Abstract
The latest threat to global health is the form of the ongoing Coronavirus Disease 2019 (COVID-19) pandemic. This new coronavirus (SARS-COV-2) started as a local outbreak in Wuhan, China but soon tightened its grip on human lives around the globe. So far, we do not have a particularly effective anti-SARS-COV-2 vaccine or antiviral agent against COVID-19. Across the globe, many research organizations such as the National Institutes of Health (NIH), United States are studying and testing various drugs and vaccines for their effectiveness against SARS-COV-2. Currently, the principle fighting tool being promoted by the World Health Organization (WHO) is the prevention of acquiring SARS-COV-2 infection by following basic health hygiene rules and social distancing. We hereby discuss major non-pharmacological and pharmacological interventions.
Keywords: COVID-19, pandemic, quarantine, remdesivir, SARS-CoV-2, social distancing
Introduction
Within the last 2 decades, we have witnessed several viral outbreaks. Amongst the coronavirus outbreaks, the major one is the severe acute respiratory syndrome coronavirus (SARS-CoV) in 2002-2003, the Middle East respiratory syndrome coronavirus (MERS-CoV) in 2012 and the latest new coronavirus (SARS-COV-2) pandemic.[1] Just like the two preceding instances of the emergence of coronavirus diseases, the COVID-19 pandemic has put critical questions for public health care, qualitative research, and medical societies. Central and state agencies, along with volunteer organizations are working together to help all communities and healthcare facilities, including rural and semi-urban areas to deal with COVID-19 coronavirus pandemic.
Taming the COVID-19 Pandemic: Everyone has a Role to Play
As the world is grappling with the COVID-19 pandemic, it is important for everyone to recognize, realize and do their bit responsibly in order to successfully contain the community spread of the SARS-CoV-2 virus. United Nations, World Health Organization (WHO) and others have repeatedly stressed on the importance of collective approach as global citizens. In general, the three pillars around which the containment strategies are formulated to mitigate any pandemic including COVID-19:
Finding measures to control the source of infection,
Finding measures to stop transmission routes, and
Finding measures to protect the susceptible population
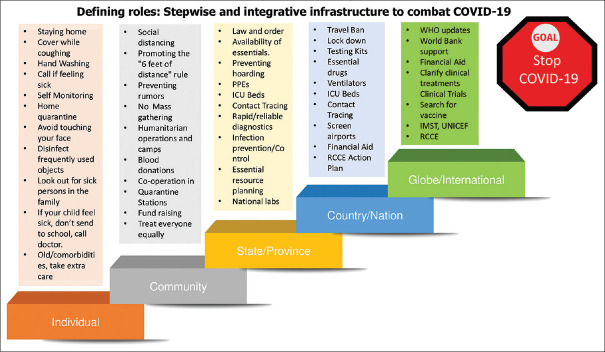
Mobilization of funds, increasing the critical care beds, providing care to confirmed COVID-19 patients, and testing the suspected cases are key to mitigate the COVID-19 pandemic, but as an individual, it is everyone's primary and moral responsibility to ensure that they abide to the government's decrees as issued [Figure 1].
Figure 1.
Defining roles: Stepwise and integrative infrastructure to combat COVID-19
Knowing COVID-19 Disease: How It Spreads, Who Can Transmit, and Their Implications on Infection Control and Prevention Strategies?
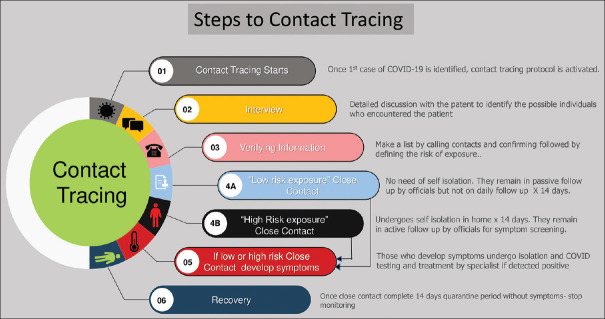
We discuss this for the purpose to educate the readers with the most recent available literature with regards to coronavirus transmission and modes of spread [Figure 2]. This will help us understand the significance of non-pharmacological interventions (NPIs) to combat against SARS-CoV-2 virus which is probably the more effective tool than the pharmacological interventions (PIs) [https://www.cdc.gov/nonpharmaceutical-interventions/index.html].
