Abstract
Rationale & Objective
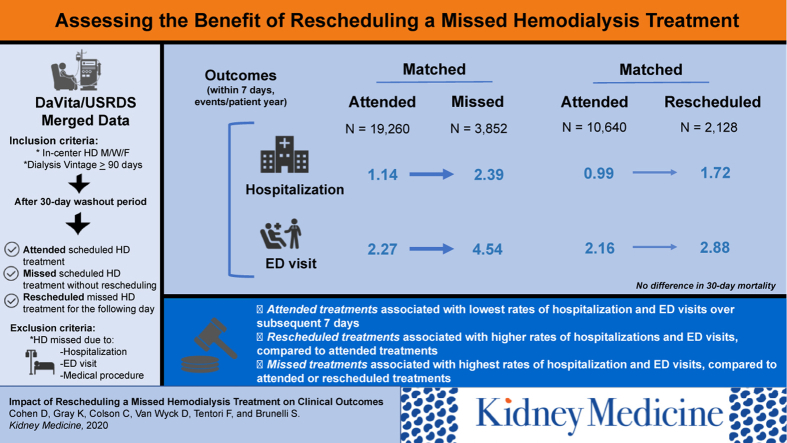
Among patients treated with in-center hemodialysis (HD), missed treatments are associated with higher subsequent rates of hospitalization and other adverse outcomes compared with attending treatment. The objective of this study was to determine whether and to what degree attending a rescheduled treatment on the day following a missed treatment ameliorates these risks.
Study Design
Retrospective, observational.
Setting & Participants
Included patients were those who were, as of any of 12 index dates during 2014, adult Medicare beneficiaries treated with in-center HD (vintage ≥ 90 days) on a Monday/Wednesday/Friday schedule.
Exposure
Treatment attendance on the index date and the subsequent day.
Outcomes
Hospital admissions, emergency department visits, mortality, blood pressure, and anemia measures, considered during the 7- and 30-day periods following exposure.
Analytical Approach
In parallel analyses, patients who missed or rescheduled treatment were each matched (1:5) to patients who attended treatment on the index date on the basis of index day of week and propensity score. Within the matched cohorts, outcomes were compared across exposures using repeated-measures generalized linear models.
Results
Compared with attending treatment (N = 19,260), a missed treatment (N = 3,852) was associated with a 2.09-fold higher rate of hospitalization in the subsequent 7 days; a rescheduled treatment (N = 2,128) was associated with a 1.68-fold higher rate of hospitalization than attending (N = 10,640). Compared with attending treatment, hospitalization rates were 1.39- and 1.28-fold higher among patients who missed and rescheduled treatment, respectively, during the 30-day outcome period. Emergency department visits followed a similar pattern of associations as hospitalization. No statistically significant associations were observed with respect to mortality for either missed or rescheduled treatments compared with attending treatment.
Limitations
Possible influence of unmeasured confounding; unknown generalizability to patients with non-Medicare insurance.
Conclusions
Attending a rescheduled in-center HD treatment attenuates but does not fully mitigate the adverse effects of a missed treatment.
Index Words: hemodialysis, treatment attendance, adherence, outcomes
Graphical abstract
Editorial, p. 3
In the United States, in-center hemodialysis (HD) is the most common treatment modality for patients with end-stage kidney disease and is currently used by almost 90% of prevalent dialysis patients.1 Despite the numerous advances made in the care of such patients during the past several decades, outcomes continue to be suboptimal. In recent years, intensive efforts have focused on improving outcomes by targeting areas such as the treatment of comorbid illnesses, management of the sequelae of end-stage kidney disease, and reduction in the use of central venous catheters for vascular access. Unfortunately, these efforts have had only a moderate impact on the hospitalization rate among in-center HD patients, which declined 14.2% from 2007 to 2014 but has remained fairly constant at approximately 1.7 admissions per patient-year since that time.1
In-center HD is a burdensome treatment regimen, with a typical schedule requiring patients to attend treatment 3 times per week (generally Monday/Wednesday/Friday or Tuesday/Thursday/Saturday) for several hours each session. In the context of such a demanding treatment regimen, it is unsurprising that in-center HD treatment attendance is imperfect, with missed treatments being fairly common. In the United States, approximately half of all missed treatments occur when the patient is admitted to the hospital2 and is receiving in-patient dialysis care. The rest of missed treatments occur when the patient is not admitted and thus represent a form of treatment nonadherence. This latter type of missed treatment is particularly common in the United States, where recent analyses indicate that patients miss treatment at a rate of approximately 8 treatments per year.2,3
Missed treatments that occur when the patient is not admitted to the hospital have significant implications with respect to clinical outcomes. They are associated with markedly higher rates of hospitalization,2, 3, 4, 5, 6 emergency department (ED) visits,4 and mortality.2,3,5, 6, 7, 8 Missed treatments are also associated with unfavorable anemia outcomes, including lower hemoglobin levels and higher erythropoiesis-stimulating agent (ESA) use.2,3 These adverse outcomes are likely due to the accumulation of excess fluid, electrolytes, and uremic toxins during the extended interdialytic interval imposed by the missed treatment.
