Abstract
Rationale & Objective
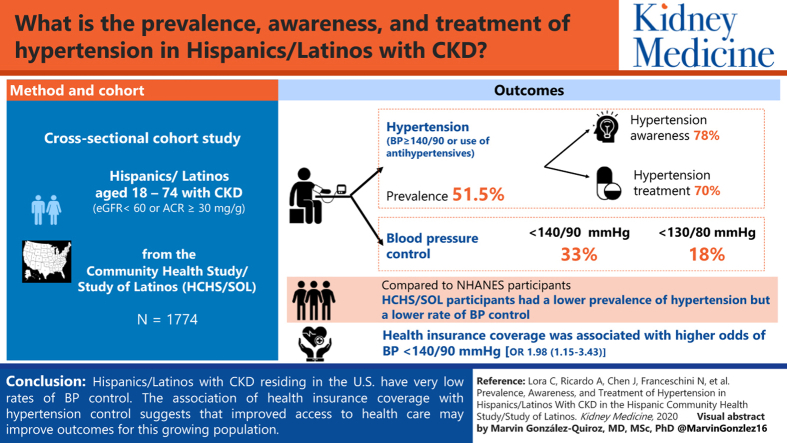
Lower rates of hypertension awareness, treatment, and control have been observed in Hispanics/Latinos compared with non-Hispanic whites. These factors have not been studied in Hispanics/Latinos with chronic kidney disease (CKD). We sought to describe the prevalence, awareness, treatment, and control of hypertension in Hispanic/Latino adults with CKD.
Study Design
Cross-sectional cohort.
Setting & Participants
US.Hispanics/Latinos aged 18 to 74 years enrolled in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) with CKD. Comparisons were made with the National Health and Nutrition Examination Survey (NHANES) 2007 to 2010.
Exposure
CKD was defined as estimated glomerular filtration rate < 60 mL/min/1.73 m2 or urinry albumin-creatinine ratio ≥ 30 mg/g creatinine.
Outcomes
Hypertension was defined as systolic blood pressure (BP) ≥ 140 or diastolic BP ≥ 90 mm Hg or use of antihypertensives. For hypertension control, 2 thresholds were examined: <140/90 and <130/80 mm Hg.
Results
The prevalence of hypertension was 51.5%; among those with hypertension, hypertension awareness and treatment were present in 78.1% and 70.4%, respectively. A low prevalence of BP control was observed (32.6% with BP < 140/90 mm Hg; 17.9% with BP < 130/80 mm Hg). Health insurance coverage was associated with higher odds of BP < 140/90 mm Hg (OR, 1.98; 95% CI, 1.15-3.43). Compared with non-Hispanic whites with CKD in NHANES, HCHS/SOL participants with CKD had a lower prevalence of hypertension but a lower rate of BP control (32.6% vs 48.6% for BP < 140/90 mm Hg).
Limitations
Use of a single measurement of creatinine, cystatin C, and urinary albumin excretion to define CKD. Single-visit measurement of BP.
Conclusions
Hispanics/Latinos with CKD residing in the United States have very low rates of BP control. The association of health insurance coverage with hypertension control suggests that improved access to health care may improve outcomes for this growing population.
Index Words: Hypertension, Hispanics/Latinos, hypertension control, hypertension treatment, health disparities
Graphical Abstract
Hispanics/Latinos are the largest minority in the United States. It is estimated that 57.5 million Hispanics/Latinos currently reside in the United States and this number is projected to double in the next 20 years.1 Consequently, there will be continued growth of the Hispanic chronic kidney disease (CKD) population.2 Compared with non-Hispanic whites, Hispanic/Latino individuals residing in the United States experience a higher incidence of end-stage kidney disease (456 vs 337 per million population).3 Although the reasons for this growing health problem are not well understood, inadequate detection and control of hypertension may be an important contributing factor. Hypertension is an established risk factor for both the development and progression of CKD.4, 5, 6, 7 Several studies have demonstrated that poorly controlled hypertension is associated with more rapid progression of CKD and that control of hypertension slows CKD progression.6,8
Analyses of the National Health and Nutrition Examination Survey (NHANES) have provided insights regarding hypertension in Hispanics/Latinos. These studies have consistently demonstrated lower rates of hypertension awareness, treatment, and control in Mexican Americans compared with non-Hispanic whites.9, 10, 11 However, data from NHANES are largely limited to Mexican Americans. Given that Hispanics/Latinos are genetically, culturally, and socioeconomically heterogeneous, findings regarding a single Hispanic/Latino background group may not be generalizable. Previously, data from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) demonstrated that blood pressure (BP) prevalence, awareness, treatment, and control varied by Hispanic/Latino background.12 However, these analyses did not focus on individuals with CKD. In view of the well-established association of hypertension with CKD progression, it is important to perform more focused analyses on those with CKD. For these reasons, we proposed to describe hypertension prevalence, awareness, treatment, and control among Hispanics/Latinos with and without CKD using data from the HCHS/SOL. Although other studies have examined rates of hypertension awareness, treatment, and control among individuals with CKD,13,14 our study is the first to do so in a diverse population of US Hispanics/Latinos with CKD.
Methods
Study Design and Participants
We performed cross-sectional analyses of baseline examination data from participants in the HCHS/SOL with CKD. CKD was defined as estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73 m2 or urinary albumin-creatinine ratio ≥ 30 mg/g. The design and methods of the HCHS/SOL have been previously described.15,16 In brief, the HCHS/SOL is a community-based longitudinal cohort study of approximately 16,000 Hispanics/Latinos aged 18 to 74 years based in 4 communities in the United States (Chicago, IL; Miami, FL; Bronx, NY; and San Diego, CA). The HCHS/SOL aims to describe the epidemiology of cardiovascular and other diseases in US Hispanics/Latinos and identify risk and protective factors for these conditions. Participants were enrolled through a stratified 2-stage area probability sampling of census block groups and households. To ensure diversity of Hispanic/Latino background groups and socioeconomic status, certain strata were oversampled. Baseline examinations occurred between 2008 and 2011.
