Summary
Background
Sunbed use increases the risk of skin cancer. The Danish sunbed legislation (2014) did not include an age limit.
Aim
To model skin cancer incidences and saved costs from potential effects of structural interventions on prevalence of sunbed use.
Materials and Methods
Survey data from 2015 were collected for 3999 Danes, representative for the Danish population in regards to age, gender and region. Skin cancer incidences were modelled in the Prevent program, using population projections, historic cancer incidence, sunbed use exposure and relative risk of sunbed use on melanoma.
Results
If structural interventions like an age limit of 18 years for sunbed use or complete ban had been included in the Danish sunbed legislation in 2014, it would have reduced the annual number of skin cancer cases with 455 or 4177, respectively, while for the entire period, 2014‐2045 the total reductions would be 3730 or 81 887 fewer cases, respectively. The cost savings from an age limit or ban, respectively, are 9 and 129 millions € during 2014‐2045.
Conclusion
Legislative restrictive measures which could reduce the sunbed use exists. Danish politicians have the opportunity, supported by the population, to reduce the skin cancer incidence and thereby to reduce the future costs of skin cancer.
Keywords: Campaign, melanoma projections, prevention, questionnaire, skin cancer, ultraviolet radiation
1. INTRODUCTION
Exposure to ultraviolet radiation (UVR) is the main risk factor for keratinocyte (SCC and BCC) and cutaneous melanoma (CM) skin cancers.1, 2 Intermittent exposure to UVR from the sun and sunbeds are important factors in the aetiology of skin cancer3, 4. In Denmark, the CM incidence (world standardized rate per 100 000) for men and women increased more than 10‐fold since the 1950s to 21.4 and 26.7 in 2010–2014, respectively.5 Similarly, the basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) incidences for men and women have increased manifold to 103.0 and 104.3 (BCC) and 17.5 and 13.9 (SCC) in 2010–2014, respectively.5 The increase is presumably a consequence of the increased attention from primary prevention campaigns and improved secondary prevention, improved diagnostics6, 7 and change in sun exposure patterns including increased travelling since the 1960s and introduction and spread of sunbed facilities in the 1980s. Half of the Danish population travel to sunny destinations each year,8, 9 approximately 60% have ever used a sunbed10 and 40% were sunburnt annually.8, 11
In 2009, the International Agency for Research on Cancer classified ultraviolet‐emitting tanning devices as ‘carcinogenic to humans’ with respect to CM.4, 12, 13, 14, 15, 16 The increased risk of CM was shown to be especially high among sunbed users younger than 30‐35 years, where more than 3 out of 4 CM cases diagnosed at this young age was caused by sunbed use. Increased risk of CM from sunbeds was shown even without the presence of sunburn.13, 15 Boniol et al17 summarized the risk of CM from sunbed use in a systematic review to be 1.2 for ever‐use and 1.59 for use initiated before the age of 35. Additionally, a dose‐response relationship was established between frequency of sunbed use and CM with an increased risk of 2% for each extra annual session. The increased risk, from sunbed use, of developing BCC and SCC was summarized by Wehner et al18 to 1.29 and 1.67, respectively. Sunbed use is highly prevalent in Denmark, especially in younger age groups and more than half of those recalling their age of initiation of sunbed use, reported to start before age 18 years.19, 20 Sunbed use was estimated to be responsible for 13% and 8% of CM cases in Denmark in women and men, respectively.17
1.1. Legislation of sunbed use
In 2007, the Danish Sun Safety Campaign was launched and the prevalence of sunbed use was significantly reduced afterwards10, 21; however, more than 1 in 10 Danes still used sunbeds in 2015.22 Concurrently with campaign activities, the campaign lobbied for regulation of commercial sunbed business, including age limits and staff requirements for sunbed studios. Together with other stakeholders like consumer councils, children organizations and a long range of health professional organizations, the effects of the campaign lead to the initiation of a national sunbed legislation, which was adopted and took effect from August 2014.23 The legislation contained similar elements as European technical standard 60 33524 in terms of emission of UV radiation. However, while Danish politicians were advised by a unanimous group of health professionals, children advocates, consumer councils, etc. (except sunbed industry‐related), to include an age limit for sunbed use in the legislation, it was not included in the final legislation.25, 26
The aim of this study was to show the potential effects on (a) future skin cancer incidence and (b) cost savings if the Danish sunbed legislation had included an 18‐year age limit on sunbed use as well as an introduction of a complete sunbed ban.
2. MATERIALS AND METHODS
2.1. Overview
We estimated the hypothetical effect of the Danish sunbed legislation in two scenarios: age limit and Ban if introduced in 2014. We modelled projections of future cancer incidence, introducing the effects of the legislation and compared with status quo using realistic estimates of relative risks in the intervention scenarios to obtain an indication of the long‐term impact of the legislation interventions on cancer incidence.
