Abstract
Crystalglobulinemia, a rare manifestation of monoclonal gammopathy, results from vascular deposition of crystallized monoclonal proteins leading to tissue injury. A 56-year-old man initially presented several years earlier with migratory polyarthralgias and blurry vision with no unifying diagnosis. Following an acute episode of malignant hypertension and rapidly progressive kidney failure, kidney biopsy was performed and was interpreted as idiopathic thrombotic microangiopathy. Further evaluation revealed an underlying monoclonal protein disorder. Slit-lamp biomicroscopy evaluation showed crystalline keratopathy. Re-evaluation of the kidney biopsy material with pronase staining confirmed crystalglobulin-induced nephropathy. The patient was initially treated with cyclophosphamide, bortezomib, and dexamethasone with partial response, followed by autologous stem cell transplantation with normalization of monoclonal protein studies, improvement in kidney function and joint symptoms, and decreased corneal deposits. His disease recurred but did not require additional treatment 1 year later. This case exemplifies the unique systemic presentation of diseases in the monoclonal gammopathy spectrum and emphasizes the need for a multidisciplinary approach when caring for these patients.
Index Words: Crystalglobulin nephropathy, crystalglobulinemia, crystalline keratopathy
Introduction
Lymphoproliferative disorders including monoclonal protein disorders have a wide range of associated clinical presentations involving multiple organ systems, and kidney involvement is well described.1, 2 Ocular involvement is increasingly recognized in the literature.3, 4, 5 Crystalglobulinemia is a rare complication of these disorders due to precipitated protein aggregates forming crystals in the microvasculature, resulting in ischemia and end-organ damage. Despite major advances in treatment, manifestations of crystalglobulinemia have been shown to persist despite multiple treatment modalities.6, 7, 8 Crystalglobulin-induced nephropathy was recently described in a patient with skin ulcerations.9 We describe a case of crystalglobulinemia with associated renal and ocular manifestations.
Case Report
A 56-year-old previously healthy white man presented with hypertensive emergency and rapidly progressive kidney failure. Before presentation, he had been evaluated elsewhere for a 3-year history of intermittent fevers and migratory polyarthritis with synovitis involving the spine, shoulders, knees, and small joints. Seronegative arthritis was diagnosed, and he started on treatment with prednisone, 50 mg/d, with partial symptom relief. He was subsequently treated with multiple immunosuppressive agents, including tumor necrosis factor inhibitors, without benefit. After 2 years of treatment, the patient developed intermittent episodes of blurry vision. Slit-lamp biomicroscopy revealed peripheral crystalline deposits in the cornea of undetermined cause.
One month before referral to our facility, the patient was admitted to a local hospital with hypertensive emergency and rapidly progressive kidney failure (creatinine, 5.4 [baseline, 1.0] mg/dL). Urinalysis revealed hematuria and proteinuria. Complete blood cell count results were normal. Results of serologic workup, including antineutrophil cytoplasmic antibody, hepatitis, cryoglobulins, and ADAMTS13 (von Willebrand factor protease) were unremarkable. Two kidney biopsies were interpreted as “thrombotic microangiopathy.” The patient underwent plasmapheresis and aggressive blood pressure control. At the time of dismissal, creatinine level had improved to 3.6 mg/dL.
The patient was subsequently referred to our institution for further evaluation. His blood pressure was reasonably well controlled on treatment with 3 agents. Serum creatinine level was stable (3.5 mg/dL). Serum C3 and C4 levels were normal. Serum protein immunoelectrophoresis was positive for a small immunoglobulin G (IgG) λ M spike. Serum free light chains were 26.1 (range, 0.57-2.63) mg/dL for λ and 3.06 (range, 0.33-1.94) mg/dL for κ, with κ:λ ratio of 0.1165 (range, 0.26-1.65). Bone marrow biopsy revealed 5% to 10% λ light chain–restricted plasma cells. Abdominal fat aspirate was negative for amyloid.
