Abstract
The aim of this work is to trace how rheumatologists all over Egypt are approaching the COVID-19 pandemic and what changes it has brought about in the patients’ care with special attention to its effect on vulnerable rheumatic disease (RD) patients. This survey further aims to help inform the rheumatology community about the changes in practice during the COVID-19 pandemic. The survey included 26 questions distributed to University staff members across Egypt members of the Egyptian College of Rheumatology (ECR). It takes 5–10 min to fill out. The practice setting of participating rheumatologists included University Teaching Hospitals that are the main rheumatology and clinical immunology service providers for adults and children RD patients. There was an overall agreement across the country in the responses to the survey that took a median time of 7 min to fill in. Potential changes in rheumatology outpatient practice by staff members evolved since the COVID-19 pandemic. None of the university rheumatology staff members has prescribed chloroquine or HCQ to prevent or treat COVID-19 in a non-hospitalized patient who was not previously on it. Twenty-three recommended decrease/avoid NSAIDs if the RD patient had confirmed COVID-19 or symptoms. There is an agreement to the key emerging frontline role of rheumatologists in treating COVID-19. During the pandemic, RD cases requiring admission were dealt with by several modified strategies. The overall agreement among the different university rheumatology departments during such critical situation has provoked the ECR to consider providing provisional guidelines for dealing with RD patients during this global catastrophe.
Keywords: Rheumatologists, Practice, Survey, COVID-19 pandemic, Egyptian college of rheumatology
Introduction
Coronavirus disease-2019 (COVID-19) is a universal pandemic as declared by the World Health Organisation [1]. Human mankind is susceptible to being infected with severe acute respiratory syndrome–coronavirus 2 (SARS‐CoV2). The virus will keep on spreading until an effective vaccine exists or herd immunity is established. Sheltering individuals at risk may successfully slow down the spread of the virus and minimize mortalities [2]. The emerging increase in patients’ volume has exposed defects in healthcare systems and challenged the capacity to provide optimal patient care and adequate safety measures to healthcare providers [3]. COVID-19 is not only threatening the resilience of national health systems, but certainly raises questions about the world’s political and financial economic future [4]. The immune system plays a crucial role during COVID-19 supported by the diminished antiviral cytokine type I interferon, increased pro-inflammatory cytokines such as interleukin-6 (IL-6), dysregulation of Th1 and Th2 lymphocytes response and the striking lymphopenia observed at different disease stages [5]. The diverse clinical presentation of COVID-19 includes manifestations which can mimic rheumatic diseases (RDs) [6] or a flare [7]. Moreover, the pandemic may shape the treatment strategy of complex RDs [8]. It is paramount that continued clinical care of patients with chronic RDs who require hydroxychloroquine (HCQ) maintenance treatment must proceed [9].
The strength and in-depth of rheumatology practice in Egypt and focused interest in managing certain RDs differs from one centre of excellence to another. As in many other countries, there is an increasing shortage of rheumatologists per population with an uneven distribution across the nation being concentrated and focused in the capital and main cities [10]. With the swiftly escalation of cases worldwide, to slow the disease spread, the Egyptian ministry of health (MOH) implemented a vast spectrum of measures that had a massive impact on the medical practice and on the university teaching hospitals. The government applied a complete lockdown of international flights and a daytime curfew [11]. Similarly, in Australia, universities moved to online teaching and meetings, closed clinics, cancelled elective surgery, redistributed staff and postponed rheumatology exams [12]. What will come in the future is whether patients with COVID-19 are at risk of developing an autoimmune RD. Viral infections are known triggers of autoimmunity [13, 14] and data on SARS-CoV-2 are just waiting to get out of the box. In spite of the downward trend of new cases in many countries due to the anti-epidemic measures and the public awareness and efforts of the health care workers, the end of this crisis is far from sight. RD patients require special attention and consideration, yet much remains unknown [15].
The aim of this work is to trace how rheumatologists all over Egypt are approaching the COVID-19 pandemic and what changes it has brought about in the patients’ care with special attention to its effect on vulnerable RD patients. This survey further aims to help inform the rheumatology community about the changes in practice during the COVID-19 pandemic.
Materials and methods
The survey included 26 questions distributed by emails (using the Microsoft Network; msn web portal) to University staff members across Egypt representing 27 Rheumatology or Internal Medicine (Rheumatology Division) Departments from 20 universities and authorizations that include 600 rheumatology staff members. Participating staff were also members of the Egyptian College of Rheumatology (ECR). It takes 5−10 min to fill out. Some questions were adapted from the Hospital for Special Surgery and Weill Cornell Medicine, New York City, USA [16] that was also uploaded on the Rheumatology group on Facebook which is the largest in the specialty with 20,000 plus members from more than 100 countries. The questions included in the survey are in English language and presented in Appendix 1. The areas covered by the survey include questions that assess the rheumatology staff members’ perspectives, from universities across the nation, on the impact of the pandemic on the socioeconomic status and awareness of the patients (9 questions), difficulties facing RD patients regarding their daily living and medications (3 questions) and the experienced changes in their practice (14 questions). The survey was designed so as to be easily filled in by the participating staff member. In an attempt to validate the survey, a pilot test was run and a revision of the survey design, content, terminologies, comprehension and easiness to fill-in was performed. For questions 1–12, a response (frequency or degree of agreement) of 5 is chosen, for questions 14−18 a yes or no response was provided. The questions were mostly close-ended (only the last 2 were open-ended) and the response was according to the mentioned instructions. Answers were recorded by receiving the filled in survey and transferring them into an excel sheet. A written consent was provided by the participating Rheumatology University staff members. The study questionnaire/survey conforms to the local ethical committees of the corresponding universities. The author contributions are in line with the International Committee of Medical Journal Editors (ICMJE 4) authorship criteria. All co-authors take full responsibility for the integrity of the study and the final manuscript.
The results were statistically analysed and findings presented as number and percentage. Chi-Square and ANOVA tests were performed to compare 2 or more groups respectively. p < 0.05 was considered significant.
Results
The practice setting of participating rheumatologists included University Teaching Hospitals that are the main rheumatology and clinical immunology service providers as well as variable private practice clinics. All the centers provide treatment to Egyptian adults and children RD patients. The results of the survey are presented in Table 1 and there is an overall agreement in the responses to the survey among rheumatology university staff members across the country. The median time to fill in the survey was 7 min.