Given that missed in-center HD treatments are common and their consequences are severe, interventions that mitigate their effects have the potential to significantly improve patient outcomes. Rescheduling a missed treatment for the subsequent day represents a logical intervention from a physiologic perspective. However, the degree to which rescheduling in this fashion can actually mitigate the effects of a missed treatment has not been examined. Because rescheduling treatments may be logistically difficult for both patients and providers, clearer understanding of the impact of this intervention is needed. In this retrospective observational study, we addressed this question by comparing a variety of clinical outcomes among contemporary in-center HD patients who: (1) attended treatment as scheduled, (2) missed treatment (for reasons other than hospitalization), and (3) missed treatment but attended a rescheduled treatment on the subsequent day.
Methods
Data Source and Time Period
All data for this study were derived from deidentified patient electronic health records that were merged directly to the US Renal Data System (USRDS) claims database without the need for probabilistic matching. A total of 12 index dates were considered, representing the Monday, Wednesday, and Friday of 4 weeks during calendar year 2014 (February 3, 5, and 7; May 5, 7, and 9; July 14, 16, and 18; and September 15, 17, and 19).
Because this study was conducted using deidentified patient data, according to title 45, part 46 of the US Department of Health and Human Services’ Code of Federal Regulations, it was deemed exempt from institutional review board or ethics committee approval (Quorum Institutional Review Board, Seattle, WA). We adhered to the Declaration of Helsinki, and informed consent was not required.
Patients, Exposures, and Matching
Included patients were those who, as of an index date, were 18 years or older, were receiving in-center HD on a Monday/Wednesday/Friday schedule at facilities that were participating providers with the DaVita Institute for Patient Safety Inc, had dialysis vintage of 90 days or longer, and were eligible for Medicare parts A and B with corresponding claims data. Monday/Wednesday/Friday patients were chosen to avoid the problem posed by missed treatments that occur on Saturdays (in which case next-day rescheduling may not be possible due to facility closures on Sundays). Medicare patients were chosen so that hospitalization events could be identified through linkage to claims data.
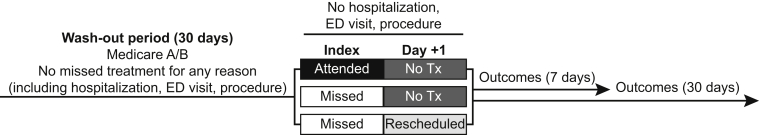
Because we were interested in the effects of a single missed treatment, we excluded patients who missed treatment due to hospitalization, ED visit, or outpatient medical procedure during the 2-day exposure window and those who missed treatment for any reason in the 30 days before the index date. In a sensitivity analysis, this final criterion was omitted such that patients were included irrespective of treatment history in the 30 days before index.
For each index date, patients were ascribed an exposure status based on their pattern of treatment attendance for the 2-day exposure period encompassing the index date and subsequent day (Fig 1). Patients who attended treatment on the index date and had no treatment on the subsequent day were designated as “attended.” Patients who missed treatment on the index date and had no treatment on the subsequent day were designated as “missed.” Patients who missed treatment on the index date but attended a treatment on the subsequent day were designated as “rescheduled.” An individual patient could be included in the study multiple times (ie, on multiple index dates) provided the patient met study inclusion/exclusion criteria on each index date considered.
Figure 1.
Study schema. A schematic representation of the study is shown. In the 30 days before the index date, eligible patients were required to have Medicare parts A and B claims availability and no missed treatments for any reason. Eligible patients were ascribed an exposure status based on their pattern of treatment attendance on the index date and following day. Outcomes were considered over the 7- and 30-day periods following exposure assignment. Abbreviations: ED, emergency department; Tx, treatment.
Patients who attended treatment on an index date were matched 5:1 to patients who missed treatment. Separately, patients who attended treatment were matched 5:1 to patients who rescheduled treatment. In both cases, patients were hard-matched on the day of the week of the index date (Monday, Wednesday, or Friday) and on the basis of propensity scores generated using a model that considered the following covariates: age, sex, race, cause, access type, Charlson Comorbidity Index score, and dialysis vintage; history of anxiety/depression, hepatitis C, diabetes, congestive heart failure, and peripheral vascular disease; and transferrin saturation, parathyroid hormone, serum phosphorus, ferritin, creatinine, calcium, albumin, Kt/V, and normalized protein catabolic rate values. Within strata defined by day of week, patients were caliper matched based on logit propensity score (the caliper width was set to equal 0.2 standard deviation of the logit propensity score difference); a 5:1 variable matching ratio was selected on the basis of the relative number of available patients who attended versus missed or rescheduled treatment.
Outcomes and Statistical Analysis
Patient characteristics were summarized as mean ± standard deviation, median and interquartile range, or count and proportion, as appropriate. Standardized differences were calculated according to standard methods9; standardized differences with an absolute value ≤10% are considered indicative of satisfactory covariate balance. Comparisons across exposure categories were made using t tests, χ2 tests, or Kruskal-Wallis tests, as appropriate.
Outcomes were considered during the 7- and 30-day periods following exposure assignment or until censoring for death, transplantation, withdrawal from dialysis, renal recovery, modality change, or loss to follow-up. Primary outcomes, ascertained from Medicare claims data, were hospitalization, ED visits, and mortality. Secondary outcomes, ascertained from electronic health records, were predialysis systolic blood pressure, hemoglobin measurements, and ESA use.
