Abstract
The neodymium:aluminum garnet laser has emerged as a generally well-tolerated tool for hair removal; however, some patients develop a folliculitis after treatment, which can limit utility. To our knowledge, the literature is currently lacking an adequate description of the etiology of laser-induced folliculitis or strategies to prevent and manage it. We present the case of a 33-year-old Caucasian male patient who developed a robust laser-induced folliculitis. We discuss management strategies and the possible mechanism of onset, as well as hypothesize that the mechanism driving laser-induced folliculitis is similar to that seen with pseudofolliculitis barbae, as the nidus for the inflammatory response appeared to be the hairs undergoing extrusion through the skin. While laser-induced folliculitis is a self-limited complication, it might discourage patients from seeking laser hair removal. In patients known to develop this adverse effect or those with hair features potentially more prone to developing folliculitis (i.e. curly, coarse hair or pili multigemini), it might be reasonable to treat with prophylactic doxycycline and topical steroids along with gentle washing techniques to assist in depilation. As demonstrated in our case, this might help to decrease the severity and duration of laser-induced folliculitis.
Keywords: Pseudofolliculitis barbae, folliculitis, laser-induced folliculitis, hair removal, laser, Nd:YAG, folliculitis treatment, folliculitis management, laser-induced pseudofolliculitis barbae
Laser therapy has evolved as an effective procedure for numerous cosmetic and medical applications. The neodymium:aluminum garnet (Nd:YAG) laser has become a practical method for hair removal, especially in patients with darker skin types.1–3 Nd:YAG laser therapy has been reported as well tolerated without serious sequelae; however, several studies have confirmed the development of posttreatment folliculitis to be a possible side effect, which can affect patient satisfaction.1,4 While most cases of folliculitis are mild and self-limited, it is an inconvenient adverse reaction and might discourage patients from seeking laser therapy again. To our knowledge, no authors have discussed the etiology of laser-induced folliculitis or strategies to prevent and manage it. Thus, we report a case of robust laser-induced folliculitis along with strategies for management and prevention.
CASE PRESENTATION
A 33-year-old Caucasian male patient with Fitzpatrick Type II skin presented for his first laser hair-removal treatment of the anterior neck due to repetitive irritation associated with shaving. He was noted to have coarse, dark facial hair with numerous pili multigemini hairs (Figure 1). An Nd:YAG laser (Cutera, Brisbane, California) was first used to perform test spots, with optimal settings determined to be 40J/cm2 with a 20-ms pulse duration and a 10-mm spot size. After the first full treatment, an immediate depilatory effect was noted with gentle wiping of a small portion of the hairs. The patient also showed diffuse erythema and mild edema of the treatment area without any burning or blistering, which resolved over 48 hours. During the next 5 to 7 days, he reported developing numerous pruritic erythematous papules and pustules in the treatment area, which slowly resolved over the subsequent 2 to 4 weeks. He noted that most of these lesions were based around a retained hair shaft and spontaneously improved once the associated hair shaft had fallen out or was extracted with tweezers. He had no issues with postinflammatory hyperpigmentation.
FIGURE 1.

Pili multigemini hairs in patient’s beard area
