Abstract
Background:
Prognostic value of Oncotype DX Breast Recurrence Score (RS) in male breast cancer patients is understudied. We evaluated associations of RS with overall mortality in male breast cancer patients and compared it to female counterparts.
Methods:
With a cohort of 848 male and 110,898 female breast cancer patients identified from the National Cancer Database (2010–2014), we estimated hazard ratios (HR) and 95% confidence intervals (CI) for overall mortality associated with RS using Cox regression models. RS was evaluated continuously, as well as by categorization following respective traditional (≤17, 18–30, ≥31) and TAILORx (≤10, 11–25, ≥26) cutoffs.
Results:
RS was positively associated with mortality in male patients (HR=1.13, 95%CI: 1.02 to 1.26 per unit RS increment) up to RS >21, after which the risk plateaued. Among female patients, mortality began to increase with RS only when RS >23 (HR=1.02, 95%CI: 1.01 to 1.02 per unit of RS increment). The intermediate- (HR=5.37, 95%CI: 1.79 to 16.11) and high-risk diseases (HR=4.28, 95%CI: 1.22 to 14.97) defined by TAILORx, but not traditional cutoffs established for female patients, were associated with elevated mortality risk in men even after adjustment for demographic, clinical characteristics and treatments, except chemotherapy.
Conclusion:
RS is associated with mortality in male breast cancer patients at a much lower threshold than that for female patients. Studies are needed to establish specific guidelines for RS thresholds for male breast cancer patients.
Keywords: Breast neoplasms, Male, Recurrence score, Prognosis, Mortality, Survival
Introduction
The Oncotype DX Breast Recurrence Score (RS) is a 21-gene marker based on expression of 16 tumor-associated genes and 5 reference genes, which was initially developed to quantify the likelihood of distant recurrence in female patients with estrogen receptor-positive (ER+) and node-negative breast cancer, with a high RS indicating a higher risk of distant recurrence (1). Since its development, the predictive and prognostic values of RS in female breast cancer patients have been validated in several prospective clinical trials, including the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-20 trial, Southwest Oncology Group (SWOG)-8814 trial, and Trial Assigning Individualized Options for Treatment (TAILORx) (2–5). Currently, RS is recommended in clinical practice to guide decisions on adjuvant systemic therapy for women with early-stage invasive breast cancer, especially for those who present with ER+, human epidermal growth factor receptor 2-negative (HER2-), and node–negative diseases (6).
For male patients with breast cancer, who account for approximately 1% of all breast cancers, diagnostic and treatment approaches are in large part based on evidence generated from female patients (7). A vast majority of male breast cancer patients are characterized with ER+ or progesterone receptor-positive (PR+), as well as HER2- diseases, in accordance to indications of RS testing (8). However, it has not been well investigated whether RS is predictive to treatment efficacy and/or prognosis among men with breast cancer.
It has been suggested that male breast cancer may have a different etiology/biology from that of female (9). A recent study, which included 322 male breast cancer patients from the Surveillance, Epidemiology, and End Results (SEER) Program, revealed that male breast cancer patients with higher RS had worse crude survival than those with lower RS (10), though the independent predictive or prognostic values of RS in men were not evaluated.
To fill this knowledge gap, we examined the association between RS and overall mortality in male breast cancer patients using data from the National Cancer Database (NCDB) and compared it to that of female patients.
Methods
Patients with a primary breast cancer diagnosis and RS testing between 2010 and 2014 were identified from the NCDB, which captures 70% of newly diagnosed cancers each year across the United States (U.S.). Patients with ER+, HER2- and stage I or II invasive breast cancers between 2010 and 2014 were included. Patients who received no surgery (n=23) were excluded (Figure 1). Because only completely de-identified information was provided by the NCDB, this study was approved by the Vanderbilt University Medical Center Institutional Review Board as a human subject exempt project, for which no informed consent is needed. This study was conducted in accordance with the Declaration of Helsinki.
Figure 1.
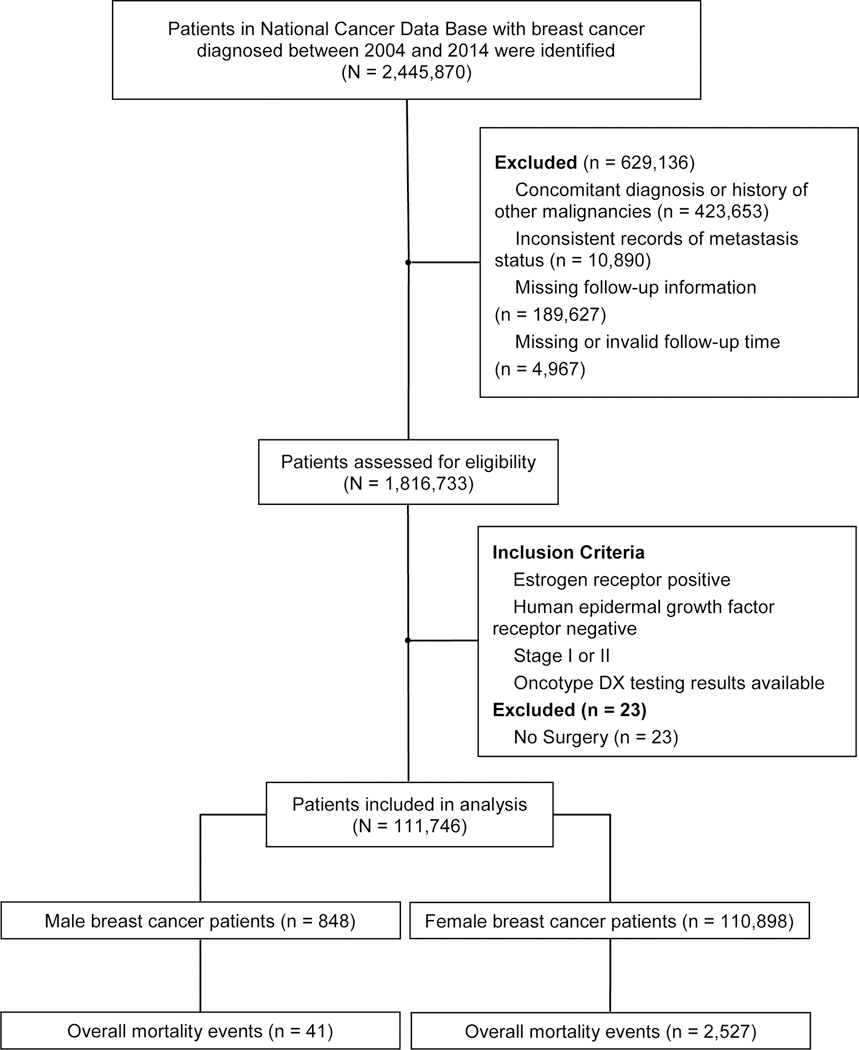
Study Flowchart
