Abstract
Rationale & Objective
In 2009, the first case of acute kidney injury and occlusive red blood cell (RBC) tubular casts associated with a high international normalized ratio in a patient receiving warfarin was identified. This entity, named warfarin-related nephropathy, was later renamed anticoagulant-related nephropathy (ARN) after similar cases with other anticoagulants were described. We provide our 10-year experience with ARN based on a single-center kidney biopsy laboratory.
Study Design
The kidney pathology database at the Ohio State University Wexner Medical Center (OSUWMC) was searched for native kidney biopsy cases consistent with ARN. Clinical data were obtained from patient medical records.
Setting & Participants
Native kidney biopsies evaluated between January 1, 2009, and December 31, 2017 at OSUWMC.
Results
Among 8,636 native kidney biopsies reviewed at the OSUWMC, there were 41 (0.5%) patients for whom deterioration in kidney function could not be explained by kidney biopsy findings alone if anticoagulation was not considered. There were 63% men and 95% were white; average age was 62 ± 14 years. Most were on warfarin therapy (N = 28), although cases were also attributed to direct-acting anticoagulants (N = 2), antiplatelet medications (N = 1), heparin or enoxaparin (N = 4), and disseminated intravascular coagulopathy (N = 6). Morphologically, there was acute tubular necrosis and RBC casts. The majority of biopsies had an underlying glomerular disease and many patients had positive serologic test results. In all these cases, the severity of kidney failure, RBC tubular casts, and hematuria were disproportionate to glomerular morphologic changes.
Limitations
Selection bias in the decision to perform a kidney biopsy.
Conclusions
ARN is an uncommon diagnosis in kidney pathology practice, but it should be considered when the number of RBC tubular casts is disproportionate to the severity of glomerular changes in a kidney biopsy in patients either receiving anticoagulation therapy or who presented with acute coagulopathy. Our data suggest that anticoagulation aggravates underlying glomerular diseases rather than directly affecting the glomerular filtration barrier.
Index Words: Kidney biopsy, warfarin-related nephropathy, anticoagulants, acute kidney injury, hematuria
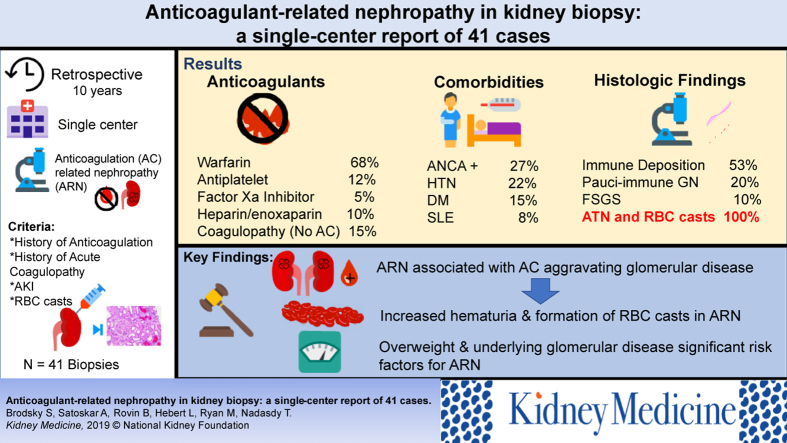
Graphical abstract
In 2009, we described the first patient who presented with acute kidney injury (AKI) while being treated with warfarin. The patient had a supratherapeutic international normalized ratio (INR) before the AKI. Kidney biopsy showed acute tubular necrosis (ATN) with occlusive red blood cell (RBC) tubular casts.1 The glomerular changes alone could not explain this severe glomerular hematuria. After searching our renal pathology database, 8 other patients with similar clinical presentation were identified. These patients also were receiving warfarin therapy with high INRs (>3.0) and had ATN and glomerular hematuria (defined by RBCs in Bowman space and RBC tubular casts and acanthocytes in urine sediment) that were unexplained by other morphology findings.1 This AKI associated with a high INR initially was named warfarin-related nephropathy.