2.2. Estimation of prevalence of sunbed use
In 2015, a question on frequency of sunbed use was included in the annual population‐based questionnaire on exposure to UV radiation and behaviour and attitude towards UV exposure.22 In total, 3999 Danes answered the questionnaire. Data were collected by computer‐assisted web interview (CAWI) by Epinion. Data were representative for the Danish population by gender, age, region and education (Table 1). Detailed data sampling strategies are available in the annual survey report on skrunedforsolen.dk.
Table 1.
Distribution of demographic characteristics and percentage of sunbed use in cross‐sectional survey on UV exposure in 2015 in 3999 Danes
| Characteristic (%) | Total n (%) | % ever‐used sunbed |
|---|---|---|
| Total (n) | 3999 (100) | |
| Gender | P < 0.001 | |
| Male | 2013 (50) | 35 |
| Female | 1986 (50) | 58 |
| Age group | P < 0.001 | |
| 15‐19 | 385 (10) | 22 |
| 20‐29 | 798 (20) | 44 |
| 30‐39 | 738 (18) | 62 |
| 40‐49 | 881 (22) | 60 |
| 50‐59 | 732 (18) | 40 |
| 60‐64 | 465 (12) | 33 |
| Region | 0.487 | |
| Capital | 1290 (32) | 47 |
| Zealand | 562 (14) | 43 |
| Northern Jutland | 406 (10) | 51 |
| Central Jutland | 906 (23) | 45 |
| Southern Denmark | 835 (21) | 47 |
| Education | 0.017 | |
| <10 y | 975 (24) | 41 |
| 10‐12 y | 1670 (42) | 47 |
| >12 y | 1290 (32) | 50 |
P‐values are for chi‐square test observed vs. expected levels of ever‐used sunbed.
Values are percentage.
Exposure to artificial UVR was determined by the question: (“How often did you use a sunbed within the past 12 months?” “More than once a week, Once a week, More than once a month, Once a month, Fewer than four times a year, Not within the past twelve months, Never”); answers to sunbed use were grouped into “ever‐users” (all categories except “never”) and “never‐users”.
2.3. The prevent model
Projection of future incidence was estimated using Prevent.27, 28 This program was adapted for the Eurocadet project to model future cancer incidence by implementation of lifestyle preventive strategies. Prevent calculated the percentages of potentially prevented cases under the scenario of interest as compared to the status quo scenario. If the scenario of interest is no exposure or exposure with minimum impact on risk, this percentage is interpretable as the population attributable fraction (PAF) of sunbed use experience, respectively, on skin cancer (CM, SCC and BCC) incidences by the year 2040: they represent the numbers of cases that would be prevented had the population not used sunbed and therefore the fraction of skin cancer cases attributable to these risk factors. Three types of data are needed to run the model; demographic data (current and projected population sizes by age and sex), risk factor‐related data (prevalence, changes in prevalence as a result of interventions and risk estimates) and disease incidence data (cancer rates and estimated annual percentage change to account for trends in disease incidence that are not associated with modelled risk factor data). The projected numbers of new cancer cases were computed based on the demographic data and under different scenarios of changes in the prevalence of risk factors. Results are projected rates and numbers with and without modelled interventions by risk factor prevalence.
2.4. Exposure: sunbed use
The prevalence of sunbed use was derived from sun behaviour questionnaires of The Danish Sun Safety Campaign as described above. The campaign was the only initiative in Denmark collecting annual data on UVR exposure continuously since 2007.8, 10, 11, 21, 29, 30 In the Prevent model, 2015‐prevalence of sunbed use was included as ever/never‐use.
2.5. Incidence data
National incidence rates for melanoma skin cancer and keratinocyte skin cancer (ICD‐10 codes: C43 and C44) by sex and 5‐year age groups were retrieved from NORDCAN5and available in Table S1. The EAPC (estimated annual percentage change) for men and women, respectively, for the past 25 years was 6.4% and 10.9% increase for SCC, 5.4% and 7.4% for BCC and 4.4% and 4.5% for melanoma.5 We chose to use a uniform conservative 4% increase in skin cancer rates for men and women for the modelling. The EAPC was applied for the first 15 years after which it remained constant at this level. For sensitivity analysis, we applied an EAPC, respectively, of 0 and 30 years.
2.6. Population projections
From Statistics Denmark we obtained the size of the population on January 1st, of the corresponding period of the latest available incidence data by 1‐year age category and sex as well as forecasted population sizes for each year up to 2045, respectively, by 5‐year age categories and sex, using the medium national growth estimates.