Data on demographic characteristics, including age at diagnosis, race, year of diagnosis, urban/rural residence, estimated annual household income and educational attainment at the zip code level, insurance, treating facility, region and distance to care were gathered from the NCDB. Available clinical characteristics included tumor size, nodal status, progesterone receptor (PR) status, histology type, Nottingham combined histologic grade (grade), lymphovascular invasion (LVI) and Charlson/Deyo score. Data on receipt of treatment (yes/no only) were obtained from the NCDB, including chemotherapy, radiotherapy and endocrine therapy. Information on breast surgery type was also collected.
Statistical analysis
The primary outcome was overall survival (OS), defined as months from cancer diagnosis to death of any cause or to last contact. Patients lost to follow-up were censored at last contact. Demographic, clinical and treatment characteristics of male and female patients were compared using Chi-squared tests for categorical variables and Student’s t-tests for continuous variables. Descriptive analyses were also carried out among patients who were eligible for Oncotype DX test to compare patients with RS tests and those without RS tests. Five-year OS across RS groups, defined by traditional and TAILORx cutoffs in men and women, were estimated and compared using the Kaplan-Meier method and log-rank test.
The age-adjusted RS-mortality association was evaluated using restricted cubic spline function (11) by treating RS as a continuous variable, with 3 knots (model automatically generated) placed. Patients were also stratified into respective low-, intermediate-, and high-risk groups based on traditional cutoffs (≤17, 18–30, and ≥31)(1) and TAILORx cutoffs (≤10, 11–25, and ≥26) (12). Cox proportional hazards models were used to estimate hazard ratios (HR) and 95% confidence intervals (CI) for the association of RS groups with overall mortality in male and female patients separately. The HRs and 95% CIs were derived with 1) adjustment for age alone, 2) additional adjustment for demographic characteristics, clinical characteristics and treatments, except chemotherapy, and 3) further adjustment for chemotherapy. Fully-adjusted associations between chemotherapy utilization and overall mortality were further evaluated among patients with intermediate-risk defined by traditional or TAILORx cutoffs. Similar analyses were not performed for high-risk patients because of the small sample size and high chemotherapy rate in male breast cancer patients. Given that the TAILORx Trial showed a significant interaction between chemotherapy treatment and age (≤50 years vs. >50 years) (5), the abovementioned Cox regression analyses were also conducted with stratification by age in women. Due to the small number of male patients aged ≤50, age-specific analyses were only conducted in male patients with age >50. Tests for interactions between RS groups and sex were conducted using maximum likelihood tests comparing fully-adjusted models with and without the interaction terms.
Sensitivity analyses were conducted after excluding patients with lymph node metastasis based on post-operative evaluation, or those who did not receive endocrine therapy (n=25,755). Ten female patients who died within 90 days after surgery were also excluded in the sensitivity analysis in order to rule out the potential influence of treatment-related deaths. All statistical tests were based on 2-sided probability, with the significance level set at P<0.05, and performed using R 3.5.1 (R Foundation, Vienna, Austria).
Results
A total 848 male and 110,898 female patients were included in the final analysis of this study, accounting for 24.9% (n=3,400) and 30.5% (n=363,958) of all male and female patients, respectively, who were eligible for Oncotype DX test (i.e., ER+, HER2-, and stage I or II invasive breast cancer). In comparison to male patients who were eligible for but did not take Oncotype DX test, male patients who took the test were younger (61.9 ± 10.4 vs. 64.9 ± 12.3; P<0.001), and tended to have smaller tumor size (19.7 ± 9.5 mm vs. 21.2 ± 17.0 mm; P=0.02), lower proportion of lymph node metastasis (19.0% vs. 36.2%; P<0.001), lower grade (grade I: 20.5% vs. 21.8%; P=0.02), and lower proportion of LVI (18.2% vs. 22.7%; P<0.001). However, after excluding patients who had lymph node metastasis and who did not receive endocrine therapy, patients with and without RS test only showed a significant difference in tumor grade (grade I: 23.2% vs. 26.0%, for patients with and without RS test, respectively; P=0.03; Supplementary Table S1, online only).
Overall, among patients who had RS results, the average RS in men was comparable to that in women (16.6 ± 12.0 vs. 17.2 ± 10.1, respectively; P=0.15), and so was the proportion of patients with RS <26 (82.6% vs. 85.5%, respectively). However, the respective proportion of patients with RS ≤10 and RS ≥31 was higher in men than women (RS ≤10: 34.7% vs. 23.4%; RS ≥31: 10.8% vs. 7.9%; P<0.001 for both; Table 1). Chemotherapy utilization increased with higher RS in both men and women; among patients with RS ≥26, 70.9% of men and 74.8% of women received chemotherapy (Table 2).