Table 1.
Responses to the questionnaire survey for changes in rheumatology practice among university rheumatology staff members
| During COVID-19 pandemic n (%) | Frequency of university rheumatology staff members response to rheumatology practice survey (n = 27) | p | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| What is the frequency of RD patients that: | < 5 | 5–10 | > 10–25 | > 25–50 | > 50 | DK | |||||
| Rely on free/insurance treatment | 0 (0) | 0 (0) | 7 (25.9) | 4 (14.8) | 13 (48.1) | 3 (11.1) | < 0.0001 | ||||
| Are below the poverty line | 0 (0) | 3 (11.1) | 4 (14.8) | 10 (37) | 8 (29.6) | 2 (7.4) | 0.001 | ||||
| Are food insecure | 1 (3.7) | 5 (18.5) | 10 (37) | 6 (22.2) | 2 (7.4) | 3 (11.1) | 0.013 | ||||
| Have a low health awareness | 0 (0) | 1 (3.7) | 5 (18.5) | 10 (37) | 11 (40.7) | 0 (0) | < 0.0001 | ||||
| Have no access to telemedicine | 6 (22.2) | 3 (11.1) | 7 (25.9) | 3 (11.1) | 5 (18.5) | 3 (11.1) | 0.54 | ||||
| Discuss their COVID-19 risk | 5 (18.5) | 4 (14.8) | 2 (7.4) | 3 (11.1) | 11 (40.7) | 1 (3.7) | 0.003 | ||||
| Discuss their medications | 4 (14.8) | 2 (7.4) | 6 (22.2) | 1 (3.7) | 14 (51.9) | 0 (0) | < 0.0001 | ||||
| Stop/reduce DMARD without advice | 11 (40.7) | 6 (22.2) | 1 (3.7) | 3 (11.1) | 0 (0) | 6 (22.2) | < 0.0001 | ||||
| Can’t obtain CQ/HCQ due to shortage | 1 (3.7) | 1 (3.7) | 2 (7.4) | 4 (14.8) | 18 (66.7) | 1 (3.7) | < 0.0001 | ||||
| Degree of agreement to the following statements: | Strongly agree | Agree | Neutral | Disagree | Strongly disagree | ||||||
| RD patients are high risk to COVID-19 | 3 (11.1) | 12 (44.4) | 5 (18.5) | 7 (25.9) | 0 (0) | 0.001 | |||||
| The pandemic reduced biologics use | 5 (18.5) | 11 (40.7) | 3 (11.1) | 8 (29.6) | 0 (0) | 0.001 | |||||
| The pandemic reduced steroids use | 1 (3.7) | 8 (29.6) | 8 (29.6) | 10 (37) | 0 (0) | < 0.0001 | |||||
| Changes in rheumatology outpatient practice included: | Defer new | Defer FU | Urgent only | Remote consults | Social media | None | |||||
| 6 (22.2) | 12 (44.4) | 17 (63) | 9 (33.3) | 24 (88.9) | 1 (3.7) | < 0.0001 | |||||
| As a rheumatology staff member do you: | Yes | No | Other | ||||||||
| Prescribe HCQ/CQ to prevent COVID-19 | 0 (0) | 27 (100) | – | ||||||||
| Prescribe HCQ/CQ to treat COVID-19 | 0 (0) | 27 (100) | – | ||||||||
| Avoid NSAIDs even with no COVID-19 | 7 (25.9) | 19 (70.4) | 1 (3.7) | (Stop only ibuprofen) | – | ||||||
| Avoid NSAIDs with confirmed COVID-19 | 23 (85.2) | 2 (7.4) | 2 (7.4) | (Could not decide) | – | ||||||
| Support a frontline role for rheumatologists | 24 (88.9) | 3 (11.1) | – | ||||||||
| With missing HCQ, instruct patients to: | Stop it | Replace | Reduce dose | ||||||||
| 21 (77.8) | 7 (25.9) | 4 (14.8) | – | ||||||||
| Patients facing difficult access to medications other than HCQ due to: | Fear of infection | Nobody to get it | Pharmacy | Financial constraint | None | ||||||
| Closed | Vacant | ||||||||||
| 7 (25.9) | 5 (18.5) | 0 (0) | 5 (18.5) | 12 (44.4) | 15 (55.6) | < 0.0001 | |||||
| Socioeconomic concerns for RD patients include: | Living alone | Living with elderly | Limited internet | Lost jobs | Limited medicare | Limited transport | |||||
| 14 (51.9) | 22 (81.5) | 17 (63) | 22 (81.5) | 24 (88.9) | 19 (70.4) | 0.02 | |||||
| RD patients do worse due to which of the following when they are of: | Illiteracy | Flares | RD | COVID | Not worse | Other | |||||
| Morbidity/mortality | |||||||||||
| Lower socioeconomic status | 24 (88.9) | 15 (55.6) | 20 (74.1) | 19 (70.4) | 1 (3.7) | 1 (3.7) | < 0.0001 | ||||
| Rural origin | 23 (85.2) | 14 (51.9) | 15 (55.6) | 14 (51.9) | 4 (14.8) | 0 (0) | < 0.0001 | ||||
| Which RD patients suffer most: | SLE | RA | SpA | OA | SSc | BD | Vasc | Gout | Ped | Other | |
| 26 (96.3) | 15 (55.6) | 5 (18.5) | 0 (0) | 9 (33.3) | 4 (14.8) | 14 (51.9) | 0 (0) | 2 (7.4) | 3 (11.1) | < 0.0001 | |
Bold values are significant at p < 0.05
COVID-19 coronavirus disease 2019, DK Doesn’t know, DMARD disease modifying antirheumatic drug, CQ/HCQ chloroquine/hydroxychloroquine, RD rheumatic disease, FU follow up, NSAIDs non-steroidal anti-inflammatory drugs, SLE systemic lupus erythematosus, RA rheumatoid arthritis, SpA spondyloarthritis, OA osteoarthritis, SSc systemic sclerosis, BD Behcets disease, Vasc. vasculitis, Ped. pediatric
Changes in rheumatology outpatient practice by staff members since the COVID-19 pandemic, involved spacing the visits and including a lower number of patients even while practicing in their private clinics, which continued to serve in view of the remarkable shutdown of university hospital services for regular cases. Patients were also directed to adapt their visits in accordance to the strictly applied governmental curfew times.