Two subsequent retrospective studies by our group described warfarin-related nephropathy in patients both with and without chronic kidney disease.2, 3 Warfarin-related nephropathy was demonstrated in an animal model of 5/6 nephrectomy rats. In the setting of anticoagulation with vitamin K antagonists, animals showed morphologic futures of warfarin-related nephropathy similar to human disease, including ATN and glomerular hemorrhage.4, 5
Later it was demonstrated that morphologic features similar to warfarin-related nephropathy may also be seen in 5/6 nephrectomy rats treated with the direct thrombin inhibitor dabigatran.6 This observation and clinical data suggested that such AKI may be associated not only with vitamin K antagonists, but other anticoagulants as well. Accordingly, the term “anticoagulant-related nephropathy” (ARN) is preferred. Since the seminal report of pathologic features of warfarin-related nephropathy,1 several investigators published case reports and retrospective studies showing AKI in association with different anticoagulants, including multiple case reports and case series that describe warfarin-related nephropathy,7, 8, 9, 10, 11, 12 case reports of dabigatran-associated AKI,13, 14, 15, 16, 17 a case report of AKI in a patient with thrombocytopenia,18 and a case of biopsy-proven ARN in a patient receiving antiplatelet medications.19
Given the existing data for this newly described entity and the presence of multiple causes for anticoagulation, we explored our database of existing kidney biopsies since our initial description of ARN to describe ARN with additional details, including agents that may predispose to this unusual cause of AKI.
Methods
This study was deemed exempt from the need for informed consent.20 We reviewed The Ohio State University Wexner Medical Center Renal and Transplant Pathology Laboratory Database between January 1, 2009, and December 31, 2017, for the following key words: “nephropathy,” “warfarin,” or “anticoagulant” or “coagulation.” Kidney biopsy pathology reports were deidentified and reviewed along with the clinical history and list of medications. Criteria for ARN included history of anticoagulation and/or coagulopathy, clinical presentation with AKI, and RBC casts in the kidney biopsy. Slides stained with hematoxylin and eosin were blindly reviewed by a renal pathologist (S.V.B.) and the percentage of RBC tubular casts was evaluated for each individual case. Interstitial fibrosis and tubular atrophy were estimated using a semiquantitative scale of 0 to 3 on slides stained with double periodic acid–Schiff/trichrome stain.21
Statistical analysis was performed using GraphPad Prizm 5.0 software (GraphPad Software). Data are presented as mean ± standard deviation, unless specified otherwise.
Results
There were 8,636 native kidney biopsy cases in the Renal Pathology database between January 1, 2009, and December 31, 2017. We identified 57 kidney biopsy reports that contained the keywords “nephropathy,” “warfarin,” “anticoagulant,” or “coagulation.” After reviewing kidney biopsy pathology reports, clinical history, and medications, 48 (0.6%) patients, for whom deterioration in kidney function could not be explained by kidney biopsy findings alone if anticoagulation was not considered, were included in the study. Among those, 7 patients had AKI and increased hematuria that were associated with anticoagulation, but kidney biopsies from those patients did not contain RBC tubular casts, making the diagnosis of glomerular bleeding uncertain. Because of the lack of RBC tubular casts in the kidney biopsy specimens, these 7 patients were excluded from further analyses, resulting in a final study population of 41 (0.5%) patients. Warfarin-related nephropathy (or ARN) was suggested in >0.63% of native kidney biopsies per year in the first 4 years of this study (2009-2012), whereas since 2014, such diagnosis was suggested in ∼0.43% of the native kidney biopsies, decreasing by ∼33%.