Table 1.
Characteristics of breast cancer patients with Oncotype DX Recurrence Score testing
| Characteristics | Male (N = 848, %) | Female (N = 110,898, %) | P |
|---|---|---|---|
| Age (years, Mean ± SD [range]) | 61.9 ± 10.4 [26–88] | 58.3 ± 10.5 [18–90] | <0.001 |
| Recurrence Score (Mean ± SD [range]) | 16.6 ± 12.0 [0–100] | 17.2 ± 10.1 [0–100] | 0.15 |
| Recurrence Score | <0.001 | ||
| 0–10 | 34.7 | 23.4 | |
| 11–17 | 23.8 | 36.1 | |
| 18–25 | 24.1 | 26.0 | |
| 26–30 | 6.6 | 6.6 | |
| 31–100 | 10.8 | 7.9 | |
| Follow-up time (months, Median) | 39.5 | 40.1 | 0.06 |
| Deaths | 41 | 2,527 | |
| Race | 0.01 | ||
| White | 86.4 | 87.0 | |
| Black | 10.0 | 7.6 | |
| Other | 2.7 | 4.4 | |
| Unknown | 0.8 | 0.9 | |
| Year of Diagnosis | 0.25 | ||
| 2010 | 12.3 | 13.8 | |
| 2011 | 20.3 | 17.8 | |
| 2012 | 20.5 | 20.1 | |
| 2013 | 23.3 | 23.0 | |
| 2014 | 23.6 | 25.3 | |
| Nottingham Combined Histological Grade | <0.001 | ||
| I | 20.5 | 30.0 | |
| II | 52.4 | 50.6 | |
| III | 21.0 | 14.1 | |
| Unknown | 6.0 | 5.3 | |
| Histology Type | <0.001 | ||
| Ductal | 83.0 | 73.9 | |
| Lobular | 3.4 | 11.7 | |
| Other | 13.6 | 14.4 | |
| Positive Progesterone Receptor | 92.7 | 90.9 | 0.29 |
| Positive Lymph Vascular Invasion | 18.2 | 13.2 | <0.001 |
| Tumor Size (mm, Mean ± SD) * | 19.7 ± 9.5 | 17.3 ± 12.3 | <0.001 |
| Lymph Node Metastasis | 19.0 | 16.9 | 0.12 |
| Comorbidity | 19.9 | 14.5 | <0.001 |
| Mastectomy | 74.4 | 32.8 | <0.001 |
| Chemotherapy | 22.6 | 23.4 | 0.49 |
| Endocrine Therapy | 86.0 | 93.0 | <0.001 |
| Radiation Therapy | 32.1 | 67.9 | <0.001 |
Exact tumor size was not available for 5 male patients and 590 female patients.
Table 2.
HRs (95% CI) for total mortality associated with the Recurrence Score categories
| Deaths/Patients | CT (%) | ET (%) | Male Patients | Deaths/Patients | CT (%) | ET (%) | Female Patients | |
|---|---|---|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | Hazard Ratio (95% CI) | |||||||
| Continuous Scale | ||||||||
| Age-adjusted | 41/848 | 22.6 | 86.0 | 1.02 (1.01 to 1.04) | 2,527/110,898 | 23.4 | 93.0 | 1.03 (1.03 to 1.03) |
| Adjusted 1 | 41/848 | 22.6 | 86.0 | 1.02 (0.99 to 1.05) | 2,527/110,898 | 23.4 | 93.0 | 1.02 (1.02 to 1.02) |
| Fully-Adjusted 2 | 41/848 | 22.6 | 86.0 | 1.02 (0.99 to 1.05) | 2,527/110,898 | 23.4 | 93.0 | 1.02 (1.02 to 1.03) |
| Traditional Cutoffs * | ||||||||
| Age-adjusted | ||||||||
| Low risk | 14/496 | 6.2 | 88.5 | reference | 1,158/65,935 | 6.7 | 93.5 | reference |
| Intermediate risk | 19/260 | 34.2 | 82.3 | 2.75 (1.38 to 5.49) | 869/36,174 | 39.3 | 93.4 | 1.32 (1.21 to 1.44) |
| High risk | 8/92 | 78.3 | 82.6 | 3.06 (1.28 to 7.32) | 500/8,789 | 83.0 | 88.2 | 3.07 (2.76 to 3.41) |
| Adjusted 1 | ||||||||
| Low risk | 14/496 | 6.2 | 88.5 | reference | 1,158/65,935 | 6.7 | 93.5 | reference |
| Intermediate risk | 19/260 | 34.1 | 82.3 | 1.82 (0.83 to 4.00) | 869/36,174 | 39.3 | 93.4 | 1.27 (1.16 to 1.39) |
| High risk | 8/92 | 78.3 | 82.6 | 1.35 (0.45 to 4.06) | 500/8,789 | 83.0 | 88.2 | 2.23 (1.96 to 2.54) |
| Fully-Adjusted 2 | ||||||||
| Low risk | 14/496 | 6.2 | 88.5 | reference | 1,158/65,935 | 6.7 | 93.5 | reference |
| Intermediate risk | 19/260 | 34.1 | 82.3 | 1.69 (0.74 to 3.86) | 869/36,174 | 54.3 | 94.6 | 1.31 (1.20 to 1.44) |
