Abstract
Rationale & Objective
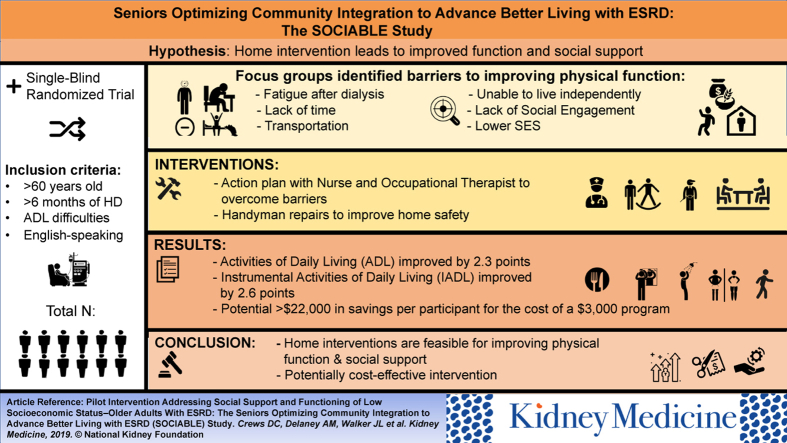
Older adults with end-stage kidney disease have increased morbidity, fatigue, and decreased physical function, which can inhibit self-care and social engagement. We pilot tested a home-based program to improve physical and social functioning of low socioeconomic status older adults treated with hemodialysis (HD).
Study Design
Qualitative study and randomized waitlist control intervention.
Setting & Participants
Older adult HD patients in Baltimore, MD.
Interventions
We identified functional needs and home environmental barriers to social engagement through focus groups; mapped findings onto aspects of an established program, which includes home visits with an occupational therapist, nurse, and handyman to provide ≤$1,300 worth of repairs, modifications, and devices; and piloted the program (Seniors Optimizing Community Integration to Advance Better Living with ESRD [SOCIABLE]) among 12 older adult HD patients. We delivered the services over 5 months in a staggered fashion.
Outcomes
Feasibility and acceptability of the intervention and change in disability scores.
Results
Focus group themes included fatigue, lack of social support, and desire to live independently. SOCIABLE pilot participants were recruited from 2 dialysis units and all were African American (50% men); mean age was 69 years. At baseline, the mean disability score for activities of daily living (ADLs) was 4.4 and for instrumental ADLs (IADLs) was 6.3 (both out of a possible 16). Among the 9 participants alive at follow-up, there was 100% intervention completion and outcomes assessment. All treated participants improved a mean score of 2.3 for ADL and 2.6 for IADL disability, and social support and social network scores improved by 4.8 and 4.6, respectively.
Limitations
Small sample size; all participants were African American.
Conclusions
A home-based intervention addressing physical and social functioning of low socioeconomic status older adults on HD therapy was feasible and acceptable.
Index Words: Disability, dialysis, socioeconomic status, home environment, social engagement, older adults, activities of daily living, qualitative study
Graphical abstract
Editorial, p. 3
Older adults with end-stage renal disease (ESRD) experience increased morbidity,1 life-constraining fatigue,2 and decreased physical function3 compared with their counterparts without ESRD. The World Health Organization’s International Classification of Functioning, Disability and Health conceptualizes a person’s level of functioning as a dynamic interaction between their health conditions, environment factors, and personal factors.4 In the case of older adults with ESRD, many live in poverty5 and confront housing and other environmental barriers that exacerbate limitations in physical function. The pervasive physical fatigue can inhibit self-care and social engagement (the extent to which an individual participates in a broad range of social roles and relationships6). Physical function is intertwined with environmental risk in this population because people with low socioeconomic status (SES) may have difficulty navigating their homes due to inadequate stairs or banisters, uneven flooring, and lack of adaptive tools. These barriers to optimal functioning may limit older adults’ ability to “age in place,” as opposed to being placed in a nursing or assisted living facility.
Multiple studies document that social support is associated with better health and functional outcomes in ESRD,7, 8, 9, 10 yet there have been few intervention studies aimed at improving the social support,11, 12 social engagement, or physical functioning13, 14, 15 of persons with ESRD. Among older adults especially, such interventions have the potential to support aging in place, reduce hospitalizations, and potentially increase home dialysis and transplantation consideration.
We previously developed and tested a program called Community Aging in Place, Advancing Better Living for Elders (CAPABLE)16, 17 for low-income older adults with physical function limitations. CAPABLE is a home-based program that includes visits with an occupational therapist, nurse, and handyman to provide ≤$1,300 worth of repairs, modifications, and devices to support physical function. This dollar amount has been found to be sufficient to provide an average of 14 small modifications and items for the home and for activities.18 In testing CAPABLE, we noted a particular need and potential benefit of the program for people with ESRD. Therefore, we proceeded to: (1) conduct focus groups of patients with ESRD to understand their needs and perceptions of CAPABLE and how best to improve their physical and social functioning, and (2) pilot the intervention among 12 older adults with ESRD to gauge feasibility and acceptability. We present our 2-stage process and findings.