Demographic characteristics and clinical data for these patients are shown in Table 1, stratified by the cause of coagulopathy. There were 26 (63%) men, and most patients (95%) were white. Average age of the cohort was 62 ± 14 years. Mean body weight was 103.7 ± 29.3 kg, mean systolic blood pressure was 130 ± 17 mm Hg, and mean diastolic blood pressure was 75 ± 11 mm Hg. Twenty-eight (68%) were receiving warfarin (INR before AKI was 5.6 ± 6.0), 1 (3%) was receiving combined clopidogrel/aspirin, 4 (10%) were receiving heparin (2, unfractionated heparin; and 2, enoxaparin), and 2 (5%) were receiving the factor Xa inhibitor apixaban. Six (15%) patients did not have records of anticoagulation therapy, but they had acute coagulopathy (such as disseminated intravascular coagulation syndrome) at the time of deterioration of kidney function and their kidney biopsy findings were consistent with ARN.
Table 1.
Clinical and Demographic Data in Patients With ARN Based on the Anticoagulation Used
| Demographic and Clinical Data | Anticoagulation |
|
|---|---|---|
| Warfarin/DOAC (n = 30) | Othera (n = 11) | |
| Age, y | 61.2 ± 15.6 | 65.5 ± 10.8 |
| Sex (male/female) | 18/12 (60%/40%) | 8/3 (73%/37%) |
| Race (W/AA) | 25/2 (93%/7%)b | 10/0b |
| Weight, kgb | 99.4 ± 22.5 | 114.6 ± 42.6 |
| Reason for anticoagulation (AF/DVT/APLS)b | 19/6/2 | 1/2/0 |
| Common comorbid conditionsc | ||
| Diabetes mellitus | 4 (13%) | 2 (18%) |
| Hypertension | 7 (23%) | 2 (18%) |
| Positive ANCA | 7 (23%) | 3 (27%) |
| SLE | 1 (3%) | 2 (18%) |
| Baseline Scr, mg/dL | 1.29 ± 0.4 | 1.17 ± 0.4 |
| Peak Scr at AKI diagnosis, mg/dL | 4.16 ± 2.0 | 4.82 ± 2.4 |
Note: Values expressed as mean ± standard deviation or number (percent).
Abbreviations: AA, African American; AF, atrial fibrillation; AKI, acute kidney injury; ANCA, antineutrophil cytoplasmic antibodies; APLS, antiphospholipid antibody syndrome; ARN, anticoagulant-related nephropathy; DOAC, direct-acting oral anticoagulant; DVT, deep vein thrombosis; Scr, serum creatinine; SLE, systemic lupus erythematous; W, white.
Other anticoagulation/coagulopathy included 1 patient using antiplatelet medications, 4 using heparin/enoxaparin, and 6 patients with disseminated intravascular coagulopathy.
Data are not available for some patients.
Some patients have more than 1 comorbid condition.
Among the common comorbid conditions, the most frequent was positive antineutrophil cytoplasmic antibody (ANCA; in 11 (27%) patients, including 7 with perinuclear ANCA, 2 with cytoplasmic ANCA, 1 with both perinuclear and cytoplasmic ANCA, and 1 with atypical ANCA). Nine (22%) patients had a clinical history of hypertension, 6 (15%) had diabetes mellitus type 2, and 3 (8%) had systemic lupus erythematous. No comorbid condition data were available for 2 patients. Serum creatinine levels had increased from 1.25 ± 0.40 mg/dL at baseline to 4.33 ± 1.99 mg/dL at the time of kidney biopsy (Table 1). Before the presentation with AKI, all patients developed either de novo hematuria (from moderate [2+ on dipstick] to gross) or had a significant increase in pre-existing hematuria.
