy lymphedema [28]. Further, An et al. [23] also cited that higher levels of anxiety and depression were associated with poor quality of life among caregivers. Lastly, three studies highlighted that lack of formal support services that characterized developing countries also resulted in poor quality of life among caregivers [3, 10, 33].
Physical burden of caregiving
Four studies emphasized that caregivers reported a moderate to severe decline in physical health [6, 10, 17, 31]. Altered sleep patterns and hypertension were the frequently reported physical symptoms experienced by the caregivers [6, 10, 17]. Zhu et al. also highlighted that low family income and increasing age are predictors of physical burden among caregivers [31].
Psychological burden of caregiving
The majority of the included studies reported that psychological burden was the most frequent stressor that caregivers encountered [6, 10, 17, 25–27, 29–33]. According to Khanjari et al. [10], more than 70% of family caregivers experienced severe psychological impacts 6 months following breast cancer diagnosis and the assumption of the caregiving role. These studies also identified some conditions described as psychological burdens among the caregivers. Six studies cited depression as a common psychological burden among caregivers [10, 24, 30–33]. Studies cited that factors such as age [32], male gender, altered sleeping pattern [10, 17, 30, 31], longer duration of caregiving [24, 26, 32], lower educational level, not sharing caregiving responsibilities [32], and decreased functional status of patients [24, 32] were significantly associated with stressors such as depression among caregivers. Additionally, anxiety had also been identified as a common psychological distress that is experienced by caregivers [17, 25]. According to Din et al., about one third of caregivers suffered from anxiety-related disorders [25]. Furthermore, Din et al. [25] reported that longer caregiving duration and absence of shared caregiving were significantly associated with anxiety disorders. Moreover, four of the included studies reported that anxiety among caregivers was caused by the uncertainties of breast cancer outcomes, fear of recurrence, and poor financial supports available to caregivers [10, 17, 25, 26, 29]. Several emotional traumas such as fear, shock, anger, and sadness were also cited by caregivers in three studies [6, 26, 29].
Disruption in social life
Hashemi-Ghasemabadi et al. [6] reported that caregivers experienced a loss of normal life. This study also reported that caregivers experienced deteriorating relationships with other family members. Some caregivers cited that they felt isolated and lacked support from family and friends, which increased the burden associated with their caregiving roles [6].
Economic burden of caregiving
Eight papers examined the economic burden associated with caregiving around breast cancer [3, 6, 10, 15, 17, 24, 27, 29]. Two studies reported that caregivers usually decreased their working hours or lost paid jobs as a result of the caregiving role [17, 24]. It was also reported that even in conditions where caregivers still engaged in paid jobs, high treatment costs coupled with the absence of fully financed healthcare system that exists in LMICs created a high economic burden for family caregivers [15, 17, 24, 27, 29]. The synthesized findings also showed that lack of basic financial resources [15, 29] and inadequate income for meeting caregiving demands [3, 6, 10, 27] also resulted in financial burden for caregivers. Further, Gabriel and Mayers [27] suggested that given the extreme financial burden that is faced by caregivers in developing countries, educational interventions might be ineffective in improving the financial well-being among caregivers.
The need for support
The need for social support was the most frequent need that was cited by the caregivers across six included studies [6, 17, 25, 29–31]. Caregivers cited that they had not received adequate social support from their families and friends [17, 25, 31]. Specifically, caregivers described the need for sharing caregiving responsibilities with other family members and friends [6, 25, 30, 31].
Nonetheless, Yeung et al. [30] and Vahidi et al. [3] reported that seeking support from families and friends among spouse caregivers may result in increased emotional distress as it may be culturally interpreted as a sign of weakness and lack of self-confidence. Further, in three studies, caregivers also stressed the importance of support from the formal care systems to help them manage patients’ symptoms in the home setting [6, 17, 29].
Interventions for improving the caregiver’s experience
Three articles examined interventions to support family caregivers [18, 19, 27]. Largely, all the studies reported significant improvement in the quality of life after psycho-educational intervention. Particularly, the improvements in caregivers’ quality of life were related to measures such as the emotional aspect of caregiving. In the first study [27], it was reported that caregivers were given psycho-educational interventions to improve their quality of life. Caregivers in the interventional group received 6 weeks of information about adjustment to the role of family caregivers and strategies to deal with the emotional aspects of caregiving. This quasi-experimental study reported that caregivers in the interventional group reported better quality of life after the 6 weeks [27]. It was reported that the provision of informational support aided in decreasing caregiving burden among the caregivers. However, the intervention did not affect the financial well-being of caregivers.