Methods
Stage 1: Focus Groups of Older In-Center Hemodialysis Patients
We performed 2 focus groups of older adult in-center hemodialysis (HD) patients treated in Baltimore, MD. We followed the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist.19
Participant Selection
Participants were eligible to participate if they were 60 years or older; English speaking; with ESRD treated with in-center HD for at least 6 months at a facility in Baltimore, MD; and with limitations in physical function (difficulty in at least 1 of the following: bathing, dressing, walking across a room, grooming [referring to things done personally to ensure a clean and neat appearance], getting on or off the toilet, and getting on or off the bed) and low SES (less than high school education, unemployment, and/or household income <$25,000 per year).
Participants were identified through advertisement to prior CAPABLE participants with ESRD and direct recruitment at an outpatient dialysis facility (DaVita J.B. Zachary). The protocol was approved by the Johns Hopkins University Institutional Review Board (IRB00097283) and DaVita Clinical Research and was adherent to the Declaration of Helsinki. Participants provided written consent and were compensated $50 for their time.
Data Collection
The focus group question guide was developed based on literature review and our prior work. Two separate guides were used: one for prior CAPABLE participants (to determine what aspects of the program they believed would be particularly helpful for patients with ESRD) and another for those who had not previously participated (Item S1). Questions focused on: (1) knowledge and beliefs about participants’ health and functional status, (2) their needs, and (3) acceptable interventions for supporting their physical and social functioning. Both focus groups were facilitated by the same trained moderator (L.L.B.) and attended by a note taker (J.S.). We audiorecorded the sessions and had them professionally transcribed verbatim by an outside company. Two focus groups were held, one at Johns Hopkins and one at DaVita J.B. Zachary dialysis center.
Data Analysis
Using thematic analysis, T.K.M.C. and J.L.W.T. manually coded the transcripts line by line to identify concepts that were inductively derived from the data. Similar codes were grouped into themes. Themes were then reviewed, discussed, and revised with input from D.C.C. and S.L.S. until agreement was reached. Representative quotes that corresponded to the emergent themes were selected for inclusion in the article.
Stage 2: Piloting the Intervention
Themes from the focus groups were then used to inform our pilot study, SOCIABLE (Seniors Optimizing Community Integration to Advance Better Living with ESRD). As in CAPABLE, we were guided by multiple frameworks.20 Our overarching framework was the Society to Cells Resilience Framework,21 which posits that intervening on more than 1 socioecologic domain (ie, physiologic, individual, and built environment) leads to more lasting effects on individual resilience (physical and psychological) than intervening on 1 domain. Second, that resilience can be fostered at critical times in the life course, such as following HD therapy initiation. Third, that people are resilient at any stage of life and can become stronger and more able even with multiple chronic conditions.21 Thus, we piloted an intervention that addressed multiple domains (including the individual and the home environment) and was aimed at fostering resilience in the context of ESRD and other chronic conditions.
Study Design
We pilot tested SOCIABLE in a single-blind, 2-group, randomized, feasibility trial conducted at participants’ homes in the Baltimore, MD, area. At enrollment, participants were randomly assigned to treatment or control (usual care). Using a waitlist design, the control group received the intervention after serving as controls. Our outcome assessor was masked to randomization assignment. Visits occurred between March 2016 and March 2017. The study protocol was approved by Johns Hopkins and was adherent to the Declaration of Helsinki. All participants provided written informed consent. The study was registered at ClinicalTrials.gov (NCT03055273).
Participant Selection
A sample size of 12 was chosen based on available resources. Eligibility was the same as in stage 1 (focus groups). Potential participants were identified among persons who participated in our focus groups (but who had not previously been in CAPABLE) and by recruitment at MedStar Good Samaritan Hospital dialysis unit from a list of potentially eligible participants provided by the medical director. After providing informed consent, participants were randomly assigned in a 1:1 ratio to the intervention (immediate) and control (delayed) groups. Participants were compensated $25 at both baseline and follow-up.
Intervention
We conducted a 5-month structured program delivered by an occupational therapist, who made up to 6 visits to each participant; a nurse, who made up to 5 visits; and a handyman, who contributed up to a full day’s work providing home repairs and making home modifications. Participants worked with the occupational therapist and nurse to identify 3 achievable goals per discipline and examined barriers to achieving those goals. For example, for a goal of being able to go out to a social event, barriers could include muscle weakness, difficulty dressing, and lack of handrails to get safely down the outside stairs. The handyman then made structural improvements, repairing the railing, so the participant could overcome the barrier of getting down the steps. The nurse worked on exercises to improve muscle strength. The occupational therapist taught energy conservation techniques and supplied assistive devices so the individual could get dressed without fatigue. Example approaches for different goals are detailed in Item S2.