| High risk | 8/92 | 78.3 | 82.6 | 1.15 (0.34 to 3.91) | 500/8,789 | 85.1 | 91.2 | 2.46 (2.13 to 2.84) |
| TAILORx Cutoffs # | ||||||||
| Age-adjusted | ||||||||
| Low risk | 4/294 | 6.8 | 88.1 | reference | 489/25,929 | 4.4 | 92.9 | reference |
| Intermediate risk | 23/406 | 16.5 | 86.0 | 4.60 (1.59 to 13.32) | 1,289/68,882 | 18.5 | 93.7 | 1.05 (0.94 to 1.16) |
| High risk | 14/148 | 70.9 | 81.8 | 7.15 (2.35 to 21.72) | 749/16,087 | 74.8 | 90.0 | 2.44 (2.18 to 2.74) |
| Adjusted 1 | ||||||||
| Low risk | 4/294 | 6.8 | 88.1 | reference | 489/25,929 | 4.4 | 92.9 | reference |
| Intermediate risk | 23/406 | 16.5 | 86.0 | 5.37 (1.79 to 16.11) | 1,289/68,882 | 18.5 | 93.7 | 1.06 (0.96 to 1.18) |
| High risk | 14/148 | 70.9 | 81.8 | 4.28 (1.22 to 14.97) | 749/16,087 | 74.8 | 90.0 | 1.92 (1.68 to 2.18) |
| Fully-Adjusted 2 | ||||||||
| Low risk | 4/294 | 6.8 | 88.1 | reference | 489/25,929 | 4.4 | 92.9 | reference |
| Intermediate risk | 23/406 | 16.5 | 86.0 | 5.33 (1.77 to 16.08) | 1,289/68,882 | 18.5 | 93.7 | 1.07 (0.97 to 1.19) |
| High risk | 14/148 | 70.9 | 81.8 | 3.56 (0.93 to 13.58) | 749/16,087 | 74.8 | 90.0 | 2.05 (1.78 to 2.37) |
Abbreviations: CT: chemotherapy, ET: endocrine therapy.
Traditional Cutoffs: low risk: Recurrence Score (RS) ≤17; intermediate risk: RS 18 to 30; high risk: RS ≥31. Based on the fully adjusted model, P value for interaction between RS and sex was 0.10.
TAILORx Cutoffs: low risk: Recurrence Score (RS) ≤10; intermediate risk: RS 11 to 25; high risk: RS ≥ 26. Based on the fully adjusted model, P value for interaction between RS and sex was 0.008.
Adjusted for: age (continuous), race, grade, histology type, Progesterone Receptor status, tumor size, lymph nodal status, lymphovascular invasion, comorbidity, surgery, endocrine therapy, radiation therapy, education, income, insurance, year of diagnosis (strata).
Additionally adjusted for chemotherapy.
Estimates of 5-year OS differed significantly across RS groups in both men and women (Figure 2). When evaluated using TAILORx cutoffs, the 5-year OS was 97.2% (95% CI: 90.3–99.2%), 91.0% (95% CI: 86.1–94.3%) and 83.2% (95% CI: 70.5–90.7%) for men with RS 0–10, RS 11–25 and RS 26–100, respectively (P=0.003). In women, patients with RS 0–10 and RS 11–25 had similar 5-year OS of 96.6% (95% CI: 96.2–96.9%) and 97.0% (95% CI: 96.8–97.2%), respectively; both were higher than that of the RS 26–100 group (92.9%, 95% CI: 92.3–93.5%; P<0.001). When estimated using traditional RS cutoffs, 5-year OS was 95.7%, 87.5% and 82.3% for men with RS 0–17, RS 18–30 and RS 31–100, respectively (P=0.02). Respective corresponding rates in women were 97.1%, 96.1% and 91.5% (P<0.001).
Figure 2. Five-year Overall Survival by Oncotype DX Recurrence Score (RS) for Male and Female Breast Cancer Patients.
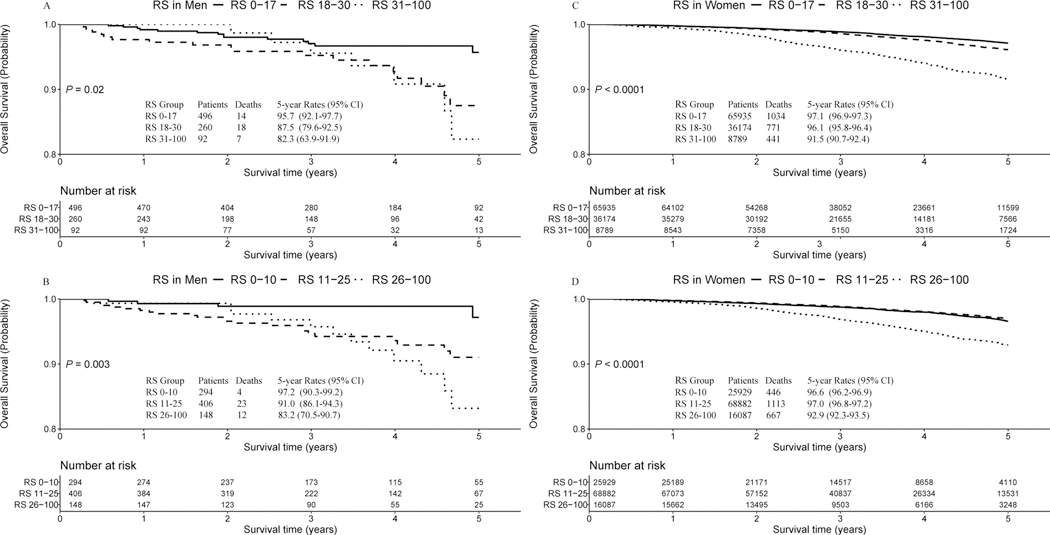
(A) 5-year survival curve for male patients according to traditional RS cutoff (i.e., 0–17,18–30, and 31–100); (B) 5-year survival curve for male patients according to TAILORx RS cutoff (i.e., 0–10,11–25, and 26–100); (C) 5-year survival curve for female patients according to traditional RS cutoff (i.e., 0–17,18–30, and 31–100); (D) 5-year survival curve for female patients according to TAILORx RS cutoff (i.e., 0–10,11–25, and 26–100).
