Abstract
Purpose
In rural areas, the management of hospitalizations and emergency department (ED) visits is an important issue, and it is compounded by factors such as the long distance to secondary care facilities, funding difficulties in many rural medical institutions, and shortage of medical staff. While better patient experience (PX) has been shown to reduce hospitalizations and ED visits, previous studies have not considered the differences between urban and rural areas. In addressing this gap, this study examines the association between PX and hospitalizations/ED visits on isolated islands.
Methods
This prospective cohort study was conducted on 5 isolated islands in Okinawa, Japan. We assessed the PX of primary care using the Japanese version of the Primary Care Assessment Tool (JPCAT), which comprises 6 domains: first contact, longitudinality, coordination, comprehensiveness (services available), comprehensiveness (services provided), and community orientation. The primary outcome was hospitalizations and ED visits in a year. We used a mixed effect model to adjust clustering within islands and individual covariates.
Findings
Of 1,258 residents, 740 responded to a questionnaire for PX measurement. There were 73 hospitalizations and 62 ED visits. Adjusting for confounding and geographical clustering, hospitalizations had significant positive association with the PX score of each patient. ED visits were not associated with the total score of the JPCAT.
Conclusion
On the isolated islands, PX in primary care had positive correlation with hospitalizations. The contrast of our findings to those of previous studies may be due to the close patient‐doctor relationship on isolated islands.
Keywords: emergency department visits, hospitalization, island health, Japanese health care, patient experiences
There is a correlation between hospitalizations and emergency department (ED) visits and high health care expenditure.1 Consequently, reducing the amount of hospitalizations and ED visits is an important role of a primary care physician. In rural areas—and isolated islands in particular—the importance of the optimal management of hospitalizations and ED visits is compounded by issues such as the long distances to secondary care, financial difficulty in many rural medical institutions, and shortage of medical staff.2
Patient experience (PX) is an indispensable factor in the provision of quality primary care.3 A measure of patient‐centeredness,4 PX is 1 of the 3 pillars of quality in health care, alongside clinical effectiveness and patient safety.5 Previous research has revealed that PX is associated with better prevention services, disease management, and care outcomes.6 Indeed, systematic reviews indicate that better PX can reduce hospitalizations and ED visits.7, 8, 9 In their systematic review, for instance, Doyle and associates reported that the positive effect of continuity in the relationship between patients and doctor/health provider—assessed by PX—had a negative impact on hospitalization and ED visits.3, 9, 10
However, previous studies—including these systematic reviews—mainly used nationally or regionally representative samples, such as data from Medicare11 or Medicaid,12, 13 and failed to account for differences between urban and rural areas. Moreover, because there are no previous studies on the association between PX and hospitalizations/ED visits in remote areas/isolated islands, it is unclear whether the relation is the same in rural/isolated areas as it is in central/urban areas. This prospective cohort study sought to address this gap by examining the relationship between PX and hospitalizations/ED visits on isolated islands. The results of this study provide useful suggestions for health care providers and policymakers in rural areas to optimize health care utilization while reducing costs.
Methods
Design
We conducted a prospective cohort study of 5 isolated islands in Okinawa Prefecture, Japan. Figure 1 illustrates the geographical location of these islands.
Figure 1.
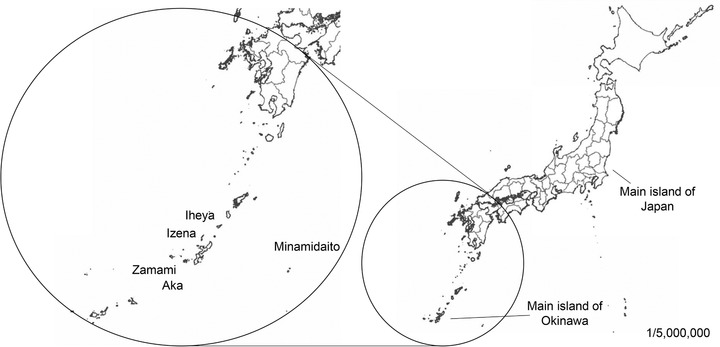
Geographical Location of 5 Islands in Okinawa in Relation to Mainland Japan.