Figure 2.
Stepwise approach of contact tracing for COVID-19
Categories of transmission
The clinical symptoms of COVID-19 usually range from an asymptomatic course to very serve acute respiratory syndrome. Currently, the confirmed COVID-19 patients are considered as the primary sources of transmission. It is no brainer to think that respiratory viruses including SARS-CoV-2 would be most contagious when an infected person is at the peak of illness. The matter of concern is the wide range of incubation time from 0-24 days.[2] This means there might be a significant proportion of individuals who will not show symptoms for almost 3 weeks yet have the potential to transmit the infection. These patients are difficult to catch and here lies the importance of social distancing, avoiding mass gathering, stringent surveillance and aggressive contact tracing [Figure 2]. We are still in learning phase regarding SARS-CoV-2 transmission, but the following are the potential categories into which a person capable to transmit infection to others should fall into:
Pre-symptomatic transmission: A direct transmission from a person before he/she develops noticeable symptoms.
Asymptomatic transmission: A direct transmission from a person who never developed noticeable symptoms ever but is potential to infect others.
Symptomatic transmission: A direct transmission from a symptomatic person, through a contact (classical routes like droplets, airborne etc.)
Environmental/community transmission: An indirect transmission via contamination, in which an infected person doesn't recall coming in close contact with a confirmed case in a contact tracing survey.
Transmission routes
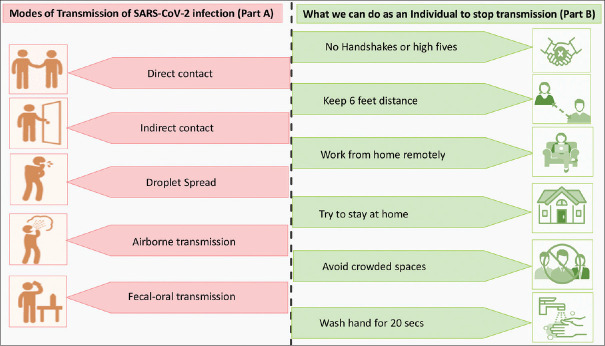
Despite COVID-19 turning from a local outbreak to global pandemic, there's a lot we still have not figured out about the way the SARS-CoV-2 virus spreads. Thanks to the data pooling and research studies, with each passing time, we're learning more about this deadly disease. From the starting, the experts from CDC and WHO have discussed “respiratory droplets” and direct close contact as the most likely mode of transmission which is common in many other respiratory viruses. Soon, new studies claimed viral shedding in stool, and saliva.[3] This finding along with the GI symptomatology of COVID-19 gave rise to the postulation of a potential fecal-oral transmission as well.[4] In addition, the scientists from University of Nebraska Medical Center have recently isolated SARS-CoV-2 viral RNA from the air and surface samples collected from COVID-19 occupied isolation rooms.[5] Procedures like intubation, nebulization, and bronchoscopy etc., can generate fine droplet nuclei (aerosols) that can travel for longer distances and remain suspended on air for longer time leading to airborne transmission [Figure 3, part A].
Figure 3.
Modes of Transmission of SARS-CoV-2 infection (Part A), and what we can do as an Individual to stop transmission (Part B)
Doremalen et al. from National Institute of Allergy and Infectious Diseases (NIAID), United States recently conducted in vitro study in order to study how long the SARS-CoV-2 survives on various surfaces? The authors found SARS-CoV-2 to be more stable on plastic and stainless steel when compared to cardboard and copper, and virus was viable and detectable up to 3 days after application to these surfaces.[6] Prolonged survival of SARS-CoV-2 on surfaces endorses the importance of frequent handwashing, avoiding touching face, nose and eyes, and sanitizing the “frequently touched items” [Figure 3, part B].
Individual Contribution
As an individual, there are many aspects through which we can contribute to help in containing the spread of COVID-19. Following few paragraphs discusses core concept of social distancing, self-quarantine, isolation depending on the degree of exposure to SARS-CoV-2 infection:
What is social distancing and why to practice?
We discussed in the section of “Categories of transmission” about the how an asymptomatic or pre-symptomatic individual could also transmit the SARS-CoV-2. Maintaining a considerable physical distance from others (who might or not might be contagious) could possibly minimize an individual's risk to catch from such individuals. So, what exactly is social distancing and how to practice it?