2.7. Effect of sunbed use on the incidence of skin cancer
The applied relative risks for sunbed use on the risk of CM and keratinocyte cancers were derived from the largest meta‐analysis’, on the subject, established by, respectively, Boniol et al and Wehner et al CM: RR = 1.2 for >35‐year‐olds and RR = 1.59 for <35‐year‐olds and RR for SCC and BCC all ages of 1.67 and 1.29, respectively. 17, 31. These findings were used as the relative risks and risk functions in our modelling (Figure 1). The relative risks and risk functions were assumed equal for all age groups within age bands and included in the study, and across time. The effect of a risk factor exposure on cancer incidence has a latency time. Prevent accommodates this through two time lags: (a) the time that the risk remains unchanged after a decline in risk factor exposure (LAT) and (b) the period during which the changes in risk factor exposure gradually affect the risk of cancer, eventually reaching risk levels of the non‐exposed (LAG).27 For this study, we used a LAT of 2 years for sunbed use and a LAG of 18 years for CM and keratinocyte cancers. LAG was modelled as a linearly declining risk. LAT and LAG for sunbed use on risk of CM have not been estimated precisely; however, short time periods were previously used from the knowledge of intermittent exposure pathway1 and the experiences from Iceland32 and sunbed use in young people.12 We assume that after 20 years, the risk is comparable to a non‐exposed population.
Figure 1.
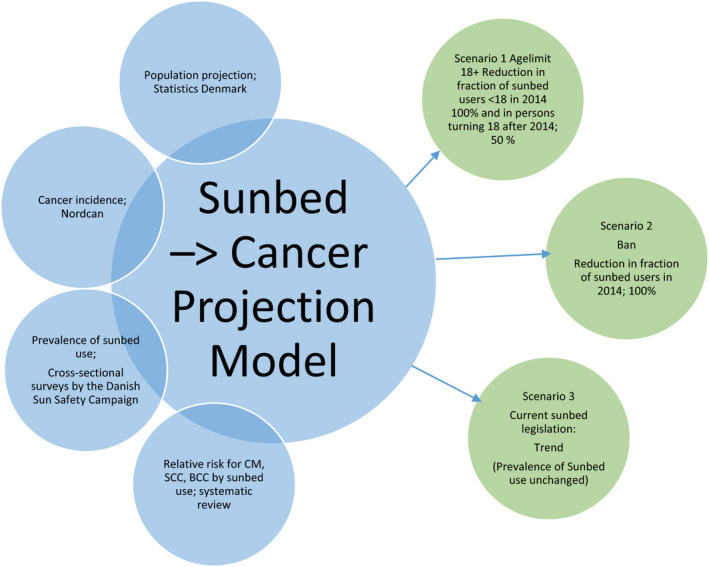
Illustration of data projections and scenario [Colour figure can be viewed at wileyonlinelibrary.com]
We have modelled the development in future skin cancer incidence in Denmark in three scenarios. We have used the potential reductions in sunbed use after 2014 to model skin cancer incidences during 2014‐45.
Scenario (1) The sunbed legislation includes an age limit of 18 years. We have assumed that the legislation would mean a 100% reduction for 0‐18‐year‐olds in the year of introduction and following a 50% decrease in sunbed use for persons turning 18 onwards as more than 50% of persons that have used a sunbed begins their use before the age of 18.
Scenario (2) The sunbed legislation includes a complete ban. This scenario assumes a 100% reduction of sunbed use for the entire population.
Scenario (3) The expected trend if prevalence of sunbed use is unchanged—current sunbed legislation (trend).
We have applied sensitivity analyses to scenario 2 to examine our assumptions. We have used the applied EAPC for 0 and 30 years, respectively, instead of the 15 years used in the main scenario. We have also applied a shorter or longer LAT+LAG time of either 2 and 8 years or 10 and 20 years.
The cost of skin cancer in Denmark was estimated to 33.3 million € annually in 2004‐2008.33 For assessment of skin cancer cost savings from the structural interventions, we used estimates of average case costs of skin cancer from Bentzen et al33 Rates were 10 263 € for CM, 6435 € for SCC and 1857 € For BCC. We assumed rates were unchanged from 2004‐2008 to 2014 where they were applied with a standard annual 3% discounting. The cost was calculated for avoided number of skin cancer cases in a given year with the discounted cost of that year.
3. RESULTS
Table 1 shows the distribution of demographic characteristics and prevalence of sunbed use from the 2015 data collection. Answers were collected from 3999 persons. The distribution of participants is representative to the Danish population on gender, age, region and education. More women compared to men and more participants aged 30‐50 compared to other ages had ever used sunbeds.
3.1. The prevalence of sunbed use influence on future skin cancer incidence
In Figure 2A‐C, we have modelled the development in the number of future skin cancer cases (CM, SCC and BCC) according to scenarios 1 and 2 in Denmark. The hypothetical results of a sunbed legislation including an 18‐year age limit would result in 186, 17 and 252 fewer cases of CM, SCC and BCC, respectively, in 2045 and similarly 1942, 113 and 1675 fewer cases in total during 2014‐2045. A complete sunbed ban would result in 475, 980 and 2722 fewer cases of CM, SCC and BCC, respectively, in 2045 and 9161, 17 351 and 55 375 fewer cases of CM, SCC and BCC, respectively, during 2014‐2045. Avoided skin cancers in the age limit scenario are most visible in the CM curve, as this skin cancer has a relatively high incidence among young people. The results of the skin cancer projections including relative percentage reductions are summarized in Table 2. It also includes projections of sensitivity variations of the ban scenario, where EAPC and LAT+LAG were examined. Sensitivity variations of the scenario showed they were fairly robust to changes in cancer incidence and time to effect.