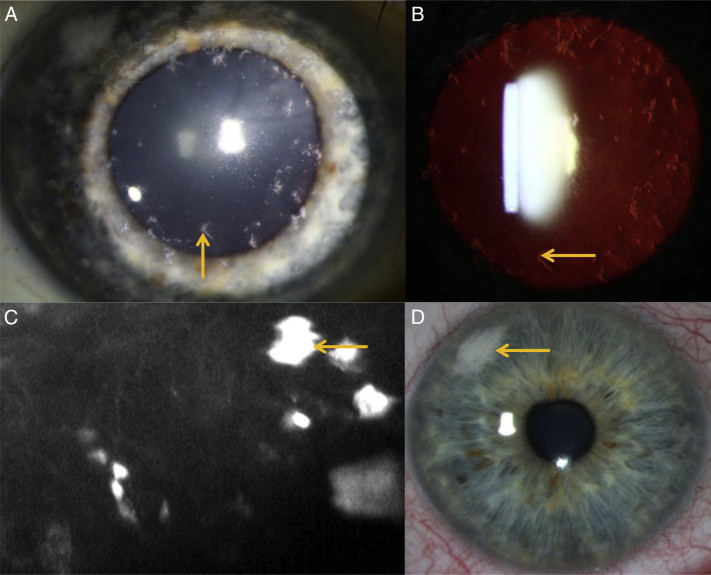
Ophthalmic evaluation revealed diffuse, subepithelial, and stromal corneal crystalline deposits in both eyes. Visual acuities were 20/20 in the right eye and 20/25 in the left eye, and funduscopy results were normal. Slit-lamp and confocal microscopy confirmed hyperreflective subepithelial and stromal corneal deposits (Fig 1A-C), consistent with crystalline keratopathy.
Figure 1.
Slit-lamp examination of the right eye in a patient with crystalglobulin-induced nephropathy shows diffuse subepithelial and stromal corneal crystalline deposits (gold arrows) visible on both (A) direct and (B) retroillumination. (C) Confocal microscopy examination shows the presence of subepithelial and stromal hyperreflective deposits. (D) Slit-lamp examination of the right eye following treatment with cyclophosphamide, bortezomib, and dexamethasone reveals fewer crystalline deposits.
The previous kidney biopsies from the other institution were reviewed again. Glomerular and vascular thrombi were seen, with segmental duplication of glomerular basement membranes. On high magnification, thrombi were composed of packed crystals (Fig 2A). Standard immunofluorescence (IF) on frozen tissue was positive for fibrinogen and negative for IgG, IgM, IgA, C3, C1q, and κ and λ light chains; however, using IF on pronase-digested paraffin-embedded tissue (Fig 2B-C), the vascular intraluminal crystals stained positive for λ with negative κ (ie, masked deposits). Crystalglobulinemia with crystalglobulin-induced nephropathy and keratopathy secondary to monoclonal gammopathy was diagnosed.
Figure 2.
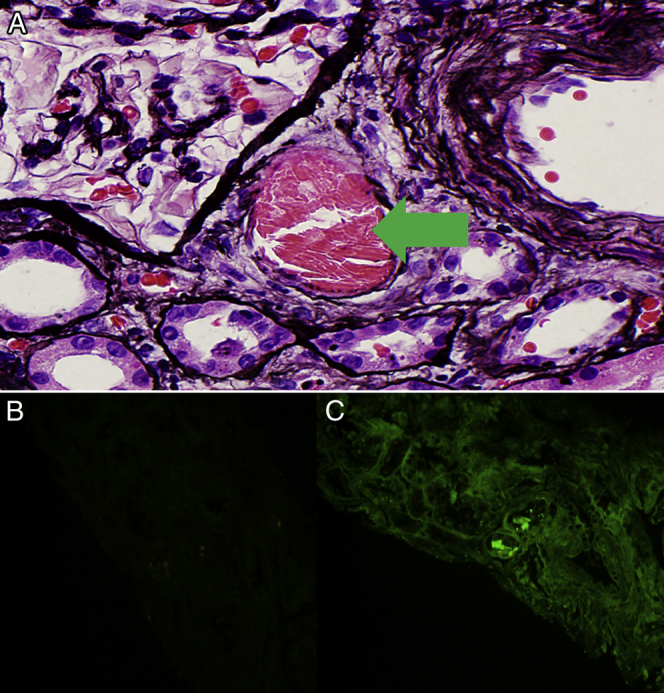
Kidney biopsy (light microscopy; silver methenamine stain) from a patient with crystalglobulin-induced nephropathy showed (A) intravascular (arrow) crystalline structures. Immunofluorescence (IF) was originally negative (not shown), but (B, C) pronase IF was negative for κ and positive for λ light chains. Electron microscopy is not shown because the sampled material did not contain crystals.