Occupational Therapist
In the first 2 visits, the occupational therapist conducted a semistructured clinical interview16 to help participants identify and prioritize functional goals. For each goal, the occupational therapist observed the participant’s performance of the relevant activity. In addition, the occupational therapist assessed the home for safety issues such as decrepit flooring, poorly lit stairs, and loose carpet. The participant and the occupational therapist identified environmental repairs, modifications, and assistive devices that would help achieve their goals. The occupational therapist then created a work order for the handyman prioritized by the participant’s goals and within the $1,300 budget for each participant’s home.22
In the remaining 4 visits, the occupational therapist used motivational interviewing and action planning techniques (on which they were trained) to discuss with the participant ways to achieve their goals. For example, these could involve trying new techniques with equipment that SOCIABLE provided or practicing to gain stamina. In the last visit, the occupational therapist and participant reviewed the goals and discussed how the participant might apply strategies they had found useful to address future challenges.22
Registered Nurse
In the registered nurse’s first visit, she used a semistructured interview to help the participant identify and prioritize goals related to pain, depression, social networks/isolation, strength and balance, medication management, or communication with medical providers.23 If the nurse identified medication issues such as timing of blood pressure medications causing dizziness, the nurse obtained participant permission and communicated the issue with the primary care provider and/or nephrologist.23 In the subsequent 4 visits, the nurse and participant planned incremental actions to address each of the participant’s goals and refined strategies based on incremental changes the participant made between visits. For example, if the participant’s goal was to improve mood, the nurse and participant might decide to try having the participant do simple Otago exercises,24 cook together with their spouse, and address the cramping after dialysis that affected the participant’s mood.
In the final visit, the nurse reviewed strategies that participants found effective and helped them consider ways to use what they learned to address future challenges.23 Finally, the nurse wrote a letter to the primary care provider and nephrologist summarizing the participant’s goal achievements.
Handyman
The handyman was given the work order from the occupational therapist and then made a preliminary visit to the participant’s home. Within 3 weeks, the handyman performed up to a full day’s work, such as adding a railing to external stairs, moving and tacking down loose wires, or installing grab bars in the bathroom.
Outcome Measures
In this pilot study, our primary outcome of interest was the feasibility and acceptability of the intervention to inform a future full-scale trial. Feasibility was assessed through examination of our recruitment and completion rates. We also examined participants’ acceptance of the intervention(s) and a limited set of intervention outcomes. Because of the study design, the time points varied in meaning for the 2 groups. At baseline, 5 months (which was postintervention for those randomly assigned to immediate treatment and was after serving as control for the intervention group), and 10 months (posttreatment for those who waited), we administered psychometrically validated measures of physical functioning, social networks, and social functioning.
Function was assessed by self-reported difficulty and need for help in performing 8 essential activities of daily living (ADLs): walking across a small room, bathing, upper and lower body dressing, eating, using the toilet, transferring in and out of bed, and grooming. Functioning on each task was classified from 0 to 2 depending on whether the person did not have difficulty in the prior month and did not need help (0), had not needed help but had difficulty (1), or needed help regardless of difficulty (2). A summary score for the 8 items was developed by Katz et al25 and ranges from 0 to 16. The score predicts future morbidity.26
Instrumental ADLs (IADLs) were assessed by self-report of difficulty on 8 items: using the telephone, shopping, preparing food, light housekeeping, washing laundry, traveling independently, taking medications independently, and managing finances independently. The response category for each task ranged from 0 to 2: did not have difficulty in the prior month and did not need help (0), did not need help but had difficulty (1), or needed help regardless of difficulty (2). The score ranged from 0 to 16.
We also assessed dialysis-specific questions related to ADLs and IADLs, including “Does going to dialysis interfere with any of the above activities? If so, which ones?” and “Do you feel tired on the day of dialysis?” Social networks were assessed using a modified Lubben Social Network Scale-Revised.27 Received support and satisfaction/negative interactions with support were assessed using the Krause and Borawski-Clark scale.28
Statistical Analysis
Participant characteristics were described using descriptive statistics. Mean values and standard deviation were used to estimate the outcome measures’ total scores pre- and postintervention. Analyses were conducted using STATA, version 15.1 (StataCorp LP).
Results
Stage 1: Focus Groups of Older In-Center HD Patients
A total of 15 eligible patients were identified, and 7 agreed to participate. Our first focus group included 2 patients (1 man and 1 woman), and the second included 2 men and 3 women (total n = 7). All focus group participants were African American. Key emergent themes and representative quotations are summarized in Table 1. Themes included desire to live independently, fatigue, lack of social support, social engagement, coping, employment impact, and acceptable/unacceptable interventions.
Table 1.