Figure 2.
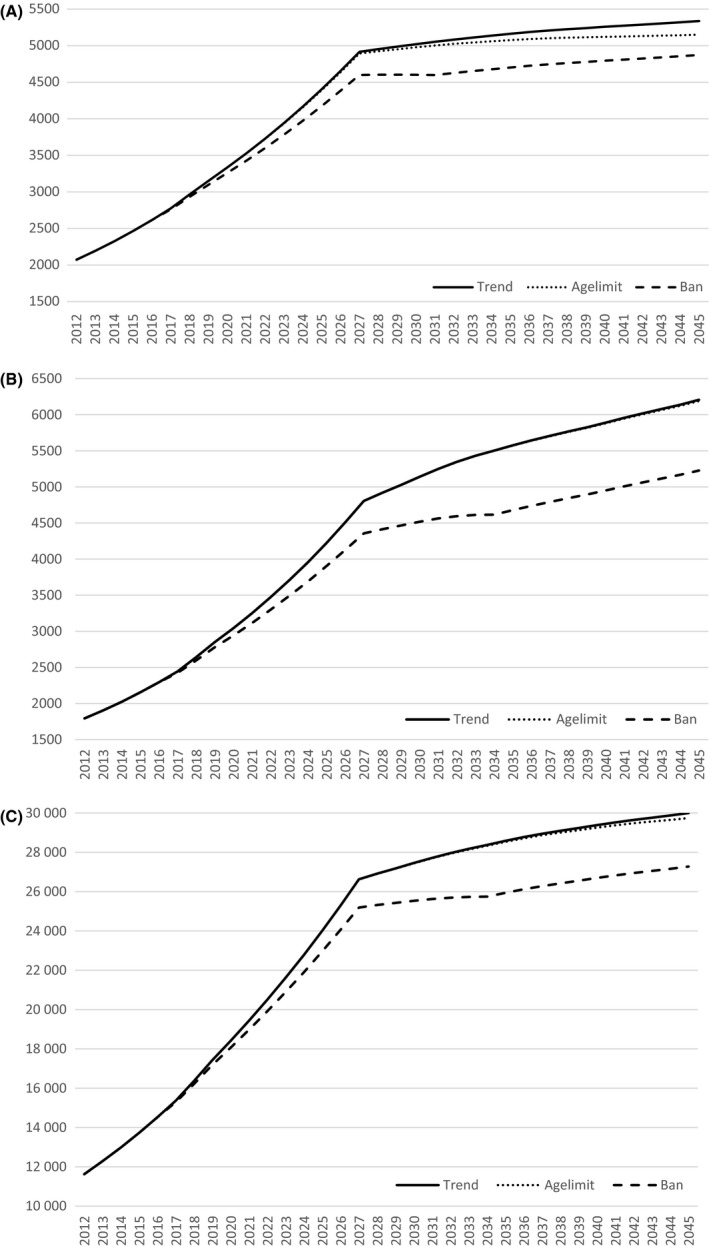
A, Development in melanoma 2014‐2045 in 2 scenarios of potential structural interventions decreasing sunbed use after 2014 compared to trend. The expected number of cutaneous melanoma cases, when sunbed use is unchanged, there is an 18 + agelimit or a complete ban. Assumed estimated annual percentage change 2014‐2029 (4% increase) and 2030‐2045 (0% constant). LAT time of 2 y and LAG time of 18 y. B, Development in squamous cell carcinoma 2014‐2045 in 2 scenarios of potential structural interventions decreasing sunbed use after 2014 compared to trend The expected number of squamous cell carcinoma cases, when sunbed use is unchanged, there is an agelimit or a complete ban. Assumed estimated annual percentage change 2014‐2029 (4% increase) and 2030‐2045 (0% constant). LAT time of 2 y and LAG time of 18 y
Table 2.
Projected number and change in number and percentage of skin cancer cases 2014‐2045 based on modelled scenarios of the change in sunbed use fraction after 2014 in Denmark compared to expected trend
| Projections based on potential structural interventions 2015 | Projections based on potential structural interventions 2015 | Sensitivity variations of Ban Scenario | ||||
|---|---|---|---|---|---|---|
| Scenario Expected number of cases with applied parameters | 18 + age limit | Ban | EAPC0 | EAPC30 | LATLAG, 2 + 8 y | LATLAG, 10 + 20 y |
| CM cases | 146 395 | 146 395 | 83 147 | 202 392 | 146 395 | 146 395 |
| SCC cases | 150 505 | 150 505 | 91 494 | 201 370 | 150 505 | 150 505 |
| BCC cases | 809 681 | 809 681 | 498 822 | 1 063 463 | 809 681 | 809 681 |
| Avoided cases from intervention | ||||||
| ΔTotal CM | 1942 (1.3%) | 9161 (6.3%) | 4687 (5.6%) | 14 125 (7.0%) | 10 634 (7.3%) | 5850 (4%) |
| ΔTotal SCC | 113 (0.1%) | 17 351 (11.5%) | 9782 (10.7%) | 25 334 (12.6%) | 19 550 (13.0%) | 11 716 (7.78%) |
| ΔTotal BCC | 1675 (0.2%) | 55 375 (6.8%) | 29 089 (5.8%) | 74 332 (7.0%) | 58 328 (7.2%) | 33 686 (4.2%) |
BCC, basal cell carcinoma; CM, cutaneous melanoma; SCC, squamous cell carcinoma.