Okinawa Prefecture consists of 54 islands, 39 of which are inhabited.14 Eighteen islands have solo practice clinics15; of these, Okinawa Prefecture has 16 prefectural clinics on 15 islands (each island has 1 clinic, except for Iriomote island, which has 2).16 Of the 15 inhabited islands with clinics, the local governments of 5 cooperated in conducting this study's survey.
Prefectural hospitals have a training program for solo primary care physicians (PCP) on isolated islands.15 On average, the PCPs on the islands evaluated in this study have 4‐6 years of experience, their clinics have 2‐4 staff (1 physician, 1 nurse, and up to 2 clerks) but no beds, and the clinics provide 24‐hour emergency medical services. The clinics are equipped with electrocardiogram, X‐ray, ultrasound, and microscope equipment; simple blood tests are also available. As there are no surgical facilities or hospitals with beds, however, patients with advanced‐care needs are referred to off‐island secondary facilities.15 A medical helicopter service is available to transport patients with emergency illnesses to the main island of Okinawa.
Participants
The study participants were all aged 65 years or older. Generally, elderly people use EDs and are admitted to hospitals at a higher rate compared to younger people,17 and we assumed outcomes such as ED visits/hospitalizations frequently occurred among elderly people based on our previous study conducted on isolated islands in Okinawa, Japan.18 The participants were residents of the 5 islands whose local governments cooperated in our survey. The characteristics of these islands are provided in Appendix 1 (available online only). The study was conducted over a period of 1 year, from October 1, 2016, to September 30, 2017; the PX survey was conducted in October‐November 2016. At the beginning of our study, approximately 1,257 residents on the 5 islands (600 male, 657 female) were aged 65 years or over.19 We delivered a questionnaire to the town offices on each island: on 4 islands, town offices received JPY ¥200 per completed response, while the town office on 1 island did not require remuneration.
Inclusion Criteria
All inhabitants of the 5 islands who were aged 65 years and over as of October 1, 2016, were included in this study.
Exclusion Criteria
Inhabitants who opted against taking part in the study and/or were unable to respond to the questionnaire due to cognitive impairment or mental disorder were excluded from this study.
Measures
Patient Experience of Primary Care
We employed the Japanese version of the Primary Care Assessment Tool (JPCAT)20 for data collection. Since its development by the Johns Hopkins Primary Care Center, the PCAT has been adapted to numerous countries to measure the quality of primary care using patient experience. The JPCAT employed in this study is based on the PCAT‐AE.21 The JPCAT scoring system is structured as follows: each response is measured on a 5‐point Likert scale, reduced by a factor of 1 and multiplied by 25. The score for each of the domains is computed as the mean value for all converted scale scores in that domain. Thus, the domain scores range from 0 to 100 points, with higher scores indicating better performance. The total score is the mean of 6 domain scores: namely, first contact, longitudinality, coordination, comprehensiveness in terms of services available, comprehensiveness in terms of services provided, and community orientation. The total score reflects an overall measure of the quality of core primary care principles. Previous studies have shown that the JPCAT has good reliability and validity,20 and that it is associated with the adoption of breast cancer screening,22 advanced care planning discussions,23 and the bypassing of PCPs.24
ED Visits and Hospitalizations
We prospectively recorded the numbers of ED visits and hospitalizations that occurred outside the islands using the electronic medical record system, “Clinic Viewer,” developed by a doctor who had been practicing on an island. This system is currently used among 16 clinics on remote islands. We ascertained the actual numbers of ED visits and hospitalizations using response letters from referral facilities and/or information from patient records. We excluded planned hospitalizations, such as elective surgery for cataracts or elective colonoscopy for patients after having a colectomy, as we assumed that planned hospitalizations might not be associated with PX because such planned admissions could mainly be for elective procedures that were unavailable in the islands.
Covariates
Covariates were selected based on a literature review to identify factors that may confound the association between patient experience and ED visits/hospitalizations. We included covariates for age, sex, number of comorbidities, years of education, household income, self‐rated health, and the existence of regular visits to a primary care clinic on each island. All covariates were evaluated as categorical variables through a self‐administered questionnaire.