None of the university rheumatology staff members has prescribed chloroquine (CQ) or HCQ to prevent or treat COVID-19 in a non-hospitalized patient who was not previously on it. For patients taking non-steroidal anti-inflammatory drugs (NSAIDs) for their RD, 19 did not recommended a decrease or stop of NSAIDs when there were no COVID-19 symptoms; seven advised a decrease/stop, while one advised to stop only Ibuprofen. However, 23 recommended to decrease/avoid NSAIDs if the RD patient had confirmed COVID-19 or symptoms while two supported to continue.
There is an agreement to the key emerging frontline role of rheumatologists in treating COVID-19 patients due to the presence of cytokine storm and relevant skin rashes with potential response to few rheumatology drugs.
When the regimen of the RD patients needed HCQ and was missing, the patients were told to stop it and continue on the rest of his/her treatment by 21 and were also told to replace it by CQ or another disease modifying anti-rheumatic drug (DMARD) by seven. Another suggestion presented by four included a dose reduction of HCQ for those who had a previous stock.
Regarding the access to medications other than CQ/HCQ, 15 reported that the patients had no difficulty while seven reported that patients are not going to pick up their medications for fear of getting COVID-19 and five mentioned that they did not have someone to get their medications for them. Although none reported a shutdown of pharmacies, running out of medications was reported by five. Financial constraints due to loss of employment and insurance during the pandemic were considered a chief trouble facing the RD patients and were reported by 12. Another reported complexity was the lack of medical reports provided for newly diagnosed cases to receive medications through governmental hospitals.
The socioeconomic concerns for RD patients were chiefly the poor access to medical care, followed in descending frequency by losing their jobs due to the pandemic, living with an elderly person, limited transportation and internet access as well as living alone. The presence of co morbidities as diabetes and interstitial lung disease (ILD) were considered additional risk factors affecting the socioeconomic status of the RD patients.
The RD patients who have a lower socioeconomic status or being of rural origin will do worse in the context of the pandemic most frequently due to lack of education or misinformation, due to an increased morbidity or mortality from COVID-19 if they get infected, due to an increased frequency or severity of flares, while one and four were in favor that the RD patients with lower status or of rural origin respectively may not do worse. It has been further suggested that during the pandemic there is a tendency to a decreased performance of the charity societies with limited donations and resources towards the RD patients.
On considering the different RDs, patients with the following disease were considered as the most suffering: systemic lupus erythematosus (SLE) by 26, rheumatoid arthritis (RA) by 15, vasculitis by 14, systemic sclerosis (SSc) by 9, spondyloarthritis (SpA) by 5, Behçets disease (BD) by 4 and pediatric RDs by 2. RDs associated with ILD were considered the most vulnerable by 2 and 1 suggested with macrophage activating syndrome (MAS) (Fig. 1).
Fig. 1.
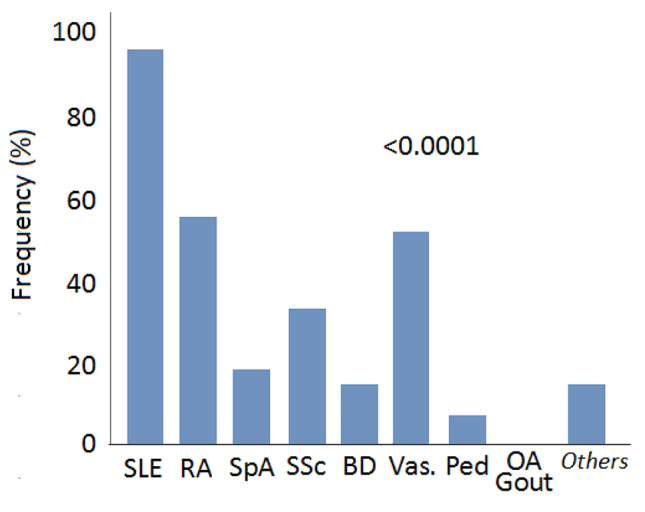
The frequency of rheumatic diseases patients suffering most during the coronavirus disease 2019 (COVID-19) pandemic
During the pandemic, RD cases requiring admission were dealt with by several modified strategies. Most of the university hospitals were only receiving emergency cases, many inpatient departments were adapted to serve the COVID-19 crisis and many Rheumatology wards were closed or admitted only severe and special cases. The period of stay was planned to be as short as possible with effective decision taking at the first stage of contact with the patient. Ultra short stay was arranged for those receiving certain biologic or IV DMARD therapy. Pediatric RD cases were admitted to general wards and remote contact with the parents was implemented. Meanwhile in order to secure the performance of the university rheumatology staff members the least effective number were managing the cases while wearing personal protective equipments (PPEs). It is noteworthy that throughout the university rheumatology wards, no cases were found to be positive for COVID-19. Very few RD cases with mild symptoms were suspected and completely recovered on monitoring. All elective procedures were postponed such as arranging for renal biopsies, diagnostic and therapeutic musculoskeletal ultrasound and capillaroscopy. Spacing of outpatient visits for follow up was adopted and many patients chose not to visit hospitals and clinics for non-serious conditions.
One of the hotspots of COVID-19 infection is Alexandria and although the measures and rules enforced by the government are optimum and strict yet the incompliance of the society is a major limitation to halting the spread of the infection. The impact of COVID-19 infection in the governorates of the Delta is moderate with a tendency to a steady rise. The affected economic status has an obvious role on the insecurely applied preventive measures by the patients in Northern governorates and another key problem leading to an additional COVID-19 burden is the influx of many citizens and even residents from Italy following the catastrophic outbreak. Hospitals from Ismailia, a city with a relatively low disease spread, are receiving positive cases for isolation from other governorates. The pattern of affection in the capital city, Cairo, is difficult to delineate especially as many residents are originally from other governorates. More endorsement of running diagnostic tests to healthcare professionals as applied to workers and employees in various companies and factors may aid in controlling the spread. It has been noticed that the pandemic may have started in Egypt by the end of 2019 before there was enough international recognition of the outbreak. There is a tendency to an increasing number of positive cases in Beni-Suef compared to the neighbor governorate Fayoum with the rising responsibility in dealing with the pandemic at the University hospitals there. As with other governorates from Upper Egypt, the economic drawbacks were more obviously hitting. The COVID-19 affection in Aswan, the popular southern touristic destination, is diverse as many reported cases include foreigners during their trips. Whether there is a certain pattern or gradient of affection across the country governorates remains to be further analysed in later studies.