Histologic findings from kidney biopsies are presented in Table 2. In general, biopsies contained 33.4 ± 20.6 glomeruli, with 7.0 ± 3.5 (14%) of those globally sclerosed. Active cellular crescents were seen in 1.1 ± 2.7 glomeruli (5% of glomeruli with open capillary loops). All patients with a presumed diagnosis of ARN had some glomerular injury. The most common finding was mild immune complex deposition in glomeruli, which was seen in 22 (53%) patients (including 14 [34%] with immunoglobulin A [IgA]-predominant, 5 (12%) with IgG-predominant deposits, and 3 (7%) with nonproliferative (International Society of Nephrology/Renal Pathology Society Classes I and II) lupus nephritis). Pauci-immune crescentic necrotizing glomerulonephritis was diagnosed in 8 (20%) patients. Four (10%) patients had focal segmental glomerulosclerosis (FSGS), and 2 (5%) had diabetic glomerulosclerosis. Five (12%) patients had other glomerular findings, including 1 with membranous glomerulonephritis, 1 with fibrillary glomerulonephritis, 1 with mild C3-containing deposits, and 2 biopsies with no specific glomerular lesions but moderately to prominently enlarged glomeruli. All biopsies had features of ATN and RBC casts in the tubules (Fig 1). On average, 18.0% ± 15.0% of tubules had RBC casts. Interstitial fibrosis and tubular atrophy were on average moderate (1.8 ± 0.7 on the scale of 0-3). Focal mild to moderate active-appearing interstitial inflammatory cell infiltrates were noted in 22 (54%) kidney biopsies. Histologic findings stratified by the type of anticoagulation used (warfarin and direct-acting oral anticoagulants [DOAC] vs others) are presented in Table 2.
Table 2.
Histologic Findings in Kidney Biopsies With Diagnosis Suggestive of ARN
| Histologic Findings | Anticoagulation |
|
|---|---|---|
| Warfarin/DOAC (n = 30) | Othera (n = 11) | |
| Glomerular lesions | ||
| IgA-predominant immune complexes in glomeruli (nonmembranous) | 13 (43%) | 1 (6%) |
| IgG-predominant immune complexes in glomeruli (nonmembranous) | 3 (10%) | 2 (12%) |
| Pauci-immune crescentic glomerulonephritis | 4 (13%) | 4 (24%) |
| Focal segmental glomerulosclerosis | 3 (10%) | 1 (6%) |
| Lupus nephritis ISN/RPS class I or II | 2 (7%) | 1 (6%) |
| Diabetic glomerulosclerosis | 1 (3%) | 1 (6%) |
| Other | 4 (13%) | 1 (6%) |
| No. of glomeruli in biopsy specimen | ||
| Total | 27.9 ± 18.2 | 37.1 ± 28.7 |
| Globally sclerotic | 3.3 ± 3.3 | 3.7 ± 4.1 |
| Cellular crescents | 1.47 ± 3.0 (4%)b | 0.27 ± 0.6 (1%)b |
| IFTAc | 1.8 ± 0.5 | 1.8 ± 0.6 |
| Tubules with red blood cell casts | 20.0 ± 16.6 | 12.7 ± 9.6 |
Abbreviations: ARN, anticoagulant-related nephropathy; DOAC, direct-acting oral anticoagulant; IFTA, interstitial fibrosis and tubular atrophy; IgA, immunoglobulin A; ISN/RPS, International Society of Nephrology/Renal Pathology Society.
Other anticoagulation/coagulopathy included 1 patient using antiplatelet medications, 4 using heparin/enoxaparin. and 6 with disseminated intravascular coagulopathy.
Percentage of glomeruli with open capillary loops.
On a semiquantitative scale of 0 to 3: 0 = no IFTA, 1 = 0% to 24% IFTA, 2 = 25% to 49% IFTA, and 3 = 50% to 100% IFTA.
Figure 1.