Statistical Analysis
To determine the associations between the JPCAT scores and hospitalizations/ED visits, a multivariate analysis was conducted using a generalized linear mixed model with a logit link function that includes a random effect for island and individual covariates as fixed effects. This model incorporated a random intercept for islands using a centering within cluster. The JPCAT scores were centered on the island mean in order to estimate patient‐level effects. The following individual covariates were included in the analysis: sex, age, number of comorbidities, educational status, household income, self‐rated health, and existence of regular visits to a primary care clinic on each island. We used multiple imputations by fully conditional specification to allow for uncertainty in the missing values for independent variables, with the JPCAT scores, sex, age, number of comorbidities, educational status, household income, self‐rated health, and existence of regular visits to a primary care clinic as variables in the imputation model. We thus created 20 imputed data sets.
According to the sample size formula demonstrated in a previous study, events per variable values of ≥10 were necessary for logistic regression analysis.25 We estimated a minimum sample size of 667 because the maximum number of variables in this study was 8. Moreover, the incidence of ED visits/hospitalizations in our target population was assessed to be 1% per month according to the previous study by Kaneko and colleagues.26 We used R version 3.3.2 (R Foundation for Statistical Computing, Vienna, Austria; https://www.r-project.org) for statistical analyses.
Ethical Considerations
This study was approved by the Research Ethics Committee of Okinawa Chubu Hospital, Japan (approval number 52, 2015), as well as the research ethics committees of Okinawa Hokubu Hospital, Okinawa Prefectural Nanbu Medical Center and Children's Medical Center, Okinawa Miyako Hospital, and Okinawa Yaeyama Hospital. We considered the response to the questionnaire as consent for the study and followed respondents for 1 year.
Results
Approximately 58.8% of respondents completed the survey, and we performed analyses of these 740 (male 345, female 395) respondents.
Table 1 provides the characteristics of the respondents. Approximately 23% were found to be aged ≥85, while 71.8% visited a primary care clinic regularly. We also found that 30% of respondents had 2 or more comorbidities. In terms of education level, 59.5% of respondents had no high school education. Finally, 64.5% of respondents had an annual household income under JPY ¥200 million (≒ less than US$ 18,000).
Table 1.
Participant Characteristics (N = 740)
| Characteristic | Number (%) |
|---|---|
| Sex | |
| Male | 339 (45.8) |
| Female | 395 (53.4) |
| Missing values: 6 (0.8) | |
| Age (years) | |
| 65‐74 | 296 (40.0) |
| 75‐84 | 264 (35.7) |
| 85‐94 | 159 (21.5) |
| 95+ | 11 (1.5) |
| Missing values: 10 (1.4) | |
| Regular visit to a doctor on an island | |
| Yes | 531 (71.8) |
| No | 150 (20.3) |
| Missing values: 59 (7.8) | |
| Number of morbidities | |
| 0 | 73 (9.9) |
| 1 | 196 (26.5) |
| 2 | 181 (24.5) |
| ≥3 | 227 (30.7) |
| Missing values: 63 (8.5) | |
| Education | |
| Less than high school | 440 (59.5) |
| High school | 181 (24.5) |
| Junior college | 24 (3.2) |
| More than or equal to college | 23 (3.1) |
| Missing values: 72 | |
| Annual household income (million ¥ JPY) | |
| <2.00 (≒18,000 US $) | 477 (64.5) |
| 2.00‐4.99 | 131 (17.7) |
| ≥5.00 | 39 (5.2) |
| Missing values: 93 (12.6) | |
| Self‐rated health | |
| Very good | 31 (4.1) |
| Good | 83 (11.2) |
| Neutral | 338 (45.7) |
| Poor | 218 (29.5) |
| Very poor | 23 (3.1) |
| Missing values: 47 (6.4) |
Table 2 provides the means and standard deviations of the JPCAT scores. Out of a possible 100 points, the average JPCAT score was 67.8. The highest scoring domain was first contact (84.5), while the lowest scoring domain was comprehensiveness in terms of services provided (39.7). There were 73 hospitalizations and 62 ED visits during the study period. The hospitalizations/ED visits group had a high JPCAT score in comparison to the nonhospitalizations/ED visits group.
Table 2.