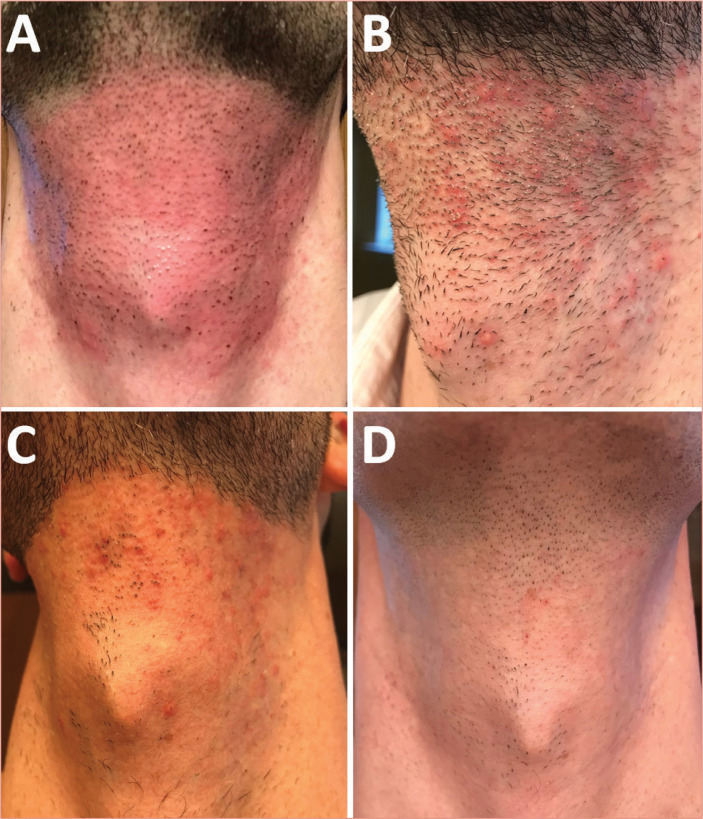
The patient presented six months later for a second treatment after experiencing hair regrowth in the treated area. The same area was treated with the same laser settings as the prior treatment. The patient again experienced diffuse erythema and mild edema of the treatment area immediately after treatment. No burning or blistering was observed (Figure 2A). He was prescribed fluocinonide 0.05% cream to be applied twice daily to the treatment area to help prevent the folliculitis he experienced after the first treatment. However, despite the use of the fluocinonide cream, he reported the appearance of erythematous papules and pustules 6 to 9 days after treatment (Figure 2B). He was prescribed a three-week course of 100mg of doxycycline daily starting 10 days after treatment and was instructed to continue gently washing the affected area and applying the fluocinonide cream. With the use of topical steroids, doxycycline, and gentle washing to assist in the removal of shedding hairs, the erythematous papules and pustules decreased over the course of a week (Figure 2C) and ultimately fully resolved (Figure 2D) as they had done with the initial treatment.
FIGURE 2.
Folliculitis induced by laser hair removal—A) Treatment region immediately after procedure, showing diffuse erythema and mild edema of the treated area; B) Nine days after treatment, development of erythematous papules and pustules; C)15 days after treatment and 5 days after starting doxycycline, decreased number of papules and pustules with marked decrease in hair density in the treatment area; and D) 3 months after treatment, full resolution of folliculitis
The patient returned four months later after experiencing near-complete hair regrowth for a third treatment with the same laser settings as the prior two sessions. He was anxious about developing folliculitis again and was interested in preventative treatment. The day before treatment, he was started on twice-daily fluocinonide cream and 100mg of doxycycline daily, which was continued for two weeks. He still developed erythematous follicular-based papules after 6 to 9 days, but they were significantly smaller, fewer in number, and less pruritic than previously seen. In addition, gentle washing of the treated area with a washcloth resulted in faster hair shedding, which was completed after two weeks. Again, all inflamed lesions resolved spontaneously once the centrally based hair shaft had shed. At subsequent treatments, this treatment strategy was adopted for good control of the folliculitis.
DISCUSSION
Our patient developed robust folliculitis in the treatment area within a week of each Nd:YAG treatment. We hypothesize that the mechanism driving this folliculitis is similar to that of pseudofolliculitis barbae (PFB), which is a chronic disorder that often manifests as inflammatory papulopustules in the beard area.5,6 PFB is caused by a foreign body inflammatory response to curved hair re-entering the skin, often after shaving; it is particularly common in African American men and individuals with curly, coarse hair.5–7 During laser hair removal, the hair follicle is destroyed through the process of photothermolysis, with the residual hair shaft extruded through the skin over time.7,8 The posttreatment folliculitis sometimes observed with this procedure might be the result of a foreign-body inflammatory reaction to the hairs being lost through extrusion, similar to the process observed with PFB. As seen in our patient, once the depilatory effect is complete, the nidus for the foreign body response is gone and the folliculitis resolves.