RS was associated with increased mortality risk in male patients until RS >21 (fully-adjusted HR=1.12, 95%CI: 1.02 to 1.24 per unit RS increment), after which the risk plateaued. In female patients, however, mortality risk began to increase only with a RS >23 (fully-adjusted HR=1.02, 95%CI: 1.01 to 1.02 per unit RS increment). Test for non-linearity was significant in both groups (Figure 3).
Figure 3. Association Pattern Between Total Mortality Curve and Oncotype DX Recurrence Score (RS) in Male and Female Breast Cancer Patients.
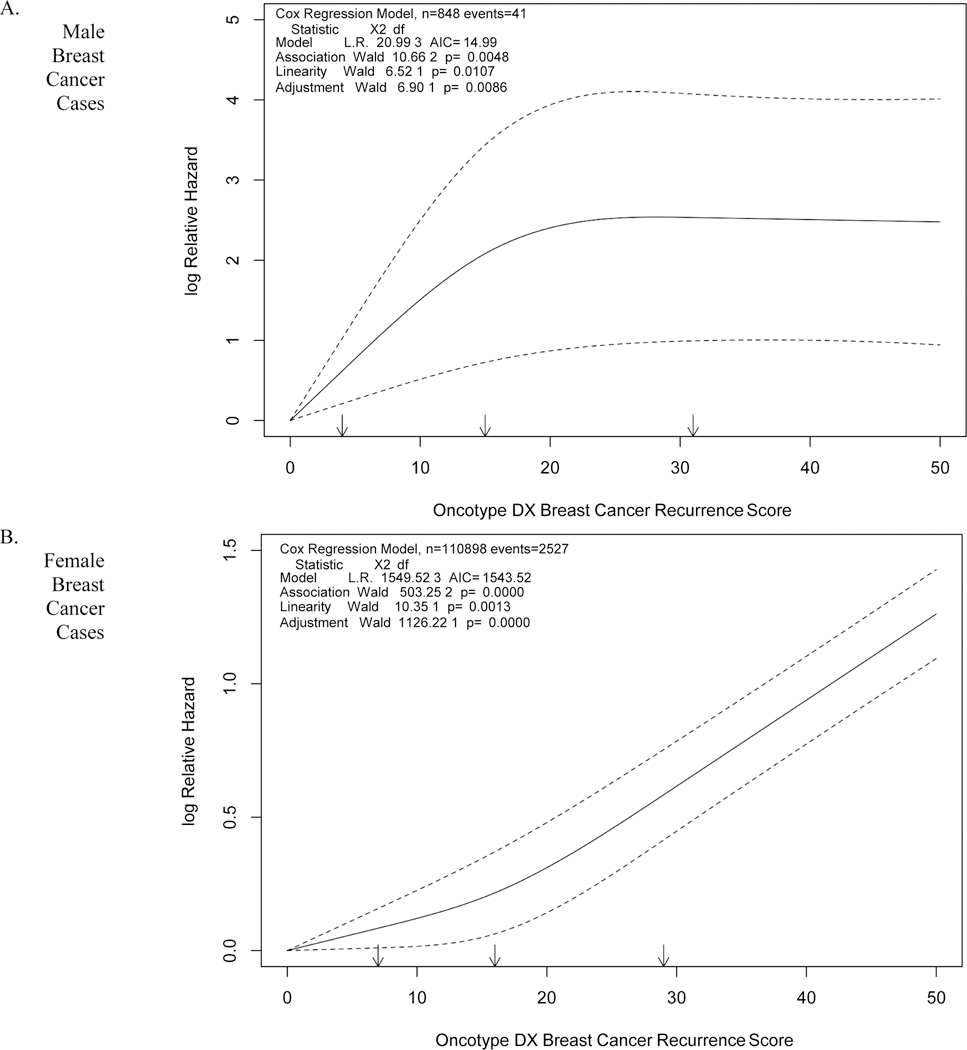
Association pattern for male breast cancer patients. (B) Association pattern for female breast cancer patients. Results were generated from restricted cubic spline regression with adjustment for age and RS as a continuous variable.
Traditional cutoffs for RS were not significantly associated with mortality in male patients (Table 2). Based on TAILORx cutoffs, after adjustment for demographic factors, clinical characteristics and treatments, except chemotherapy, male patients with RS 11–25 (HR=5.37, 95%CI: 1.79 to 16.11) or ≥26 (HR=4.28, 95%CI: 1.22 to 14.97) had a higher mortality risk compared to those with RS ≤10. Additional adjustment for chemotherapy resulted in little attenuation of HR for the intermediate-risk group (HR=5.33, 95%CI: 1.77 to 16.08), but some attenuations for the high-risk group (HR=3.56, 95%CI: 0.93 to 13.58). In comparison, female patients in the high-risk group had a 2.0-fold (fully-adjusted HR=2.05, 95%CI: 1.78 to 2.37 for TAILORx cutoffs) to 2.5-fold (fully-adjusted HR=2.46, 95%CI: 2.13 to 2.84 for traditional cutoffs) elevated risk of mortality compared with their low-risk counterparts. Women with RS 11–25 did not have higher mortality risk compared to those with RS ≤10 (fully-adjusted HR=1.06, 95%CI: 0.96 to 1.18; Table 2). Significant interactions between sex and RS group were observed for TAILORx cutoffs (P for interaction = 0.008) but not for traditional cutoffs (P for interaction = 0.10). These associations were observed in male patients age >50 years and in female patients irrespective of age ≤50 or >50 years (Supplementary Table S2, Supplementary Table S3; online only). Analyses restricted to female patients who did not receive chemotherapy showed that, in comparison to RS ≤10, RS ≥26 was associated with an increased mortality (HR=2.00, 95%CI: 1.69 to 2.37), but RS 11–25 was not significantly associated with mortality (HR=1.08, 95%CI: 0.97 to 1.21). Similar analyses could not be conducted in men due to the small sample size.