Distribution of the JPCAT
| JPCAT Scores Mean (SD) | Total (N = 740) | Hospitalizations (N = 73) | Nonhospitalizations (N = 667) |
|---|---|---|---|
| Total score | 67.8 (15.6) | 72.2 (12.6) | 67.3 (15.8) |
| First contact | 84.5 (17.2) | 86.0 (17.0) | 84.3 (17.3) |
| Longitudinality | 76.7 (19.8) | 83.3 (17.5) | 76.0 (19.9) |
| Coordination | 73.4 (25.3) | 85.7 (20.2) | 72.7 (25.4) |
| Comprehensiveness (service available) | 65.4 (24.6) | 69.4 (23.1) | 65.0 (24.7) |
| Comprehensiveness (service provided) | 39.7 (28.7) | 39.9 (27.9) | 39.7 (28.8) |
| Community orientation | 65.9 (21.7) | 69.5 (22.5) | 65.5 (21.6) |
| ED visits (N = 62) | Non‐ED visits (N = 678) | ||
| JPCAT scores mean (SD) | |||
| Total score | 72.0 (13.3) | 67.4 (15.7) | |
| First contact | 85.5 (18.2) | 84.4 (17.2) | |
| Longitudinality | 82.1 (17.0) | 76.2 (20.0) | |
| Coordination | 86.3 (20.7) | 72.8 (25.3) | |
| Comprehensiveness (service available) | 70.1 (22.7) | 65.0 (24.7) | |
| Comprehensiveness (service provided) | 39.0 (30.7) | 39.7 (28.5) | |
| Community orientation | 68.9 (23.1) | 65.7 (21.5) |
SD, standard deviation; ED, emergency department.
Tables 3 and 4 display the results of the mixed effect model analyses of the association between patient experience of primary care and hospitalizations/ED visits. After adjusting for possible confounders and clustering within clinics, a higher total JPCAT score was significantly associated with hospitalizations: odds ratio (OR) per 1 standard deviation increase = 1.39; 95% confidence interval (CI): 1.03‐1.86; P = .03. ED visits were not associated with the total JPCAT score. In terms of each domain of PX, longitudinality was associated with hospitalizations, while coordination was associated with hospitalizations and ED visits. This is statistically significant.
Table 3.
Factors Associated With Hospitalizations (n = 740)a
| JPCAT Scale | Adjusted OR per 1 SD Increase (95% CI) | P Value |
|---|---|---|
| Total score | 1.39 (1.03‐1.86) | .030 |
| First contact | 1.08 (0.84‐1.40) | .577 |
| Longitudinality | 1.47 (1.06‐2.04) | .021 |
| Coordination | 1.81 (1.29‐2.64) | .001 |
| Comprehensiveness (service available) | 1.12 (0.84‐1.48) | .446 |
| Comprehensiveness (service provided) | .94 (0.72‐1.24) | .067 |
| Community orientation | 1.30 (0.97‐1.76) | .075 |
JPCAT, Japanese version of the Primary Care Assessment Tool; OR, odds ratio.
aGeneralized linear mixed model; adjusted for age, sex, education, household income, number of comorbidities, and self‐rated health.
Table 4.
Factors Associated With ED Visits (n = 740)a
| JPCAT Scale | Adjusted OR per 1 SD Increase (95% CI) | P Value |
|---|---|---|
| Total score | 1.32 (0.96‐1.81) | .089 |
| First contact | 1.14 (0.85‐1.51) | .383 |
| Longitudinality | 1.34 (0.95‐1.88) | .091 |
| Coordination | 1.74 (1.22‐2.55) | .003 |
| Comprehensiveness (service available) | 1.13 (0.83‐1.56) | .429 |
| Comprehensiveness (service provided) | 0.89 (065‐1.18) | .375 |
| Community orientation | 1.19 (0.85‐1.68) | .300 |
ED, emergency department; JPCAT, Japanese version of the Primary Care Assessment Tool; OR, odds ratio.
aGeneralized linear mixed model; adjusted for age, sex, education, household income, number of comorbidities, and self‐rated health.
Discussion
This study evidences that there is better PX in the hospitalizations/ED visits group than in the nonhospitalizations/ED visits group. After adjusting for age, sex, chronic health problems, years of education, household income, and self‐rated health, the total JPCAT and longitudinality scores were associated with hospitalizations. Moreover, the coordination score was associated with ED visits.