The study protocol was approved by each center’s institutional review board and the research was conducted in accordance with the ethical principles of the Declaration of Helsinki. Study participants provided written informed consent.
Instruments and Measurements
Demographic variables of age, sex, income, education, insurance status, place of birth, and length of residency in the United States were self-reported. Participants self-reported their background as Cuban, Dominican, Mexican, Puerto Rican, or Central or South American. The category “other” was used for participants belonging to a group not listed or to more than 1 group. Medical history was obtained and medication inventory was used to list currently used medications. Height and weight were measured and body mass index (BMI) was calculated as kg/m2.
BP was measured using an OMRON HEM-907 XL (Omrom Health Care, Inc) automatic sphygomanometer. With the participant seated, 3 readings 1 minute apart were obtained from the right arm using 1 of 4 cuffs depending on the upper arm circumference. Hypertension was defined as an average reading ≥ 140 mm Hg systolic or 90 mm Hg diastolic or use of antihypertensive medications. Hypertension awareness was defined as presence of hypertension and an affirmative answer to the question: “Has a doctor ever said that you have high blood pressure or hypertension?” Treatment for hypertension was defined as answering yes to the following question: “Were any of the medications that you took during the last 4 weeks for high blood pressure or hypertension?” For hypertension control, 2 threshholds were examined: systolic BP < 140 mm Hg or diastolic BP < 90 mm Hg, as well as systolic BP < 130 or diastolic BP < 80 mm Hg based on guideline recommendations.17,18
Creatinine was measured in serum and urine on a Roche Modular P Chemistry Analyzer (Roche Diagnostics Corp) using a creatinase enzymatic method (Roche Diagnostics). Serum creatinine measurements are isotope-dilution mass spectrometry traceable. Urinary albumin was measured using an immunoturbidometric method on the ProSpec nephelometric analyzer (Dade Behring GMBH; D-35041). The CKD Epidemiology Collaboration (CKD-EPI) creatinine–cystatin C equation was used to estimate GFR.19 CKD was staged using the Kidney Disease Outcomes Quality Initiative practice guidelines.20 In addition, prevalence of hypertension, awareness, treatment, and control by eGFR and albuminuria categories using the Kidney Disease: Improving Global Outcomes 2009 definition and classification of CKD are presented in Table 1, Table 2, Table 3, Table 4.21
Table 1.
Prevalence of Hypertension by eGFR and Albuminuria Category Using Kidney Disease: Improving Global Outcomes 2009 Definition and Classification of Chronic Kidney Disease
| Albuminuria Stages, Description and Range, mg/g |
||
|---|---|---|
| A1 |
A2, A3 |
|
| <30 | ≥30 | |
| eGFR stages, description and range, mL/min/1.73 m2 | ||
| G1 | ||
| >90 | 13.6% | 38.2%a |
| G2 | ||
| 60-89 | 43.1% | 66.7%a |
| G3-G5a | ||
| <60 | 69.5%a | 78.3%a |
Abbreviation: eGFR, estimated glomerular filtration rate.
Individuals included in the analyses.
Table 2.
Prevalence of Hypertension Awareness by eGFR and Albuminuria Category Using Kidney Disease: Improving Global Outcomes 2009 Definition and Classification of Chronic Kidney Disease
| Albuminuria Stages, Description and Range, mg/g |
||
|---|---|---|
| A1 |
A2, A3 |
|
| <30 | ≥30 | |
| eGFR stages, description and range, mL/min/1.73 m2 | ||
| G1 | ||
| >90 | 65.1% | 72.9%a |
| G2 | ||
| 60-89 | 75.7% | 74.8%a |
| G3-G5a | ||
| <60 | 86.8%a | 89.3%a |
Abbreviation: eGFR, estimated glomerular filtration rate.
Individuals included in the analyses.
Table 3.
Prevalence of Hypertension Treatment by eGFR and Albuminuria Category Using Kidney Disease: Improving Global Outcomes 2009 Definition and Classification of Chronic Kidney Disease
| Albuminuria Stages, Description and Range, mg/g |
||
|---|---|---|
| A1 |
A2, A3 |
|
| <30 | ≥30 | |
| eGFR stages, description and range, mL/min/1.73 m2 | ||
| G1 | ||
| >90 | 51.7% | 57.9%a |
| G2 | ||
| 60-89 | 73.2% | 72.3%a |
| G3-G5a | ||
| <60 | 86.7%a | 84.5%a |
Abbreviation: eGFR, estimated glomerular filtration rate.
Individuals included in the analyses.
Table 4.
Prevalence of Hypertension Control (BP < 140/90 mm Hg) by eGFR and Albuminuria Category Using Kidney Disease: Improving Global Outcomes 2009 Definition and Classification of Chronic Kidney Disease
| % | Albuminuria Stages, Description and Range, mg/g |
|
|---|---|---|
| A1 |
A2, A3 |
|
| <30 | ≥30 | |
| eGFR stages, description and range, mL/min/1.73 m2 | ||
| G1 | ||
| >90 | 33.8% | 29.4%a |
| G2 | ||
| 60-89 | 44.3% | 21.5%a |
| G3-G5a | ||
| <60 | 57.8%a | 31.3%a |
Abbreviations: BP, blood pressure; eGFR, estimated glomerular filtration rate.
Individuals included in the analyses.