Discussion
The state of RD patients under the COVID-19 pandemic is concerning with the possibility of respiratory failure when infected. In many RDs, proinflammatory cytokines, interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α) and IL-1 are central in the pathogenic process and may also be accountable for the tissue damage in multiple organs in patients with COVID-19 [7].
Many of the rheumatology patients on immunosuppressants are at higher risk of impaired viral clearance and severe COVID-19 [15]. Long-term use of steroids and immunosuppressives may also increase the risk of infection. A mutual impact of COVID-19 and RDs is likely [7] yet their relationship is complex [6]. The cytokine storm is only the tip of the iceberg and in order to add to the current knowledge of rheumatologists on the inflammatory milieu in the course of COVID-19, rheumatology experts should integrate in the cutting edge leading teams [5]. However, rheumatologic patients may be unexpectedly protected, by virtue of the medications used to control their disease [15].
Most aspects of rheumatology practice and teaching have changed since the onset of the COVID-19 pandemic [12]. In a similar survey for neurologists practice, a noteworthy variability in preparedness and responsiveness to the COVID-19 pandemic was demonstrated, impacted by region, health care setting and practice model [3]. The concept of “treat-to-target” should be stressed in order to identify the right therapy for the right patient [5].
Most of rheumatology staff members agreed that most of the RD patients have low health awareness during the COVID-19 pandemic, although the Egyptian government has taken major steps to educate the public and limit the spread of the disease. Knowledge was significantly lower among elder, illiterate, lower socioeconomic and those from rural areas [17].
The frequency of patients that do not have access to telemedicine varied across the governorates. The global crisis has limited physical consultation and minimized healthcare access. Teleconsultation allowed for an adjunctive role in mild conditions to the comfort of patient's homes thus limiting the risk of exposure of both the physician and patient [18]. Hydroxychloroquine, an essential treatment for many RD patients, is gaining widespread attention as a potential treatment for COVID-19. Rapid dissemination of over interpreted data has potential consequences mainly for those RD conditions for which HCQ has demonstrated benefits in preventing organ damage and life-threatening disease flares [19]. In the present survey, more than 50% of the patients would discuss the COVID-19 risk and medications while the majority reported that < 5% of the RD patients would stop or reduce the dose of their DMARD without medical advice. In the USA, more than 50% of RD patients described a significant disruption to their rheumatology care including postponed appointments, self-imposed or physician-directed changes to mediations [20].
In the present work, all university rheumatology staff agreed that they would not prescribe HCQ to prevent or treat COVID-19. However the majority reported that most of the patients can't obtain HCQ/CQ due to shortage. Much controversy has arisen regarding the potential benefit of HCQ in the treatment or prevention of COVID-19 [19–21]. In a huge recent study on COVID-19 patients treated by HCQ/CQ, it was not possible to confirm their benefit on in-hospital outcomes. HCQ did not reduce the risk of death among hospitalised patients with this new disease.[22]. After high or moderate risk exposure to COVID-19, HCQ did not prevent illness or confirmed infection [23]. Rheumatologists must join the scientific community and support the recommendation that any use of HCQ to treat COVID-19 must be limited to the hospital and/or ICU settings. Off-label use should be prohibited as there is no current evidence that HCQ can prevent SARS-CoV2 infection [9]. In Italy, the third most infected country worldwide, RD patients being treated with HCQ did not develop any symptoms suggestive of COVID-19 and was well tolerated. The immunomodulatory properties of HCQ may contribute to the suppression of the cytokine storm syndrome (CSS) [21].
In the present survey, more than 50% consider RD patients at a higher risk of COVID-19 while the rest disagreed or were neutral. Adult and pediatric patients with RDs on targeted biologic and synthetic DMARDs do not seem to present a higher risk of COVID-19 or a more severe disease outcome when compared to the general population [22]. Many agreed to reduce the use of biologics during the pandemic. May be this is also due to the inability to receive it properly during the country shutdown. However, there is a disagreement that the pandemic reduced the dose of steroids used. Interestingly, many of the therapies that are currently under exploration in clinical trials to treat the CSS associated with COVID-19 are immunomodulatory agents frequently used to treat a variety of RDs [24]. Thus, biologics used by RD patients may spare them a CSS in the setting of COVID-19 [25]. It is reasonable that reserving the immune system in better balance allows for a more effective overall host response. It is preferable that RD patients remain on their current therapies, but to withhold immunosuppressives in the setting of confirmed COVID-19 infection [26]. An early course of corticosteroid, specifically methylprednisolone, at the onset of dyspnoea, was found to attenuate progression to the hyper-inflammation phase that requires escalation of care in patients with COVID-19 [27].The right decision regarding the existing therapy of RD patients remains unsettled, yet factors such as the underlying disease status, comorbidities, individual treatments, and combinations of therapies will affect the outcome. Until then, basic general strategies including social distancing, hand washing, wearing a mask etc., will benefit RD patients considerably [25, 28].
In this survey, most of the rheumatology staff members would enhance the remote contact of patients via social media platforms and allow only for urgent cases to be physically examined. There was an increasing tendency to postpone follow up and new RD cases. Similarly in Italy the national legal briefs were to postpone the non-urgent out-patients rheumatologic visits in order to allow more space and time in taking care of COVID-19 patients [13]. It has been reported that the attendance of the rheumatology clinics dropped by 15–30% after the outbreak while rheumatology patients typically require frequent follow-up visits to ensure disease control and to monitor therapy [15].
Rheumatologists would contact the patients by telephone to estimate their standing, severity and urgency of their condition when an appointment was already scheduled. Similar to the situation in Egypt, the grand challenge was with patients waiting for their first clinical examination as a remote appointment may not give a picture of the full scenario [13].