All comparisons were performed within the matched cohorts. Comparisons between exposure groups were made using repeated-measures generalized linear models (to account for the fact that an individual patient might contribute multiple observations to the study). Count outcomes (hospitalizations and ESA doses) were estimated using negative binomial models (log link, negative binomial distribution), continuous outcomes (potassium, hemoglobin, systolic blood pressure, and ESA dose per treatment) were estimated using linear models (identity link, normal distribution), and mortality was estimated using a generalized estimating equation (logit link, binary distribution). Comparisons between patients who attended versus rescheduled their treatment were further adjusted for baseline ferritin and transferrin saturation values; comparisons between patients who attended versus missed their treatment had no additional adjustments. All matching and analyses were performed using SAS, version 9.4 (SAS Institute, Inc).
Results
Patient Characteristics
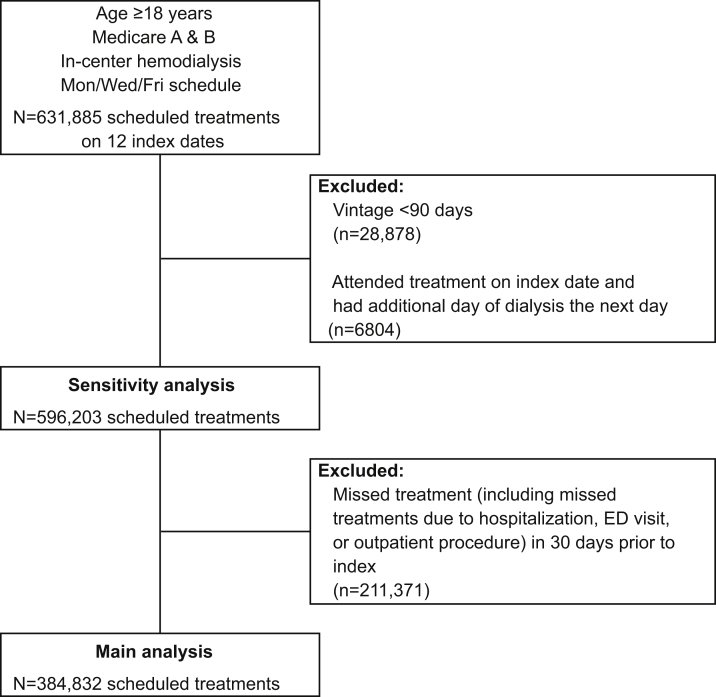
Of 384,832 scheduled treatments that met inclusion criteria for the main analysis (Fig 2), 378,391 were attended as scheduled, 4,141 were missed, and 2,300 were rescheduled for the following day. Before matching, patients who missed treatment on the index date were younger, more likely to use a central venous catheter for vascular access, and of newer dialysis vintage compared with patients who attended treatment. Less pronounced imbalances were also observed for a variety of other characteristics (Table 1). Patients who rescheduled treatment were likewise younger and of newer dialysis vintage compared with patients who attended treatment. Those who rescheduled were also somewhat more likely to be of white race and had slightly lower values for ferritin and transferrin saturation. After matching, all characteristics were well balanced between patients who missed treatment (N = 3,852) and matched patients who attended treatment (N = 19,260; Table 2). Likewise, after matching, all characteristics were well balanced between patients who rescheduled treatment (N = 2,128) and matched patients who attended treatment (N = 10,640; Table 2), with the exception of ferritin and transferrin saturation values. Subsequent comparisons between patients who rescheduled and those who attended were adjusted for these 2 variables.
Figure 2.
Study flow diagram. Selection of scheduled treatments meeting study inclusion/exclusion criteria for the main and sensitivity analyses is shown. Abbreviation: ED, emergency department.
Table 1.
Baseline Characteristics of Patients Who Attended, Missed, or Rescheduled Treatment, Before Matching
| Attended (N = 378,391) | Missed (N = 4,141) | Standardized Difference, %a | Pa | Rescheduled (N = 2,300) | Standardized Difference, %a | Pa | |
|---|---|---|---|---|---|---|---|
| Age, y | 63.2 ± 14.2 | 61.4 ± 13.9 | −12.9 | <0.001 | 61.3 ± 14.9 | −13.5 | <0.001 |