EAPC0 and EAPC30 correspond to number of years with the estimated annual percentage change in incidence of 4%. Remaining years are constant (0%).
Main scenarios apply EAPC 4% 2014‐2029 and 0% 2030‐45 and 2 + 18 y LAT+LAG time.
In Figure 3, we show the potential cost savings of an age limit or a ban distributed by skin cancer type and total. The potential cost savings are 9 million € for an age limit and, as expected, much larger from a ban with savings of 129 million €. Even though more BCCs are avoided compared to SCC and CM, the contribution in potential savings is approximately equal from the three types of skin cancer because the average cost per case is higher for SCC and especially CM, compared to BCC.
Figure 3.
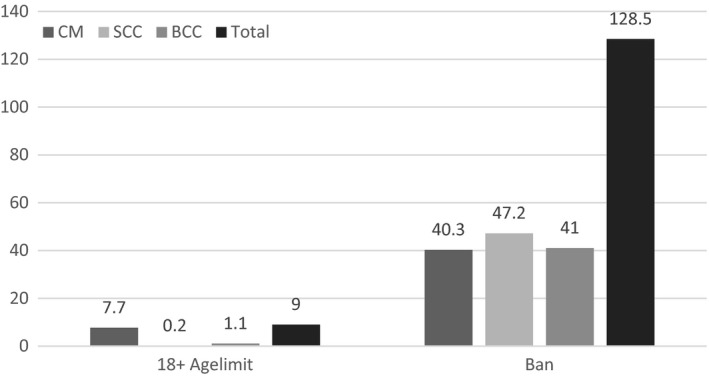
Potential saved costs from avoided skin cancers 2014‐2045 in million € Cost‐savings based on the number of potential avoided cases and the discontinued average case‐costs
4. DISCUSSION
We have shown that a sunbed legislation with an age limit as based on economical and health professional advice would have prevented almost 500 cases of skin cancer annually in 2045 and more than 4000 cases in total during 2014‐2045. Further, we have shown that progressive legislation, as a sunbed ban would have the largest possible impact on reducing the number of skin cancer cases by more than 80 000 corresponding to about 7% of all skin cancers in Denmark. Furthermore, we showed large cost savings from avoided skin cancer cases by implementation of structural interventions.
4.1. Strengths and limitations
Regarding a prognosis of the cancer incidence in absolute numbers, there are unknown factors, we are not able to include in the model like improved diagnostics, equipment, change in strength of UV spectrum or output in sunbeds6, 34 or other changes in UV exposure. However, as we are using the difference between two cancer incidence numbers this has minor influence on results. The reductions in skin cancer are based on the assumed reductions in sunbed use. If legislation, for example, is not properly implemented, skin cancer reductions will be influenced accordingly.
The reason that the skin cancer incidence in the years already passed is different from the actual incidence development is that additional factors are involved. About years 2002‐2004, the dermatoscope was introduced among dermatologists in Denmark, which probably increased the rate of detection6 in a period. In the following period, a plateau is seen from around 2011.5 Most likely, the decreased incidence rate is a consequence of the earlier detection/treatment, an effect also seen in various screening programmes. While the increasing skin cancer incidences raised the awareness in the media of the disease through the 1990s in 2007, the multicomponent Intervention of the Danish Sun Safety Campaign increased this awareness manifold. The increased awareness could also lead to an increase in mole check by the general physician, which again could lead to an increased number of diagnosed cases. We were not able to measure this. While, for example, the cancer risk after stopping smoking in the exposed population is assumed to be comparable to the non‐exposed population after a certain number of years, the skin cancer risk from sunbed may follow a similar pattern; however, the relation between UV radiation and skin cancer is often evaluated for a lifetime and UV exposure from the natural sun continues even though people quit using sunbeds. If the assumption of 20 years LAT+LAG time is shorter or longer, we may under or overestimate the benefits of the reductions in sunbed use; however, as shown in our sensitivity analysis extending the LAT+LAG time to 30 years still provides significant reductions in skin cancer incidence. Furthermore, recent sunbed use was shown to increase risk of skin cancer compared to non‐recent use.35 The model did not include any potential positive health effects of commercial sunbed use, because there was considered to be none, like, for example, from vitamin D–related illness as vitamin D is not a general problem in the population group affected by the discussed interventions.36 In addition, any vitamin D supplementation needed in subgroups is available from non‐harmful sources.