As per CDC, social distancing, which is also known as “physical distancing,” stands for keeping a space between oneself and other people outside home. The three essential components of in order to practice social distancing are- [1] Stay at least 6 feet (2 meters) from other people[2] Do not gather in groups, and[3] Stay out of crowded places and avoid mass gatherings [https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html].
Concept of “6 feet (2 meters) rule” has come up from the studies which showed that a person's exhaled air can travel anywhere from 3 to 6 feet which is called the breathing zone. Other person within the 3 to 6 feet is expected to inhale some of other person's exhaled breath.
What is self-quarantine and who should practice?
The practice of quarantine is not new and traces back to the old era of 14th-15th century. It originally came from “quarantena“, the Venetian language form, which means “40 days”. During that time, a 40-day isolation of ships and the crew members was practiced ensuring prevention against the plague.
The same principle can help protect the unexposed people by preventing exposure to the COVID-19 confirmed (by isolation) or suspected person (by quarantine). An individual who is exposed to a COVID-19 confirmed case might need to practice self-quarantine. Health experts based on the exposure divide it to “high risk” versus “low risk” exposure. “High risk or 1st degree exposures” are recommended to self-quarantine themselves for 14 days which provides enough time to know if they will become symptomatic and contagious. Contrarily, 2nd degree or more are considered as “Low risk exposures” and they are generally not required to be actively monitored, nor do they need to be quarantined.
Standard self-quarantine measures include:
Practicing standard hygiene and washing hands as per standards frequently
Self-monitoring for upper respiratory tract symptoms, temperature or shortness of breath
Keeping away personal use items like towels, cloths and utensils
Staying at home and not allowing any visitors
Maintaining social distancing even at home that is staying away by at least 2 meters from family members.
What is isolation and who are the ones to follow?
Isolation is a step ahead to quarantine and is used for individuals with confirmed COVID-19 disease. Isolation can be done either at home or in hospital depending upon how sick the person is. If practicing home-isolation then, patient should seek immediate medical attention in case of worsening symptoms like difficulty breathing. The assessment to discontinue home isolation varies on a case-by-case basis, in consultation with treating physicians.
In brief, social distancing is a measure for everyone to follow in order to prevent exposure to self or others by maintaining physical distance. Isolation and quarantine are the measures that prohibits confirmed or suspected cases from transmitting infection to the susceptible public by restricting their movements [Figure 3]. Other expectations from an individual as a responsible citizen are: [https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html]
• Helping yourself
Following the right way of hand washing (soap and running water for 20 secs, following all steps)
Frequent cleaning of hands with alcohol-based hand sanitizers.
Covering the face while coughing
Avoid close contact when having cough, fever and myalgia.
Safe disposal of the used masks or soiled materials
Self-monitoring for symptoms (fever, myalgia, dry cough)
Call doctor and get emergency help if you become short of breath
Be smart and well informed [www.who.int/COVID-19]
Follow the public health advice issued by local health authority and WHO
Avoid eating in public places and dining out. Instead use drive thru or delivery options.
Avoid unnecessary travels, shopping malls
Post pone routine surgeries, health care appointments.
Have extra supplies for live saving drugs like anticancer medications, anti-diabetic medications, blood thinners, anticoagulants etc.
• Helping others
Don't spread rumors and fake news and always check for the authenticity of the news
Disinfecting the objects and surfaces of frequent use like tables, door handles, light switches, countertops etc.
Educate young kids and children to follow health hygiene practice
Emotional support: Be kind and supportive to others
Check in frequently those affected with COVID-19
Be respectful towards affected people
Do not visit nursing homes or long-term facility care
• Helping society
Share the latest and genuine information
Avoid social gathering and crowded places
Social distancing
Do not stockpile essential items (groceries and food items) more than required
Recognizing the Vulnerable Population and Providing Extra Care
There are ample evidence that have shown that older individuals, patients with multiple co-morbidities, cancer patients etc., have more probability to have complicated course, and a higher mortality.[7,8] The following subset of population are vulnerable to critical illness, and hence need special attention in home, community and in medical centers.
Old frail individuals
-
People with disabilities
- People with limitation in mobility or who cannot prevent themselves coming into close contact with others.