| Female sex | 162,957 (43.1%) | 1,903 (46.0%) | 5.8 | <0.001 | 1,080 (47.0%) | 7.8 | <0.001 |
| Race | <0.001 | <0.001 | |||||
| White | 144,235 (38.1%) | 1,645 (39.7%) | 3.3 | 988 (43.0%) | 9.9 | ||
| African American | 139,767 (36.9%) | 1,623 (39.2%) | 4.6 | 838 (36.4%) | −1.0 | ||
| Hispanic | 64,250 (17.0%) | 614 (14.8%) | −5.9 | 324 (14.1%) | −8.0 | ||
| Asian | 14,259 (3.8%) | 82 (2.0%) | −10.7 | 68 (3.0%) | −4.5 | ||
| Other/unknown | 15,880 (4.2%) | 177 (4.3%) | 0.4 | 82 (3.6%) | −3.3 | ||
| Vascular access | <0.001 | <0.001 | |||||
| AVF | 269,618 (71.3%) | 2,790 (67.4%) | −8.4 | 1,533 (66.7%) | −10.0 | ||
| AVG | 76,868 (20.3%) | 866 (20.9%) | 1.5 | 534 (23.2%) | 7.0 | ||
| CVC | 31,899 (8.4%) | 485 (11.7%) | 10.9 | 233 (10.1%) | 5.9 | ||
| Dialysis vintage, mo | 50 [25-84] | 45 [22-79] | −8.4 | <0.001 | 46 [22-80.5] | −5.5 | <0.001 |
| Body weight, kg | 81.8 ± 22.7 | 81.9 ± 22.2 | 0.6 | 0.72 | 83.4 ± 23.6 | 6.9 | <0.001 |
| Cause of ESRD | 0.07 | 0.02 | |||||
| Diabetes | 170,028 (44.9%) | 1,856 (44.8%) | −0.2 | 1,043 (45.3%) | 0.8 | ||
| Hypertension | 117,555 (31.1%) | 1,234 (29.8%) | −2.8 | 660 (28.7%) | −5.2 | ||
| Other | 90,808 (24.0%) | 1,051 (25.4%) | 3.2 | 597 (26.0%) | 4.5 | ||
| Diabetes | 259,732 (68.6%) | 2,815 (68.0%) | −1.4 | 0.36 | 1,616 (70.3%) | 3.5 | 0.10 |
| CHF | 67,712 (17.9%) | 768 (18.5%) | 1.7 | 0.28 | 457 (19.9%) | 5.0 | 0.01 |
| Anxiety/depression | 24,602 (6.5%) | 316 (7.6%) | 4.4 | 0.003 | 196 (8.5%) | 7.7 | <0.001 |
| Hepatitis C | 3,224 (0.9%) | 56 (1.4%) | 4.8 | <0.001 | 21 (0.9%) | 0.7 | 0.75 |
| PVD | 29,429 (7.8%) | 328 (7.9%) | 0.5 | 0.73 | 186 (8.1%) | 1.1 | 0.58 |
| Albumin, g/dL | 3.9 ± 0.4 | 3.9 ± 0.4 | −6.6 | <0.001 | 3.9 ± 0.4 | −6.2 | 0.003 |
| Calcium, mg/dL | 9.0 ± 0.7 | 9.0 ± 0.7 | −0.4 | 0.79 | 8.9 ± 0.7 | −4.3 | 0.04 |
| Phosphate, mg/d | 5.1 ± 1.5 | 5.2 ± 1.5 | 3.4 | 0.03 | 5.2 ± 1.5 | 6.8 | <0.001 |
| PTH, pg/mL | 349 [231-522] | 352 [229-519] | 2.3 | 0.61 | 363.5 [236-547] | 4.1 | 0.004 |
| Ferritin, ng/mL | 741 ± 349 | 722 ± 368 | −5.3 | <0.001 | 703 ± 350 | −10.9 | <0.001 |
| TSAT, % | 30.3 ± 12.5 | 30.0 ± 12.8 | −2.6 | 0.09 | 29.0 ± 12.0 | −10.4 | <0.001 |
| Hemoglobin, g/dL | 11.0 ± 1.1 | 11.0 ± 1.2 | 1.2 | 0.43 | 11.0 ± 1.2 | −1.6 | 0.44 |
| Creatinine, mg/dL | 8.9 ± 3.0 | 8.6 ± 3.1 | −8.3 | <0.001 | 8.8 ± 3.2 | −2.1 | 0.32 |
| Kt/V | 1.6 ± 0.3 | 1.6 ± 0.3 | −8.1 | <0.001 | 1.6 ± 0.3 | −5.6 | 0.007 |
| nPCR, g/kg/d | 1.03 ± 0.28 | 0.98 ± 0.28 | −19.3 | <0.001 | 1.03 ± 0.29 | −1.1 | 0.59 |
Note: Values for categorical variables are given as number (percent), and continuous variables are given as mean ± standard deviation or median [interquartile range]. Conversion factors for units: calcium in mg/dL to mmol/L, ×0.2495; creatinine in mg/dL to μmol/L, ×88.4.
Abbreviations: AVF, arteriovenous fistula; AVG, arteriovenous graft; CHF, congestive heart failure; CVC, central venous catheter; ESRD, end-stage renal disease; nPCR, normalized protein catabolic rate; PTH, parathyroid hormone; PVD, peripheral vascular disease; TSAT, transferrin saturation.
Versus attended.
Table 2.