4.2. Reduction in sunbed use
Denmark had one of the highest reported frequencies of sunbed use in the world before the Danish Sun Safety Campaign was launched.10 Even though large reductions have taken place, the prevalence of sunbed use is now just comparable to other European countries, for example, 14% within the past year in Germany in 2012.37 The past years the reduction in sunbed use in Denmark has levelled off and structural interventions are needed for further reductions as campaigns are only sufficient to a perceptible audience.
Sunbed use was shown to be common even at very young ages. We have previously reported that children from the age of 8 years had been using sunbeds in Denmark,30 which was likewise reported in England.38 In 2008, 13% of 12‐14‐year‐olds reported sunbed use. In addition to lack of age limits, unstaffed sunbed studios is the main reason that children can be exposed to harmful UV radiation in sunbeds. New strengthening evidence from Lazovich et al12 of the influence of sunbed exposure for the development of CM in people younger than 30 years of age emphasizes the importance of having means to limit the sunbed use in young people.
In the Danish population, there has been an increasing support in the population for an age limit, which today has reached 4 out of 6 Danes being supportive and 1 out of 6 against while the remaining sixth is undecided.20
4.3. Consequences and recommendations
Guy et al39 showed that an age limit is effective in reducing the level of sunbed use. Thus, the results we have modelled of structural interventions are realistic predictions that are possible to achieve. We have shown that, had the Danish sunbed legislation of 2014 been based on the professional advice given, this would have added to future reductions in skin cancer. Additionally, we showed that the most efficient way to reduce the level of skin cancer is a complete ban, which was shown to be a feasible legislation in both Australia and Brazil.40 Gordon et al41 estimated avoidable skin cancers from average UVR exposure (solar vs. artificial) in Australia previous to their sunbed ban; however, while this method has several strengths compared to ours it does not include effects from the intermittent exposure pathway and as such this conservative method may have underestimated the actual number of avoidable skin cancers.
The WHO suggests that countries ban sunbeds or alternatively restrict (staff supervision, age limit, high‐risk individuals), manage (licence, radiation output and time limits, staff training, tax) and inform (health risks, display warning, ban marketing) to protect their populations.42 In 2017, the majority of countries in western Europe and the majority of American states have introduced age limits for sunbed use to protect children, and states with age limits succeeded in reducing the prevalence of sunbed use.39 Furthermore, the first countries, Australia and Brazil, have completely banned sunbed use to protect their population against the detrimental effects of sunbed use on human health and to reduce government spending related to skin cancer diagnostics and treatment.40 Belgium is to our knowledge the first European country to recommend a ban against sunbed use,43 while Denmark is now one of few remaining western European countries without an age limit to protect children and youth.44
Our results show significant skin cancer reductions and cost savings that emphasize both the economic and health potential of the results and we hope to motivate government administration to implement structural interventions to reduce the sunbed use in Denmark, by revision of the Danish sunbed legislation, which was adopted in 2014. The legislation was composed with severe contraries to the unambiguous economic and health professional arguments provided in the consultation. Other countries with insufficient protection of minors or the population against sunbed use can equally well benefit from our results according to the level of their prevalence of sunbed use.
5. CONCLUSION
Several legislative restrictive measures exist which would be beneficial to introduce to reduce the sunbed use further at the current stage. Danish politicians have the opportunity, supported by the population, to reduce the skin cancer incidence and thereby reduce the future costs of skin cancer. The health and economic benefits of structural interventions towards sunbed use to protect the Danish population, including minors, are huge.
CONFLICTS OF INTEREST
The authors have declared that no competing interests exist.
TRANSPARENCY DECLARATION
Brian Køster affirms that the manuscript is an honest, accurate and transparent account of the study being reported, that no important aspects of the study have been omitted and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Supporting information
ACKNOWLEDGEMENTS
The Danish Sun Safety Campaign acknowledges all the contributions, including from volunteers and members of the Danish Cancer Society as well as survey participants from Userneeds and Epinion, to optimize the campaign and campaign evaluation.
Køster B, Meyer MKH, Andersson TM‐L, Engholm G, Dalum P. Skin cancer projections and cost savings 2014‐2045 of improvements to the Danish sunbed legislation of 2014. Photodermatol Photoimmunol Photomed. 2019;35:78–86. 10.1111/phpp.12424
Funding information
This study was supported by TrygFonden.
REFERENCES
- 1. Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63(1–3):8‐18. [DOI] [PubMed] [Google Scholar]
- 2. IARC . Radiation: Volume 100 D – a review of human carcinogens. Lyon, France: International Agency for Research on Cancer (IARC), World Health Organization (WHO); 2012. [Google Scholar]
- 3. Gandini S, Sera F, Cattaruzza MS, et al. Meta‐analysis of risk factors for cutaneous melanoma: II Sun exposure. Eur J Cancer. 2005;41(1):45‐60. [DOI] [PubMed] [Google Scholar]
- 4. Veierod MB, Adami HO, Lund E, Armstrong BK, Weiderpass E. Sun and solarium exposure and melanoma risk: effects of age, pigmentary characteristics, and nevi. Cancer Epidemiol Biomarkers Prev. 2010;19(1):111‐120. [DOI] [PubMed] [Google Scholar]
- 5. Engholm G, Ferlay J, Christensen N, et al. NORDCAN: Cancer incidence, mortality, prevalence and survival in the Nordic Countries, Version 7.3 (08.07.2016). Association of the Nordic Cancer Registries. Danish Cancer Society. 2016. http://www.ancr.nu. Accessed August 15, 2016.
