Abstract
Background:
Submucous fibrosis with a high incidence rate in the Indian subcontinent is a devastating disease affecting the oral cavity and oropharynx.
Aims and Objective:
To evaluate the efficacy of injection placentrex and injection hydrocortisone in oral submucous fibrosis patients in increasing mouth opening, burning sensation, and improve the mucosal lining.
Materials and Methods:
We recruited 60 patients with Stage II and Stage III of the ailment, who were randomly divided into Group A and Group B. They were administered submucosal injections of hydrocortisone and placentrex along with physiotherapy and oral iron, nutrients, and B-carotene supplements over a period of 2 months.
Interpretations and Results:
The pinnacle rate of the incidence was found in the age group of 30 to 40 years among both the genders. Statistically significant difference (P = 0.0001), that is, 5.19 ± 1.33 in Group A and 11.69 ± 1.26 mm in Group B was noted in the mean mouth opening values. Statistically significant difference in burning sensation was noted to be better in Group A than in Group B.
Discussion and Conclusion:
Overall hydrocortisone seems to be a better regimen for improving the mucosal health and increasing the mouth opening as compared to placentrix regimen. Although Placentrex is better than hydrocortisone in reducing burning sensation.
Keywords: Hydrocortisone, oral submucous fibrosis, placentrex
Introduction
The universe of medicinal science is loaded with a plenty of conditions, both physiological and neurotic which show a huge number of indications—which mankind has figured out how to survive while others, he is the pursuing a persevering war against. The oral cavity has been depicted as a mirror that mirrors the strength of the person. One such condition debilitating the Indian subcontinent is oral submucous fibrosis (OSMF).[1] According to Chandramani More and Naman Rao (2019), it is a debilitating, progressive, irreversible collagen metabolic disorder induced by chronic chewing of areca nut and its commercial preparations; affecting the oral mucosa and occasionally the pharynx and esophagus; leading to mucosal stiffness and functional morbidity; and has a potential risk of malignant transformation. This condition was first described as Vedari by Susruta in ancient manuscripts.[2] It is not only prevalent in India subcontinent but also in countries like Kenya, China, United Kingdom, and Saudi Arabia.
The pathogenesis of OSMF is multifactorial. Various factors such as areca nut chewing, excessive ingestion of chilies, hereditary, and immunologic procedures may trigger the inflammatory procedure causing a juxtaepithelial inflammatory response in the oral mucosa. Arecoline, an alkaloid found in betel nuts stimulates fibroblasts to increase the production of collagen. Nutritional deficiencies like iron insufficiency anemia, vitamin B complex deficiency, and malnutrition interfere with the repair if the inflamed oral mucosa leading to insufficient healing and defective scarring.[3,4] Over the years, a lot of literature has been published discussing the various treatment strategies for OSMF.[5,6] First and foremost strategy is discontinuing the habit. The condition is treated according to the various signs and symptoms presented by the patient.
Glucocorticoids have been the drug of choice due to its anti-inflammatory action, inhibits the proliferation of fibroblasts, upregulates collagen synthesis, and down-regulates collagenase production. They are administered topically as 1.5 cc of intralesional injection over the period of 12 weeks.[7,8] Another drug of choice that has been developed over the years is the placental extracts (Placentrax). It is an aqueous extract of human placenta that contains nucleotides, enzymes like alkaline and acid phosphatase, vitamins like Vit E, B1, B2, B4, B6, pantothenic acid, nicotinic acid, P-amino benzoic acid, folic acid,essential and non-essential amino acids, and certain trace elements. Main effects of placental extracts are anti-inflammatory along with significant analgesic action, which increases blood circulation and tissue vascularity, arrest tissue growth stagnation, and lower immune response factor. Placentrex contains Vitamin E, which prevents the formation of toxic substances due to its anti-oxidant property. Vitamin A plays a major role in induction and control of epithelial differentiation. The basal cells are stimulated to produce mucous and inhibit keratinisation. Vitamin A slows, delays, arrests, or even reverses the invasive malignant potential thus along with Vitamin E improves the mucosal color, mouth opening, and reduces fibrous bands. Local injection of placentrex is safe, cheap, and effective in OSMF without any significant side effects and contra indication. It has a long lasting effect so can be administered in early stages of OSMF with significant results.[9,10]
The present study was conducted in the Department of Oral and Maxillofacial Surgery, Vyas Dental College and Hospital with the aim of studying the outcome of injecting placentrex and hydrocortisone. Also, to evaluate the mouth opening after injecting hydrocortisone and placentrex over a period of 2 months.