- People with difficulty in comprehending or practicing the heath hygiene measures
- People who are not able to communicate their concerning symptoms
- Pregnant women (current or recent within two weeks)
-
Multiple comorbidities
- Patients with benign hematological diseases disorders (e.g. Thalassemia, sickle cell disease etc.)
- Patients with malignancies
- Patients with Chronic kidney disease, and patients on dialysis
- Patients with Chronic liver disease (e.g. cirrhosis, chronic hepatitis)
- Patients with compromised immune system (e.g. chemotherapy, radiation, post organ or stem cell transplant, taking immunosuppressants like mycophenolate, steroids, cyclosporine, HIV or AIDS)
- Patients with endocrine disorders and metabolic disorders (e.g. diabetes mellitus, inherited metabolic disorders, mitochondrial disorders)
- Patients with cardiovascular disorders (e.g. congestive heart failure, coronary artery disease)
- Patients with chronic lung disorders (e.g. asthma, emphysema)
- Patients with neurological or neurodevelopment conditions (e.g. stroke, cerebral palsy)
Role of Community and faith-based organizations
Community responsibility is nothing, but the magnified version of every individual's conducts put together. Worldwide, there have been incidences reported on breeching the authorities’ law and regulations, mass gathering and holding religious events. These acts not only risk the individuals involved in such activities and gatherings but also nullifies the hard work and efforts put together by disciplined members of the community. In such condition's leaders of faith-based organizations who are being followed as role models in the community need to come forward and endorse the importance of social distancing and practicing health hygiene. They can serve as the connecting link between government/heath agencies and community people.[9]
Role of Social Media in COVID-19 Pandemic: Both a Blessing and a Curse
During SARS pandemic in 2002-03, social media and telecommunication was not widely accessible. Moving forward, during last 2 decades there has been a enormous advancement in telecom and mass media sectors. State agencies have a dual challenge at present, first is COVID-19 pandemic and second associated “Infodemic”.[10] Apart from the traditional media channels like newspapers, broadcasting and television, now there are new generation media portals like WhatsApp, Telegram, Twitter etc., which are more popular and are easy to reach. The circulation of fake news and rumors regarding COVID-19 disease has also therefore become a nuisance. WHO, CDC and many central agencies are constantly monitoring for any false propaganda to avoid unnecessary panic. The emphasize should be on the transmitting a latest, authentic and resourceful information in a timely fashion using the popular and commonly used social media. [https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for public/myth-busters]
Role of State and Nation Agencies: National Preparedness and Response
While whole hierarchical infrastructure is responsible, but the national government is default leader for overall coordination, communication and execution during COVID-19 pandemic. The state/central governments and agencies have the most burden to gather the heath and financial resources and implement in an efficient manner.
Features of an efficient pandemic response taskforce
Planning and executing a preparedness exercise are the best way to be ahead of curve to contain a pandemic like current COVID-19 pandemic. Such pandemic preparedness exercises occur within the framework of national and international priorities, available funds, and limited resources.
Singapore built a robust system; The Disease Outbreak Response System Condition (DORSCON) framework was established after SARS and H1N1 for tracing and containing epidemics/pandemics.[11] South Korea and Taiwan are other two countries who have followed stringent contact tracing and were able to successfully contain the COVID-19 damage. The story of Singapore's successful containment of virus spread was scripted by the scientists, health officials and doctors from National Centre for Infectious Diseases (NCID), the National Public Health Laboratory (NPHL), and the Agency for Science, Technology and Research (A*STAR). Lin et al. from NCID recently outlined the Singapore's COVID-19 response model which included the following major steps taken leading to mitigation of the SARS-CoV-2 infection.[12]
Immediate mapping of COVID-19's possible transmission routes
Developing rapid and reliable diagnostics
Establishing clinical criteria to classify patients
Charting the clinical treatment protocol based on available literature
Communicating the right and authentic information proactively via social media
Providing the healthcare workers with adequate PPEs
International collaboration on developing a vaccine
Risk communication, community engagement (RCCE): A WHO initiative
In response to COVID-19, WHO is also promoting an excellent model to ensure a two-way interaction between health authorities and at-risk populations. The model, known as risk communication, community engagement (RCCE), constitutes an effective action plan for an efficient communication with the community people, engaging with NGO's, local authorities and other health care providers to help them organize and safeguard themselves, and others. [https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/risk-communication-and-community-engagement]
Briefly, the major strategies towards a successful containment of COVID-19 pandemic are rapid identification, diagnosis and treatment of the cases, efficient contact tracing and follow up, infection prevention and control in clinics, old age homes, and rehabilitation centers, appropriate screening of travelers, and dissemination of correct information via awareness and educational programs.