Statistical Analysis
The HCHS/SOL recruitment process oversampled certain groups; therefore, analyses were weighted to adjust for sampling probability. Hypertension prevalence, awareness, treatment, and control were calculated for individuals with CKD using the total number of participants with hypertension in each category. Using χ2 tests or t test, we compared differences in demographics and clinical variables among individuals with CKD by hypertension, awareness, treatment, and control status.
For awareness, treatment, and control, only individuals with hypertension were included in the analyses. Using 3 separate models for each of the dependent variables, we evaluated the potential association of demographic and clinic factors (age, sex, income, education, health insurance, diabetes, BMI, Hispanic/Latino background group, CKD stage, and albuminuria) with awareness, treatment, and control using multivariable logistic regression. These potential confounding variables were chosen a-priori based on the existing literature.22, 23, 24 All variables were included simultaneously in each of the 3 models. Comparisons of prevalence, awareness, and control were made between HCHS/SOL and NHANES data from 2007 to 2008 and 2009 to 2010 because these periods overlap with the HCHS/SOL baseline examination. All analyses used SAS, version 9.4 (SAS Institute).
Results
Study Population
Of the 1,818 HSHS/SOL participants with CKD, 44 had missing data. Among the 1,774 included in the analytic cohort, mean age was 49 years, 57% were women, 61% had health insurance, 51% had BMI > 30 kg/m2, mean eGFR was 92 mL/min/1.73 m2, and median urinary albumin-creatinine ratio was 60 mg/g.
Hypertension Prevalence, Awareness, Treatment, and Control
The prevalence of hypertension was 51.5%. Among individuls with hypertension, 78.1% were aware and 70.4% were receiving treatment. A low proportion of individuals with hypertension had adequate BP control (BP < 140/90 mm Hg, 32.6%; BP < 130/80 mm Hg, 17.9%).
Compared with individuals without hypertension, individuals with hypertension were more likely to be 45 years and older and men (Table 5). In addition, individuals with hypertension were more likey to be non–United States born and to have lived in the United States for 10 or more years. These individuals were also more likely to have an income <$20,000, less than a high school education, health insurance coverage, diabetes, and BMI ≥ 30 kg/m2 compared with individuals without hypertension. Individuals with hypertension were more likely to be of Cuban or Puerto Rican background and less likely to be of Mexican background. Furthermore, individuals with hypertension had lower eGFRs than those without hypertension.
Table 5.
Prevalence of Hypertension Among Target Population With CKD
| Overall | Hypertension Prevalence |
||
|---|---|---|---|
| Yes | No | ||
| No. | 977 | 797 | |
| Age, y | |||
| 18-44 | 37.9% | 15.3% | 61.8%a |
| 45-64 | 38.6% | 48.0% | 28.6%a |
| ≥65 | 23.6% | 36.7% | 9.6%a |
| Female sex | 56.7% | 48.4% | 65.7%a |
| Income ≤ $20,000 | 48.9% | 53.2% | 44.3%a |
| Income, unknown | 9.2% | 8.3% | 10.2% |
| Education < high school | 41.0% | 45.2% | 36.5%a |
| Health insurance | 61.2% | 69.3% | 52.7%a |
| Diabetes | 41.2% | 55.8% | 25.7%a |
| BMI ≥ 30 kg/m2 | 51.2% | 59.4% | 42.4%a |
| Hispanic/Latino background | |||
| Mexican | 34.9% | 26.2% | 44.1%a |
| Cuban | 22.9% | 29.1% | 16.3%a |
| Puerto Rican | 20.1% | 24.9% | 15.1%a |
| Dominican | 9.1% | 8.7% | 9.6% |
| Central American | 6.8% | 5.8% | 7.9% |
| South American | 3.4% | 2.9% | 3.9% |
| Other | 2.9% | 2.4% | 3.3% |
| Spanish language preference | 79.7% | 83.5% | 75.6%a |
| US born | 17.7% | 13.3% | 22.4%a |
| Living in US > 10 y | 77.6% | 81.6% | 73.3%a |
| eGFR, mL/min/1.73 m2 | 91.9 (1.1) | 80.4 (1.4) | 104.1 (1.4)a |
| Albuminuria, g/g creatinine | 59.8 [35.6-151.6] | 65.0 [34.4-186.4] | 56.5 [36.9-121.8] |
Note: Values for categorical variables are given as percentage; values for continuous variable , as mean (standard error) or median [interquartile range].
Abbreviations: BMI, body mass index; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; US, United States.
P < 0.05.
Compared with individuals with hypertension who were not aware of hypertension, individuals aware of hypertension were more likely to have lived in the United States for 10 or more years, be of Dominican background, and have health insurance, diabetes, and lower eGFRs (Table 6). Compared with untreated individuals with hypertension, individuals with treated hypertension were older and more likely to have health insurance, diabetes, and lower eGFRs.
Table 6.