Materials and Methods
This was a prospective study conducted on patients referred to the Department of Oral and Maxillofacial Surgery, Vyas Dental College and Hospital, Jodhpur. The study was approved by institutional research ethical committee VDCH/2017/J3/OS4. A total of 200 patients diagnosed with OSMF were screened between January 2017 and January 2019 based on our inclusion and exclusion criteria. Diagnosis was based on the clinical signs and symptoms, presence or absence of burning sensation, and maximal interincisal opening. In our study, we graded the clinical signs and symptoms based on the classification system proposed by Kakkar and Puri:[11]
Grade I: Presence of only blanching of oral mucosa without symptoms
Grade II: Presence of blanching and burning sensation, dryness of the mouth, vesicles or ulcers in the mouth
Grade III: Presence of blanching and burning sensation, dryness of the mouth, vesicles or ulcers in the mouth with restriction of mouth opening and palpable bands all over the mouth without tongue involvement
Grade IV: Presence of blanching and burning sensation, dryness of the mouth, vesicles or ulcers in the mouth with restriction of mouth opening and palpable bands all over the mouth with tongue involvement
Grade V: Presence of all features of Grade IV associated with chronic ulcer and histopathologically proven carcinoma.
Presence or absence of burning sensation was assessed based on Katharia S.K. and B.K. Varma's classification:[12]
Grade 0 - No burning sensation
Grade 1 - Mild burning sensation
Grade 2 - Moderate burning sensation
Grade 3 - Severe burning sensation.
Maximal interincisal distance (mouth opening) was based on the following grades:[13]
Grade I: Mouth opening 35 mm or above
Grade II: Mouth opening 25 mm to 35 mm
Grade III: Mouth opening 15 mm to 25 mm
Grade IV: Mouth opening less than 15 mm.
Taking the above criteria into consideration, patients with clinically diagnosed OSMF were included into the study. Also, patients who were ready to quit the habit and were willing to be part of the follow-up protocol were included in the study. Keeping the above criteria in mind, patients in clinical stage of Grade II and Grade III, a score of 1 and above and ones belonging to Group II and III were included in the study. On the other hand, patients who received any form of treatment before this and are not willing to quit their habit were excluded from the study.
Routine blood investigations like complete blood count (CBC), RBS, HIV, and HBSAg were done before the beginning of the treatment. Patients from both the genders and up to the age limit of 60 years were included in the group. All the selected patients were randomly divided into Group A and Group B. In Group A, 30 patients were injected with 2 ml of placentrex in the areas where fibrous bands were present, over the period of 3 months, at the rate of 2 injections per week. Similarly, in Group B, 30 patients were injected with 2 ml of hydrocortisone which were administered at a rate of 2 injections in 1 week over a period of 3 months. As there is a difference in the cost of placental extracts and hydrocortisone and as there is no evidence in available literature regarding superior efficacy of one over the other, the choice of the medication was based on the patient's preference. These were diluted in lignocaine to reduce local irritation and ensure better spread. It was administered submucosally over the involved sites using an insulin syringe and needle to minimize the fibrosis caused due to repeated injection. Patients were asked not to rinse their mouth for at least 1 hour after taking the above 2 types of submucosal injections. All patients were instructed to stop any further tobacco abuse in any form. Patients were prescribed carotene and multivitamins and were instructed to do local massage of the oral cavity by placing the middle 3 fingers in the mouth and the thumb over the cheek, to help break the fibrous bands and improve local vascularity. The patients were followed up at the end of the 8th week and 12th week periodically. The observations were tabulated and the results were analyzed in terms of:
Decrease in burning sensation
Improvement in mouth opening (maximal interincisal mouth opening)
Increase in the terms of mucosal health.
Features like decrease in ulceration and vesiculation and tongue protrusion were also observed and were noted but were not tabulated as there was no mechanism to quantify the observations.