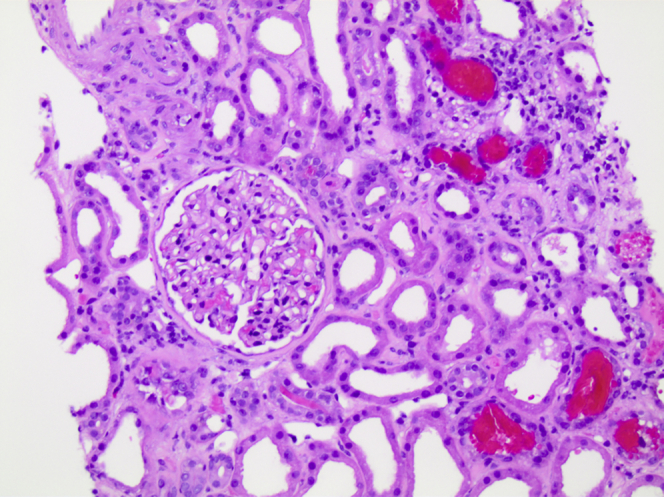
Common light microscopy findings in patients with anticoagulant-related nephropathy (ARN). In a patient with ARN, red blood cell tubular casts and acute tubular injury are the common light microscopy morphologic findings. Glomeruli usually do not show significant morphologic changes.
Discussion
Our 10-year study from a single-center pathology laboratory suggests that ARN is an uncommon diagnosis in kidney pathology practice, but that ARN should be considered when the number of RBC tubular casts is disproportionate to the severity of glomerular changes in a kidney biopsy specimen in patients who are either receiving anticoagulation therapy or present with acute coagulopathy. Our data further suggest that ARN develops in individuals with underlying glomerular diseases, reinforcing the notion that any agent or condition resulting in coagulopathy may result in ARN.
Our study shows that the prevalence of ARN in kidney biopsies was low, at ∼0.5%. Several possibilities may influence the low prevalence of ARN described here. First, we do not know how many of the native kidney biopsies that we received in our renal pathology laboratory are from patients previously receiving anticoagulation. Therefore, the percentage of patients on anticoagulation therapy who developed ARN cannot be evaluated based on the total number of kidney biopsies. Second, nephrologists (and radiologists) are reluctant to perform a kidney biopsy in a patient on anticoagulation therapy; therefore, the true incidence rate of ARN cannot be determined based on the kidney biopsy database. Third, with the recognition of warfarin-related nephropathy (and ARN), the number of kidney biopsies from patients with AKI on anticoagulation therapy is decreasing because nephrologists now associate AKI with anticoagulation and may be less likely to perform kidney biopsies in such patients.
In addition, we recognized 7 patients on anticoagulation therapy who had AKI and significantly increased hematuria, but the kidney biopsy did not show RBC casts in the tubules. Although these patients had increased hematuria, we do not have morphologic evidence of glomerular hemorrhage because the kidney biopsies did not show RBC tubular casts; therefore, the diagnosis of ARN cannot be made with certainty. A sampling error could occur, but this is less likely because in patients with ARN there is an increased number of RBC tubular casts or tubular RBCs that is disproportional to the glomerular morphologic changes (such as mild immune complex deposition or very focal crescentic glomerulonephritis). Therefore, AKI in these patients is probably secondary to other causes or may be due to oxidative stress because of free iron and hemoglobin tubular toxicity.22 Therefore, at this moment, the diagnosis of ARN is reserved only for cases in which an excessive number of RBC tubular casts is present in a kidney biopsy.
Our data reinforce prior findings that ARN develops in patients with underlying glomerular diseases. We identified different pathologic changes in glomeruli. The spectrum of these changes is broad, from focal cellular crescents to glomerular enlargement. The most common pathologic finding, seen in more than a half of the biopsies, was mild immune complex deposition in glomeruli. These glomeruli had mild segmental immune complex deposits (most commonly IgA, but including some patients with class I or II lupus nephritis) and did not show significant proliferative lesions by light microscopy. Therefore, the presence of numerous RBC tubular casts could not be explained just by these glomerular findings.