Baseline Characteristics of Patients Who Attended, Missed, or Rescheduled Treatment, After Matching
| Attended (N = 19,260) | Missed (N = 3,852) | Standardized Difference, %a | Pa | Attended (N = 10,640) | Rescheduled (N = 2,128) | Standardized Difference, %a | Pa | |
|---|---|---|---|---|---|---|---|---|
| Age, y | 61.4 ± 14.6 | 61.5 ± 13.8 | 0.6 | 0.73 | 61.4 ± 14.7 | 61.3 ± 14.8 | −0.8 | 0.73 |
| Female sex | 8,901 (46.2%) | 1,773 (46.0%) | −0.4 | 0.83 | 4,995 (46.9%) | 994 (46.7%) | −0.5 | 0.84 |
| Race | 0.87 | 0.83 | ||||||
| White | 7,544 (39.2%) | 1,515 (39.3%) | 0.3 | 4,616 (43.4%) | 911 (42.8%) | −1.2 | ||
| African American | 7,605 (39.5%) | 1,510 (39.2%) | −0.6 | 3,919 (36.8%) | 778 (36.6%) | −0.6 | ||
| Hispanic | 2,851 (14.8%) | 583 (15.1%) | 0.9 | 1,408 (13.2%) | 296 (13.9%) | 2.0 | ||
| Asian | 439 (2.3%) | 78 (2.0%) | −1.8 | 347 (3.3%) | 66 (3.1%) | −0.9 | ||
| Other/unknown | 821 (4.3%) | 166 (4.3%) | 0.2 | 350 (3.3%) | 77 (3.6%) | 1.8 | ||
| Vascular access | 0.97 | 0.83 | ||||||
| AVF | 12,945 (67.2%) | 2,595 (67.4%) | 0.3 | 7,111 (66.8%) | 1,414 (66.4%) | −0.8 | ||
| AVG | 4,073 (21.1%) | 808 (21.0%) | −0.4 | 2,398 (22.5%) | 492 (23.1%) | 1.4 | ||
| CVC | 2,242 (11.6%) | 449 (11.7%) | 0.0 | 1,131 (10.6%) | 222 (10.4%) | −0.6 | ||
| Dialysis vintage, mo | 46 [22-79] | 45.5 [22-78] | 0.0 | 0.50 | 46 [23-80] | 46 [22-80] | −0.3 | 0.30 |
| Body weight, kg | 81.8 ± 22.8 | 81.7 ± 22.2 | −0.3 | 0.85 | 83.0 ± 23.4 | 83.0 ± 23.3 | 0.2 | 0.92 |
| Cause of ESRD | 0.78 | 0.81 | ||||||
| Diabetes | 8,731 (45.3%) | 1,731 (44.9%) | −0.8 | 4,812 (45.2%) | 963 (45.3%) | 0.1 | ||
| Hypertension | 5,595 (29.0%) | 1,141 (29.6%) | 1.3 | 3,127 (29.4%) | 613 (28.8%) | −1.3 | ||
| Other | 4,934 (25.6%) | 980 (25.4%) | −0.4 | 2,701 (25.4%) | 552 (25.9%) | 1.3 | ||
| Diabetes | 13,146 (68.3%) | 2,627 (68.2%) | −0.1 | 0.94 | 7,507 (70.6%) | 1,490 (70.0%) | −1.2 | 0.62 |
| CHF | 3,575 (18.6%) | 722 (18.7%) | 0.5 | 0.79 | 2,079 (19.5%) | 416 (19.5%) | 0 | >0.99 |
| Anxiety/depression | 1,478 (7.7%) | 303 (7.9%) | 0.7 | 0.68 | 917 (8.6%) | 182 (8.6%) | −0.2 | 0.92 |
| Hepatitis C | 167 (0.9%) | 53 (1.4%) | 4.8 | 0.003 | 102 (1.0%) | 18 (0.8%) | −1.2 | 0.62 |
| PVD | 1,547 (8.0%) | 308 (8.0%) | −0.1 | 0.94 | 911 (8.6%) | 175 (8.2%) | −1.2 | 0.61 |
| Albumin, g/dL | 3.8 ± 0.4 | 3.8 ± 0.4 | −0.1 | 0.94 | 3.8 ± 0.4 | 3.8 ± 0.4 | 0.3 | 0.89 |
| Calcium, mg/dL | 9.0 ± 0.7 | 9.0 ± 0.7 | −0.2 | 0.92 | 8.9 ± 0.7 | 8.9 ± 0.7 | −0.4 | 0.86 |
| Phosphate, mg/dL | 5.2 ± 1.5 | 5.2 ± 1.5 | −1.1 | 0.53 | 5.2 ± 1.5 | 5.2 ± 1.5 | 0.6 | 0.81 |
| PTH, pg/mL | 349 [229-528] | 350 [228-517] | −0.1 | 0.90 | 356 [230-532] | 361 [236-546.5] | 0.9 | 0.13 |
| Ferritin, ng/mL | 722 ± 352 | 720 ± 361 | −0.7 | 0.67 | 726 ± 348 | 702 ± 348 | −6.9 | 0.004 |
| TSAT, %, | 29.9 ± 12.5 | 29.9 ± 12.8 | −0.4 | 0.84 | 30.1 ± 12.6 | 29.1 ± 12.0 | −7.8 | 0.001 |
| Hemoglobin, g/dL | 11.0 ± 1.1 | 11.0 ± 1.2 | −0.4 | 0.82 | 11.0 ± 1.1 | 11.0 ± 1.1 | −0.3 | 0.90 |
| Creatinine, mg/dL | 8.7 ± 3.0 | 8.6 ± 3.0 | −1.1 | 0.54 | 8.8 ± 3.1 | 8.8 ± 3.1 | 0.2 | 0.94 |
| Kt/V | 1.6 ± 0.3 | 1.6 ± 0.3 | 0 | 0.98 | 1.6 ± 0.3 | 1.6 ± 0.3 | −0.4 | 0.87 |
| nPCR, g/kg/d | 0.98 ± 0.27 | 0.98 ± 0.28 | 0.2 | 0.92 | 1.03 ± 0.28 | 1.03 ± 0.28 | −0.7 | 0.76 |
Note: Values for categorical variables are given as number (percent), and continuous variables are given as mean ± standard deviation or median [interquartile range]. Conversion factors for units: calcium in mg/dL to mmol/L, ×0.2495; creatinine in mg/dL to μmol/L, ×88.4.
Abbreviations: AVF, arteriovenous fistula; AVG, arteriovenous graft; CHF, congestive heart failure; CVC, central venous catheter; ESRD, end-stage renal disease; nPCR, normalized protein catabolic rate; PTH, parathyroid hormone; PVD, peripheral vascular disease; TSAT, transferrin saturation.
Versus attended.