The recorded tabulated observations were analyzed using the Pearson's Chi-Square test for equality of variances on the SPSS v20 software.
Results
The normality tests, Kolmogorov-Smirnov, and Shapiro-Wilks revealed that the variable (mouth opening) followed normal distribution. Therefore, to analyze the data, parametric methods were applied. To compare mean values between procedures independent sample t-test was applied. Mean values between pre- and post-intervention were compared with paired t-test. To compare proportions between procedures, Chi-Square test was applied, if any expected cell frequency was less than five then Fisher's exact test was used. To analyze the data, SPSS (IBM SPSS Statistics for Windows, Version 23.0, Armonk, NY: IBM Corp. Released 2015) was used. Significance level was fixed as 5% (α = 0.05).
The overall mean age of the patients in our study was 29.93 ± 5.75 years, where Group A showed a mean age of 28.61 ± 5.43 years and Group B reported a mean age of 31.34 ± 5.84. Out of the 60 people, 35 (58.3%) patients were males and 25 (41.7%) females. The gender distribution was 1.22:1, with more male participants in Group A and in Group B [Graphs 1 and 2].
Graph 1.
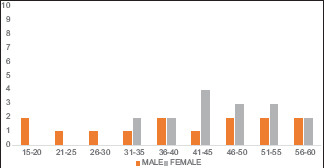
Showing gender distribution in the Group A
Graph 2.
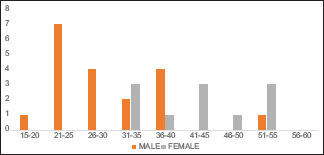
Showing gender distribution in the Group B
Mouth opening
At baseline, mean mouth opening in placentrex and hydrcortisone group was 24.81 ± 1.11 mm and 23.14 ± 1.25 mm, respectively. At post-treatment, mean mouth opening with placentrex injection was 30.00 ± 0.86 mm with a highly statistically significant (P-0.001) increase in mouth opening of 5.19 mm ± 1.33 mm and mouth opening increased to 34.83 mm ± 0.85 mm with hydrocortisone injection showing a highly statistically significant (P-0.001) improvement of 11.69 ± 1.26 mm [Table 1].
Table 1.
Paired samples T-Test to compare mean mouth opening between pre- and post-treatments
| Procedure | Mouth Opening (mm) | n | Mean | Std. Dev. | Mean Difference | Std. De. of difference | P |
|---|---|---|---|---|---|---|---|
| Placentrex | Post-Treatment | 31 | 30.00 | 0.856 | 5.194 | 1.327 | <0.001 |
| Pre-Treatment | 31 | 24.81 | 1.108 | ||||
| Hydrocortisone | Post-Treatment | 29 | 34.83 | 0.848 | 11.690 | 1.257 | <0.001 |
| Pre-Treatment | 29 | 23.14 | 1.246 |
P<0.05 is highly significant
Burning sensation
The distribution of burning sensation at baseline in Group A was mild in 32.3%, moderate in 35.5%, and severe in 32.3%. In Group B, burning sensation was mild in 27.6%, moderate in 34.5%, and severe in 37.9%. Post-treatment 29.0% patients in Group A reported mild burning sensation, 32.3% reported no burning sensation. In Group B, post-treatment burning sensation was mild in 48.3% patients and only 17.2% patients reported no burning sensation. These proportions are statistically highly significant (P < 0.001) [Graph 3].
Graph 3.
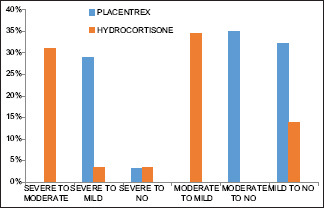
Showing the percentage of burning sensation in both groups post-treatments
Our results reported 100% reduction in pre-treatment mild and moderate burning sensation post-placentrax injection. In this group, 90% patients with severe burning sensation pre-treatment reported mild burning sensation post-treatment and 10% patients were completely cured. On the other hand, in Group B, 12.5% patients with mild burning sensation reported moderate burning sensation post-treatment and 37.5% patients remained unchanged. All the patients with moderate burning sensation improved to mild burning sensation post-treatment, whereas 81.8% patients with severe burning sensation reported moderate burning sensation vand 9.1% reduced to mild burning sensation.