The patient was initiated on treatment with weekly cyclophosphamide, bortezomib, and dexamethasone (CyBorD) with improvement in arthritis. Visual acuity remained 20/20 in both eyes, with decreased corneal crystalline deposits on follow-up slit-lamp examination 6 months later (Fig 1D). After 6 cycles of CyBorD, he achieved a partial response, and creatinine level improved to 1.9 mg/dL. He subsequently underwent autologous stem cell transplantation. He had resolution of rheumatologic symptoms, while his visual symptoms were stable. Serum λ level normalized and creatinine level nadired at 1.4 mg/dL. Three months later, he developed worsening bilateral knee arthritis responsive to intra-articular steroid injection and increasing hypertension. Creatinine level peaked at 2.0 mg/dL, and λ light chains increased to 5.92 mg/dL. Repeat bone marrow biopsy revealed <0.1% monotypic λ light chain plasma cells. His disease stabilized without intervention, and 1 year later his creatinine level was 1.6 mg/dL, off chemotherapy.
Discussion
We present a case of crystalglobulin-induced nephropathy and keratopathy, which posed a diagnostic challenge given the initial vague symptoms that mimicked other systemic diseases, including rheumatologic disorders and thrombotic microangiopathy. However, thorough evaluation of the kidney biopsy specimen, including pronase IF, and the finding of crystalline keratopathy culminated in the correct diagnosis.
Monoclonal protein–related kidney diseases have a highly variable presentation. Depending on tumor burden, type of monoclonal protein, and associated physical characteristics of the urinary milieu, these proteins can deposit in the kidney or other tissues, leading to multiorgan injury. Rarely, patients produce clonal proteins forming crystal deposits. The most commonly reported monoclonal protein–related crystalline nephropathies are light chain proximal tubulopathy, crystalline light chain cast nephropathy, crystal-storing histiocytosis, and more rarely, cryocrystalglobulinemia or crystalglobulinemia (a subset of monoclonal protein–associated renal lesions outlined in Box 1).1, 2, 9
Box 1. Monoclonal Protein–Related Renal Lesions.
Monoclonal Immunoglobulin Deposits
Organized
-
•
Fibrillar: Immunotactoid-related amyloidosis, monoclonal fibrillary glomerulonephritis
-
•
Microtubular: Immunotactoid glomerulonephritis, type I and type II cryoglobulinemic glomerulonephritis
-
•
Crystalline deposits or inclusions: LCPT, crystal-storing histiocytosis, and crystalglobulin or cryocrystalglobulin glomerulonephritis
Nonorganized
-
•
MIDD
-
•
PGNMID
-
•
Waldenstrom macroglobulinemia–associated nephropathy (intracapillary monoclonal deposits disease)
Lesions Without Monoclonal Deposits
-
•
Myeloma cast nephropathy
-
•
Direct interstitial invasion of multiple myeloma
-
•
C3 glomerulopathy with monoclonal gammopathy
-
•
Thrombotic microangiopathy
Abbreviations: LCPT, light chain proximal tubulopathy; MIDD, monoclonal immunoglobulin deposit disease; PGNMID, proliferative glomerulonephritis with monoclonal immune deposits.
Crystalglobulinemia, also known as cryocrystalglobulinemia, was first described by von Bonsdorff in 1938; crystallizing serum proteins at colder temperatures that dissolved upon rewarming were found in a patient with multiple myeloma.8 The mechanism of crystal formation is not well understood. Spontaneous crystallization of light chains can occur when excess κ V domain fragment together with the entire κ light chain.10 This leads to a protease-resistant protein with the ability to aggregate and crystallize.10 The formation of these crystalline substructures likely takes place within the endoplasmic reticulum of plasma cells, where protein and immunoglobulin synthesis occurs,11 as well as within the acidic lysosome environment after secreted light chains are endocytosed by these organelles as described in light chain proximal tubulopathy and crystal-storing histiocytosis.11, 12 The crystalline structures precipitate when there is supersaturation, observed in vitro with IgG3 in cryoglobulinemia.13 Crystalglobulinemia is reportedly associated with in vivo formation of monoclonal antibodies against albumin, as well as abnormal N-glycosylation of oligosaccharides on the κ chain of crystalglobulins, leading to protein misfolding and insolubility of immunoglobulins.12, 14
Clinical manifestations are a result of small-vessel inflammation and thrombosis leading to end-organ injury.9, 11 A proposed mechanism of injury is the extracellular deposition of these crystalline structures within the microvasculature and subsequent damage to the vascular epithelium, leading to increased vascular permeability and recruitment of inflammatory mediators with activation of the clotting cascade, culminating in thrombosis with subsequent fibrosis of the vessel and surrounding tissue.15 Patients can present with acute kidney injury, renal artery thrombosis, skin rash/ulcerations, neurologic manifestations, neuropathy, polyarthritis, and blurry vision.3, 4, 5, 6, 7, 8, 9, 13, 14, 15, 16, 17, 18
The latter symptom is a result of crystalline keratopathy that develops as a result of precipitation of these immunoglobulin crystals in the cornea.3, 4, 5 Crystalline keratopathy has been reported in <1% of patients with myeloma-related disorders.3, 4, 5 The crystals can involve any of the layers of the cornea, differentiating crystalglobulin-induced keratopathy from other crystal-depositing diseases. When diagnosed, patients require systemic evaluation.5 Corneal biopsy, while potentially helpful, is not required when systemic evaluation including biopsy of other affected organs reveals a monoclonal protein disorder.