The second most common finding was focal crescentic glomerulonephritis (usually pauci-immune). Although RBC tubular casts are a hallmark of crescentic glomerulonephritis, the number of RBC tubular casts in these patients was significantly higher than the number of glomeruli with crescents, suggesting that anticoagulation played a role in the formation of this excessive number of RBC tubular casts. Other glomerular diseases that were seen in patients with ARN included FSGS, diabetic glomerulosclerosis, membranous glomerulonephritis, and mild C3 deposits.
In all these cases, AKI was associated either with excessive anticoagulation (INR > 3.0) or the initiation of anticoagulation therapy (such as in patients with heparin- or DOAC-associated AKI). Therefore, we propose that rather than directly affecting the glomerular filtration barrier, excessive anticoagulation aggravates an underlying glomerular disease and increases glomerular hematuria, which leads to the formation of RBC casts and ATN. Several patients with pauci-immune crescentic glomerulonephritis did not have clinical symptoms of this disease until they initiated anticoagulation therapy, but kidney biopsies from these patients showed fibrocellular and fibrous crescents, indicating chronic glomerular disease.
Demographically, patients with ARN in our study population were obese, suggesting that glomerular hyperfiltration/hyperperfusion plays a significant role in the pathogenesis of ARN. Indeed, we modeled ARN in a 5/6 nephrectomy rat model that is characterized by glomerular hyperfiltration/hyperperfusion.4, 5, 6 These animals developed ARN within 3 weeks after the ablative surgery, much earlier than changes of FSGS could be seen histologically.4, 6
The major limitation of the current study is selection bias in the decision to perform kidney biopsy in patients with AKI who are on anticoagulation therapy. Nephrologists are reluctant to perform biopsy on such patients, and sometimes only other laboratory data (such as positive ANCA tests) may prompt the biopsy decision. However, the number of biopsies with ARN decreased as the nephrology and pathology community became more aware that AKI may be associated with anticoagulation therapy, potentially resulting in an empiric clinical diagnosis without a kidney biopsy, particularly in individuals with high INRs. Clinical features of ARN and a suggested algorithm for the evaluation of patients receiving anticoagulation who present with AKI were recently described by our group.23
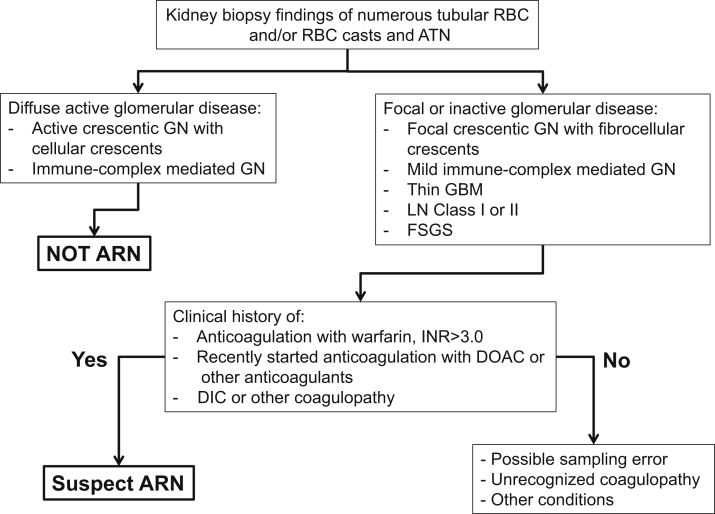
In conclusion, ARN is an uncommon diagnosis in renal pathology practice, but it should be considered when there is a discrepancy between the severity of glomerular changes and number of RBC tubular casts in a kidney biopsy in patients on anticoagulant therapy or who presented with acute coagulopathy and hematuria (Fig 2). The glomerular changes in patients with suspected ARN are insufficient to explain the occurrence of substantial hematuria and RBC casts in tubules, but the high prevalence of underlying glomerular diseases and obesity suggests that ARN may be most likely to occur in individuals with pre-existing glomerular damage by increasing their susceptibility to glomerular bleeding in the setting of systemic anticoagulation or other coagulopathy.