The second education intervention study [18] examined the effect of a supportive educational program on the caring burden and quality of life of family caregivers. The intervention group in this study reported a clear increase in caregivers’ knowledge about breast cancer management, physical, psychological, spiritual, and environmental dimensions of health. Lastly, the third study [19] evaluated the effect of an educational and telephone follow-up on caregiver burden. Results from this showed that caregiver burden decreased significantly among the intervention group.
Coping
Three of the included studies reported on coping strategies used by family caregivers [10, 17, 29]. These studies reported that religious coping such as putting one’s faith in God was vital in improving the quality of life among caregivers [10, 17, 29]. Two of the studies further reported that caregivers reported that being religious provided them with meaning in their caregiving roles [10, 17]. Further, one study also showed that previous knowledge on breast cancer aided caregivers to cope effectively in their caring role [29].
Discussion
In this systematic review, key evidence on family caregivers of women diagnosed with breast cancer in LMICs has been highlighted. Reviews focusing on caregivers of women with breast cancer in LMICs are missing in the literature. The current systematic review, therefore, addressed this gap by adding to the knowledge in this area.
The current review demonstrated that family members, including male spouses, assumed the caregiving role for women diagnosed with breast cancer. Based on this finding, future research using comparative study designs should be conducted to examine how breast cancer caregiving differs among male and female caregivers. This systematic review further highlighted the roles that are played by family caregivers in providing physical, spiritual, emotional, and financial support to women with breast cancer in LMICs [3, 4]. Furthermore, studies in this review highlighted the significant role played by caregivers in symptom management [3, 4, 26]. Despite this important finding, only one of the included studies [4] provided information on how symptoms such as pain, lymphedema, and breast wound are managed in the home by the caregivers. The level of empirical evidence addressing how family caregivers manage symptoms in LMICs where there is evidence of limited formal support structures needs further exploration using qualitative methods.
The review identified a range of burdens that are encountered by caregivers. Caregivers reported challenges such as fear, depression, and hypertension [6, 25, 31]. Financial challenges such as lack of transportation, loss of a paid job, and high treatment cost were also fundamental sources of stress for caregivers across several studies in this review [3, 26, 27, 29]. This finding is expected, considering the financial burden that such caregiver roles put on families. This is because these caregivers are already overburdened by the lack of formal support services and poor economic status in LMICs. Therefore, these identified challenges encountered by the caregivers in LMICs in their caregiving roles represent areas in the caregivers’ lives that need to be addressed in policy formulation.
Also, it was reported that disease severity and declining functional status impacted the quality of life of the caregivers [3, 15, 26, 31]. As such, how the caregivers’ challenges change according to the progression of breast cancer is an important topic for further exploration in future longitudinal studies.
The findings of this review also showed that educational and psychological interventions could prove as relevant tools in improving the wellbeing of family caregivers [18, 19, 27]. Accordingly, it would be important for future study to focus on the development of educational and supportive interventions for family caregivers to help address their challenges.
One of the most striking gaps observed in this systematic review is the lack of qualitative studies on the caregivers of women with breast cancer in LMICs. Only four studies explored the experiences and challenges that were faced by the caregivers in their caregiving roles using qualitative designs [4, 6, 17, 29]. This finding therefore offers opportunity for further qualitative works into breast cancer caregiving in LMICs. This method of enquiry will produce a rich, detailed, and rigorous data on the phenomenon by allowing participants to naturally share their lived experiences in their setting.
Lastly, there are a few studies that explored other aspects of caregiver wellbeing such as disruption in social life, coping measures, and intervention for caregivers [6]. Therefore, a need exists to focus future studies on these areas of the caregiver wellbeing.
Strengths and limitations
Some limitations of this systematic review are worth noting. First, this review found a relatively small number of relevant studies. With a publication period from January 2000 to March 2020, only 19 studies that had reported on family caregivers of breast cancer patients were identified and synthesized. This may hinder the generalizability of the research findings. However, with expanded attention to breast cancer caregivers in LMICs, this review can drive future research and also inform policy. Further limitation is language restriction. Non-English language articles were excluded due to the limited capacity to access professional language services. This is challenging since family caregiving in breast cancer is socio-cultural and context-specific. Excluding articles in non-English languages may have resulted in a limited understanding of the phenomenon under review and therefore poses a risk of bias in extrapolating the results to a broader population. Further, not considering studies that had been published in the developed countries might have resulted in the exclusion of relevant studies.