Selected Participant Quotations for Key Themes Identified in Focus Groups of Older Adults on Hemodialysis and With Functional Limitations
| Theme | Quotations | Group |
|---|---|---|
| Desire to Live Independently | ||
| Avoid nursing home | “It took every ounce of mental energy that I had to get out of that nursing home… I just don’t want to go back. And I can’t stand it, I couldn’t stand it. And I thought it was going to kill me. Where you have no independence. It’s, you’re at their beck and call for everything. Even when you don’t want to eat, for an example, you’re stuck.” M, FG1 | 1 |
| Fatigue | ||
| Dialysis days | “My challenge is getting up in the morning, trying to prepare for that day, when I have dialysis. And that means that my time is limited. And sometimes I feel like I want to fix breakfast and sometimes I don’t. I might look around and see that I have to clean the kitchen and I don’t do it. The bedroom need to be made up; I don’t have the energy to do it and I don’t want to do it. I just want to hurry up and get out so I have to go to dialysis, so I can get there on time, so I can get back. Maybe finish up what I left. So after dialysis I am, I feel like I’m not tired until I actually leave. That’s when it starts. I feel sometimes I get a little shaky and a little bit off balance, but then I just rest. That’s my main thing, I have to rest. Once I’m rested up, I’m okay, and then I have enough energy to clean my kitchen and that’s it. And then I’m through for the night.” F, FG1 | 1 |
| Lack of Social Support | ||
| Family | “Family members, I’ll start there. Naturally, they really don’t understand the disease. As you talk about it with them, they’re busy trying to tell you what they done heard from other people. That gets on your nerves. Try and explain to them that that’s not the way it is with me. And they, then after they get their little opinion in and their point in, they become a little disinterested. They don’t really care. They kind of like, they distance themselves, and they do it, they try to do it in different ways. And I can tell, because you don’t hear from them as often as you did at first.” F, FG1 “…like when I need to go shopping and get food and just go look for some clothes if I want to, or be asked to taken somewhere, I have to hear a whole spiel. That kind of stuff bothers you. I shouldn’t have to explain to you what I want— And they want you to explain it, why this and that, and how long it will take, all that kind of stuff. So then, you say, hey, I don’t need that. I don’t need that. So you depend on your other services to help you get through.” F, FG1 |
1 |
| Social Engagement | ||
| Going out | “I haven’t been nowhere all winter, all spring, and maybe I can get out this summer. There’s just so [much] happening going on. It just makes me just stay home.” M, FG2 “I do get out when I feel like it, and use to go to church every Sunday, but I go when I feel like going and they know how I am.” F, FG2 “I went to the beach for Memorial Day.” F, FG2 |
2 |
| Isolation from friends | “I don’t have the friends I used to have. Well, once I got sick, and I couldn’t get out there like I used to, and then when I could get myself together to get out there, I really didn’t want no bother. Because I was sort of like embarrassed, believe it or not. I just didn’t want nobody to know what was going on.” M, FG2 “Because they already, they done judged your illness and you, too. So, and with friends, I might have one or two good friends that really understand what’s happening, but they too have their limits. And so, I narrow it down to maybe one person.” F, FG1 |
1, 2 |
| Coping | ||
| Maintaining joy | “Don’t let nobody take your joy. Now, I’m the type of person that have joy all the time, because I asked God for peace, and God gave me peace, no matter what. And I just thank and praise God for everything.” F, FG2 | 2 |
| Employment Impact | ||
| Inability to work | “See now that’s the one thing that I missed. Not working and not being around people, because I did, I used to work at… And I was used to being around people and doing and things like that. But I could not keep my job because of the timeframe. You couldn’t get there on time.” F, FG2 | 2 |
| Acceptable/Unacceptable Interventions | ||
| Handyman services | “I’m in the senior building and everything’s on one floor and the bathroom is nice and wide. I don’t have a bathtub; it’s a shower though. And that I feel could be improved. You know, I really don’t like the way the shower is… I would put a bar in there, so I can grip myself when I come in. And the kind of shower I have is the kind you have, it’s like a nozzle and you have to operate with your hand, rather than have the sprout [sic] that I like, that I could adjust it down there like that. If I had that, it would be better.” F, FG2 “I don’t want nothing changed. Like I’m saying, I don’t need the handy man, because I don’t want nothing changed in my house. I mean, in my house, I’ve been there so long, everything, half the stuff I put in there myself. So I don’t want nobody tinkering with it. See I know electrical, plumbing, what else do you got, carpentry, a little bit. So I mean, when something broke in my house, I took care of it.” M, FG2 |
2 |
| Goal setting | “I was saying I would like to walk again on my own. Without help… I like to do things on my own. And then when I do them, sometimes it works out, sometimes it don’t. But mostly it works out. I got sick, and I got like, as I came out the hospital, I got weak and couldn’t walk. That’s it.” F, FG2 | 2 |
Abbreviations: F, female; FG1(2), focus group 1(2); M, male.
Participants generally believed that individuals on dialysis therapy face more challenges when compared with their counterparts who are not on dialysis therapy. They identified fatigue after dialysis, transportation for getting to and from places, and time needed to prepare for daily activities as barriers to their self-care and social engagement. Several participants noticed changes in their receipt of social support and social interactions following dialysis therapy initiation. Some thought that family members distanced themselves, whereas others isolated themselves because they did not want to be bothered or felt embarrassed asking for help. Many felt isolated due to the strenuous dialysis schedule or the time required to prepare to go out into the community.
Participants also noted some difficulty managing their health conditions. A few indicated having trouble communicating with their physician(s) about managing their health conditions. Participants identified the bathroom as a potential hazard for falling due to issues with getting in and out of the shower and challenges with using the shower head. In addition, climbing up steps and the limited amount of space in senior housing created higher risk for bumping into furniture or falling. Within the theme of acceptable/unacceptable interventions, most participants thought that if they were given the opportunity to create their own health goals, it would increase their motivation to achieve them. All participants were interested in having an occupational therapist come into their home; however, some expressed resistance to having home nurse and handyman services.