While the systematic review by Doyle et al3 shows that better PX is related to fewer hospitalizations, the results of our study conducted on isolated islands indicate the opposite. This difference may be due to the close relationship between doctors and patients on the rural/isolated islands. Generally, PCPs consider PX as an impact factor and sometimes find themselves in a dilemma between “satisfying patients and performing good health care.”27 Moreover, rural PCPs tend to establish closer relationships with their patients in comparison to those in urban areas.28 This is particularly the case with regard to chronic conditions, with doctors in rural communities tending to have greater familiarity with their patients, as well as their families, histories, and circumstances.29 Consequently, rural PCPs may conduct excessive triage to avoid undermining this close relationship.
This rural/urban contrast with regard the association between PX and hospitalizations may also result from the positive association between hospitalizations and longitudinality. In terms of the JPCAT, both longitudinality and coordination were associated with hospitalizations. As a result of this association, longitudinality may cause close relationships between doctors and patients. However, the domain of coordination included the patient's past experience of referrals; as such, past referrals to secondary care facilities may be associated with referrals and hospitalizations during the study period. Additionally, PCPs may actively reduce risks to good PX through coordination.
With regard to ED visits, the total JPCAT score did not indicate significant differences, with ED visits and coordination showing a similar association. This can be explained by the low incidence of ED visits compared to hospitalizations. Since the point estimation was 1.32—compared to the 1.39 of hospitalizations—the lack of significant association between the total JPCAT score and ED visits may be attributable to the low number of events. This may be related to past experience of referrals to the main island, as well as the association between the coordination score and hospitalizations.
Study Strengths
This is the first study to examine the association between PX and hospitalizations/ED visits on isolated islands. Furthermore, we employed the JPCAT as an indicator of PX, which has been used by past studies to assess PX in primary care. In doing so, and by using a mixed effect model, we could adjust possible confounding factors and clustering within islands.
Study Limitations
This study has several limitations. First, there is a concern regarding the response rate of 58.8%, which may not be high enough. In the case of patient experience surveys, however, there is little evidence that low response rate introduces selective nonresponse bias.30 Second, several residents (eg, patients with terminal cancer or on dialysis) may have relocated from the islands during the study period because of the difficulties associated with regular visits to medical facilities on the main island of Okinawa. However, the net migration rate of these islands was 0.65% during the period of study. As such, while it is important to consider this possibility in future studies, we feel that it is unlikely that migration affected our results.31 Third, although data regarding the reasons for referral, severity of illness, and final diagnosis are important in assessing the association between PX and hospitalizations/ED visits, we were unable to obtain this information. This is mainly because PCPs did not use a common code when recording the reason for visits and diagnoses. However, because PX is associated with subjective health status rather than objective indicators such as a diagnosis or disease severity32 and we adjusted subjective health status in the study, the influence from lack of information on a diagnosis and disease severity might be limited. Fourth, we were unable to evaluate the follow‐up rate because this study measured the hospitalizations/ED visits through the electronic medical record in each island. Although patients with severe symptoms and in need of hospitalization/an ED visit usually contact the clinics at first, they may potentially skip the PCPs altogether—particularly those with low PX. Consequently, our study did not include patients with low PX in each clinic. Finally, this study did not include inhabitants unable to respond to the questionnaire due to cognitive impairment and mental disorder, such as dementia. Also, this study did not include people aged 64 years and younger. Thus, our results should be applied carefully to younger populations.
Conclusion
PX and especially longitudinality and coordination in primary care, may have a positive correlation with hospitalizations and ED visits on isolated islands. PCPs may conduct excessive triage to avoid undermining their close relationships with patients. To explore factors associated with the results of the study, further quantitative and qualitative research regarding the association between PX and patient behavior on isolated islands is required.
Supporting information
Appendix 1. Characteristics of the 5 Islands Included in This Study
Disclosures
The authors declare there are no potential competing interests relevant to this work. This study was approved by the Research Ethics Committee of Okinawa Chubu Hospital, Japan (approval number 52, 2015), as well as the research ethics committees of Okinawa Hokubu Hospital, Okinawa Prefectural Nanbu Medical Center and Children's Medical Center, Okinawa Miyako Hospital, and Okinawa Yaeyama Hospital.