In addition, it was not feasible to synthesize the results in a meta-analysis as the included studies were clearly heterogenous. For instance, the included studies used different methods such as correlational studies, cross-sectional designs, and self-reported data to obtain caregivers’ reported experiences. It was however decided a priori to include all studies regardless of their study design as the aim of this study was to investigate the diversity of studies reporting on caregivers of women living with breast cancer in LMICs, thus obtaining a broad perspective of the phenomenon under review.
The strength of this systematic review includes the use of an MMAT tool for the quality appraisal by two independent reviewers. Also, we are the first to systematically map evidence and report on the experiences of family caregivers of breast cancer patients in low- and middle-income countries.
Conclusions
The incidence of breast cancer is increasing in LMICs. This has serious implications for family caregivers. The burden associated with the caregiving role is further amplified by limited availability and access to palliative services and formal structures to support caregivers in their caring roles. Also, due to factors such as financial constraints, there may be a lack of social protection policies for breast cancer caregivers. The high psychological and financial burdens associated with caregiving in developing countries create the need to raise awareness about the neglected needs of family caregivers.
Enhanced support for caregivers should be highlighted as a priority in LMICs. There are numerous gaps in policy and education about caregivers that need to be addressed. The available evidence in this review does not comprehensively address how caregiver challenges can be reduced. Therefore, further research is needed to generate empirical data to inform an evidence-based approach to addressing family caregivers’ challenges in LMICs.
Contribution of the paper
What is known about this topic?
Breast cancer is a common malignancy among women in LMICs.
There is a transition of breast cancer treatment from the in-patient setting to the out-patient setting.
What this paper adds:
Evidence on family caregivers of breast cancer patients in LMICs.
Identify the limited evidence and the existing gaps in research related to breast cancer caregiving that urgently needs to be addressed.
Family caregivers play a key role in providing home care for breast cancer patients in LMICs.
Family caregivers experience challenges in their caregiving role.
Supplementary information
Additional file 1: Table S1. Search strategy.
Acknowledgments
None.
Abbreviations
- LMICs
Low-and middle-income countries
- MMAT
Mixed Methods Appraisal Tool
Authors’ contributions
GK: conceptualization, design, literature search, review/screening of articles, drafting of the original manuscript, review, editing, and approval of the manuscript for publication. ABBM: conceptualization, design, supervision, literature search, review/screening of articles, drafting of the original manuscript, review, editing, and approval of the manuscript for publication. KBM: literature search, review/screening of articles, review, editing, and approval of the manuscript for publication. All other authors: review, editing, and approval of the manuscript for publication.
Funding
The authors have no funding support for this study.
Availability of data and materials
All data generated or analyzed during this study are included in this published article (and its supplementary information files). The data can be accessed at figshare data repository through 10.6084/m9.figshare.12089205.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Grace Kusi, Email: gracekusi816@yahoo.com.
Adwoa Bemah Boamah Mensah, Email: bbemahc2000@gmail.com.
Kofi Boamah Mensah, Email: kofimensah227@yahoo.co.uk.
Veronica Millicent Dzomeku, Email: vmdzomeku@gmail.com.
Felix Apiribu, Email: fapiribu@yahoo.com.
Precious Adade Duodu, Email: padadeduodu@yahoo.com.
Bakinam Adamu, Email: mathewbakinam@yahoo.com.
Pascal Agbadi, Email: pascalagbadi@gmail.com.
Kwadwo Osei Bonsu, Email: kbonsu2880@gmail.com.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13643-020-01408-4.