The survey response was in favor of avoiding NSAIDs in confirmed cases but not if there are no COVID-19 infection. Ibuprofen or renin-angiotensin system inhibitors could worsen COVID-19 by activating the SARS-CoV-2 access receptor, angiotensin-converting enzyme-2. NSAIDs should be used at the least effective dose for the shortest possible period [29] when needed for COVID-19 patients. Paracetamol remains the first line analgesic antipyretic. Opioids, with the potential for respiratory depression should be carefully prescribed in COVID-19 patients. When steroids are necessary, patients should continue to receive them [30].
There is a growing body of evidence supporting a potential role of rheumatologists on the front line which is in agreement to the perspective of most of the responses to the survey. The considerable knowledge and long expertise concerning RD drugs currently being tested in the treatment of COVID-19 such as CQ, HCQ, tocilizumab, Jak1 inhibitors and anti-IL-1, ideally place rheumatologists on the frontlines in the search for possible solutions [4] and in understanding the mechanisms underlying this disease [5]. As rheumatologists are aware of immune imbalance and cytokines among their patients, they can champion the screening for, and diagnosis of, CSS among hospitalized COVID-19 patients [11]. Rheumatologists must advocate strongly for continued access to HCQ for valid clinical indications [9].
With the striking shortage of HCQ available for RD patients to use for controlling their diseases, most of the rheumatologists considered stopping the drug with no change in the rest of the regimen while almost a quarter would advice to replace it by another DMARD. A smart suggestion, for those with a predetermined stock, was to reduce the dose. Rheumatologists anticipate challenges in clinical care and must counsel patients about the appropriate use of HCQ in the management of RDs, provide valid scientific information regarding evidence for effect in COVID-19, and be ready to provide alternative drug treatment in the event that HCQ may be allocated away from routine rheumatology clinical care to treat seriously ill viral-infected patients. Furthermore, the shortage of HCQ forms a possible ethical dilemma [9].
Most of the patients did not find difficulty to access the DMARDs other than HCQ/CQ. However, those facing obscurity were mostly reported to be due to financial constraints during the pandemic. While patients on immunosuppressives are thought to be at higher risk of severe illness related to COVID-19. Drugs used to treat RDs [31] are also being employed to manage complications of COVID-19 [32] so the ultimate impact on patients risk is unclear [20].
Among the socioeconomic concerns for RD patients, limited access to medical healthcare, lost jobs and living with elderly showed the highest impact. Limited access to transportation and internet service were additional obstacles. In agreement, difficulties in the accessibility of technology and patients’ illiteracy majorly limited the feasible way out via telemedicine [13].
In this survey, illiteracy, comorbidities and flare are among the main causes for a worse outcome of RD patients especially those of low socioeconomic status and of rural origin. Although not mentioned among the reported causes for a RD patient to do worse, physical inactivity during social isolation adds to the cardiovascular burden [33].
The SLE, RA and vasculitic patients were considered the most vulnerable to suffer during the pandemic. In a study from a hotspot area in Italy, 6/67 Takayasu arteritis (TA) patients could not receive their infliximab infusions due to the national lockdown and had to be switched to adalimumab, two were referred to local nearby hospitals and two had their infusions temporarily postponed due to clinical stability. Also 13/67 TA and 11/95 giant cell arteritis (GCA) patients had symptoms or a close contact with a positive case. However another two with TA and two with GCA were positive for COVID-19. All four cases fully recovered and background immunosuppression did not negatively impact on COVID-19 course. The latest EULAR recommendations against routinely stopping or reducing medications in RD patients are supported [34]. Pediatric RD cases among the Egyptian rheumatology staff members were considered the least to suffer during the pandemic. In agreement, an encouraging report from Italy found that none of the 123 pediatric rheumatology patients (primarily juvenile idiopathic arthritis) on background biologic therapy had either confirmed or suspected COVID-19 [25]. The immune systems of children and adults are different,both with respect to their composition and functional responsiveness and children have a qualitatively different response to the SARS-CoV2 virus. The reasons for this mild COVID-19 disease in children remain elusive [2]. Adult and paediatric patients with RD on biologics do not seem to present a higher risk of COVID-19 or a more severe disease outcome when compared to general population [35].
Immune-mediated multi-organ diseases such as IgG4-related disease with an associated ILD or MAS are at risk of COVID-19 infection [36]. ILD is commonly seen in RA, primary Sjögren’s syndrome (pSS), SSc and dermatomyositis. A differential diagnosis should be made to identify the origin of interstitial lesions. Respiratory failure is more common in RD patients infected with COVID-19 and discrimination from a disease flare should be considered [7].
In Egypt, during the pandemic RD cases requiring admission were dealt with by several modified strategies as most of the university hospitals were only receiving emergency cases, many inpatient departments were adapted to serve the COVID-19 crisis. The shortest effective period of stay was considered for all inpatients. As in Italy [13], patients receiving intravenous treatment at hospitals were postponed. Otherwise, treatments were maintained during pandemic as most immunosuppressives are lifesaving. Inpatient consultations were continued yet the different allocation of the hospital beds and the fear of some patients to even drive to a hospital may have reduced the effective number of hospitalized patients with RDs [13].
According to official reports May,2020 by the WHO Egypt [37], Cairo and Giza have been on top of the list of confirmed COVID-19 cases followed by Alexandria, Qalubia, Menoufia, Damietta, Luxor, Beni-Suef, Gharbia, Aswan, Qena and Dakahlia. Then comes Beheira, Port Said, Fayoum and Red Sea, An even lower affection was reported from Sharkia Kafr El-Sheikh, Assuit and Minia. The least reports came from Sohag, South Sinai with almost no cases from Matrouh, New Valley, Ismailia and Suez. As numbers are dynamically changing on daily basis such sequence and reports could change. RD patient-oriented outcomes and behavioural changes during COVID-19 infection are not sufficiently captured [20].
As the end to the COVID-19 spread is unanticipated, therapeutic regulation is needed for the management of RD patients to avoid added risk [8]. The increased susceptibility to the COVID-19 serious complications, make it indispensable to provide a roadmap to Egyptian rheumatologists.
During a pandemic, practice guidelines are needed to improve protection for physicians and their patients, endorse recommended changes, readiness for managing COVID-19, optimize future awareness for any pathogens with pandemic potential and counteract the negative impact on the patients quality of life [3, 38].