Stage 2: Piloting the Intervention
Recruitment was completed in less than 1 month. Five participants were enrolled from our focus groups and 7 were enrolled from a dialysis facility to achieve our prespecified target of 12 participants. Among those alive at the end of the study, we had 100% intervention completion and outcomes assessment (Fig S1)
Participants had a mean age of 68.7 years. All were African American. Mean ADL and IADL disability scores at enrollment were 4.4 and 6.3, respectively. Among the 7 participants who reported years on dialysis therapy, the mean time was estimated at 5 years.
Six participants each were assigned to the intervention (immediate) and control (delayed) groups (Table 2). In the intervention (immediate) group, improvements in all measures were observed following the intervention (from 0 to 5 months) and were more favorable than for measures of the control (delayed) group assessed at the same point (5 months). In the control (delayed) group, 3 participants died while waiting to receive the intervention. For the 3 who completed the intervention, improvements in all outcome measures were observed at 10 months (Tables 3 and 4; Fig S2). Overall, combining immediate and delayed groups, participants improved a mean of 2.3 ADLs and 2.6 IADLs on the respective physical functioning scales (meaning that the level of disability decreased; improvements of at least 1 are considered clinically significant29), and social support and social network scores improved by 4.8 and 4.6, respectively.
Table 2.
Baseline Characteristics of SOCIABLE Participants, by Treatment Group
| Characteristic | Control (delayed) (N = 6) | Intervention (immediate) (N = 6) |
|---|---|---|
| Age,a y | 68.6 (7.8)a | 69.5 (4.6) |
| African American race | 6 (100%) | 6 (100%) |
| Male sex | 3 (50%) | 4 (66.7%) |
| ≥High school education | 3 (50%) | 4 (66.7%) |
| ADL disability scale score | 3 (1-11) | 2.5 (0-12) |
| IADL disability scale score | 6 (2-10) | 5.5 (3-10) |
Note: n = 12. Values expressed as mean (standard deviation), number (percent), or median (range).
Abbreviations: ADL, activities of daily living; IADL, instrumental activities of daily living; SOCIABLE, Seniors Optimizing Community Integration to Advance Better Living with ESRD.
Of 5 participants.
Table 3.
Outcome Comparisons for SOCIABLE Intervention and Control Groups
| Intervention (immediate) Group |
Control (delayed) Group |
|||||
|---|---|---|---|---|---|---|
| Baseline Score (n = 6) | Score at 5 mo Postintervention (n = 6) | Difference | Baseline Score (n = 3)a | Score at 5 mo Postintervention (n = 3)a | Difference | |
| ADL disability score (higher = worse) | 4.8 ± 5.3 | 2.0 ± 3.03 | −2.8 ± 3.7 | 2.0 ± 1.7 | 0.7 ± 1.2 | −1.3 ± 0.6 |
| IADL disability score (higher = worse) | 6.3 ± 3.1 | 3.8 ± 3.06 | −2.5 ± 1.9 | 6.0 ± 7.2 | 3.3 ± 3.2 | −2.7 ± 4.04 |
| Social Support and Satisfaction score (higher = greater) | 43.8 ± 10.5 | 46.5 ± 10.3 | 2.7 ± 7.2 | 35.3 ±17.2 | 44.3 ± 19.4 | 9.0 ± 7.2 |
| Social Network score (higher = larger network) | 19.8 ± 10.5 | 24.7 ± 9.5 | 4.8 ± 4.6 | 15.7 ± 5.9 | 20.0 ± 9.0 | 4.3 ± 5.9 |
Note: Data presented as mean ± standard deviation.
Abbreviations: ADL, activities of daily living; IADL, instrumental activities of daily living; SOCIABLE, Seniors Optimizing Community Integration to Advance Better Living with ESRD.
n = 3 at baseline and postintervention for the control (delayed) group due to 3 deaths occurring before the group received the intervention.
Table 4.
Raw Scores for SOCIABLE Intervention and Control Groups
| Group/Participant No. | ADL |
IADL |
Social Network |
Social Support/Satisfaction |
||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |
| Intervention (immediate) | ||||||||
| 1 | 1 | 0 | 3 | 0 | 26 | 24 | 50 | 55 |
| 3 | 11 | 8 | 10 | 9 | 0 | 7 | 29 | 27 |
| 6 | 12 | 2 | 10 | 4 | 24 | 32 | 53 | 55 |
| 8 | 3 | 1 | 7 | 5 | 27 | 34 | 49 | 46 |
| 10 | 2 | 1 | 4 | 2 | 16 | 25 | 50 | 48 |
| 12 | 0 | 0 | 4 | 3 | 26 | 26 | 32 | 48 |
| Control (delayed) | ||||||||
| 2 | 1 | 0 | 14 | 7 | 18 | 29 | 54 | 61 |
| 4 | 4 | 2 | 4 | 2 | 9 | 11 | 20 | 23 |
| 7 | 1 | 0 | 0 | 1 | 20 | 20 | 32 | 49 |
Abbreviations: ADL, activities of daily living; IADL, instrumental activities of daily living; SOCIABLE, Seniors Optimizing Community Integration to Advance Better Living with ESRD.