References
- 1.Shafaie FS, Mirghafourvand M, Amirzehni J. Predictors of quality of life in patients with breast cancer. Indian J Palliat Care. 2019;25:73. doi: 10.4103/IJPC.IJPC_119_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rivera-Franco MM, Leon-Rodriguez E. Delays in breast cancer detection and treatment in developing countries. Breast Cancer Basic Clin Res. 2018;12:117822341775267. doi: 10.1177/1178223417752677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vahidi M, Mahdavi N, Asghari E, Ebrahimi H, Ziaei JE, Hosseinzadeh M, et al. Other side of breast cancer: factors associated with caregiver burden. Asian Nurs Res (Korean Soc Nurs Sci). 2016;10:201–6. 10.1016/j.anr.2016.06.002. [DOI] [PubMed]
- 4.Kusi G, Boamah Mensah AB, Boamah Mensah K, Dzomeku VM, Apiribu F, Duodu PA. Caregiving motivations and experiences among family caregivers of patients living with advanced breast cancer in Ghana. PLoS One. 2020;15:e0229683. doi: 10.1371/journal.pone.0229683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zelle S, Nyarko K, Bosu W, Aikins M, Niëns L, Lauer J, et al. Costs, effects and cost-effectiveness of breast cancer control in Ghana. Trop Med Int Heal. 2012;17:1031–1043. doi: 10.1111/j.1365-3156.2012.03021.x. [DOI] [PubMed] [Google Scholar]
- 6.Hashemi-Ghasemabadi M, Taleghani F, Yousefy A, Kohan S. Transition to the new role of caregiving for families of patients with breast cancer: a qualitative descriptive exploratory study. Support Care Cancer. 2016; 24:1269–76. 10.1007/s00520-015-2906-3. [DOI] [PubMed]
- 7.Muliira JK, Kizza IB, Nakitende G. Roles of family caregivers and perceived burden when caring for hospitalized adult cancer patients: perspective from a low-income country. Cancer Nurs. 2019;42:208–217. doi: 10.1097/NCC.0000000000000591. [DOI] [PubMed] [Google Scholar]
- 8.Alexander A, Kaluve R, Prabhu J, Korlimarla A, Srinath B, Manjunath S, et al. The impact of breast cancer on the patient and the family in Indian perspective. Indian J Palliat Care. 2019;25:66–72. doi: 10.4103/IJPC.IJPC_158_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ozaki A, Tsubokura M, Leppold C, Sawano T, Tsukada M, Nemoto T, et al. The importance of family caregiving to achieving palliative care at home: a case report of end-of-life breast cancer in an area struck by the 2011 Fukushima nuclear crisis: a case report. Medicine (Baltimore) 2017;96:e8721. doi: 10.1097/MD.0000000000008721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khanjari S, Langius-Eklöf A, Oskouie F, Sundberg K. Family caregivers of women with breast cancer in Iran report high psychological impact six months after diagnosis. Eur J Oncol Nurs. 2014. [DOI] [PubMed]
- 11.Chronopoulou K, Sakkas D, Damigos D. Caregiving burden and psychological distress of breast cancer patients’ husbands after mastectomy. Int J Caring Sci. 2016;9:909–913. [Google Scholar]
- 12.Fekih-Romdhane F, Henchiri H, Ridha R, Labbane R, Cheour M. Level of psychological distress and perceived distress and perceived burden among spouses of women with breast cancer. Encephalon. 2019;45:190-2. 10.1016/j.encep.2018.09.003. [DOI] [PubMed]
- 13.Holst-Hansson A, Idvall E, Bolmsjo I, Wennick A. Hoping to reach a safe haven—Swedish families’ lived experiences when a family member is diagnosed with breast cncer. Eur J Oncol Nurs. 2017;31:52–58. doi: 10.1016/j.ejon.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Cheng T, Jackman M, Mcquestion M, Fitch M. ‘Knowledge is power’: perceived needs and preferred services of male partners of women newly diagnosed with breast cancer. 2014. p. 474. [DOI] [PubMed] [Google Scholar]
- 15.Gabriel I, Aluko J, Okeme M. Caregiver burden among informal caregivers of women with breast cancer. Biomed J Sci Tech. 2019;15:1–9. 10.26717/BJSTR.2019.15.002704.
- 16.World Bank Groupplu. World Bank Country and Lending Groups. The World Bank. http://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed 15 Mar 2020.
- 17.Wulandari SK, Hermayanti Y, Yamin A, Efendi F, Padjadjaran U, Airlangga U. Family process with breast cancer patient (Sarah Kartika Wulandari et al.). 2015;:180–8. http://eprints.ners.unair.ac.id/494/1/breast cancer.pdf.