The improved understanding of the host antiviral responses may help develop safe and effective immunotherapeutic strategies against COVID-19 in the foreseeable future [39]. There is an urgent need to develop a SARS-CoV-2 vaccine that may prevent further seasonal outbreaks of the infection [40].
This leading piece of work presents an overview on the Egyptian rheumatologists' practice during the emergence of the COVID-19 pandemic that may help narrow the gaps in daily clinical practice when dealing with similar extra-ordinary situations. The low sample size of contributing university staff members may seem as a limitation to this study, however, participants effectively and adequately represented all Egyptian universities and governorates of a heavily populated nation during this global critical state.
The responses presented in this survey could change over time as the highly dynamic situation and guidelines for the COVID-19 crisis evolve. The overall agreement among the different university rheumatology departments during such critical situation has provoked the Egyptian College of Rheumatology (ECR) to undertake this responsibility and provide provisional guidelines for dealing with RD patients during this global catastrophe. Egyptian Rheumatology staff members will continue to work, teach and treat RD patients and keep on modifying the approach while learning from the evolving experience of other high spot countries such as China, Italy, Spain the UK and the United States.
Acknowledgment
The authors would like to thank Dr. Bella Mehta, MBBS, MS—Rheumatology, Internal Medicine, Hospital for Special Surgery, New York-Presbyterian University Hospital and Weill Cornell Medical College, for offering the outlines for some of the adapted questions included in the survey. Coronavirus disease 2019 (ECR COVID-19) Study Group, Egyptian College of Rheumatology.
Appendix 1
Questionnaire survey for changes in rheumatology practice among university rheumatology staff members
For questions 1–9, select the most appropriate frequency (< 5%, 10–25%, 25–50%, > 50% or don’t know) in response to the proposed questions:
What frequency of the RD patients:
1. Rely on the medical insurance and medications provided by university hospitals?
2. Are considered below the poverty line?
3. Are considered food insecure as a result of the pandemic?
4. Have low health awareness and info?
5. Do not have access to telemedicine visits to contact the physicians?
6. Have contacted you to discuss their COVID-19 risk in the context of their RD?
7. Have contacted you to discuss their medications in the context of COVID-19?
8. Have discontinued/reduced (without medical advice) at least one immunosuppressive to alleviate their risk for COVID-19?
9. Have been unable to obtain their regular HCQ/CQ due to shortages?
For questions 10–12, select the most appropriate agreement response (strongly agree, agree, neutral, disagree, and strongly disagree) to the mentioned statements:
10. Patients with rheumatic diseases are at a higher risk of COVID-19 irrespective of their immunosuppressive medications.
11. The pandemic has directed the rheumatologists to reduce the use/dosage/frequency of biologics.
12. The pandemic has directed the rheumatologists to reduce the use/dosage/frequency of corticosteroids.
Select all that apply to question.
13. How did the rheumatology outpatient practice change since the pandemic?
New patients’ appointments were postponed.
All follow-up visits were postponed.
Only urgent cases were seen in-person.
Appointments were switched to remote telehealth/video consultations.
Using social media platforms as WhatsApp and Facebook.
There was no change.
Other (please specify).
For questions 14–18 select a yes or no response and specify if there is another answer.
14. Have you prescribed HCQ/CQ to prevent COVID-19, for a non-hospitalized patient who was not previously on it?
15. Have you prescribed HCQ/CQ to treat COVID-19, in a non-hospitalized patient who was not previously on it?
16. For patients taking NSAIDs for RDs, are you recommending they decrease and/or avoid NSAIDs when they have no COVID-19 symptoms?
17. For patients taking NSAIDs for rheumatic diseases, are you recommending they decrease and/or avoid NSAIDs when they have confirmed COVID-19 or symptoms?
18. Is there an emerging role for rheumatologists in treating COVID-19 patients due to the presence of the cytokine storm, the relevant skin rashes and the potential response to few rheumatology drugs?
19. When HCQ was missing, the regimen for the RD patients was modified by instructing the patients to stop it and continue on the rest of the treatment or to replace it by another drug? (Specify the replacement drug and mention if there were any further modifications).
20. Do the RD patients have problems with access to their medications other than HCQ/CQ, because of the pandemic? (select all that apply)
- Yes: not going to receive the medications for fear of getting COVID-19.
- Not having someone to get their medications for them.
- Pharmacies shutting down.
- Pharmacies running out of medications.
- Financial constraints (loss of employment/ insurance) during the pandemic.
No.
Other (please specify).
21. What are the concerns for the RD patients (if any) regarding their socioeconomic status? (select all that apply)
They live alone.
They are living with an elderly person.
They have poor access to technology/ internet.
They have lost their employment due to COVID-19.
They have restricted access to medical care.
They have limited access to transportation.
No, this doesn’t apply to our RD patients.
Other (please specify).
22. In the context of the pandemic, would RD patients do worse if they had a lower socioeconomic status? (select all that apply)
- Yes due to:
- Lack education or have misinformation.
- Increased frequency or severity of flares.
- Increased morbidity or mortality from their underlying disease.
- Increased morbidity or mortality from COVID-19 if they get infected.
No, they may not do worse.
Other (please specify).
23. In the context of the pandemic, would RD patients do worse if they come from rural areas? (select all that apply)
- Yes due to:
- Lack education or have misinformation.
- Increased frequency or severity of flares.
- Increased morbidity or mortality from their underlying disease.
- Increased morbidity or mortality from COVID-19 if they get infected.
No, they may not do worse.
Other (please specify).
24. Patients of which RD are suffering most: SLE, RA, SpA, OA, SSc, BD, vasculitis, Gout, pediatric cases or others (specify)? (select all that apply). Mention in brief the chief underlying reasons.
25. How did the COVID-19 affect those rheumatic disease patients requiring admission?
26. How heavily did the COVID-19 affect your governorate in view of the estimated daily positive cases?
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Compliance with ethical standards
Conflict of interest
None.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tamer A. Gheita, Email: gheitamer@hotmail.com, Email: gheitamer@kasralainy.edu.eg
Mohamed N. Salem, Email: mnabil2011@yahoo.com
Nahla N. Eesa, Email: nahlanaeem@gmail.com, Email: nahla.ali@kasralainy.edu.eg
Noha M. Khalil, Email: nohakhalil78@hotmail.com
Nada M. Gamal, Email: drnadagamal80@gmail.com
Rasha Abdel Noor, Email: rashaabdelnoor@med.tanta.edu.eg.