Laser hair removal has shown promise as a therapy for PFB, acne keloidalis nuchae, hidradenitis suppurativa, and pilonidal disease and is generally well tolerated;6,9–13 however, posttreatment folliculitis has been reported as a side effect.1,4,14 It is currently unclear which patient populations are more likely to develop this laser-induced folliculitis. If the pathophysiology is similar to that of PFB, then African American men or individuals with coarse, dark hair and pili multigemini hairs might have an increased risk of developing folliculitis with laser therapy. Our patient developed a robust folliculitis after laser treatment, likely due to his coarse hair and pili multigemini hairs. In individuals who are known to develop folliculitis after laser hair removal, have numerous pili multigemini hairs, or have a history of irritant folliculitis secondary to shaving, it might be reasonable to pretreat with topical steroids and oral doxycycline. The use of prophylactic fluocinonide cream and doxycycline along with gentle washing significantly reduced the severity and duration of folliculitis in the case presented here. While this reaction might be unavoidable in some individuals, the anti-inflammatory effects of steroids and doxycycline combined with the depilatory effect of gentle washing with a clean cloth will likely improve laser-induced folliculitis. By offering patients who are prone to this side effect a reasonable pretreatment regimen, laser therapy will remain a tolerable and effective treatment option for those seeking cosmetic hair removal and therapy for PFB, hidradenitis suppurativa, and other conditions.11–13,15
REFERENCES
- Bouzari N, Tabatabai H, Firooz A, Dowlati Y. Laser hair removal: comparison of long-pulsed Dd:YAG, long-pulsed alexandrite, and long-pulsed diode lasers [abstract]. J Am Acad Dermatol. 2004;50:P163. doi: 10.1111/j.1524-4725.2004.30163.x. [DOI] [PubMed] [Google Scholar]
- Tanzi EL, Alster TS. Long-pulsed 1064-nm Nd:YAG laser-assisted hair removal in all skin types. Dermatol Surg. 2004;30(1):13–17. doi: 10.1111/j.1524-4725.2004.30007.x. [DOI] [PubMed] [Google Scholar]
- Lanigan SW. Incidence of side effects after laser hair removal. J Am Acad Dermatol. 2003;49(5):882–886. doi: 10.1016/s0190-9622(03)02106-6. [DOI] [PubMed] [Google Scholar]
- Lim SP, Lanigan SW. A review of the adverse effects of laser hair removal. Lasers Med Sci. 2006;21(3):121–125. doi: 10.1007/s10103-006-0377-y. [DOI] [PubMed] [Google Scholar]
- Garcia-Zuazaga J. Pseudofolliculitis barbae: review and update on new treatment modalities. Mil Med. 2003;168(7):561–564. [PubMed] [Google Scholar]
- Alexis A, Heath CR, Halder RM. Folliculitis keloidalis nuchae and pseudofolliculitis barbae: are prevention and effective treatment within reach? Dermatol Clin. 2014;32(2):183–191. doi: 10.1016/j.det.2013.12.001. [DOI] [PubMed] [Google Scholar]
- Gan SD, Graber EM. Laser hair removal: a review. Dermatol Surg. 2013;39(6):823–838. doi: 10.1111/dsu.12116. [DOI] [PubMed] [Google Scholar]
- Ibrahimi OA, Avram MM, Hanke CW et al. Laser hair removal. Dermatol Ther. 2011;24(1):94–107. doi: 10.1111/j.1529-8019.2010.01382.x. [DOI] [PubMed] [Google Scholar]
- Esmat SM, Abdel Hay RM, Abu Zeid OM, Hosni HN. The efficacy of laser-assisted hair removal in the treatment of acne keloidalis nuchae; a pilot study. Eur J Dermatol. 2012;22(5):645–650. doi: 10.1684/ejd.2012.1830. [DOI] [PubMed] [Google Scholar]
- Tawfik A, Osman MA, Rashwan I. A novel treatment of acne keloidalis nuchae by long-pulsed alexandrite laser. Dermatol Surg. 2018;44(3):413–420. doi: 10.1097/DSS.0000000000001336. [DOI] [PubMed] [Google Scholar]
- Smith MK, Nicholson CL, Parks-Miller A, Hamzavi IH. Hidradenitis suppurativa: an update on connecting the tracts. F1000Res. 2017;6:1272. doi: 10.12688/f1000research.11337.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragoni F, Moretti S, Cannarozzo G, Campolmi P. Treatment of recurrent pilonidal cysts with nd-YAG laser: report of our experience. J Dermatolog Treat. 2018;29(1):65–67. doi: 10.1080/09546634.2017.1329513. [DOI] [PubMed] [Google Scholar]
- Nussbaum D, Friedman A. Pseudofolliculitis barbae: a review of current treatment options. J Drugs Dermatol. 2019;18(3):246–250. [PubMed] [Google Scholar]
- Toosi P, Sadighha A, Sharifian A, Razavi GM. A comparison study of the efficacy and side effects of different light sources in hair removal. Lasers Med Sci. 2006;21(1):1–4. doi: 10.1007/s10103-006-0373-2. [DOI] [PubMed] [Google Scholar]
- Koch D, Pratsou P, Szczecinska W et al. The diverse application of laser hair removal therapy: a tertiary laser unit’s experience with less common indications and a literature overview. Lasers Med Sci. 2015;30:453–467. doi: 10.1007/s10103-013-1464-5. [DOI] [PubMed] [Google Scholar]