Discussion
We conducted focus groups among low-SES older adults treated with HD and with limitations in physical function and identified key themes of fatigue, lack of social support, and the desire to live independently. We then pilot tested in the ESRD population a home-based intervention and noted subsequent improvements in measures of physical and social functioning. Our results suggest that home-based interventions of this kind are feasible and acceptable and can lead to favorable outcomes in this vulnerable population.
Fatigue is a major challenge for HD patients and was identified as a high-priority symptom for which patients desire innovations in therapeutic options.30 Although there is currently no standardized outcome measure for fatigue in HD patients,31 approaches such as our study, which address both the person and their environment, might offer a means to meaningfully reduce symptoms. Energy conservation techniques, such as those taught by our occupational therapist, might be particularly impactful for HD patients.
Our focus group participants discussed a strong desire to live independently, underscoring the importance of efforts to improve the functional status of this population. While our pilot intervention participants had been on dialysis therapy for about 5 years, a study of 97 primarily independent adults 80 years or older (78% living independently) found that >30% had functional loss requiring caregiver support or nursing home transfer within 6 months following dialysis therapy initiation. At 1 year, only 23% of this cohort was living independently.32
Although our pilot intervention was not designed to examine statistical significance between groups, the improvement in ADLs and IADLs is similar to results from prior CAPABLE studies that were adequately powered.16, 17 These show a more than 7 times return on investment in subsequent savings, including >$22,000 to Medicare per participant for the cost of a $3,000 program.33 Because older adults on dialysis therapy have high hospitalization and nursing home use,34 the savings for older adults with ESRD may be even greater.
Our study had limitations. Our focus group and pilot phases both included small samples, including 1 group with only 2 participants. There was also some overlap between focus group and pilot participants (with 5 focus group participants later participating in the pilot). Participants in the focus groups may have been sensitized to find the pilot intervention acceptable. We also used a waitlist/delayed intervention design, which facilitates recruitment because study teams can promise that each participant will receive the intervention, but this design limits the ability to examine long-term impacts (not relevant in this feasibility pilot). Other study designs, including those using an attention control group to mitigate the impact of social desirability bias, should be tested. In addition, all participants in our study were African American. While this in part likely reflects the overrepresentation of African Americans among patients with ESRD,1 our findings may not generalize to all dialysis populations. Also, our study population included only established older adult HD patients, several of whom had survived more than 5 years on dialysis therapy. New HD patients may face different challenges and targeting them in interventions such as this might prevent some of the hospitalizations common in the early months following HD therapy initiation.34 Finally, in our pilot study, we did not assess the intervention’s impact on several key patient-reported outcomes in ESRD, including quality of life and depressive symptoms, which should be assessed in a full-scale trial.
Strengths of our study include our focus on major challenges facing older adult HD patients and our efforts to test an established home-based program for older adults in the general population among the ESRD population.
In conclusion, we identified several concerns and then successfully pilot tested a home-based intervention aimed at improving the physical and social functioning of low-SES older adult HD patients. The shift in the United States toward value-based care has elevated awareness that drivers of health largely fall outside the brick-and-mortar facilities of the health care system and can be found in the places where people live, work, and play.35, 36, 37 As a result, there is increased opportunity through new funding models to reduce the costs of care and improve the US population’s health by addressing nonmedical factors.38, 39 Our findings suggest that home-based interventions addressing limitations in physical function for older adults on dialysis therapy may be feasible and impactful, yet there is currently no home-based standard of care for patients with ESRD. Whether such interventions could increase aging in place, reduce hospitalizations, and increase home dialysis and transplantation consideration in this population is worthy of investigation.
Article Information
Authors’ Full Names and Academic Degrees
Deidra C. Crews, MD, ScM, Alice M. Delaney, PhD, MEd, MA, Janiece L. Walker Taylor, PhD, RN, Thomas K.M. Cudjoe, MD, MPH, Manka Nkimbeng, MPH, RN, Laken Roberts, MPH, Jessica Savage, MSN, Allyson Evelyn-Gustave, OTR/L, Jill Roth, RN, Dingfen Han, PhD, LaPricia Lewis Boyér, BSN, Roland J. Thorpe Jr, PhD, David L. Roth, PhD, Laura N. Gitlin, PhD, and Sarah L. Szanton, PhD, ANP.
Authors’ Contributions
Research idea and study design: DCC, LNG, SLS, DLR; data acquisition: AMD, JS, AE-G, JR, LLB; data analysis/interpretation: DH, LR, RJT, TKMC, DCC, SLS, JS, JLWT, LNG, DLR, MN; statistical analysis: DH; supervision or mentorship: SLS, LNG. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
This study was funded by grant P30AG048773 from the National Institute on Aging, National Institutes of Health (NIH), Bethesda, MD. Dr Crews was supported by grant K23DK097184 from the National Institute of Diabetes and Digestive and Kidney Diseases, NIH, Bethesda, MD. The funders of this study had no role in study design; collection, analysis, or interpretation of data; writing the report; or the decision to submit the report for publication.
Financial Disclosure
The authors declare that they have no relevant financial interests.