Overall reduction in burning sensation in Groups A and B was highly statistically significant (P < 0.001). In placentrex group, the reduction of burning sensation from pre-treatment to post-treatment was severe to mild in 29.0%, severe to no sensation in 3.2%, moderate to no sensation in 35.5%, and mild to no sensation in 32.3%. In hydrocortisone procedure, the reduction of burning sensation from pre-treatment to post-treatment was severe to moderate in 31.0%, severe to mild in 3.4%, severe to no sensation in 3.4%, moderate to mild in 34.5%, mild to no sensation in 10.3%, and in one case (3.4%), the sensation worsened [Table 2].
Table 2.
Efficacy of both placentrex and hydrocortisone in case of improvement in burning sensation
| Improvement in burning sensation | Procedure | P | |||||
|---|---|---|---|---|---|---|---|
| Placentrex | Hydrocortisone | Total | |||||
| n | % | n | % | n | % | ||
| Severe to Moderate | 0 | 0.0 | 9 | 31.0 | 9 | 15.0 | <0.001 |
| Severe to Mild | 9 | 29.0 | 1 | 3.4 | 10 | 16.7 | |
| Severe to No | 1 | 3.2 | 1 | 3.4 | 2 | 3.3 | |
| Moderate to Mild | 0 | 0.0 | 10 | 34.5 | 10 | 16.7 | |
| Moderate to No | 10 | 35.5 | 0 | 0.0 | 11 | 18.3 | |
| Mild to No | 10 | 32.3 | 4 | 13.8 | 14 | 23.3 | |
| No change | 0 | 0.0 | 3 | 10.3 | 3 | 5.0 | |
| Worsened | 0 | 0.0 | 2 | 3.4 | 1 | 1.7 | |
| Total | 30 | 100.0 | 30 | 100.0 | 60 | 100.0 | |
Discussion
In our study of 60 patients, the patients were divided into 2 groups. First group was given submucosal injection of hydrocortisone and second group was given injection of placentrex with the mixing of local anesthetic agent lignocaine 2% with adrenaline 1:80000. There was improvement in burning sensation, blanching, ulceration and vesiculation, and mouth opening in 100% of patients.
In our study group, OSMF had an age range of 15-60 yrs. The peak incidence of disease in our series occurred in the 35-40 year age group. This finding was similar to the More et al., who reported a mean age of 36.67 ± 13.35 years. Other long-term studies conducted over a period of 7-10 years reported a peak incidence of 20-30 years.[14] We reported a male predominance which is similar to studies conducted by Sharma et al. and Kumar et al. In our study, mouth opening and burning sensation were better in males in both the groups. For improving mucosal health, hydrocortisone responded well in males and females responded well to placentrix.[15,16]
Areca nut significantly contributed toward pathogenesis of OSMF. In our series, the incidence of areca nut chewing habit was 100%, this included areca nut chewed alone or in combination of pan masala, gutkha, and betel quid. The incidence seen in our study concurs closely with the work done by Sharma et al. and Selvam et al.[14,17] Arecoline is an alkaloid found in areca nut predominantly known to increase the collagen production by stimulating fibroblasts, elevates the mRNA and protein expression of cystatin C, inhibits metalloproteinases, and stimulates tissue inhibitor of metalloproteinases. Keratinocyte growth factor-1, insulin-like growth factor-1, and IL-6 expression are upregulated in OSMF patients. All these factors cause increased collagen production and decreased breakdown.[18] In our study, burning sensation of mouth (100%) was the most common symptom followed by decreased mouth opening (95%). Ear ache and dysphagia were the least reported symptoms occurring in each 5% cases. The results concur with that of Van Wyk et al.[19] In our study, the signs closely mimicked those of Khanna et al.[20] in that the most common signs seen were trismus, blanching of mucosa, and presence of fibrous bands.