Figure 2.
Proposed diagnostic algorithm in patients with suspected anticoagulant-related nephropathy (ARN). If a kidney biopsy shows numerous red blood cells (RBCs) in tubules or RBC casts without appropriate glomerular injury, clinical history and laboratory data should be reviewed to exclude excessive anticoagulation with warfarin (international normalized ratio [INR] > 3.0), new onset of anticoagulation therapy, or coagulopathy (although the current terminology is ARN, our data suggest that patients with underlying coagulopathy such as disseminated intravascular coagulopathy [DIC] may experience glomerular hemorrhage and ARN-like findings in the kidney biopsy). Abbreviations: ATN, acute tubular necrosis; DOAC, direct-acting oral anticoagulant; FSGS, focal segmental glomerulosclerosis; GBM, glomerular basement membrane; GN, glomerulonephritis; LN, lupus nephritis.
Article Information
Authors’ Full Names and Academic Degrees
Sergey V. Brodsky, MD, PhD, Anjali Satoskar, MD, Jessica Hemminger, MD, Brad Rovin, MD, Lee Hebert, MD, Margaret S. Ryan, MD, and Tibor Nadasdy, MD, PhD.
Authors’ Contributions
Research idea and study design: SVB, LH, TN; data acquisition: SVB, AS, JH, MR; data analysis/interpretation: SVB, BR, LH, TN; statistical analysis: SVB; MR, JH; supervision or mentorship: BR, LH, TN. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
This study partially was supported by National Institutes of Health grant DK117102 to Dr Brodsky. The funder had no role in study design; data collection, analysis, or reporting; or the decision to submit for publication.
Financial Disclosure
The authors declare that they have no relevant financial interests.
Peer Review
Received December 5, 2018. Evaluated by 2 external peer reviewers, with direct editorial input from the Editor-in-Chief. Accepted in revised form March 4, 2019.
Footnotes
Complete author and article information provided before references.
References
- 1.Brodsky S.V., Satoskar A., Chen J. Acute kidney injury during warfarin therapy associated with obstructive tubular red blood cell casts: a report of 9 cases. Am J Kidney Dis. 2009;54(6):1121–1126. doi: 10.1053/j.ajkd.2009.04.024. [DOI] [PubMed] [Google Scholar]
- 2.Brodsky S.V., Collins M., Park E. Warfarin therapy that results in an international normalization ratio above the therapeutic range is associated with accelerated progression of chronic kidney disease. Nephron Clin Pract. 2010;115(2):c142–c146. doi: 10.1159/000312877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brodsky S.V., Nadasdy T., Rovin B.H. Warfarin-related nephropathy occurs in patients with and without chronic kidney disease and is associated with an increased mortality rate. Kidney Int. 2011;80(2):181–189. doi: 10.1038/ki.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ozcan A., Ware K., Calomeni E. 5/6 nephrectomy as a validated rat model mimicking human warfarin-related nephropathy. Am J Nephrol. 2012;35(4):356–364. doi: 10.1159/000337918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ware K., Brodsky P., Satoskar A.A. Warfarin-related nephropathy modeled by nephron reduction and excessive anticoagulation. J Am Soc Nephrol. 2011;22(10):1856–1862. doi: 10.1681/ASN.2010101110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ryan M., Ware K., Qamri Z. Warfarin-related nephropathy is the tip of the iceberg: direct thrombin inhibitor dabigatran induces glomerular hemorrhage with acute kidney injury in rats. Nephrol Dial Transplant. 2014;29(12):2228–2234. doi: 10.1093/ndt/gft380. [DOI] [PubMed] [Google Scholar]