Awareness and Treatment of Hypertension Among Target Population With CKD and Hypertension
| Hypertension Awareness |
Hypertension Treatment |
|||
|---|---|---|---|---|
| Yes | No | Yes | No | |
| No. | 770 | 207 | 685 | 292 |
| Age, y | ||||
| 18-44 | 13.6% | 21.6% | 12.1% | 23.1%a |
| 45-64 | 48.0% | 47.8% | 45.3% | 54.2% |
| ≥65 | 38.4% | 30.6% | 42.6% | 22.7%a |
| Female sex | 49.7% | 43.9% | 50.3% | 44.1% |
| Income ≤ $20,000 | 55.5% | 45.2% | 55.2% | 48.6% |
| Income, unknown | 7.8% | 9.9% | 8.7% | 7.3% |
| Education < high school | 44.1% | 49.1% | 46.6% | 41.8% |
| Health insurance | 73.5% | 54.0% | 77.1% | 50.7% |
| Diabetes | 59.1% | 44.0%a | 61.9% | 41.3%a |
| BMI ≥ 30 kg/m2 | 59.2% | 60.1% | 61.1% | 55.4% |
| Hispanic/Latino background | ||||
| Mexican | 25.6% | 28.5% | 25.6% | 27.8% |
| Cuban | 29.8% | 26.3% | 30.0% | 26.8% |
| Puerto Rican | 25.1% | 24.3% | 25.2% | 24.3% |
| Dominican | 10.0% | 4.4%a | 10.2% | 5.3% |
| Central American | 5.5% | 6.9% | 4.4% | 9.1%a |
| South American | 2.4% | 4.5% | 2.5% | 3.7% |
| Other | 1.7% | 5.2% | 2.2% | 3.0% |
| Spanish language preference | 82.9% | 85.6% | 83.0% | 84.6% |
| US Born | 12.9% | 14.5% | 12.2% | 15.9% |
| Living in the US > 10 y | 84.1% | 72.9%a | 84.1% | 75.8% |
| eGFR, mL/min/1.73 m2 | 77.7 (1.4) | 90.2 (2.8)a | 75.5 (1.5) | 92.1 (2.2)a |
| Albumuria, g/g creatinine | 61.7 [32.8-183.1] | 77.6 [43.5-208.3] | 61.8 [32.1-183.4] | 68.7 [41.9-192.5] |
Note: Values for categorical variables are given as percentage; values for continuous variable , as mean (standard error) or median [interquartile range].
Abbreviations: BMI, body mass index; CKD, chronic kidney disease; eGFR, estimated glomerulsr filtration rate; US, United States.
P < 0.05.
Compared with individuals with hypertension with BPs ≥ 140/90 mm Hg, individuals with hypertension who had BPs < 140/90 mm Hg were more likely to have health insurance, have diabetes, and be United States born (Table 7). In addition, individuals with BPs < 140/90 mm Hg were more likely to be aware of their diagnosis of hypertension and reported taking a higher number of antihypertensive medications. Similar characteristics were observed when comparing individuals with BPs ≥130/80 versus <130/80 mm Hg.
Table 7.
Demographic and Clinical Characteristics by BP Control Goals Among Target Population with CKD and Hypertension
| JNC8 |
ACC/AHA |
|||
|---|---|---|---|---|
| BP < 140/90 mm Hg | BP ≥ 140/90 mm Hg | BP < 130/80 mm Hg | BP ≥ 130/80 mm Hg | |
| No. | 342 | 635 | 205 | 772 |
| Age, y | ||||
| 18-44 | 17.1% | 14.7% | 17.2% | 15.1% |
| 45-64 | 44.4% | 49.4% | 48.2% | 47.6% |
| ≥65 | 38.6% | 36.0% | 34.6% | 37.3% |
| Female sex | 53.2% | 46.0% | 55.3% | 46.8% |
| Income ≤ $20,000 | 52.4% | 53.8% | 54.4% | 53.1% |
| Education < high school | 38.8% | 38.8%a | 38.8% | 38.8% |
| Health insurance | 77.7% | 65.6%a | 75.8% | 68.2% |
| Diabetes | 67.2% | 50.2%a | 67.4% | 53.2%a |
| BMI ≥ 30 kg/m2 | 61.6% | 58.4% | 60.8% | 59.1% |
| Hispanic/Latino background | ||||
| Mexican American | 29.1% | 24.6% | 30.7% | 25.0% |
| Cuban American | 28.3% | 29.1% | 31.1% | 28.4% |
| Puerto Rican | 27.2% | 24.0% | 25.6% | 24.9% |
| Dominican | 8.8% | 8.9% | 6.9% | 9.3% |
| Central American | 3.3% | 6.9%a | 2.8% | 6.4%a |
| South American | 2.5% | 3.2% | 1.7% | 3.2% |
| Other | 0.7% | 3.4%a | 1.3% | 2.8% |
| Spanish language preference | 79.1% | 85.4% | 78.0% | 84.5% |
| US born | 18.6% | 10.6%a | 20.0% | 11.7% |
| Living in the US > 10 y | 86.1% | 79.6% | 80.2% | 82.0% |
| eGFR, mL/min/1.73 m2 | 76.4% | 82.3% | 75.4% | 81.4% |
| Albuminuria | 51.1 [17.0-139.1] | 69.9 [38.8-220.3] | 50.7 [15.9-136.9] | 68.0 [35.6-197.5] |
| Hypertension awareness, yes | 85.1% | 74.5%a | 80.2% | 77.4% |
| No. of antihypertensives | 1.9 | 1.2a | 1.9 | 1.3a |
| Diuretics | 48.9% | 28.5%a | 44.4% | 33.2%a |
| RAAS blockade | 25.0% | 14.1%a | 23.8% | 16.3% |
Note: Values for categorical variables are given as percentage; values for continuous variables, as mean or median [interquartile range].
Abbreviations: ACC/AHA, American College of Cardiology/American Heart Association guidelines; BMI, body mass index; BP, blood pressure; CKD chronic kidney disease; eGFR, estimated glomerulsr filtration rate; JNC, Eighth Joint National Committee; RAAS, renin-angiotensin-aldosterone system; US, United States.
P < 0.05.