Renal involvement, termed crystalglobulin-induced nephropathy, is characterized by the presence of large extracellular crystals within the lumen of arterioles, arteries, and/or glomerular capillaries.9 The presentation is highly variable, with many cases leading to rapidly progressive kidney failure requiring hemodialysis.7, 9, 13
The diagnosis of crystalglobulinemia is challenging. Although some crystalglobulins cryoprecipitate, not all are easily detectable and they do not resolubilize at warmer temperatures.9, 11, 14, 18 Histology is crucial in establishing the diagnosis. On light microscopy, the presence of hypereosinophilic extracellular crystals within the glomerular capillary loops and/or surrounding vasculature warrants further investigation. An important test for making the diagnosis of crystalglobulinemia is IF on paraffin-embedded tissue. In our patient, IF results on frozen tissue were negative, but when one has a high degree of clinical suspicion of the lesion, the value of paraffin IF after pronase digestion, which could open up the antigenic sites, is paramount.19 When monoclonality is detected, one must proceed with workup to search for the monoclonal protein. The recommended testing is serum and urine immunoelectrophoresis with immunofixation, serum free light chains, and bone marrow biopsy.19 Patients can present with low levels of the monoclonal protein, which can be missed if only a single test is used for screening.20 Our clinical laboratory has recently migrated to mass spectrometry, which is a more sensitive assay.
Management begins with clone-directed therapy, even if patients do not meet criteria for multiple myeloma. Initial treatment can include steroids and proteasome inhibitors with consideration for bone marrow transplantation, depending on response. The role of plasmapheresis in removing monoclonal proteins to prevent ongoing crystal precipitation can be considered in some cases.9, 20 Our patient underwent plasmapheresis, albeit for a different diagnosis, and kidney function improved. He did not undergo further plasmapheresis when he presented to our institution given his stable kidney function. In all cases, close monitoring of the hematologic response is needed because remission is rare and relapse is common despite these measures.7, 9, 13
In summary, our case exemplifies the need for a multidisciplinary approach with collaboration and understanding of a patient’s rheumatologic, ophthalmologic, renal, and hematologic issues to provide optimal individualized patient care. Early diagnosis and therapy are key in changing the disease course and preventing long-term end-organ damage.
Article Information
Authors’ Full Names and Academic Degrees
Matthew R. D’Costa, MD, Lauren A. Dalvin, MD, Sandhya Manohar, MBBS, Leo J. Maguire, MD, Joseph P. Grande, MD, PhD, Wilson I. Gonsalves, MD, Samih H. Nasr, MD, and Marie C. Hogan, MD, PhD.
Support
None.
Financial Disclosure
The authors declare that they have no relevant financial interests.
Peer Review
Received December 3, 2018. Evaluated by 2 external peer reviewers, with direct editorial input from an Associate Editor and the Editor-in-Chief. Accepted in revised form January 31, 2019.
Footnotes
Complete author and article information provided before references.