Funding
This study was supported by the Byoutaiseiri Institute. The study sponsor had no role in the study design, data collection, analysis and interpretation, writing of the report, or the decision to submit the article for publication.
Acknowledgments
We thank the members of the Okinawan Remote Islands‐Practice Based Research Network: Makoto Ozaki, MD; Masafumi Funato, MD; Syo Yonaha, MD; Keita Yamashiro, MD; Eitaro Jiroku, MD; Toshiki Sakugawa, MD; Kazutaka Yoshida, MD; Genki Kinjyo, MD; Tadahiro Yonaha, MD; Yusuke Saishoji, MD; Tatsuya Sakai, MD; Takamitsu Miyake, MD; Shoko Murata, MD; Taiki Asato, MD; Kaku Kuroda, MD; Moe Ozawa, MD; Yoshifumi Sugiyama, MD; Sho Koki, MD; Koji Yamakoshi, MD; Masaki Ishihara, MD; and Ryo Adaniya, MD. We also thank all town offices and all inhabitants on the 5 islands.
References
- 1. Johansen ME. Comparing medical ecology, utilization, and expenditures between 1996–1997 and 2011–2012. Ann Fam Med. 2017;15(4):313‐321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Geyman JP, Norris TE, Hart G, eds. Textbook of Rural Medicine. Part 1: Overview of Rural Health Care New York, NY: McGraw‐Hill; 2001. [Google Scholar]
- 3. Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3(1):1‐18. 10.1136/bmjopen-2012-001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Browne K, Roseman D, Shaller D, Edgman‐Levitan S. Analysis & commentary: measuring patient experience as a strategy for improving primary care. Health Aff. 2010;29(5):921‐925. 10.1377/hlthaff.2010.0238. [DOI] [PubMed] [Google Scholar]
- 5. Institute of Medicine (US) Committee on Quality of Health Care in America . Crossing the Quality Chasm: a New Health System for the 21st Century. Washington, DC: The National Academies Press; 2001. 10.17226/10027. [DOI] [PubMed] [Google Scholar]
- 6. Sequist TD, Schneider EC, Anastario M, et al. Quality monitoring of physicians: linking patients’ experiences of care to clinical quality and outcomes. J Gen Intern Med. 2008;23(11):1784‐1790. 10.1007/s11606-008-0760-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Drotar D. Physician behavior in the care of pediatric chronic illness: association with health outcomes and treatment adherence. J Dev Behav Pediatr. 2009;30(3):246‐254. 10.1097/DBP.0b013e3181a7ed42. [DOI] [PubMed] [Google Scholar]
- 8. Cabana MD, Jee SH. Does continuity of care improve patient outcomes? J Fam Pract. 2004;53(12):974‐980. [PubMed] [Google Scholar]
- 9. Saultz JW, Lochner J. Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med. 2005;3(2):159‐166. 10.1370/afm.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sans‐Corrales M, Pujol‐Ribera E, Gené‐Badia J, et al. Family medicine attributes related to satisfaction, health and costs. Fam Pract. 2006;23(3):308‐316. 10.1093/fampra/cmi112. [DOI] [PubMed] [Google Scholar]
- 11. Weiss LJ, Blustein J., Faithful patients: the effect of long‐term physician‐patient relationships on the costs and use of health care by older Americans. Am J Public Health. 1996;86(12):1742‐1747. 10.2105/AJPH.86.12.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gill JM, Mainous AG III. The role of provider continuity in preventing hospitalizations. Arch Fam Med. 1998;7(4):352‐357. 10.1001/archfami.7.4.352. [DOI] [PubMed] [Google Scholar]
- 13. Mainous AG, Gill JM. The importance of continuity of care in the likelihood of future hospitalization: is site of care equivalent to a primary clinician? Am J Public Health. 1998;88(10):1539‐1541. 10.2105/AJPH.88.10.1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Okinawa Prefecture . Okinawa remote islands: population; 2017. Available at: http://www.pref.okinawa.jp/site/kikaku/chiikirito/ritoshinko/documents/ixtusyousaisinn.pdf. Accessed July 3, 2018.