Flattening the COVID-19 epidemiological curve
It is important to understand that without any intervention, the epidemiological curve for COVID-19 pandemic will have rapid acceleration, especially critical and sick COVID-19 cases which would most likely overburden the health care capacity. Hence, ideal would be to intervene to aim for flattening the epidemiological the curve by:[1] decreasing the acceleration,[2] decreasing the peak, and[3] prolonging the pandemic so that all cases (including new and old ones) fall within the threshold of health care capacity of a particular country [Figure 4]. A hypothetical mathematical model on US and UK have shown that an unmitigated COVID-19 pandemic would kill approximately exceed 20,000,000 and 500,000 respectively (assuming 30% attack rate and 2% mortality rate). Hence, these gigantic death figures signify the importance of a timely intervention.
Figure 4.
Schema to understand the impact of interventions on flattening the curve
Looking for an ideal Intervention strategy
For containment of COVID-19 pandemic, countries can follow either of the two typical intervention strategies:[1] Suppression approach, locking down cities at epicenter, and general social distancing, or[2] Mitigation approach, that only aims for pandemic to slow down but not a complete halt. For reducing peak healthcare demand. Both strategies have their own merits and demerits; it becomes exceedingly tough to say which one is better and every country needs to introspect its health resources, percentage population to disease susceptibility and economic stability before choosing any of the two approach.[13]
• Suppression strategy
This is an intense strategy out of both. It aims in implementing measures in order to reverse the basic reproduction number (R0) to less than 1.[14] This will possibly reduce the total number of cases to significantly lower numbers – which health care system could easily tackle. Social distancing of entire population, locking down the entire epicenter, nearby cities, full travel ban, closure of schools, universities, preventing people to go to work and mass gathering are few of the drastic steps during exercising this strategy. The merit is that this aims to bring a complete halt to pandemic growth and possibly reverse it by aiming for a R0 < 1. The downfall is that it is indeed a very stringent step which may not be practical and feasible for many countries. Also, maintaining this strategy indefinitely till definitive therapies like vaccine or medicine are available will need community and public cooperation. Also, due to stringent lockdown, the likelihood to develop herd immunity is minimal which poses a threat for recurrence of pandemic in the form of the second wave as soon as restrictions are uplifted.
• Mitigation Strategy
This is lesser intense strategy which aims to slow down the pandemic without aim of decreasing the R0 to less than 1. This allows the pandemic to go ahead but at a controlled rate. This has advantage of reducing the peak health care demand so that the cases would be accommodated within the capacity of health care system. In mitigation strategy, social distancing is limited to be the elderly, patients with chronic diseases or with multiple comorbidities only. The downfall of this strategy is a slow peak may not necessarily be below the health capacity of a particular country. It depends on how well resourceful the country was before pandemic, the crippled the infrastructure, the more likelihood that peak despite slow rising would ultimately overpower the health capacity. Another drawback is that mitigation strategy has to be continued for longer period than suppression strategy till every individual develops a sufficient level of herd immunity.
Global Contribution: PAN-Collaboration to Contain COVID-19 Pandemic
The current COVID-19 pandemic is a quality check of the threshold and stability of various sectors, health care systems, economic stability, national and international ties, and social safety nets. Although almost all countries are COVID-19 struck but the impact of the pandemic has been variable in terms of mortality, disease burden, and economic damage. International organizations like WHO, UN, World bank and many other multinational non-governmental organizations (NGOs) are engaged in collaborative work system to fight against COVID-19 pandemic.
WHO was the first to respond to the call from China regarding the outbreak on 1st Jan 2020. With WHO's initiative, an Incident Management Support Team (IMST) was set up with a three-tier system functioning at headquarters, regional headquarters and country level. Since then, WHO is constantly engaging with all countries and national agencies while they prepare themselves to respond to COVID-19 pandemic. WHO is also closely working it other close allies like United Nations (UN) and International Monetary Fund (IMF). The World Bank group has launched its first COVID-19 pandemic health support with special attention towards the underdeveloped nations. Given the unparalleled challenges, the broader economic program plans to spend up to $160 billion over next 15 months. The funds are expected to be utilized across different sectors towards wellbeing of the poor and vulnerable, backing businesses, and to overturn the economy slowdown. Other organizations like The UN Children's Fund (UNICEF) are involved supplying essential personal protective equipment like N95 respirators, surgical masks, thermometers, testing COVID testing kits, gloves and medical gowns across the globe.