Hydrocortisone plays an important role in suppressing immune system by reducing activity and volume of lymphatic system. It reduces the inflammatory component by suppressing the migration of polymorphonuclear leukocytes and by reversing capillary permeability. It is a better corticosteroid for intralesional injection as it has better local potency, longer duration of action, and lesser systemic absorption. Steroids suppress the soluble factors released by sensitized lymphocytes, prevents fibrosis by decreasing fibroblastic proliferation, and collagen deposition. Steroids help in providing the initial symptomatic relief in patients with restricted mouth opening as it helps in clearing the juxta-epithelial inflammation along with collagen formation.[21,22]
Placental extract contains growth factors with anti-inflammatory and antiplatelet activity. The action of placenta extract is essentially biogenic stimulation and use is based on the tissue therapy method. According to this theory when animal and vegetable tissues are severed from the parent body and exposed to unfavorable conditions, but not mortal to their existence, the tissues undergo biogenic readjustment leading to development of substance in the state of their survival to ensure their vitality of biogenic stimulation. Such tissues or their extract when implanted or injected into the body after resistance of pathogenic factors stimulates metabolic regenerative process thereby favoring recovery.[23,24]
We felt that the period of follow-up was less and the patients should be followed up for a longer period to assess the true potential of the treatment regimens. A more detailed subdivision based on the type of tobacco abuse and duration to the onset and responders needs to be made. A correlation between the pre- and post-interventional hematologic status and to the responders also needs to be investigated. Although there were more participants, there were many people who relapsed on their habits and had to be excluded. So, a strong counselling team should also be made a part of the future investigations.
Overall, hydrocortisone seems to be a better regimen to improve the mucosal health and increase the mouth opening as compared to placentrex regimen. Although placentrex is better than hydrocortisone in reducing burning sensation.
Conclusion
The malady of submucous fibrosis is one of the most poorly understood and unsatisfactorily treated diseases. This is mainly because an exact etiology has not been identified, although considerable data have been accrued over the years in support of the role of areca nut. OSMF when detected in early stage is a reversible, hence primary health care centers play an important role in promoting health and awareness among patients with tobacco chewing, smoking habit. Health care providers should be able to identify the alarming symptoms presented by the patients such as burning sensation in the oral cavity and progressive difficulty in mouth opening and take necessary steps at the earliest. Innumerable medical modalities of treatment have been tried ranging from vitamin supplements, topical steroid applications, oral rinses with vinegar, oral physiotherapy to submucosal steroid injections, and inj placentrix. Overall, hydrocortisone seems to be a better regimen to improve the mucosal health and increase the mouth opening as compared to placentrex regimen. Although, placentrex is better than hydrocortisone in reducing burning sensation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Jha VK, Kandula S, Chinnannavar SN, Rout P, Mishra S, Bajoria AA. Oral submucous fibrosis: Correlation of clinical grading to various habit factors. J Int Soc Prev Community Dent. 2019;9:363–71. doi: 10.4103/jispcd.JISPCD_92_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ray JG, Chatterjee R, Chaudhuri K. Oral submucous fibrosis: A global challenge. Rising incidence, risk factors, management, and research priorities. Periodontology. 2000;2019(80):200–12. doi: 10.1111/prd.12277. [DOI] [PubMed] [Google Scholar]
- 3.Rai A, Siddiqui M, Parveen S, Parveen S, Rasheed A, Ali S. Molecular pathogenesis of oral submucous fibrosis: A critical appraisal. Biomed Pharmacol J. 2019;12:2027–36. [Google Scholar]
- 4.Priyadarshini SR, Das R, Panigrahi R, Pati AR, Choudhury BK. Betel nut chewing: A brief review. Indian J Public Health Res Dev. 2019:10. [Google Scholar]