- 15. Motomura K. Reflective practice and situated learning in remote medicine. An Off J Japan Prim Care Assoc. 2012;35(2):165‐167. [Google Scholar]
- 16. Okinawa Prefecture . Okinawa remote islands: living environment; 2017. Available at: http://www.pref.okinawa.jp/site/kikaku/chiikirito/ritoshinko/documents/eyonn.pdf. Accessed July 3, 2018.
- 17. Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2016;39:238‐247. [DOI] [PubMed] [Google Scholar]
- 18. Kaneko M, Motomura K, Mori H, et al. Gatekeeping function of primary care physicians under Japan's free‐access system: a prospective open cohort study involving 14 isolated islands. Fam Pract, cmy084. 2018. Available at: 10.1093/fampra/cmy084. [Epub ahead of print]. Accessed November 26, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Okinawa Prefecture. Population based on basic resident register; 2016. Available at: http://www.pref.okinawa.jp/site/kikaku/shichoson/2422.html. Accessed July 3, 2018.
- 20. Aoki T, Inoue M, Nakayama T. Development and validation of the Japanese version of Primary Care Assessment Tool. Fam Pract. 2016;33(1):112‐117. 10.1093/fampra/cmv087. [DOI] [PubMed] [Google Scholar]
- 21. Shi L, Starfield B, Xu J. Validating the adult primary care assessment tool. J Fam Pract. 2001;50(2):161‐175. [Google Scholar]
- 22. Aoki T, Inoue M. Primary care patient experience and cancer screening uptake among women: an exploratory cross‐sectional study in a Japanese population. Asia Pac Fam Med. 2017;16(1):3 10.1186/s12930-017-0033-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Aoki T, Miyashita J, Yamamoto Y, et al. Patient experience of primary care and advance care planning: a multicentre cross‐sectional study in Japan. Fam Pract. 2017;34(2):206‐212. 10.1093/fampra/cmw126. [DOI] [PubMed] [Google Scholar]
- 24. Takuya A, Yosuke Y, Tatsuyoshi I, et al. Effect of patient experience on bypassing a primary care gatekeeper: a multicenter prospective cohort study in Japan. J Gen Intern Med. 2017;33(5):722‐728. 10.1007/s11606-017-4245-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Peduzzi P, Concato J, Kemper E, Holford TR, Feinstem AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373‐1379. 10.1016/S0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- 26. Kaneko M, Matsushima M, Irving G. The ecology of medical care on an isolated island in Okinawa, Japan: a retrospective open cohort study. BMC Health Serv Res. 2017;17(1):37 10.1186/s12913-017-1979-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Edwards A, Evans R, White P, Elwyn G. Experiencing patient‐experience surveys: a qualitative study of the accounts of GPs. Br J Gen Pract. 2011;61(585):157‐166. 10.3399/bjgp11X567072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pohontsch NJ, Hansen H, Schäfer I, Scherer M. General practitioners’ perception of being a doctor in urban vs. rural regions in Germany: a focus group study. Fam Pract. 2018;35(2):209‐215. 10.1093/fampra/cmx083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Brundisini F, Giacomini M, DeJean D, Vanstone M, Winsor S, Smith A. Chronic disease patients’ experiences with accessing health care in rural and remote areas: a systematic review and qualitative meta‐synthesis. Ont Health Technol Assess Ser. 2013;13(15):1‐33. [PMC free article] [PubMed] [Google Scholar]
- 30. Roland M, Elliott M, Lyratzopoulos G, et al. Reliability of patient responses in pay for performance schemes: analysis of national General Practitioner Patient Survey data in England. BMJ. 2009;339(7727):955 10.1136/bmj.b3851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Okinawa Prefecture. Population movement report; 2017. Available at: http://www.pref.okinawa.jp/toukeika/estimates/2017/annual/top.html. Accessed July 3, 2018.
- 32. Paddison C, Elliot M, Parker R, et al. Should measures of patient experience in primary care be adjusted for case mix? Evidence from the English General Practice Patient Survey. BMJ Qual Saf. 2012;Aug 21(8):634‐640. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1. Characteristics of the 5 Islands Included in This Study