Additional chemotherapy was associated with lower risk of mortality among women with RS 18–30 (HR=0.83, 95%CI: 0.71 to 0.97), and non-significant reduction in mortality among women with RS 11–25 (HR=0.89, 95%CI: 0.76 to 1.05; Table 3). When stratified by age, the lower mortality risk associated with chemotherapy was only observed among older women with RS 18–30 (HR=0.82, 95%CI: 0.69 to 0.97), but not among those aged ≤50 with RS 18–30 (HR=0.96, 95%CI: 0.64 to 1.44), or among those with RS 11–25 regardless of age (i.e., HR=0.97, 95%CI: 0.65 to 1.44 for women aged ≤50; HR=0.87, 95%CI: 0.73 to 1.04 for women aged >50; Supplementary Table S4, online only). No significant association between chemotherapy and mortality was observed among male patients with intermediate-risk; i.e., RS 18–30 (traditional cutoffs: HR=1.37, 95%CI: 0.32 to 5.82) or RS 11–25 (TAILORx cutoffs: HR=3.50, 95%CI: 0.98 to 12.53), although these analyses were based on a much smaller sample size (Table 3). Similar analyses by age at diagnosis could not be done in male cases due to a small sample size.
Table 3.
HRs (95% CI) for total mortality associated with chemotherapy status among intermediate-risk patients*
| Deaths/Patients | ET (%) | Male Patients | Deaths/Patients | ET (%) | Female Patients | |
|---|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | Hazard Ratio (95% CI) | |||||
| All patients | ||||||
| RS 18–30 | ||||||
| No Chemotherapy | 11/164 | 85.4 | reference | 575/21,460 | 93.1 | reference |
| Chemotherapy | 8/89 | 80.1 | 1.37 (0.32 to 5.82) | 282/14,217 | 94.3 | 0.83 (0.71 to 0.97) |
| RS 11–25 | ||||||
| No Chemotherapy | 17/329 | 88.4 | reference | 1075/54,902 | 93.9 | reference |
| Chemotherapy | 6/67 | 79.1 | 3.50 (0.98 to 12.53) | 194/12,750 | 94.5 | 0.89 (0.76 to 1.05) |
| Patients with Negative Lymph Node and Receipt of Endocrine Therapy | ||||||
| RS 18–30 | ||||||
| No Chemotherapy | 8/126 | 100.0 | reference | 385/17,475 | 100.0 | reference |
| Chemotherapy | 4/54 | 100.0 | 1.15 (0.02 to 8.72) | 155/10,307 | 100.0 | 0.80 (0.66 to 0.98) |
| RS 11–25 | ||||||
| No Chemotherapy | 12/252 | 100.0 | reference | 733/44,243 | 100.0 | reference |
| Chemotherapy | 3/39 | 100.0 | 4.89 (0.46 to 52.34) | 98/8,141 | 100.0 | 0.87 (0.70 to 1.09) |
Abbreviations: ET: endocrine therapy; RS: Oncotype DX Breast Recurrence Score.
Patients with unknown chemotherapy status were excluded from this analysis.
Four female patients with RS 18–30 and 8 female patients with RS 11–25 who died within 90 days after surgery were excluded from this analysis. No male patients died within 90 days after surgery.
Adjusted for: age (continuous), race, grade, histology type, Progesterone Receptor status, tumor size, lymphovascular invasion, comorbidity, surgery, radiation therapy, education, income, insurance, year of diagnosis (strata). Lymph nodal status and endocrine therapy status were also included for adjustment when analysis was conducted within all populations.
Sensitivity analyses excluding patients with lymph node metastasis, or those who did not receive endocrine therapy, showed overall similar patterns (Table 3; Supplementary Table S5, online only).
Discussion
In this large-scale registry-based study, we found that distribution and association patterns of RS with mortality in male breast cancer patients were different from those in their female counterparts. RS was prognostic for mortality among male patients, but with a lower threshold than that for female patients. Little benefit from chemotherapy was observed for those with intermediate-risk male patients, defined either by TAILORx or traditional cutoffs, although this group, overall, was at high mortality risk.
The RS algorithm was developed based on multigene profiles from female breast cancer patients to quantify the risk of distant recurrence (1). Despite the overall similar averaged RS between men and women, we observed higher proportions of both high and low RS in male breast cancer patients than their female counterparts. This is similar to previous reports based on data from the SEER Program, as well as those from a single institution (10,13,14). The observed differences in RS distribution between men and women suggest that male breast cancer may have distinct biology and different prognostic factors compared to female patients. Studies have suggested that pathogenic mutations and epigenetic alterations involved in male breast carcinogenesis do not exactly overlap with those of women (15). For example, BRCA2 and CHEK2 were more frequent in male compared to female cases (16). A study by Massarweh et al. revealed that, among breast cancer patients with RS testing, men in comparison to women had higher mean expression levels for ER related genes, as well as proliferation and invasion related genes (10). Future comparative studies on sex-specific pathogenic alterations in breast cancer may provide more insight on underlying mechanisms.