Peer Review
Received November 13, 2018. Evaluated by 2 external peer reviewers, with direct editorial input from the Statistical Editor and the Editor-in-Chief. Accepted in revised form December 24, 2018.
Footnotes
Complete author and article information provided before references.
Item S1: Focus group moderator guide.
Item S2: CAPABLE targeted areas, goals, and treatment approaches.
Figure S1: Flow diagram of trial participation.
Figure S2: Dot plots of individual participants’ outcomes, by intervention group.
Supplementary Material
Item S1. Focus group moderator guide.
Item S2. CAPABLE targeted areas, goals, and treatment approaches.
Figure S1. Flow diagram of trial participation.
Figure S2. Dot plots of individual participants’ outcomes, by intervention group.
References
- 1.Saran R., Robinson B., Abbott K.C. US Renal Data System 2017 Annual Data Report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2018;71(3 suppl 1):S1–S672. doi: 10.1053/j.ajkd.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O'Sullivan D., McCarthy G. An exploration of the relationship between fatigue and physical functioning in patients with end stage renal disease receiving haemodialysis. J Clin Nurs. 2007;16(11C):276–284. doi: 10.1111/j.1365-2702.2007.01965.x. [DOI] [PubMed] [Google Scholar]
- 3.Kittiskulnam P., Sheshadri A., Johansen K.L. Consequences of CKD on functioning. Semin Nephrol. 2016;36(4):305–318. doi: 10.1016/j.semnephrol.2016.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . WHO; Geneva, Switzerland: 2001. International Classification of Functioning, Disability and Health: ICF. [Google Scholar]
- 5.Kimmel P.L., Fwu C.W., Eggers P.W. Segregation, income disparities, and survival in hemodialysis patients. J Am Soc Nephrol. 2013;24(2):293–301. doi: 10.1681/ASN.2012070659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Avison W.R., McLeod J.D., Pescosolido B.A. Springer; Boston, MA: 2007. Mental Health, Social Mirror. [Google Scholar]
- 7.Plantinga L.C., Fink N.E., Harrington-Levey R. Association of social support with outcomes in incident dialysis patients. Clin J Am Soc Nephrol. 2010;5(8):1480–1488. doi: 10.2215/CJN.01240210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Untas A., Thumma J., Rascle N. The associations of social support and other psychosocial factors with mortality and quality of life in the Dialysis Outcomes and Practice Patterns Study. Clin J Am Soc Nephrol. 2011;6(1):142–152. doi: 10.2215/CJN.02340310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spinale J., Cohen S.D., Khetpal P. Spirituality, social support, and survival in hemodialysis patients. Clin J Am Soc Nephrol. 2008;3(6):1620–1627. doi: 10.2215/CJN.01790408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thong M.S., Kaptein A.A., Krediet R.T., Boeschoten E.W., Dekker F.W. Social support predicts survival in dialysis patients. Nephrol Dial Transplant. 2007;22(3):845–850. doi: 10.1093/ndt/gfl700. [DOI] [PubMed] [Google Scholar]
- 11.Friend R., Singletary Y., Mendell N.R., Nurse H. Group participation and survival among patients with end-stage renal disease. Am J Public Health. 1986;76(6):670–672. doi: 10.2105/ajph.76.6.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen S.D. Social support interventions will improve the quality of life of ESRD patients. Semin Dial. 2013;26(3):262–265. doi: 10.1111/sdi.12064. [DOI] [PubMed] [Google Scholar]
- 13.Johansen K.L. Exercise in the end-stage renal disease population. J Am Soc Nephrol. 2007;18(6):1845–1854. doi: 10.1681/ASN.2007010009. [DOI] [PubMed] [Google Scholar]
- 14.Johansen K.L., Painter P. Exercise in individuals with CKD. Am J Kidney Dis. 2012;59(1):126–134. doi: 10.1053/j.ajkd.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Farragher J., Jassal S.V. Rehabilitation of the geriatric dialysis patient. Semin Dial. 2012;25(6):649–656. doi: 10.1111/sdi.12014. [DOI] [PubMed] [Google Scholar]
- 16.Szanton S.L., Leff B., Wolff J.L., Roberts L., Gitlin L.N. Home-based care program reduces disability and promotes aging in place. Health Aff (Millwood) 2016;35(9):1558–1563. doi: 10.1377/hlthaff.2016.0140. [DOI] [PubMed] [Google Scholar]
- 17.Szanton S.L., Thorpe R.J., Boyd C. Community aging in place, advancing better living for elders: a bio-behavioral-environmental intervention to improve function and health-related quality of life in disabled older adults. J Am Geriatr Soc. 2011;59(12):2314–2320. doi: 10.1111/j.1532-5415.2011.03698.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Granbom M., Evelyn-Gustave A., Gitlin L., Szanton S.L. Vol 23. The American Occupational Therapy Association; 2018. Helping older adults age in place: environmental modifications of the CAPABLE Program; pp. 8–14. (OT Practice). [Google Scholar]