Correlates of Awareness, Treatment, and Control of Hypertension
In multivariable analyses, individuals with stage 3 CKD or higher were more than 3 times more likely to have hypertension awareness than those with stage 1 CKD (odds ratio [OR], 3.48; 95% confidence interval [CI], 1.60-7.59; Table 8). Additionally, compared with individuals with diabetes, individuals without diabetes were less likely to be aware of hypertension (OR, 0.51; 95% CI, 0.32-0.81). The odds of treatment were more than 2-fold greater for individuals with health insurance than those without health insurance (OR, 2.44; 95% CI, 1.49-4.01). There was a graded association between CKD stage and treatment (stage 2 vs stage 1, OR. 1.76; 95% CI, 1.10-2.81; stage 3 vs stage 1, OR, 3.44; 95% CI, 1.88-6.28). Individuals without diabetes had lower odds of treatment compared with those with diabetes (OR, 0.43; 95% CI, 0.27-0.66). Furthermore, individuals with BMI ≥ 30 kg/m2 were more likely to be treated for hypertension than those with a lower BMI (OR, 1.49; 95% CI, 1.01-2.18).
Table 8.
Multivariable Logistic Regression ORs (95% CIs) for Awareness, Treatment, and Control of Hypertension in CKD
| Awareness OR (95% CI) | Treatment OR (95% CI) | Control < 140/90 mm Hg OR (95% CI) | Control < 130/80 mm Hg OR (95% CI) | |
|---|---|---|---|---|
| Age, y | ||||
| 18-44 | 1.00 | 1.00 | 1.00 | 1.00 |
| 45-64 | 1.44 (0.73-2.83) | 1.36 (0.72-2.54) | 0.54 (0.30-0.99) | 0.55 (0.26-1.15) |
| ≥65 | 1.05 (0.45-2.47) | 1.61 (0.73-3.55) | 0.39 (0.18-0.83) | 0.26 (0.12-0.59) |
| Sex | ||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 |
| Female | 1.30 (0.84-1.99) | 1.32 (0.85-2.06) | 1.40 (0.91-2.16) | 1.34 (0.82-2.19) |
| Income | ||||
| ≤$20,000 | 1.00 | 1.00 | 1.00 | 1.00 |
| >$20,000 | 0.80 (0.50-1.28) | 0.93 (0.63-1.38) | 1.17 (0.73-1.87) | 0.83 (0.50-1.37) |
| Unknown | 0.77 (0.49-1.22) | 0.96 (0.65-1.41) | 1.15 (0.71-1.86) | 0.85 (0.50-1.42) |
| Education | ||||
| <High school | 1.00 | 1.00 | 1.00 | 1.00 |
| High school | 1.52 (0.81-2.85) | 1.31 (0.73-2.36) | 1.70 (0.98-2.93) | 1.04 (0.54-1.99) |
| >High school | 1.54 (0.91-2.61) | 1.00 (0.64-1.56) | 1.86 (1.15-3.00) | 1.42 (0.79-2.56) |
| Health insurance | ||||
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 2.10 (1.21-3.66) | 2.44 (1.49-4.01) | 1.98 (1.15-3.43) | 1.74 (0.95-3.19) |
| Diabetes | ||||
| Yes | 1.00 | 1.00 | 1.00 | 1.00 |
| No | 0.51 (0.32-0.81) | 0.43 (0.27-0.66) | 0.38 (0.24-0.60) | 0.45 (0.27-0.76) |
| BMI ≥ 30 kg/m2 | ||||
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.02 (0.65-1.61) | 1.49 (1.01-2.18) | 0.98 (0.65-1.47) | 0.88 (0.54-1.42) |
| Background | ||||
| Mexican American | 1.00 | 1.00 | 1.00 | 1.00 |
| Cuban | 1.82 (0.55-6.06) | 3.01 (1.12-8.11) | 1.04 (0.44-2.44) | 0.84 (0.27-2.60) |
| Puerto Rican | 0.91 (0.37-2.23) | 1.14 (0.53-2.49) | 0.84 (0.40-1.78) | 0.54 (0.22-1.31) |
| Dominican | 1.89 (0.57-6.23) | 2.54 (0.79-8.17) | 0.75 (0.29-1.97) | 0.35 (0.10-1.15) |
| Central American | 1.69 (0.53-5.42) | 1.77 (0.63-4.97) | 0.72 (0.27-1.91) | 0.43 (0.13-1.43) |
| South American | 0.87 (0.24-3.11) | 1.94 (0.64-5.90) | 1.00 (0.36-2.81) | 0.48 (0.14-1.63) |
| Other | ||||
| CKD stage | ||||
| 1 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 1.06 (0.63-1.81) | 1.76 (1.10-2.81) | 0.78 (0.44-1.36) | 1.15 (0.65-2.04) |
| ≥3 | 3.48 (1.60-7.59) | 3.44 (1.88-6.28) | 1.33 (0.66-2.70) | 1.66 (0.67-4.11) |
| Albuminuria | ||||
| <30 mg/g Cr | 1.00 | 1.00 | 1.00 | 1.00 |
| 30-300 mg/g Cr | 1.49 (0.50-4.39) | 0.86 (0.37-1.98) | 0.29 (0.13-0.65) | 0.42 (0.14-1.22) |
| >300 mg/g Cr | 1.01 (0.36-2.82) | 0.90 (0.38-2.12) | 0.21 (0.09-0.49) | 0.25 (0.10-0.59) |
Note: Adjusted for all the variables listed plus center and acculturation.
Abbrevations: BMI, body mass index; CI, confidence interval; CKD, chronic kidney disease; Cr, creatinine; OR, odds ratio.