Primary Outcomes
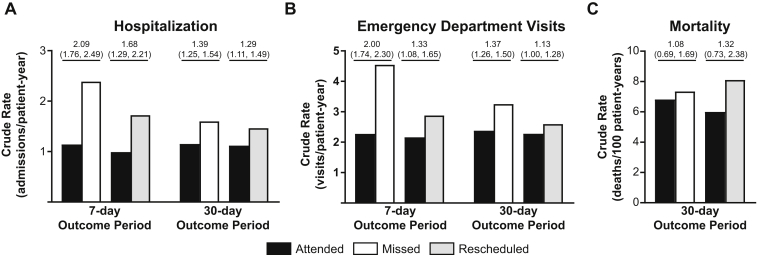
During the 7 days following exposure assignment, a missed treatment was associated with an annualized hospitalization rate of 2.39 admissions/patient-year versus a rate of 1.14 admissions/patient-year for attending treatment (Table S1), corresponding to an incidence rate ratio (IRR) of 2.09 (95% confidence interval [CI], 1.76-2.49), referent to attending treatment (Fig 3A). During the same outcome period, a rescheduled treatment was associated with a hospitalization rate of 1.72 admissions/patient-year versus 0.99 admissions/patient-year for attending treatment, corresponding to an IRR of 1.68 (95% CI, 1.29-2.21), referent to attending treatment. Similar, if somewhat less potent, associations were observed during the 30-day outcome window, during which a missed treatment was associated with a 1.39-fold higher rate of hospitalization compared with attending treatment, and a rescheduled treatment was associated with a 1.29-fold higher rate.
Figure 3.
Primary outcomes by treatment attendance status. (A) Crude hospitalization rates per patient-year are plotted for the indicated outcome periods following an attended treatment (black bars), a missed treatment (white bars), or a rescheduled treatment (grey bars). Corresponding incidence rate ratios (95% confidence intervals) are shown above each pair of bars. (B) As for A but show the outcome of emergency department visits. (C) As for A but show mortality rate per 100 patient-years. Corresponding odds ratios (95% confidence intervals) are shown above each pair of bars.
A similar pattern of associations was observed with respect to ED visits (Fig 3B). During the 7 days following exposure assignment, a missed treatment was associated with an ED visit rate of 4.54 visits/patient-year versus 2.27 visits/patient-year for attending treatment, corresponding to an IRR of 2.00 (95% CI, 1.74-2.30), referent to attending treatment. During the same outcome period, a rescheduled treatment was associated with an ED visit rate of 2.88 visits/patient-year versus 2.16 visits/patient year for attending treatment, corresponding to an IRR of 1.33 (95% CI, 1.08-1.65). Similar associations were observed during the 30-day outcome window, during which a missed treatment was associated with a 1.37-fold higher rate of ED visits compared with attending treatment, and a rescheduled treatment was associated with a 1.13-fold higher rate.
Mortality could not be evaluated during the 7-day outcome window due to a paucity of events. During the 30-day outcome window (Fig 3C), mortality rates were 7.34 and 6.81 deaths/100 patient-years among those who missed and attended treatment, respectively. This difference was not statistically significant (odds ratio of 1.08 [95% CI, 0.69-1.69] referent to attending treatment). Likewise, mortality rates during the 30-day outcome window were 8.10 and 6.00 deaths/100 patient-years among patients who rescheduled and attended treatment, respectively. This difference was not statistically significant (odds ratio, 1.32 [95% CI, 0.73-2.38]).
Secondary Outcomes
During the 7-day outcome period (Table 3), a missed treatment was associated with higher predialysis systolic blood pressure (mean difference, 3.36 [95% CI, 2.54-4.18] mm Hg) than attending treatment. This trend was less potent but remained statistically significant during the 30-day outcome period (mean difference, 1.75 [95% CI, 1.02-2.48] mm Hg). No statistically significant differences were observed between rescheduled versus attended treatments with respect to systolic blood pressure during either the 7- or 30-day outcome windows.
Table 3.
Secondary Outcomes by Treatment Attendance Status
| Attended Mean (95% CI) | Missed Mean (95% CI) | Comparison (95% CI)a | Attended Mean (95% CI) | Rescheduled Mean (95% CI) | Comparison (95% CI)a | |
|---|---|---|---|---|---|---|
| 7-d Outcome Period | ||||||
| Predialysis systolic blood pressure, mm Hg | 147 (147 to 148) | 151 (150 to 152) | 3.36 (2.54 to 4.18) | 147 (147 to 148) | 146 (145 to 147) | −0.76 (−1.86 to 0.35) |
| 30-d Outcome Period | ||||||
| Predialysis systolic blood pressure, mm Hg | 147 (147 to 147) | 149 (148 to 150) | 1.75 (1.02 to 2.48) | 147 (146 to 147) | 147 (146 to 147) | −0.25 (−1.25 to 0.75) |
| Hemoglobin, mg/dL | 11.0 (11.0 to 11.0) | 10.8 (10.7 to 10.8) | −0.22 (−0.26 to −0.18) | 11.0 (11.0 to 11.0) | 10.9 (10.8 to 10.9) | −0.12 (−0.17 to −0.07) |
| ESA | ||||||
| Administrations/pt-y | 95.9 (95.1 to 96.8) | 93.6 (91.8 to 95.4) | 0.98 (0.96 to 1.00) | 97.7 (96.6 to 98.8) | 95.5 (93.1 to 98.0) | 0.98 (0.95 to 1.01) |
| Dose, U/treatment | 4,418 (4,364 to 4,472) | 4,607 (4,480 to 4,734) | 188 (53 to 324) | 4,425 (4,353 to 4,497) | 4,484 (4,321 to 4,646) | 58 (−118 to 234) |
Abbreviations: CI, confidence interval; ESA, erythropoiesis stimulating agent; pt, patient.