- 19.Tong A., Sainsbury P., Craig J. Consolidated Criteria for Reporting Qualitative Research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 20.Gitlin L.N., Czaja S. Springer Publishing Company; New York, NY: 2016. Behavioral Intervention Research: Designing, Evaluating and Implementing. [Google Scholar]
- 21.Szanton S.L., Gill J.M. Facilitating resilience using a society-to-cells framework: a theory of nursing essentials applied to research and practice. ANS Adv Nurs Sci. 2010;33(4):329–343. doi: 10.1097/ANS.0b013e3181fb2ea2. [DOI] [PubMed] [Google Scholar]
- 22.Szanton S.L., Wolff J.W., Leff B. CAPABLE trial: a randomized controlled trial of nurse, occupational therapist and handyman to reduce disability among older adults: rationale and design. Contemp Clin Trials. 2014;38(1):102–112. doi: 10.1016/j.cct.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pho A.T., Tanner E.K., Roth J., Greeley M.E., Dorsey C.D., Szanton S.L. Nursing strategies for promoting and maintaining function among community-living older adults: the CAPABLE intervention. Geriatr Nurs. 2012;33(6):439–445. doi: 10.1016/j.gerinurse.2012.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thomas S., Mackintosh S., Halbert J. Does the 'Otago exercise programme' reduce mortality and falls in older adults? A systematic review and meta-analysis. Age Ageing. 2010;39(6):681–687. doi: 10.1093/ageing/afq102. [DOI] [PubMed] [Google Scholar]
- 25.Katz S., Ford A.B., Moskowitz R.W., Jackson B.A., Jaffe M.W. Studies of illness in the aged. The Index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 26.Wallace M., SM Reliability and validity of Katz ADL Index. Am J Nurs. 2008;108(4):4–5. [Google Scholar]
- 27.Lubben J., Gironda M. Centrality of social ties to the health and well being of older adults. In: Harooytan B.B.L., editor. Social Work and Health Care in an Aging World. Springer; New York, NY: 2003. pp. 319–350. [Google Scholar]
- 28.Krause N., Borawski-Clark E. Social class differences in social support among older adults. Gerontologist. 1995;35(4):498–508. doi: 10.1093/geront/35.4.498. [DOI] [PubMed] [Google Scholar]
- 29.Gill T.M., Baker D.I., Gottschalk M., Peduzzi P.N., Allore H., Byers A. A program to prevent functional decline in physically frail, elderly persons who live at home. N Engl J Med. 2002;347(14):1068–1074. doi: 10.1056/NEJMoa020423. [DOI] [PubMed] [Google Scholar]
- 30.Flythe J.E., Hilliard T., Castillo G. Symptom prioritization among adults receiving in-center hemodialysis: a mixed methods study. Clin J Am Soc Nephrol. 2018;13(5):735–745. doi: 10.2215/CJN.10850917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ju A., Unruh M., Davison S. Establishing a core outcome measure for fatigue in patients on hemodialysis: a Standardized Outcomes in Nephrology-Hemodialysis (SONG-HD) Consensus Workshop Report. Am J Kidney Dis. 2018;72(1):104–112. doi: 10.1053/j.ajkd.2017.12.018. [DOI] [PubMed] [Google Scholar]
- 32.Jassal S.V., Chiu E., Hladunewich M. Loss of independence in patients starting dialysis at 80 years of age or older. N Engl J Med. 2009;361(16):1612–1613. doi: 10.1056/NEJMc0905289. [DOI] [PubMed] [Google Scholar]
- 33.Ruiz S., Snyder L.P., Rotondo C., Cross-Barnet C., Colligan E.M., Giuriceo K. Innovative home visit models associated with reductions in costs, hospitalizations, and emergency department use. Health Aff (Millwood) 2017;36(3):425–432. doi: 10.1377/hlthaff.2016.1305. [DOI] [PubMed] [Google Scholar]
- 34.Crews D.C., Scialla J.J., Liu J. Predialysis health, dialysis timing, and outcomes among older United States adults. J Am Soc Nephrol. 2014;25(2):370–379. doi: 10.1681/ASN.2013050567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kindig D.A., Asada Y., Booske B. A population health framework for setting national and state health goals. JAMA. 2008;299(17):2081–2083. doi: 10.1001/jama.299.17.2081. [DOI] [PubMed] [Google Scholar]
- 36.Marmot M., Allen J., Bell R., Bloomer E., Goldblatt P. WHO European review of social determinants of health and the health divide. Lancet. 2012;380(9846):1011–1029. doi: 10.1016/S0140-6736(12)61228-8. [DOI] [PubMed] [Google Scholar]
- 37.Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy People 2020. 2016 https://www.healthypeople.gov/ [Google Scholar]
- 38.Centers for Medicare & Medicaid Services . 2016. Health care innovation awards round one project profiles.https://innovation.cms.gov/files/x/hcia-project-profiles.pdf [Google Scholar]
- 39.Centers for Medicare & Medicaid Services . 2016. Health care innovation awards round two.https://innovation.cms.gov/initiatives/Health-Care-Innovation-Awards/Round-2.html [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Item S1. Focus group moderator guide.
Item S2. CAPABLE targeted areas, goals, and treatment approaches.
Figure S1. Flow diagram of trial participation.
Figure S2. Dot plots of individual participants’ outcomes, by intervention group.