In female breast cancer, prognostic values of RS on cancer outcome, as well as predictive values of chemotherapy benefit, have been well validated in both clinical trials and routine practice settings (3–5,17), and RS has been recommended for clinical utility (18). Our findings on the prognostic and predictive values of RS on female breast cancer patients are consistent with previous reports (4,17–19). We found that female patients with RS 11–25 had only a modest increased mortality compared to those with RS ≤10. We also found no overall mortality benefit of chemotherapy for women with RS 11–25, irrespective of age (i.e., ≤50 or >50), which is generally in line with results from TAILORx Trials (5,20). These findings support the 2018 National Comprehensive Cancer Network guidelines to increase the risk cutoff to 26 for female breast cancer patients (21), as well as the updated clinical practice guidelines by the American Society of Clinical Oncology (6). We carried out additional analyses for women aged ≤50 with RS 16–25, for whom a chemotherapy benefit on distant recurrence free survival was recently reported in the TAILORx Trial (20). We found a borderline significant overall mortality benefit for this group of patients (HR=0.84, 95%CI: 0.70 to 1.00; not reported in the tables). These results support the validity of our findings.
To the best of our knowledge, the prognostic and predictive values of RS in male breast cancer patients have not been well evaluated. In our study, we found significantly different 5-year OS in men across RS groups, either defined by traditional or TAILORx cutoffs, especially when evaluated using the TAILORx cutoffs. This is consistent with the study of Massarweh et al., which used data from the SEER Program and estimated OS and breast cancer specific survival (BCSS) for 322 male breast cancer patients, according to traditional RS cutoffs (10). They also observed significantly different 5-year OS and BCSS estimates across RS groups in the entire study male population, though the differences did not remain significant in 276 male patients without node metastasis (P=0.22 for OS, and P=0.08 for BCSS, respectively). In our study, after adjustment for demographic, clinical and treatment factors, we found that a much lower RS cutoff for risk classification is needed for male compared to female breast cancer patients. TAILORx cutoffs, but not traditional cutoffs, were associated with significantly increased mortality among male breast cancer patients. Interestingly, the association for the high-risk group was only modestly attenuated after additional adjustment for chemotherapy, and chemotherapy was not significantly associated with mortality among male patients with RS 11–25 or those with RS 18–30. This may suggest that RS may only be associated with total mortality but not robustly predict the benefit of adjuvant chemotherapy for male breast cancer patients. However, the sample size for the analysis related to chemotherapy is small. In addition, our study was not equipped to investigate the predictive value of Oncotype DX due to the lack of detailed treatment information and compliance data in the NCDB. It is noteworthy that treatment for male breast cancer, including those based on the RS categorization, is primarily based on the knowledge gained from clinical trials conducted in female patients (8). In addition, previous studies have shown that compliance to treatments was poorer in men than women (22,23). Furthermore, there may be biological differences between male and female breast cancer (9). Thus, studies directly evaluating whether RS is predictive to treatment in male breast cancer patients are warranted.
The strengths of our study include the relatively large sample size and generalizability. Our study included 848 male patients with both RS results and mortality data, which is larger than the previous SEER based study, which included only 322 male patients with survival data (10). Compared to the SEER Program, which covers 28% of the U.S. population (24), the NCDB captures approximately 70% of newly diagnosed cancer cases across the U.S., further enhancing the generalizability of our study. In our analysis, we also accounted for a wide range of clinical covariates, including information on endocrine therapy, which was the backbone of systemic treatment for ER+ breast cancer patients, but which was not covered in the previous SEER-data derived study. However, our study has limited statistical power for subgroup analyses, including age and chemotherapy specific analyses, and these findings should be interpreted with caution. We included all patients with RS results in our study, some of whom may not be qualified for receiving Oncotype DX test, according to the current guideline. We conducted additional analysis restricting our analysis to populations strictly following the inclusion criteria of the TAILORx Trial (i.e., ER+, HER2-, node-negative, tumor size 1.1–5.0 cm, and aged 18–75 years) (5). We found that 70.9% of those female patients had low clinical risk (CR, defined by tumor size and grade), and 29.1% had high CR (data was not shown in tables), in exact agreement with proportions reported in the TAILORx Trial (5). The RS-mortality association remained little changed among these patients. Furthermore, our findings were not materially changed in sensitivity analysis when patients who had lymph node metastasis or did not receive endocrine therapy were excluded. In addition, patients with RS results had generally comparable biologic characteristics to those who were eligible for but did not take Oncotype DX test. All these indicate that bias related to patient selection is not a major concern for our study. A major limitation for our study is that information on recurrence and causes of death was not recorded in the NCDB, and thus, BCSS could not be evaluated. Lack of information on genetic tests (e.g., BRCA mutation) is also a limitation. Finally, the follow-up time was relatively short, and subsequent analyses with long-term follow-up is warranted.
In conclusion, among routine oncology care populations with early-stage breast cancer, RS is prognostic for total morality in both male and female patients, but with distinct association patterns. Mortality increased in much lower ranges of RS for male than female breast cancer patients. Studies are needed to develop RS categorization specifically for male breast cancer patients.
Supplementary Material
Translational Relevance.
Oncotype DX Breast Recurrence Score (RS) has been well validated and recommended to be used to select female ER-positive, HER2-negative early stage breast cancer patients with a high recurrence risk for chemotherapy. Our study showed that, in routine oncology practice setting, RS predicts total mortality in both male and female breast cancer patients but following distinct patterns. This finding highlights the need to develop RS categorization specifically for male breast cancer patients. Studies on sex-specific pathogenic alterations in breast cancer are needed to clarify the underlying mechanisms.