- 18.Bahrami M, Farzi S. The effect of a supportive educational program based on COPE model on caring burden and quality of life in family caregivers of women with breast cancer. Iran J Nurs Midwifery Res 2014;19:119–126. http://www.ncbi.nlm.nih.gov/pubmed/24834079%0A, http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4020019. Accessed 7 Dec 2019. [PMC free article] [PubMed]
- 19.Kochaki Nejad Z, Aghdam AM, Hassankhani H, Sanaat Z. The effects of a patient-caregiver education and follow-up program on the breast cancer caregiver strain index. Iran Red Crescent Med J. 2016;18:e21627. doi: 10.5812/ircmj.21627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pluye P, Gagnon MP, Griffiths F, Johnson-Lafleur J. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in mixed studies reviews. Int J Nurs Stud. 2009;46:529–546. doi: 10.1016/j.ijnurstu.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 21.Pace R, Pluye P, Bartlett G, Macaulay A, Salsberg J, Jagosh J, et al. Testing the reliability and efficiency of the pilot mixed methods appraisal tool (MMAT) for systematic mixed studies review. Int J Nurs Stud. 2012;49:47–53. doi: 10.1016/j.ijnurstu.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 22.McHugh ML. Lessons in biostatistics interrater reliability: the kappa statistic. Biochem Medica. 2012;22:276–82 https://hrcak.srce.hr/89395. Accessed 18 Nov 2019. [PMC free article] [PubMed]
- 23.An Y, Fu G, Yuan G. Quality of life in patients with breast cancer: the influence of family caregiver’s burden and the mediation of patient’s anxiety and depression. J Nerv Ment Dis. 2019;207:921–926. doi: 10.1097/NMD.0000000000001040. [DOI] [PubMed] [Google Scholar]
- 24.Jaafar NRN, Din SHS, Zakaria H, Saini SM, Ahmad SNA, Midin M, et al. Clinical depression while caring for loved ones with breast cancer. Compr Psychiatry 2014;55:S52–S59. 10.1016/j.comppsych.2013.03.003. [DOI] [PubMed]
- 25.Din SHS, Jaafar NRN, Zakaria H, Saini SM, Ahmad SNA, Midin M. Anxiety disorders in family caregivers of breast cancer patients receiving oncologic treatment in Malaysia. 2017;18:465–71. 10.22034/APJCP.2017.18.2.465. [DOI] [PMC free article] [PubMed]
- 26.Sahadevan S, Namboodiri V. Depression in caregivers of patients with breast cancer. Indian J Psychiatry. 2019;61:277. doi: 10.4103/psychiatry.IndianJPsychiatry_46_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gabriel I, Mayers P. Effects of a psychosocial intervention on the quality of life of primary caregivers of women with breast cancer. Eur J Oncol Nurs. 2019;38:85–91. 10.1016/j.ejon.2018.12.003. [DOI] [PubMed]
- 28.Giray E, Akyuz G. Assessment of family caregiver burden and its relationships between quality of life, arm disability, grip strength, and lymphedema symptoms in women with postmastectomy lymphedema: a prospective cross-sectional study. Eur J Breast Heal. 2019;15:111–118. doi: 10.5152/ejbh.2019.4385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moreno-González MM, Galarza-Tejada DM, Tejada-Tayabas LM. Experiencias del cuidado familiar durante el cáncer de mama: la perspectiva de los cuidadores. Rev Esc Enferm USP. 2019;53:e03466. doi: 10.1590/s1980-220x2018012203466. [DOI] [PubMed] [Google Scholar]
- 30.Yeung N, Zhang Y, Ji Y, Lu G, Lu Q. Guilt among husaband caregivers of Chinese women with breast cancer: the roles of male gender-role norm, caregiving burden and coping processes. Eur J Cancer Care (Engl) 2018;27:e12872. doi: 10.1111/ecc.12872. [DOI] [PubMed] [Google Scholar]
- 31.Zhu P, Fu J, Wang B, Lin J, Wang Y, Fang N, et al. Quality of life of male spouse caregivers for breast cancer patients in China. 2014;15:4181–5. 10.7314/APJCP.2014.15.10.4181. [DOI] [PubMed]
- 32.Mahadevan R, Jaafaraafar NRN, Din SHS, Ahmad SNA, Baharuddin A, Razali R. The stress of caregiving: a study of family caregivers of breast cancer patients receiving oncologic treatment at a Malaysian general hospital. Sains Malaysiana. 2013;42:1019–1026. [Google Scholar]
- 33.Ali M, Gorji H, Bouzar Z, Haghshenas M, Kasaeeyan AA. Quality of life and depression in caregivers of patients with breast cancer. ? 2012;5:1. 10.1186/1756-0500-5-310. [DOI] [PMC free article] [PubMed]
- 34.Laryea DO, Awuah B, Amoako YA, Osei-Bonsu E, Dogbe J, Larsen-Reindorf R, et al. Cancer incidence in Ghana, 2012: evidence from a population-based cancer registry. BMC Cancer. 2014;14:382. doi: 10.1186/1471-2407-14-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khanjari S, Langius-Eklöf A, Oskouie F, Sundberg K. Family caregivers of women with breast cancer in Iran report high psychological impact six months after diagnosis. Eur J Oncol Nursing. 2014;18:630–635. doi: 10.1016/j.ejon.2014.06.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Search strategy.
Data Availability Statement
All data generated or analyzed during this study are included in this published article (and its supplementary information files). The data can be accessed at figshare data repository through 10.6084/m9.figshare.12089205.