Comparison for ESA administrations is incidence rate ratio; all others are mean difference. All comparisons are expressed referent to “Attended.”
During the 30-day outcome period, a missed treatment was associated with lower mean hemoglobin values compared with attending treatment (mean difference, −0.22 [95% CI, −0.26 to −0.18] g/dL). During the same outcome period, a rescheduled treatment was also associated with lower mean hemoglobin levels than attending treatment, although the difference was less pronounced (mean difference, −0.12 [95% CI, −0.17 to −0.07]). A missed treatment was associated with a higher ESA dose per treatment (mean difference, 188 [95% CI, 53-324] U/treatment) compared with attending. No statistically significant difference in ESA dose per treatment was detected between attending versus rescheduled treatments. The rate of ESA administrations per patient-year was not associated with treatment attendance pattern in either comparison.
Sensitivity Analysis
The analyses described considered only patients who did not miss treatment for any reason (including hospitalization) in the 30 days before index. In a sensitivity analysis, all patients meeting the study inclusion criteria were considered irrespective of their treatment attendance pattern in the 30 days before index (Fig 1). In this expanded cohort (N = 596,203 scheduled treatments; Tables S2 and S3), associations between treatment attendance patterns at index (attended, missed, and rescheduled) and the outcomes of hospitalization and ED visits were similar to those observed in the main analysis (Fig S1A and B; Tables S4 and S5). However, in the sensitivity analysis, a missed treatment was associated with a significantly higher risk for death than attending treatment (odds ratio, 1.37 [95% CI, 1.12-1.67]; Fig S1C), whereas no significant association was detected with respect to a rescheduled treatment versus attending treatment (odds ratio, 1.23 [95% CI, 0.89-1.70]).
Discussion
This study, which separately compared outcomes following either a rescheduled or a missed treatment versus attending treatment, found that compared with attending treatment, a missed treatment was associated with a significantly higher rate of hospitalization and ED visits. Although rescheduling a missed treatment to the subsequent day was still associated with higher rates of these 2 outcomes than attending treatment, the magnitude of the elevation in rate appeared to be less pronounced in the context of a rescheduled treatment compared with a missed treatment. A similar pattern of associations was observed with respect to blood pressure, hemoglobin level, and ESA use. In each case, a missed treatment was associated with less favorable outcomes compared with attending treatment, and these outcomes were less unfavorable when the index missed treatment was rescheduled. Together, these findings suggest that the risk imposed by a missed treatment was partially mitigated (ie, of quantitatively lower magnitude) when the missed treatment was rescheduled, presumably through the removal of excess fluid and uremic toxins that would otherwise persist until the next scheduled in-center HD treatment.
The main analysis presented in this study was designed to isolate the impact of treatment attendance patterns on the index date and the subsequent day. To that end, patients with a missed treatment for any reason (including hospitalization) in the 30 days before the index date were excluded. This criterion likely selected for patients who were healthier and/or had better overall treatment adherence patterns than the population as a whole, as suggested by the relatively low rates of hospitalization and mortality observed among controls in this selected cohort. The hospitalization and mortality rates observed in the sensitivity analysis, which eliminated the requirement for perfect treatment attendance before the index date, were much more comparable to the current US in-center HD population as a whole.1 Nonetheless, the associations detected between treatment attendance patterns and outcomes were similar between the 2 cohorts, suggesting that the benefits of rescheduling a missed treatment may be significant regardless of a patient’s treatment history in the period leading up to any individual missed treatment.
Our findings suggest that improving primary adherence through the avoidance of missed treatments represents a more potent approach for improving outcomes than rescheduling treatments when they have been missed. Significant opportunity exists for improving treatment adherence insofar as nonadherence to the dialysis schedule has been persistently more common in the United States than in other developed countries.3,10 However, the fact that missed treatment rates in the United States have remained consistently high despite a clear understanding of the risks imposed by missed treatments underscores the challenges inherent to improving treatment adherence. Missed treatments may arise due to a range of causes,4 some of which may be difficult to mitigate. Lower health literacy may also contribute to poor treatment adherence.11 Given the long-standing difficulty achieving substantial improvements in the missed treatment rate, rescheduling missed treatments for the next day represents a relatively straightforward intervention that may markedly improve patient outcomes.
This study should be interpreted in the context of its limitations. This study was limited to Medicare patients due to data availability; generalizability to patients with other insurance types is not known. Only patients who dialyzed on a Monday/Wednesday/Friday schedule were considered. The implications of a missed treatment occurring on the Saturday of a Tuesday/Thursday/Saturday schedule, when opportunities to reschedule for Sunday may be very limited, are not addressed by the current work. To minimize potential confounding, we used a matched study design, matching in parallel patients who missed treatment and patients who rescheduled treatment with controls who attended dialysis as scheduled. This approach precluded a direct statistical comparison of the outcomes following a missed versus a rescheduled treatment; this comparison must therefore be triangulated indirectly by comparison to a common referent. Although this consequence is not ideal, we deemed it necessary to maximize the internal validity of our findings. As is the case for all retrospective observational studies, residual confounding may have influenced these findings. We report associations only; cause and effect are not determined.