Abdel Hafeez Moshrif, Email: dr.moshrif@live.com.
Rawhya El Shereef, Email: rawhyaelshereef@yahoo.com.
Faten Ismail, Email: faten_ismail70@yahoo.com.
Nermeen Noshy, Email: nermeennoshyaziz@gmail.com.
Rasha M. Fawzy, Email: dr.rasha.fawzy@hotmail.com
Emad Elshebini, Email: emadelshebini@gmail.com.
Iman Khalifa, Email: iman.khalifa@hotmail.com.
Hanan El Saadany, Email: hanan0777@hotmail.com.
Samar Tharwat, Email: samartharwat2000@mans.edu.eg.
Amany El-Najjar, Email: elnajjaramany@gmail.com.
Yousra Abdel Fattah, Email: yousrahashim@gmail.com.
Rehab Sallam, Email: rehabsallam@hotmail.com.
Amany S. El-Bahnasawy, Email: d_amy75@yahoo.com
Ola Gharbia, Email: dr_ola_gharbia@hotmail.com.
Eman Hassan, Email: emanhassan96@yahoo.com.
Amira ElShanawany, Email: amira.pmrheum@gmail.com.
Eman F. Mohamed, Email: emydr@ymail.com
Soha Senara, Email: senara.soha@yahoo.com.
Mervat Ismail, Email: miaa_a11@yahoo.com.
Samah I. Nasef, Email: dr.samah.ismaeel@gmail.com
Ahmed M. Abdalla, Email: ahmed.mos10@gmail.com
Dina Elessawi, Email: dinaelessawi@hotmail.com.
Samar M. Fawzy, Email: samarfawzy1@yahoo.com
Esam Abu Alfadl, Email: abualfadl71@yahoo.com.
Asmaa Khalifa, Email: ahmed_elsaman@med.sohag.edu.eg.
Nouran M. Abaza, Email: nouranabaza@hotmail.com
References
- 1.World Health Organisation. WHO Director-General’s opening remarks at the media briefing on COVID-19. 11 March 2020. 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 2.Brodin P. Why is COVID-19 so mild in children? Acta Paediatr. 2020;109(6):1082–1083. doi: 10.1111/apa.15271. [DOI] [PubMed] [Google Scholar]
- 3.Sharma A, Maxwell CR, Farmer J, Greene-Chandos D, LaFaver K, Benameur K. Initial experiences of US neurologists in practice during the COVID-19 pandemic via survey. Neurology. 2020 doi: 10.1212/WNL.0000000000009844. [DOI] [PubMed] [Google Scholar]
- 4.Marotto D, Sarzi-Puttini P. What is the role of rheumatologists in the era of COVID-19? Autoimmun Rev. 2020;19(6):102539. doi: 10.1016/j.autrev.2020.102539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferro F, Elefante E, Baldini C, Bartoloni E, Puxeddu I, Talarico R, et al. COVID-19: the new challenge for rheumatologists. Clin Exp Rheumatol. 2020;38(2):175–180. [PubMed] [Google Scholar]
- 6.Kucharz EJ. Should coronavirus disease 2019 concern rheumatologists? Pol Arch Intern Med. 2020 doi: 10.20452/pamw.15366. [DOI] [PubMed] [Google Scholar]
- 7.Ye C, Cai S, Shen G, Guan H, Zhou L, Hu Y, et al. Clinical features of rheumatic patients infected with COVID-19 in Wuhan, China. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ragni E, Mangiavini L, Viganò M, Brini AT, Peretti GM, Banfi G, et al. Management of osteoarthritis during COVID-19 pandemic. Clin Pharmacol Ther. 2020 doi: 10.1002/cpt.1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scuccimarri R, Sutton E, Fitzcharles M. Hydroxychloroquine: a potential ethical dilemma for rheumatologists during the COVID-19 pandemic. J Rheumatol. 2020;47(6):783–786. doi: 10.3899/jrheum.200369. [DOI] [PubMed] [Google Scholar]
- 10.Gheita TA, Eesa NN. Rheumatology in Egypt: back to the future. Rheumatol Int. 2019;39(1):1–12. doi: 10.1007/s00296-018-4192-0. [DOI] [PubMed] [Google Scholar]
- 11.Gheita TA, Kenawy SA. Egypt’s groundwork blessing during the COVID-19 pandemic curse: rheumatologic experience. Eur J Rheumatol. 2020 doi: 10.5152/eurjrheum.2020.2058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cai K, He J, Wong PKK, Manolios N. The impact of COVID-19 on rheumatology clinical practice and university teaching in Sydney, Australia. Eur J Rheumatol. 2020 doi: 10.5152/eurjrheum.2020.20060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perricone C, Gerli R. Being a rheumatologist and a patient with a rheumatic disease today: a perspective at the time of COVID-19. Eur J Rheumatol. 2020 doi: 10.5152/eurjrheum.2020.2057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Qiu CC, Caricchio R, Gallucci S. Triggers of autoimmunity: the role of bacterial infections in the extracellular exposure of lupus nuclear autoantigens. Front Immunol. 2019;10:2608. doi: 10.3389/fimmu.2019.02608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.So H, Mok CC (2020) COVID-19 and rheumatic diseases: practical issues. J Clin Rheumatol Immunol 1–4
- 16.COVID-19 rheumatology physician survey hospital for special surgery, New York-Presbyterian University Hospital and Weill Cornell Medical College. https://www.surveygizmo.com/s3/5533802/COVID-19-Rheumatology-Physician-Survey
- 17.Abdelhafiz AS, Mohammed Z, Ibrahim ME, Ziady HH, Alorabi M, Ayyad M et al (2020) Knowledge, perceptions, and attitude of Egyptians towards the novel coronavirus disease (COVID-19). Community Health 1–10 [DOI] [PMC free article] [PubMed]
- 18.Sharma A, Jindal V, Singla P, Goldust M, Mhatre M (2020) Will Teledermatology be the silver lining during and after COVID-19? Dermatol Ther e13643. doi: 10.1111/dth.13643 (epub ahead of print) [DOI] [PMC free article] [PubMed]
- 19.Kim AHJ, Sparks JA, Liew JW, Putman MS, Berenbaum F, Duarte-Garcia A, et al. A rush to judgment? Rapid reporting and dissemination of results and its consequences regarding the use of hydroxychloroquine for COVID-19. Ann Intern Med. 2020;172(12):819–821. doi: 10.7326/M20-1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sirotich E, Dillingham S, Grainger R, Hausmann JS. COVID-19 Global Rheumatology Alliance Steering Committee. Capturing patient-reported outcomes during the COVID-19 pandemic: Development of the COVID-19 global rheumatology alliance patient experience survey. Arthritis Care Res (Hoboken). 2020 May 9; epub ahead of print. doi: 10.1002/acr.24257.21 [DOI] [PMC free article] [PubMed]