- 6. Helvind NM, Holmich LR, Smith S, et al. Incidence of in situ and invasive melanoma in Denmark from 1985 through 2012: a National Database Study of 24,059 melanoma cases. JAMA Dermatol. 2015;151(10):1087‐1095. [DOI] [PubMed] [Google Scholar]
- 7. Bay C, Kejs AM, Storm HH, Engholm G. Incidence and survival in patients with cutaneous melanoma by morphology, anatomical site and TNM stage: a Danish Population‐based Register Study 1989‐2011. Cancer Epidemiol. 2015;39(1):1‐7. [DOI] [PubMed] [Google Scholar]
- 8. Koster B, Thorgaard C, Philip A, Clemmensen IH. Vacations to sunny destinations, sunburn, and intention to tan: a cross‐sectional study in Denmark, 2007‐2009. Scand J Public Health. 2011;39(1):64‐69. [DOI] [PubMed] [Google Scholar]
- 9. Behrens CL, Schiøth C, Christensen AS. Sun habits of the Danes in sunny vacations 2015. (Report in Danish accessed at www.skrunedforsolen.dk). 2016. Accessed January 2018.
- 10. Koster B, Thorgaard C, Philip A, Clemmensen I. Sunbed use and campaign initiatives in the Danish population, 2007‐2009: a cross‐sectional study. J Eur Acad Dermatol Venereol. 2011;25(11):1351‐1355. [DOI] [PubMed] [Google Scholar]
- 11. Koster B, Thorgaard C, Philip A, Clemmensen IH. Prevalence of sunburn and sun‐related behaviour in the Danish population: a cross‐sectional study. Scand J Public Health. 2010;38(5):548‐552. [DOI] [PubMed] [Google Scholar]
- 12. Lazovich D, Isaksson Vogel R, Weinstock MA, Nelson HH, Ahmed RL, Berwick M. Association between indoor tanning and melanoma in younger men and women. JAMA Dermatol. 2016;152(3):268‐275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vogel RI, Ahmed RL, Nelson HH, Berwick M, Weinstock MA, Lazovich D. Exposure to indoor tanning without burning and melanoma risk by sunburn history. J Natl Cancer Inst. 2014;106(7). http://doi.org.10.1093/jnci/dju219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lazovich D, Vogel RI, Berwick M, Weinstock MA, Anderson KE, Warshaw EM. Indoor tanning and risk of melanoma: a case‐control study in a highly exposed population. Cancer Epidemiol Biomarkers Prev. 2010;19(6):1557‐1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cust AE, Armstrong BK, Goumas C, et al. Sunbed use during adolescence and early adulthood is associated with increased risk of early‐onset melanoma. Int J Cancer. 2010;128:2425‐2435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. El GF, Baan R, Straif K, et al. A review of human carcinogens–part D: radiation. Lancet Oncol. 2009;10(8):751‐752. [DOI] [PubMed] [Google Scholar]
- 17. Boniol M, Autier P, Boyle P, Gandini S. Cutaneous melanoma attributable to sunbed use: systematic review and meta‐analysis. BMJ. 2012;345:e4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wehner MR, Chren MM, Nameth D, et al. International prevalence of indoor tanning: a systematic review and meta‐analysis. JAMA Dermatol. 2014;150(4):390‐400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Meyer MKH, Mortensen JH, , Behrens CL. Unges solarievaner 2015 [Youth Sunbed use 2015, in Danish]. Copenhagen: Danish Cancer Society & TrygFonden smba; (TryghedsGruppen smba), 2016. English summary available at: www.skrunedforsolen.dk (Accessed 31 March, 2017). 2016. 978‐87‐7064‐328‐3. [Google Scholar]
- 20. Behrens CL, Schiøth C, Christensen AS. Danskernes solarievaner 2015 – en kortlægning [Sunbed use of the Danes 2015, in Danish]. Copenhagen: Danish Cancer Society & TrygFonden smba; (TryghedsGruppen smba), 2016. wwwskrunedforsolendk (Accessed 31 March, 2017). [Google Scholar]
- 21. Koster B, Thorgaard C, Clemmensen IH, Philip A. Sunbed use in the Danish population in 2007: a cross‐sectional study. Prev Med. 2009;48(3):288‐290. [DOI] [PubMed] [Google Scholar]
- 22. Julie H, Mortensen CLB, Brian K. Danskernes solariebrug 2016 – Notat [Sunbed habits of the Danes 2016‐ Brief (in Danish)]. 2016.