- 7.Larpparisuth N., Cheunsuchon B., Chawanasuntorapoj R. Warfarin related nephropathy: the first case report in Thailand. J Med Assoc Thailand. 2015;98(2):212–216. [PubMed] [Google Scholar]
- 8.Zerah L., Brocheriou I., Galichon P. [Warfarin-related nephropathy: a case report] Rev Med Intern. 2015;36(1):51–54. doi: 10.1016/j.revmed.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 9.An J.N., Ahn S.Y., Yoon C.H. The occurrence of warfarin-related nephropathy and effects on renal and patient outcomes in Korean patients. PloS One. 2013;8(4) doi: 10.1371/journal.pone.0057661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mendonca S., Gupta D., Valsan A. Warfarin related acute kidney injury: a case report. Indian J Nephrol. 2017;27(1):78–80. doi: 10.4103/0971-4065.177142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mendonca S., Valsan A.K. Warfarin induced glomerulonephropathy. J Assoc Physicians India. 2016;64(1):125. [Google Scholar]
- 12.Piran S., Traquair H., Chan N. Incidence and risk factors for acute kidney injury in patients with excessive anticoagulation on warfarin: a retrospective study. J Thromb Thrombolysis. 2018;45(4):557–561. doi: 10.1007/s11239-018-1626-1. [DOI] [PubMed] [Google Scholar]
- 13.Sharfuddin N., Nourbakhsh M., Box A. Anticoagulant related nephropathy induced by dabigatran. Case Rep Nephrol. 2018;2018:7381505. doi: 10.1155/2018/7381505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kadiyala D, Brewster UC, Moeckel GW. Dabigatran induced acute kidney injury. Paper presented at: American Society of Nephrology Annual Meeting; November 1-4, 2012; San Diego, CA. FR-PO1122.
- 15.Moeckel G.W., Luciano R.L., Brewster U.C. Warfarin-related nephropathy in a patient with mild IgA nephropathy on dabigatran and aspirin. Clin Kidney J. 2013;6(5):507–509. doi: 10.1093/ckj/sft076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shafi S.T., Negrete H., Roy P. A case of dabigatran-associated acute renal failure. WMJ. 2013;112(4):173–175. quiz 176. [PubMed] [Google Scholar]
- 17.Li X., Cheung C.Y. Dabigatran causing severe acute kidney injury in a patient with liver cirrhosis. CEN Case Rep. 2019;8(2):125–127. doi: 10.1007/s13730-019-00378-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Medani C.R., Pearl P.L., Hall-Craggs M. Acute renal failure, hemolytic anemia, and thrombocytopenia in poststreptococcal glomerulonephritis. South Med J. 1987;80(3):370–373. doi: 10.1097/00007611-198703000-00025. [DOI] [PubMed] [Google Scholar]
- 19.Kratka K., Havrda M., Honsova E. Bioptically proven "anticoagulation-related nephropathy" induced by dual antiplatelet therapy. Case Rep Nephrol Dial. 2018;8(3):216–222. doi: 10.1159/000493093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.US Department of Health and Human Services. Protection of human subjects. Code of Federal regulations 45: Public welfare 1995; Title 45(Sections 46-101 to 46-409): Revised January 15, 2009. [PubMed]
- 21.Brodsky S.V., Albawardi A., Satoskar A.A. When one plus one equals more than two--a novel stain for renal biopsies is a combination of two classical stains. Histol Histopathol. 2010;25(11):1379–1383. doi: 10.14670/HH-25.1379. [DOI] [PubMed] [Google Scholar]
- 22.Ware K., Qamri Z., Ozcan A. N-Acetylcysteine ameliorates acute kidney injury but not glomerular hemorrhage in an animal model of warfarin-related nephropathy. Am J Physiol Renal Physiol. 2013;304(12):F1421–F1427. doi: 10.1152/ajprenal.00689.2012. [DOI] [PubMed] [Google Scholar]
- 23.Brodsky S., Eikelboom J., Hebert L.A. Anticoagulant-related nephropathy. J Am Soc Nephrol. 2018;29(12):2787–2793. doi: 10.1681/ASN.2018070741. [DOI] [PMC free article] [PubMed] [Google Scholar]