- 5.Chole RH, Patil R. Drug treatment of oral sub mucous fibrosis–A review. Int J Contemp Med Res. 2016;3:996–8. [Google Scholar]
- 6.Chalkoo AH, Oberoi IS, Dhingra K. Assessment of various treatment modalities for the treatment of oral submucous fibrosis: A comparative study. J Adv Med Dent Sci Res. 2017;5:120. [Google Scholar]
- 7.Sri SB, Sathiyawathie RS, Gurunathan D. A review of perioperative corticosteroid use in oral and maxillofacial surgery. Drug Invent Today. 2019;12:611–3. [Google Scholar]
- 8.Bansal M. Efficacy of local and systemic corticosteroid and hyaluronidase therapy in oral submucous fibrosis: A histopathological study. Int J Otorhinolaryngol Head Neck Surg. 2019;5:459–64. [Google Scholar]
- 9.Shinde C, Saawarn N, Kohli S, Khare P, Singh A, Sagar K. Comparative efficacy of intralesional placental extract and intralesional triamcinolone acetonide in the management of OSMF. J Indian Acad Oral Med Radiol. 2019;31:328–328. [Google Scholar]
- 10.Rao NR, Villa A, More CB, Jayasinghe RD, Kerr AR, Johnson NW. Oral submucous fibrosis: A contemporary narrative review with a proposed inter-professional approach for an early diagnosis and clinical management. J Otolaryngol Head Neck Surg. 2020;49:3. doi: 10.1186/s40463-020-0399-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.James L, Shetty A, Rishi D, Abraham M. Management of oral submucous fibrosis with injection of hyaluronidase and dexamethasone in grade III oral submucous fibrosis: A retrospective study. J Int Oral Health. 2015;7:82. [PMC free article] [PubMed] [Google Scholar]
- 12.Wollina U, Verma SB, Ali FM, Patil K. Oral submucous fibrosis: An update. Clin Cosmetic Investig Dermatol. 2015;8:193. doi: 10.2147/CCID.S80576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reddy V, Wanjari PV, Reddy N, Reddy P. Oral submucous fibrosis: Correlation of clinical grading to various habit factors. Int J Dent Clin. 2011:3:21–4. doi: 10.4103/jispcd.JISPCD_92_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharma R, Raj SS, Miahra G, Reddy YG, Shenava S, Narang P. Prevalence of oral submucous fibrosis in patients visiting dental college in rural area of Jaipur, Rajasthan. J Indian Acad Oral Med Radiol. 2012;24:1–411. [Google Scholar]
- 15.Kumar A, Bagewadi A, Keluskar V, Singh M. Efficacy of lycopene in the management of oral submucous fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:207–13. doi: 10.1016/j.tripleo.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 16.More CB, Asrani M, Patel H, Adalja C. Oral submucous fibrosis – A hospital based retrospective study. Journal of Pearldent. 2010;1:25–31. [Google Scholar]
- 17.Selvam NP, Dayanand AA. Lycopene in the management of oral submucous fibrosis. Asian J Pharm Clin Res. 2013;6:58–61. [Google Scholar]
- 18.Kondaiah P, Pant I, Khan I. Molecular pathways regulated by areca nut in the etiopathogenesis of oral submucous fibrosis. Periodontology. 2000;2019(80):213–24. doi: 10.1111/prd.12266. [DOI] [PubMed] [Google Scholar]
- 19.Tom A, Baghirath V, Krishna B, Ganepalli A, Kumar JV, Mohan SP. Ultrastructural changes of collagen in different histopathological grades of oral submucous fibrosis. J Pharm Bioallied Sci. 2019;11(Suppl 2):S309. doi: 10.4103/JPBS.JPBS_20_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peng Q, Li H, Chen J, Wang Y, Tang Z. Oral submucous fibrosis in Asian countries. J Oral Pathol Med. 2019 doi: 10.1111/jop.12924. doi: 101111/jop 12924. [DOI] [PubMed] [Google Scholar]
- 21.Jimson S, Sankari SL, Masthan KM, Babu NA. Oral submucous fibrosis: A review on etiopathogenesis and recent trends in management. Indian J Public Health Res Dev. 2019;10:3123–7. [Google Scholar]
- 22.Tilakaratne WM, Ekanayaka RP, Herath M, Jayasinghe RD, Sitheeque M, Amarasinghe H. Intralesional corticosteroids as a treatment for restricted mouth opening in oral submucous fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122:224–31. doi: 10.1016/j.oooo.2015.11.023. [DOI] [PubMed] [Google Scholar]
- 23.Naik SM, Appaji MK, Goutham MK. Comparative study of intralesional triamicinolone acetonide and hyaluronidase Vs placental extract in 60 cases of oral submucous fibrosis. Indian J Head Neck Surg. 2012;3:59–65. [Google Scholar]
- 24.Singh DT, Padshetty S, Shreen S, Begam N, Vishwakarma SK, Khan AA. Injection placentrex in the management of oral submucous fibrosis. Int J Mod Sci Eng Technol. 2015;2:23–30. [Google Scholar]