- 23. Queen Margrethe II/by Minister of Health NH . The Danish Sunbed Legislation (in Danish). 2014. [cited 2017 7. May]. https://www.retsinformation.dk/Forms/R0710.aspx?id=163654. Accessed January 2018.
- 24. Facta S, Fusette SS, Bonino A, Anglesio L, D'Amore G. UV emissions from artificial tanning devices and their compliance with the European Technical Standard. Health Phys. 2013;104(4):385‐393. [DOI] [PubMed] [Google Scholar]
- 25. Danish Sunbed Legislation . Consultation http://www.ft.dk/samling/20131/lovforslag/l163/bilag/1/1350927.pdf. Accessed May 8, 2017.
- 26. Danish Sunbed Legislation . https://www.retsinformation.dk/Forms/R0710.aspx?id=163654 Accessed May 8, 2017. 2014.
- 27. Soerjomataram I, de Vries E, Engholm G, et al. Impact of a smoking and alcohol intervention programme on lung and breast cancer incidence in Denmark: an example of dynamic modelling with Prevent. Eur J Cancer. 2010;46(14):2617‐2624. [DOI] [PubMed] [Google Scholar]
- 28. Barendregt J. http://www.epigear.com/index_files/prevent.html [cited 2016 01.10.2016]. Accessed January 2018.
- 29. Meyer MK, Koster B, Juul L, et al. Sunbed use among 64,000 Danish students and the associations with demographic factors, health‐related behaviours, and appearance‐related factors. Prev Med. 2017;100:17‐24. [DOI] [PubMed] [Google Scholar]
- 30. Krarup AF, Koster B, Thorgaard C, Philip A, Clemmensen IH. Sunbed use by children aged 8‐18 years in Denmark in 2008: a cross‐sectional study. Br J Dermatol. 2011;165(1):214‐216. [DOI] [PubMed] [Google Scholar]
- 31. Wehner MR, Shive ML, Chren MM, Han J, Qureshi AA, Linos E. Indoor tanning and non‐melanoma skin cancer: systematic review and meta‐analysis. BMJ. 2012;345:e5909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hery C, Tryggvadottir L, Sigurdsson T, et al. A melanoma epidemic in Iceland: possible influence of sunbed use. Am J Epidemiol. 2010;172(7):6. [DOI] [PubMed] [Google Scholar]
- 33. Bentzen J, Kjellberg J, Thorgaard C, Engholm G, Phillip A, Storm HH. Costs of illness for melanoma and nonmelanoma skin cancer in Denmark. Eur J Cancer Prev. 2013;22:569‐576. [DOI] [PubMed] [Google Scholar]
- 34. Nilsen LT, Hannevik M, Aalerud TN, Johnsen B, Friberg EG, Veierod MB. Trends in UV irradiance of tanning devices in Norway: 1983‐2005. Photochem Photobiol. 2008;84(5):1100‐1108. [DOI] [PubMed] [Google Scholar]
- 35. Ghiasvand R, Rueegg CS, Weiderpass E, Green AC, Lund E, Veierod MB. Indoor tanning and melanoma risk: long‐term evidence from a prospective Population‐Based Cohort Study. Am J Epidemiol. 2017;185(3):147‐156. [DOI] [PubMed] [Google Scholar]
- 36. Hansen L, Tjonneland A, Koster B, et al. Sun exposure guidelines and serum vitamin D status in Denmark: The StatusD Study. Nutrients. 2016;8(5):266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Schneider S, Diehl K, Bock C, et al. Sunbed use, user characteristics, and motivations for tanning: results from the German Population‐Based SUN‐Study. JAMA Dermatol. 2012;2012:1‐7. [DOI] [PubMed] [Google Scholar]
- 38. Thomson CS, Woolnough S, Wickenden M, Hiom S, Twelves CJ. Sunbed use in children aged 11‐17 in England: face to face quota sampling surveys in the National Prevalence Study and Six Cities Study. BMJ. 2010;340:c877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Guy GP Jr, Berkowitz Z, Jones SE, et al. State indoor tanning laws and adolescent indoor tanning. Am J Public Health. 2014;104(4):e69‐e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sinclair CA, Makin JK, Tang A, Brozek I, Rock V. The role of public health advocacy in achieving an outright ban on commercial tanning beds in Australia. Am J Public Health. 2014;104(2):e7‐e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Gordon LG, Hirst NG, Gies PH, Green AC. What impact would effective solarium regulation have in Australia? Med J Aust. 2008;189(7):375‐378. [DOI] [PubMed] [Google Scholar]
- 42. WHO . Artificial tanning devices ‐ Public health interventions to manage sunbeds. Geneva: World Health Organization; 2017. [Google Scholar]
- 43. Belgium SHC . Advisory report of the superior health council no. 9216. Recommendations on the use of artificial UV devices in Belgium. 2017. Contract No.: 9216.
- 44. WHO . Legislation of artificial tanning sunbeds 2017 [cited 2017 July 2017]. Available from: http://apps.who.int/gho/data/node.main.SUNBEDS?lang=en. Accessed January 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