- 21.Vastarella M, Patrì A, Annunziata MC, Cantelli M, Nappa P, Tasso M, et al. Can hydroxychloroquine be useful in the prevention of COVID-19? An Italian survey in dermatological and rheumatological patients already under treatment. J Am Acad Dermatol. 2020;83(1):e77–e79. doi: 10.1016/j.jaad.2020.04.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Randomised Evaluation of COVid-19 thERapY (RECOVERY) Trial on hydroxychloroquine. No clinical benefit from use of hydroxychloroquine in hospitalised patients with COVID-19: Statement from the Chief Investigators of the RECOVERY trial on hydroxychloroquine. 2020 June 5; https://www.recoverytrial.net/files/hcq-recovery-statement-050620-final-002.pdf
- 23.Boulware DR, Pullen MF, Bangdiwala AS, Pastick KA, Lofgren SM, Okafor EC, et al. A randomized trial of hydroxychloroquine as postexposure prophylaxis for Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMoa2016638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Henderson LA, Canna SW, Schulert GS, Volpi S, Lee PY, Kernan KF, et al. On the alert for cytokine storm: immunopathology in COVID-19. Arthritis Rheumatol. 2020;72(7):1059–1063. doi: 10.1002/art.41285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cron RQ, Chatham WW. The question of whether to remain on therapy for chronic rheumatic diseases in the setting of the covid-19 pandemic. J Rheumatol. 2020 doi: 10.3899/jrheum.200492. [DOI] [PubMed] [Google Scholar]
- 26.Ceribelli A, Motta F, De Santis M, Ansari AA, Ridgway WM, Gershwin ME, et al. Recommendations for coronavirus infection in rheumatic diseases treated with biologic therapy. J Autoimmun. 2020;109:102442. doi: 10.1016/j.jaut.2020.102442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fadel R, Morrison AR, Vahia A, Smith ZR, Chaudhry Z, Bhargava P, et al. Early short course corticosteroids in hospitalized patients with COVID-19. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grech V. Unknown unknowns—COVID-19 and potential global mortality. Early Hum Dev. 2020;144:105026. doi: 10.1016/j.earlhumdev.2020.105026. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 29.Zolk O, Hafner S, Schmidt CQ, German Society for Experimental and Clinical Pharmacology and Toxicology (DGPT) COVID-19 pandemic and therapy with ibuprofen or renin-angiotensin system blockers: no need for interruptions or changes in ongoing chronic treatments. Naunyn Schmiedebergs Arch Pharmacol. 2020;393(7):1131–1135. doi: 10.1007/s00210-020-01890-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tan SHS, Hong CC, Saha S, Murphy D, Hui JH (2020) Medications in COVID-19 patients: summarizing the current literature from an orthopaedic perspective. Int Orthop 1–5 [DOI] [PMC free article] [PubMed]
- 31.Centers for Disease Control. Coronavirus Disease 2019 (COVID-19): at risk for severe illness. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/groups-at-higher-risk.html Accessed 23 May 2020
- 32.Zumla A, Hui DS, Azhar EI, Memish ZA, Maeurer M. Reducing mortality from 2019-nCoV: host-directed therapies should be an option. Lancet. 2020;395(10224):e35–e36. doi: 10.1016/S0140-6736(20)30305-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peçanha T, Goessler KF, Roschel H, Gualano B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am J Physiol Heart Circ Physiol. 2020;318(6):H1441–H1446. doi: 10.1152/ajpheart.00268.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tomelleri A, Sartorelli S, Campochiaro C, Baldissera EM, Dagna L. Impact of COVID-19 pandemic on patients with large-vessel vasculitis in Italy: a monocentric survey. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Michelena X, Borrell H, López-Corbeto M, López-Lasanta M, Moreno E, Pascual-Pastor M, et al. Incidence of COVID-19 in a cohort of adult and paediatric patients with rheumatic diseases treated with targeted biologic and synthetic disease-modifying anti-rheumatic drugs. Semin Arthritis Rheum. 2020;50(4):564–570. doi: 10.1016/j.semarthrit.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen Y, Dong Y, Cai S, Ye C, Dong L. Clinical characteristics of IgG4-RD patients infected with COVID-19 in Hubei, China. Semin Arthritis Rheum. 2020;50(4):559–563. doi: 10.1016/j.semarthrit.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization in Egypt (2020) Distribution of confirmed COVID-19 cases in the Egyptian governorates. May 1 2020; https://www.saudi24.news/2020/05/a-document-for-world-health-reveals-the-distribution-of-corona-injuries-in-egypt-politics-news.html
- 38.Zomalheto Z, Assogba C, Dossou-yovo H (2020) Impact of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) infection and disease -2019 (COVID-19) on the quality of life of rheumatoid arthritis patients in Benin. The Egyptian Rheumatologist (epub ahead of print) [DOI] [PMC free article] [PubMed]
- 39.Gasparyan AY, Misra DP, Yessirkepov M, Zimba O. Perspectives of immune therapy in coronavirus disease 2019. J Korean Med Sci. 2020;35(18):e176. doi: 10.3346/jkms.2020.35.e176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Misra DP, Agarwal V, Gasparyan AY, Zimba O. Rheumatologists’ perspective on coronavirus disease 19 (COVID-19) and potential therapeutic targets. Clin Rheumatol. 2020;39(7):2055–2062. doi: 10.1007/s10067-020-05073-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