Acknowledgement
All information was derived from the American College of Surgeons’ National Cancer Database, the American College of Surgeons and the Commission on Cancer are not responsible for conclusions drawn from the data. We would like to thank Dr. Mary Shannon Byers, PhD, MS, for her assistance in editing this manuscript. S. Reid is a fellow of the Vanderbilt Training of the Molecular and Genetic Epidemiology of Cancer (T32 CA160056). F. Wang is supported by the program of China Scholarship Council (201806225032).
Footnotes
Disclaimer: The authors declare no potential conflicts of interest.
Reference
- 1.Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351(27):2817–2826. [DOI] [PubMed] [Google Scholar]
- 2.Sparano JA, Paik S. Development of the 21-gene assay and its application in clinical practice and clinical trials. J Clin Oncol. 2008;26(5):721–728. [DOI] [PubMed] [Google Scholar]
- 3.Mamounas EP, Tang G, Fisher B, et al. Association between the 21-gene recurrence score assay and risk of locoregional recurrence in node-negative, estrogen receptor-positive breast cancer: results from NSABP B-14 and NSABP B-20. J Clin Oncol. 2010;28(10):1677–1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paik S, Tang G, Shak S, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24(23):3726–3734. [DOI] [PubMed] [Google Scholar]
- 5.Sparano JA, Gray RJ, Makower DF, et al. Adjuvant Chemotherapy Guided by a 21-Gene Expression Assay in Breast Cancer. N Engl J Med. 2018;379(2):111–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andre F, Ismaila N, Henry NL, et al. Use of Biomarkers to Guide Decisions on Adjuvant Systemic Therapy for Women With Early-Stage Invasive Breast Cancer: ASCO Clinical Practice Guideline Update—Integration of Results From TAILORx. J Clin Oncol. 2019;37(22):1956–1964. [DOI] [PubMed] [Google Scholar]
- 7.Miao H, Verkooijen HM, Chia K-S, et al. Incidence and outcome of male breast cancer: an international population-based study. J Clin Oncol. 2011;29(33):4381–4386. [DOI] [PubMed] [Google Scholar]
- 8.Giordano SH. Breast Cancer in Men. N Engl J Med. 2018;378(24):2311–2320. [DOI] [PubMed] [Google Scholar]
- 9.Fentiman IS. Male breast cancer is not congruent with the female disease. Crit Rev Oncol Hematol. 2016;101:119–124. [DOI] [PubMed] [Google Scholar]
- 10.Massarweh SA, Sledge GW, Miller DP, McCullough D, Petkov VI, Shak S. Molecular Characterization and Mortality From Breast Cancer in Men. J Clin Oncol. 2018;36(14):1396–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harrell F Jr. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. New York City: Springer-Verlag; 2001. [Google Scholar]
- 12.Sparano JA, Gray RJ, Makower DF, et al. Prospective Validation of a 21-Gene Expression Assay in Breast Cancer. N Engl J Med. 2015;373(21):2005–2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Altman AM, Kizy S, Yuan J, et al. Distribution of 21-Gene Recurrence Scores in Male Breast Cancer in the United States. Ann Surg Oncol. 2018;25(8):2296–2302. [DOI] [PubMed] [Google Scholar]
- 14.Turashvili G, Gonzalez-Loperena M, Brogi E, et al. The 21-Gene Recurrence Score in Male Breast Cancer. Ann Surg Oncol. 2018;25(6):1530–1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rizzolo P, Silvestri V, Tommasi S, et al. Male breast cancer: genetics, epigenetics, and ethical aspects. Ann Oncol. 2013;24 Suppl 8:viii75-viii82. doi: 10.1093/annonc/mdt316 [DOI] [PubMed] [Google Scholar]
- 16.Pritzlaff M, Summerour P, McFarland R, et al. Male breast cancer in a multi-gene panel testing cohort: insights and unexpected results. Breast Cancer Res Treat. 2017;161(3):575–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dowsett M, Cuzick J, Wale C, et al. Prediction of risk of distant recurrence using the 21-gene recurrence score in node-negative and node-positive postmenopausal patients with breast cancer treated with anastrozole or tamoxifen: a TransATAC study. J Clin Oncol. 2010;28(11):1829–1834. [DOI] [PubMed] [Google Scholar]
- 18.Harris LN, Ismaila N, McShane LM, et al. Use of Biomarkers to Guide Decisions on Adjuvant Systemic Therapy for Women With Early-Stage Invasive Breast Cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2016;34(10):1134–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ibraheem AF, Press DJ, Olopade OI, Huo D. Community clinical practice patterns and mortality in patients with intermediate oncotype DX recurrence scores: Who benefits from chemotherapy? Cancer. 2019;125(2):213–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sparano JA, Gray RJ, Ravdin PM, et al. Clinical and Genomic Risk to Guide the Use of Adjuvant Therapy for Breast Cancer. N Engl J Med. 2019;380(25):2395–2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Comprehensive Cancer Network. Breast Cancer (Version 4.2019). https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Published 2019. Accessed March 12, 2019.
- 22.Kiluk JV, Lee MC, Park CK, et al. Male breast cancer: management and follow-up recommendations. Breast J. 2011;17(5):503–509. [DOI] [PubMed] [Google Scholar]
- 23.Venigalla S, Carmona R, Guttmann DM, et al. Use and Effectiveness of Adjuvant Endocrine Therapy for Hormone Receptor–Positive Breast Cancer in Men. JAMA Oncol. 2018;4(10):e181114-e181114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