References
- 1.Blade J., Fernandez-Llama P., Bosch F. Renal failure in multiple myeloma: presenting features and predictors of outcome in 94 patients from a single institution. Arch Intern Med. 1998;158(17):1889–1893. doi: 10.1001/archinte.158.17.1889. [DOI] [PubMed] [Google Scholar]
- 2.Nasr S.H., Valeri A.M., Sethi S. Clinicopathologic correlations in multiple myeloma: a case series of 190 patients with kidney biopsies. Am J Kidney Dis. 2012;59(6):786–794. doi: 10.1053/j.ajkd.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 3.Busch C., Koh S., Oie Y., Ichii M., Kanakura Y., Nishida K. In vivo confocal microscopy of multiple myeloma associated crystalline keratopathy. Am J Hematol. 2017;92(6):593–594. doi: 10.1002/ajh.24692. [DOI] [PubMed] [Google Scholar]
- 4.Houben N., Foets B. Confocal microscopy in multiple myeloma associated crystalline keratopathy: case report. Bull Soc Belge Ophtalmol. 2006;300:13–17. [PubMed] [Google Scholar]
- 5.Koo H., Oh D.H., Chun Y.S., Kim J.C. A case of crystalline keratopathy in monoclonal gammopathy of undetermined significance (MGUS) Korean J Ophthalmol. 2011;25(3):202–295. doi: 10.3341/kjo.2011.25.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ball N.J., Wickert W., Marx L.H., Thaell J.F. Crystalglobulinemia syndrome. A manifestation of multiple myeloma. Cancer. 1993;71(4):1231–1234. doi: 10.1002/1097-0142(19930215)71:4<1231::aid-cncr2820710410>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 7.Leung N., Buadi F.K., Song K.W., Magil A.B., Cornell L.D. A case of bilateral renal arterial thrombosis associated with cryocrystalglobulinaemia. NDT Plus. 2010;3(1):74–77. doi: 10.1093/ndtplus/sfp140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stone G.C., Wall B.A., Oppliger I.R. A vasculopathy with deposition of lambda light chain crystals. Ann Intern Med. 1989;110(4):275–278. doi: 10.7326/0003-4819-110-4-275. [DOI] [PubMed] [Google Scholar]
- 9.Gupta V., El Ters M., Kashani K., Leung N., Nasr S.H. Crystalglobulin-induced nephropathy. J Am Soc Nephrol. 2015;26(3):525–529. doi: 10.1681/ASN.2014050509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aucouturier P., Bauwens M., Khamlichi A.A. Monoclonal Ig L chain and L chain V domain fragment crystallization in myeloma-associated Fanconi's syndrome. J Immunol. 1993;150(8):3561–3568. [PubMed] [Google Scholar]
- 11.Hasegawa H. Aggregates, crystals, gels, and amyloids: intracellular and extracellular phenotypes at the crossroads of immunoglobulin physicochemical property and cell physiology. Int J Cell Biol. 2013;2013:604867. doi: 10.1155/2013/604867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schoengen A., Schreiner T., Anselstetter V. Cryocrystalglobulinemia: pH-dependent precipitation of a monoclonal IgG-kappa-immunoglobulin. Blut. 1989;58(5):255–260. doi: 10.1007/BF00320915. [DOI] [PubMed] [Google Scholar]
- 13.Tsuji T., Itoh Y., Nakamura T., Toyozumi Y., Arima N., Tsuda H. Crystalglobulinemia syndrome due to monoclonal gammopathy of renal significance. QJM. 2015;108(5):417–418. doi: 10.1093/qjmed/hcu114. [DOI] [PubMed] [Google Scholar]
- 14.Abe N., Tomita T., Bohgaki M., Kasahara H., Koike T. Crystalglobulinemia manifesting as chronic arthralgia and acute limb ischemia: a clinical case report. Medicine (Baltimore) 2017;96(16):e6643. doi: 10.1097/MD.0000000000006643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hasegawa H., Ozawa T., Tada N. Multiple myeloma-associated systemic vasculopathy due to crystalglobulin or polyarteritis nodosa. Arthritis Rheum. 1996;39(2):330–334. doi: 10.1002/art.1780390224. [DOI] [PubMed] [Google Scholar]
- 16.Hashimoto R., Toda T., Tsutsumi H., Ohta M., Mori M. Abnormal N-glycosylation of the immunoglobulin G kappa chain in a multiple myeloma patient with crystalglobulinemia: case report. Int J Hematol. 2007;85(3):203–206. doi: 10.1532/IJH97.06074. [DOI] [PubMed] [Google Scholar]
- 17.Mills L.E., Brettman L.R., Jentoft J.E., Viner E.D., Bernier G.M. Crystallocryoglobulinemia resulting from human monoclonal antibodies to albumin. Ann Intern Med. 1983;99(5):601–604. doi: 10.7326/0003-4819-99-5-601. [DOI] [PubMed] [Google Scholar]
- 18.DeLyria P.A., Avedschmidt S.E., Yamada C., Farkash E.A. Fatal cryocrystalglobulinemia with intravascular and renal tubular crystalline deposits. Am J Kidney Dis. 2016;67(5):787–791. doi: 10.1053/j.ajkd.2015.11.014. [DOI] [PubMed] [Google Scholar]
- 19.Nasr S.H., Galgano S.J., Markowitz G.S., Stokes M.B., D'Agati V.D. Immunofluorescence on pronase-digested paraffin sections: a valuable salvage technique for renal biopsies. Kidney Int. 2006;70(12):2148–2151. doi: 10.1038/sj.ki.5001990. [DOI] [PubMed] [Google Scholar]
- 20.Leung N. My patient with monoclonal gammopathy of undetermined significance has a kidney problem. J Onconephrol. 2017;1(1):18–23. [Google Scholar]