Compared with individuals aged 18 to 44 years, individuals aged 45 to 64 and 65 years or older had lower odds of BP < 140/90 mm Hg (OR, 0.54; 95% CI, 0.30-0.99; OR, 0.39; 95% CI, 0.18-0.83, respectively). Factors associated with increased odds of BP < 140/90 mm Hg included education more than high school (OR, 1.86; 95% CI, 1.15-3.00) and health insurance versus no health insurance (OR, 1.98; 95% CI, 1.15-3.43). In addition, nondiabetic status was associated with lower odds of hypertension control (OR, 0.38; 95% CI, 0.24-0.60). Albuminuria with albumin excretion > 30 mg/g creatinine was also associated with lower odds of hypertension control (OR, 0.29; 95% CI, 0.13-0.65). A similar pattern was observed for factors associated with BP < 130/80 mm Hg.
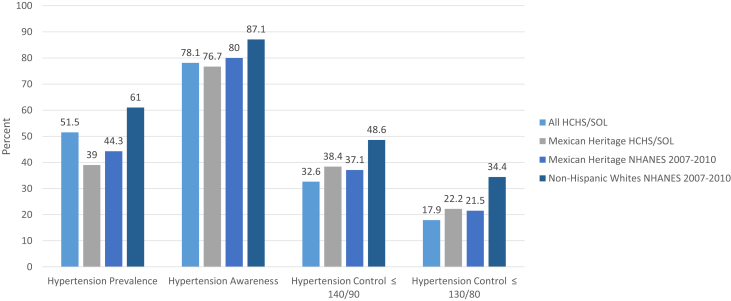
Comparison of Findings in HCHS/SOL Versus NHANES 2007-2010
The prevalence of hypertension in HCHS/SOL participants with CKD was lower than the prevalence in non-Hispanic whites with CKD in NHANES (Fig 1). Hypertension awareness and control were higher among non-Hispanic whites than in the other groups.
Figure 1.
Hypertension prevalence, awareness, and control in the Hispanics Community Health Study/Study of Latinos (HCHS/SOL) and National Health and Nutrition Examination Survey (NHANES) 2007 to 2010. Prevalence of hypertension in HCHS/SOL participants with chronic kidney disease (CKD) was lower than the prevalence in non-Hispanic whites with CKD in NHANES. Hypertension awareness and control were higher among non-Hispanic whites than in the other groups. Of note, rates among individuals of Mexican background were similar in the 2 cohorts.
Discussion
In a large diverse cohort of Hispanic/Latinos, individuals with CKD had a high prevalence of hypertension accompanied by a low prevalence of hypertension awareness, treatment, and control. Among individuals with CKD and hypertension, more than one-quarter were not being treated. Furthermore, only 32.7% had adequate BP control to a goal of <140/90 mm Hg and only 17.9% achieved BP < 130/80 mm Hg. In addition, we found a strong association between health insurance coverage and BP control, suggesting that public health initiatives are needed to improve access to health care for this growing population.
A low prevalence of treatment and control of hypertension in Hispanics/Latinos in the general population has been previously described.9,10 An analysis of data from NHANES 1999 to 2002 demonstrated that Mexican Americans had lower rates of BP control than both non-Hispanic whites and blacks, but these analyses focused on general population data and not on persons with CKD.10 A more recent analysis of NHANES data suggests that awareness, treatment, and control of hypertension in the Hispanic/Latino population may be improving, but rates still remain significantly below those of non-Hispanic whites.9
Other studies have examined the prevalence of hypertension treatment and control in CKD. Similar to our findings, an analysis of data from the Framingham Heart Study Offspring Cohort found higher prevalences of hypertension and suboptimal BP control among individuals with CKD as compared with individuals without CKD.25 Other studies have also reported high rates of suboptimal BP control in individuals with CKD.13,14 However, these studies did not include an adequate representation of Hispanics/Latinos. Suboptimal BP control, a well-established risk factor for CKD progression, is of particular relevance to Hispanics/Latinos in view of the expected continued growth of this population and their higher incident end-stage kidney disease rates as compared with non-Hispanics.3 In the Hispanic Chronic Renal Insufficiency Cohort (CRIC) Study, which included individuals with more advanced CKD, poor BP control and left ventricular hypertrophy were more common in Hispanics/Latinos compared with non-Hispanic whites.26,27 Longitudinal findings from this study suggested that poor BP control contributed to higher end-stage kidney disease incident rates in Hispanics compared with non-Hispanic whites.28 The current study demonstrates that disparities in BP control are also present in Hispanics/Latinos with earlier stages of CKD. This is important because improved BP control in earlier CKD would be expected to have a major impact on long-term outcomes.
A key finding of our study was that individuals with health insurance had better BP control. Lack of health insurance may lead to decreased access to health care and medications. Our findings are of particular concern in view of recent reports of increasing rates of uninsurance among Hispanics/Latinos,29 as well as uncertainty regarding the future of the Affordable Care Act. Furthermore, in 2019, the Executive Branch of US government released a Public Charge Rule, which would prevent immigrants from receiving a green card if it seems that they will require public assistance.30 This rule has the potential to further decrease access to health care access for Hispanics/Latinos, particularly those who are undocumented.
Others have demonstrated associations of health insurance and access to care with BP control.31, 32, 33 In a recent study of more than 150,000 adults with hypertension, uninsured individuals experienced more barriers to accessing health care and were less likely to use antihypertensive medications and have a routine checkup in the past year.34 In a cohort of individuals at risk for CKD, increased access to care was associated with increased odds of BP control, as well as with decreased risk for incident CKD.33 Similarly, an analysis of NHANES demonstrated a higher prevalence of BP control among individuals who had private insurance versus none and among those with a usual source of health care versus none.31 In addition, we found that higher educational attainment was associated with improved BP control. These findings suggest that culturally sensitive public health initiatives are needed to target individuals with lower educational attainment. These initiatives need to be linguistically appropriate, include programing and materials with colors and images that promote acceptance, and explain the relevance to the population.35 For examples, studies have successfully used community members (promotoras) to deliver interventions to improve hypertension control.36,37
The strength of our study is the large community sample with representation of varied Hispanic/Latino backgrounds from across the United States.