In conclusion, this study demonstrates that attending a rescheduled treatment on the day following a missed treatment is associated with prognostic implications that are numerically less unfavorable than those of missing a treatment outright, both compared to attending treatment as scheduled. Thus, while improving primary treatment adherence among in-center HD patients remains a priority, efforts to reschedule otherwise missed treatments may improve patient outcomes. Efforts to raise awareness among patients and providers about the risks of missing treatment and the benefits of rescheduling a missed treatment when possible represent critical steps in this regard.
Article Information
Authors’ Full Names and Academic Degrees
Dena E. Cohen, PhD, Kathryn S. Gray, MS, Carey Colson, MBA, David B. Van Wyck, MD, Francesca Tentori, MD, MS, and Steven M. Brunelli, MD, MSCE.
Authors’ Contributions
Research idea and study design: DEC, KSG, SMB; data acquisition: CC; data analysis/interpretation: DEC, KSG, SMB, DBVW, FT; statistical analysis: KSG. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
None.
Financial Disclosure
Dr Cohen, Ms Gray, Ms Colson, and Drs Tentori and Brunelli are employees of DaVita Clinical Research, a contractor to the DaVita Institute for Patient Safety. Dr Brunelli’s spouse is an employee of AstraZeneca. Dr Van Wyck is an employee of DaVita, Inc, owns stock therein, and performs services for the DaVita Institute for Patient Safety through a workforce sharing agreement with DaVita, Inc.
Acknowledgements
This publication is the result of a research project conducted by the DaVita Institute for Patient Safety, Inc, a federally listed Patient Safety Organization, and is published with its permission. The data discussed here have been certified as nonidentifiable pursuant to 42 CFR 3.212 (a; 1). DaVita Clinical Research is a contractor to the DaVita Institute for Patient Safety, Inc. The data reported here were supplied by the USRDS.
Disclaimer
The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the US government.
Prior Presentation
A portion of these findings were presented at the American Society for Nephrology Kidney Week 2018; San Diego, CA; October 25-28, 2018.
Peer Review
Received April 10, 2019. Evaluated by 2 external peer reviewers, with direct editorial input from the Statistical Editor and the Editor-in-Chief. Accepted in revised form October 6, 2019.
Footnotes
Complete author and article information provided before references.
Figure S1: Primary outcomes by treatment attendance status
Table S1: Summary of Primary Outcomes for Main Analysis
Table S2: Baseline Characteristics of Patients Who Attended, Missed, or Rescheduled Treatment, Before Matching
Table S3: Baseline Characteristics of Patients Who Attended, Missed, or Rescheduled Treatment, After Matching
Table S4: Summary of Primary Outcomes for Sensitivity Analysis
Table S5: Secondary Outcomes by Treatment Attendance Status
Supplementary Material
Figure S1; Tables S1-S5.
References
- 1.Saran R., Li Y., Robinson B. US Renal Data System 2015 Annual Data Report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2016;l67(3 suppl 1):S1–S434. doi: 10.1053/j.ajkd.2015.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gray K.S., Cohen D.E., Brunelli S.M. In-center hemodialysis absenteeism: prevalence and association with outcomes. Clinicoecon Outcomes Res. 2017;9:307–315. doi: 10.2147/CEOR.S136577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al Salmi I., Larkina M., Wang M. Missed hemodialysis treatments: international variation, predictors, and outcomes in the Dialysis Outcomes and Practice Patterns Study (DOPPS) Am J Kidney Dis. 2018;72(5):634–643. doi: 10.1053/j.ajkd.2018.04.019. [DOI] [PubMed] [Google Scholar]
- 4.Chan K.E., Thadhani R.I., Maddux F.W. Adherence barriers to chronic dialysis in the United States. J Am Soc Nephrol. 2014;25(11):2642–2648. doi: 10.1681/ASN.2013111160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Obialo C.I., Hunt W.C., Bashir K., Zager P.G. Relationship of missed and shortened hemodialysis treatments to hospitalization and mortality: observations from a US dialysis network. Clin Kidney J. 2012;5(4):315–319. doi: 10.1093/ckj/sfs071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saran R., Bragg-Gresham J.L., Rayner H.C. Nonadherence in hemodialysis: associations with mortality, hospitalization, and practice patterns in the DOPPS. Kidney Int. 2003;64(1):254–262. doi: 10.1046/j.1523-1755.2003.00064.x. [DOI] [PubMed] [Google Scholar]
- 7.Leggat J.E., Jr., Orzol S.M., Hulbert-Shearon T.E. Noncompliance in hemodialysis: predictors and survival analysis. Am J Kidney Dis. 1998;32(1):139–145. doi: 10.1053/ajkd.1998.v32.pm9669435. [DOI] [PubMed] [Google Scholar]
- 8.Unruh M.L., Evans I.V., Fink N.E., Powe N.R., Meyer K.B. Skipped treatments, markers of nutritional nonadherence, and survival among incident hemodialysis patients. Am J Kidney Dis. 2005;46(6):1107–1116. doi: 10.1053/j.ajkd.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 9.Austin P.C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bleyer A.J., Hylander B., Sudo H. An international study of patient compliance with hemodialysis. JAMA. 1999;281(13):1211–1213. doi: 10.1001/jama.281.13.1211. [DOI] [PubMed] [Google Scholar]
- 11.Green J.A., Mor M.K., Shields A.M. Associations of health literacy with dialysis adherence and health resource utilization in patients receiving maintenance hemodialysis. Am J Kidney Dis. 2013;62(1):73–80. doi: 10.1053/j.ajkd.2012.12.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1; Tables S1-S5.