Limitations include the use of a single measurement of creatinine, cystatin C, and urinary albumin excretion to define CKD. In addition, BP was measured at a single visit. In clinical practice, the diagnosis of hypertension relies on measurements over time. Nonetheless, this methodology allows for comparisons with other studies that have used the same approach. Finally, we were not able to ascertain medication adherence, which may explain differences in BP control and may mediate the relationship we found between health insurance and BP control.
In conclusion, we found a high prevalence of hypertension and a low prevalence of awareness, treatment, and control among Hispanics/Latinos with CKD, a group at high risk for future cardiovascular disease events and end-stage kidney disease. Improvement of hypertension awareness, treatment, and control should be a public health priority to reduce the disproportionate burden of CKD in this growing population.
Article Information
Authors’ Full Names and Academic Degrees
Claudia M. Lora, MD, Ana C. Ricardo, MD, Jinsong Chen, PhD, Nora Franceschini, MD, Holly J. Kramer, MD, MPH, Michal L. Melamed, MD, Leopoldo Raij, MD, Sylvia E. Rosas, MD, Neil Schneiderman, MD, Martha Daviglus, MD,and James P. Lash, MD.
Authors’ Contributions
Research idea and study design: CML, ACR, JPL; data acquisition: CML, ACR, JPL; data analysis/interpretation: CML, ACR, JC, NF, HJK, MLM, LR, SER, NS, MD, JPL; statistical analysis: JC; supervision or mentorship: CML, JPL, MD. Each author contributed important intellectual content during manuscript drafting or revision, accepts personal accountability for the author’s own contributions, and agrees to ensure that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
The HCHS/SOL was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following institutes/centers/offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Institute on Minority Health and Health Disparities, National Institute on Deafness and Other Communication Disorders, National Institute of Dental and Craniofacial Research, National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institute of Neurological Disorders and Stroke, National Institutes of Health Institution-Office of Dietary Supplements, and Dr Lash is funded by NIDDK K24 DK092290. The funders did not have a role in study design; data collection, analysis, or reporting; or the decision to submit for publication.
Financial Disclosure
The authors declare that they have no relevant financial interests.
Acknowledgements
The authors thank the staff and participants of HCHS/SOL for their important contributions. Investigators website: http://www.cscc.unc.edu/hchs/.
Peer Review
Received August 20, 2019. Evaluated by 3 external peer reviewers, with direct editorial input from the Statistical Editor and the Editor-in-Chief. Accepted in revised form February 17, 2020.
Footnotes
Complete author and article information provided before references.
References
- 1.U.S. Census Bureau Hispanic heritage month 2017. https://www.census.gov/newsroom/facts-for-features/2017/hispanic-heritage.html
- 2.Desai N., Lora C.M., Lash J.P., Ricardo A.C. CKD and ESRD in US Hispanics. Am J Kidney Dis. 2018;73(1):102–111. doi: 10.1053/j.ajkd.2018.02.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.US Renal Data System USRDS 2016 Annual Data Report. https://www.usrds.org/adr.aspx
- 4.Fox C.S., Larson M.G., Leip E.P., Culleton B., Wilson P.W.F., Levy D. Predictors of new-onset kidney disease in a community-based population. JAMA. 2004;291(7):844–850. doi: 10.1001/jama.291.7.844. [DOI] [PubMed] [Google Scholar]
- 5.Hunsicker L.G., Adler S., Caggiula A. Predictors of the progression of renal disease in the Modification of Diet in Renal Disease Study. Kidney Int. 1997;51(6):1908–1919. doi: 10.1038/ki.1997.260. [DOI] [PubMed] [Google Scholar]
- 6.Klag M.J., Whelton P.K., Randall B.L. Blood pressure and end-stage renal disease in men. N Engl J Med. 1996;334(1):13–18. doi: 10.1056/NEJM199601043340103. [DOI] [PubMed] [Google Scholar]
- 7.Young J.H., Klag M.J., Muntner P., Whyte J.L., Pahor M., Coresh J. Blood pressure and decline in kidney function: findings from the Systolic Hypertension in the Elderly Program (SHEP) J Am Soc Nephrol. 2002;13(11):2776–2782. doi: 10.1097/01.asn.0000031805.09178.37. [DOI] [PubMed] [Google Scholar]
- 8.Shulman N.B., Ford C.E., Hall W.D. Prognostic value of serum creatinine and effect of treatment of hypertension on renal function. Results from the Hypertension Detection and Follow-up Program. The Hypertension Detection and Follow-up Program Cooperative Group. Hypertens Dallas Tex 1979. 1989;13(5 suppl 1):I80–I93. doi: 10.1161/01.hyp.13.5_suppl.i80. [DOI] [PubMed] [Google Scholar]
- 9.Egan B.M., Zhao Y., Axon R.N. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303(20):2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 10.Giles T., Aranda J.M., Suh D.-C. Ethnic/racial variations in blood pressure awareness, treatment, and control. J Clin Hypertens. 2007;9(5):345–354. doi: 10.1111/j.1524-6175.2007.06432.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention (CDC) Racial/ethnic disparities in the awareness, treatment, and control of hypertension - United States, 2003-2010. MMWR Morb Mortal Wkly Rep. 2013;62(18):351–355. [PMC free article] [PubMed] [Google Scholar]
- 12.Sorlie P.D., Allison M.A., Avilés-Santa M.L. Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens. 2014;27(6):793–800. doi: 10.1093/ajh/hpu003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peralta C.A., Hicks L.S., Chertow G.M. Control of hypertension in adults with chronic kidney disease in the United States. Hypertens Dallas Tex 1979. 2005;45(6):1119–1124. doi: 10.1161/01.HYP.0000164577.81087.70. [DOI] [PubMed] [Google Scholar]
- 14.Muntner P., Anderson A., Charleston J. Hypertension awareness, treatment, and control in adults with CKD: results from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis. 2010;55(3):441–451. doi: 10.1053/j.ajkd.2009.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sorlie P.D., Avilés-Santa L.M., Wassertheil-Smoller S. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20(8):629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lavange L.M., Kalsbeek W.D., Sorlie P.D. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20(8):642–649. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.James P.A., Oparil S., Carter B.L. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311(5):507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 18.Whelton P.K., Carey R.M., Aronow W.S. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017;72(11):1187–1197. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 19.Inker L.A., Schmid C.H., Tighiouart H. Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med. 2012;367(1):20–29. doi: 10.1056/NEJMoa1114248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.KDOQI KDOQI clinical practice guidelines and clinical practice recommendations for diabetes and chronic kidney disease. Am J Kidney Dis. 2007;49(2 suppl 2):S12–S154. doi: 10.1053/j.ajkd.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 21.Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3(1):1–150. [Google Scholar]
- 22.Norris K., Nissenson A.R. Race, gender, and socioeconomic disparities in CKD in the United States. J Am Soc Nephrol. 2008;19(7):1261–1270. doi: 10.1681/ASN.2008030276. [DOI] [PubMed] [Google Scholar]
- 23.Hemmelgarn B.R., Manns B.J., Lloyd A. Relation between kidney function, proteinuria, and adverse outcomes. JAMA. 2010;303(5):423–429. doi: 10.1001/jama.2010.39. [DOI] [PubMed] [Google Scholar]
- 24.Ricardo A.C., Yang W., Sha D. Sex-related disparities in CKD progression. J Am Soc Nephrol. 2018;30(1):137–148. doi: 10.1681/ASN.2018030296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parikh N.I., Hwang S.-J., Larson M.G., Meigs J.B., Levy D., Fox C.S. Cardiovascular disease risk factors in chronic kidney disease: overall burden and rates of treatment and control. Arch Intern Med. 2006;166(17):1884–1891. doi: 10.1001/archinte.166.17.1884. [DOI] [PubMed] [Google Scholar]
- 26.Fischer M.J., Go A.S., Lora C.M. CKD in Hispanics: baseline characteristics from the CRIC (Chronic Renal Insufficiency Cohort) and Hispanic-CRIC Studies. Am J Kidney Dis. 2011;58(2):214–227. doi: 10.1053/j.ajkd.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ricardo A.C., Lash J.P., Fischer M.J. Cardiovascular disease among Hispanics and non-Hispanics in the Chronic Renal Insufficiency Cohort (CRIC) study. Clin J Am Soc Nephrol. 2011;6(9):2121–2131. doi: 10.2215/CJN.11341210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fischer M.J., Hsu J.Y., Lora C.M. CKD progression and mortality among Hispanics and non-Hispanics. J Am Soc Nephrol. 2016;27(11):3488–3497. doi: 10.1681/ASN.2015050570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Inc G U.S. uninsured rate steady at 12.2% in fourth quarter of 2017. Gallup.com. http://news.gallup.com/poll/225383/uninsured-rate-steady-fourth-quarter-2017.aspx
- 30.Final Rule on Public Charge Ground of Inadmissibility. USCIS. https://www.uscis.gov/legal-resources/final-rule-public-charge-ground-inadmissibility Published October 16, 2019.
- 31.He J., Muntner P., Chen J., Roccella E.J., Streiffer R.H., Whelton P.K. Factors associated with hypertension control in the general population of the United States. Arch Intern Med. 2002;162(9):1051–1058. doi: 10.1001/archinte.162.9.1051. [DOI] [PubMed] [Google Scholar]
- 32.Hicks L.S., Fairchild D.G., Horng M.S., Orav E.J., Bates D.W., Ayanian J.Z. Determinants of JNC VI guideline adherence, intensity of drug therapy, and blood pressure control by race and ethnicity. Hypertens Dallas Tex 1979. 2004;44(4):429–434. doi: 10.1161/01.HYP.0000141439.34834.84. [DOI] [PubMed] [Google Scholar]
- 33.Evans K., Coresh J., Bash L.D. Race differences in access to health care and disparities in incident chronic kidney disease in the US. Nephrol Dial Transplant. 2011;26(3):899–908. doi: 10.1093/ndt/gfq473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fang J., Yang Q., Ayala C., Loustalot F. Disparities in access to care among US adults with self-reported hypertension. Am J Hypertens. 2014;27(11):1377–1386. doi: 10.1093/ajh/hpu061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kreuter M.W., Lukwago S.N., Bucholtz R.D.D.C., Clark E.M., Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. 2003;30(2):133–146. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]
- 36.Balcazar H.G., Byrd T.L., Ortiz M., Tondapu S.R., Chavez M. A randomized community intervention to improve hypertension control among Mexican Americans: using the promotoras de salud community outreach model. J Health Care Poor Underserved. 2009;20(4):1079–1094. doi: 10.1353/hpu.0.0209. [DOI] [PubMed] [Google Scholar]
- 37.Rocha-Goldberg M.D.P., Corsino L., Batch B. Hypertension Improvement Project (HIP) Latino: results of a pilot study of lifestyle intervention for lowering blood pressure in Latino adults. Ethn Health. 2010;15(3):269–282. doi: 10.1080/13557851003674997. [DOI] [PMC free article] [PubMed] [Google Scholar]