Pharmacological Interventions
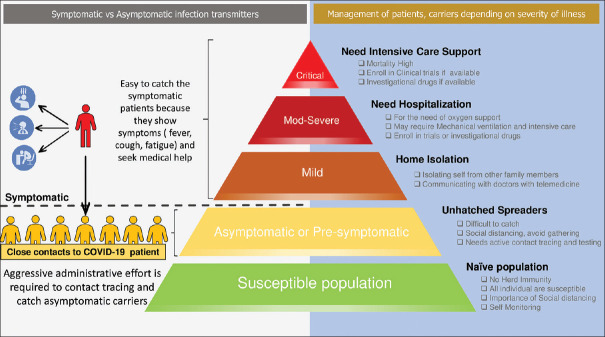
Unfortunately, to date, no drug or vaccine has demonstrated an efficacy for COVID-19 patients [Figure 5]. Some of the treatments are currently being assessed for their role in COVID-19. Most of these agents have shown efficacy for other diseases, but, their use for COVID-19 remains investigational and under trial.
Figure 5.
Schema of management of patients, carriers depending on severity of illness
• Remdesivir: Remdesivir has been found to have activity against SARS-CoV-2 in vitro and against SARS and MERS in both vitro and animal studies. In total, there are 6 remdesivir related ongoing studies which are expected to enlighten us more regarding its therapeutic dose, days of therapy, side effects and effectiveness over standard care in near future. A recent preliminary data on this drug shows that out of 53 severe COVID-19 patients who received remdesivir, more than two-thirds (68%) of the patients improved. The common adverse events noted were increased liver enzymes, loose stools, skin rash, rise in creatinine, and hypotension.[15]
• Convalescent plasma: This is a passive antibody therapy and has been recently in news for its potential use to treat COVID-19 patients. The basic concept is to make use of the high titers of neutralizing immunoglobulin-containing plasma from recovered COVID-19 patients. This therapy was also found useful during previous SARS pandemic. Report of use of convalescent plasma on 5 mechanically ventilated COVID-19 patients at Shenzhen Third People's Hospital, China have shown encouraging results. The study showed a decrease in nasopharyngeal SARS-CoV-2 viral load, a reduction in COVID-19 disease severity score, and an improved oxygenation at the end of 12 days of plasma therapy.[16] The logistic challenge behind its generalization could be finding an appropriate donor and confirming high titers of neutralizing activity of plasma. While it is too early to conclude, but based on experience with previous outbreaks, and preliminary results on COVID-19, this therapy has the potential to decrease the severity of critically ill patients.
• High-dose intravenous immunoglobulin (IVIg): IVIg is another blood product that constitutes of polyclonal immunoglobulins extracted from healthy donors. IVIg has a well-established role in many autoimmune, infectious, neuromuscular, and idiopathic disorders. Previously conducted studies have shown that IVIg has an immunomodulatory and a “tune down” effect via its interaction with T-cells, antigen-presenting cells and other cytokine producing cells.[17] Based on reports of its clinical benefits with tolerable side-effects in SARS and MERS patients, IVIg therapy is currently being used on case-by-case basis for COVID-19 patients as well. Cao et al. in their 3 patients’ series found IVIg use to be associated with clinical and radiological improvement and that all 3 patients survived and were successfully discharged.[18] Currently, a RCT (NCT 04261426) is underway to evaluate the efficacy of high-dose IVIg in severe COVID-19, which is expected to give us more evidence.
• Hydroxychloroquine/chloroquine: Both these agents have been stated to inhibit SARS-CoV-2 in vitro. However, due to insufficient data on humans so far, FDA strongly recommends enrolling COVID-19 patients on clinical trials whenever possible. Outside clinical trial, FDA has permitted emergency use authorization of hydroxychloroquine (HCQ) on a case-by-case basis. Many study groups are claiming HCQ use was associated with a faster recovery time, decreased nasopharyngeal viral shedding, improved radiological chest imaging findings, and lower chance of progression to severe illness. Unfortunately, many of these studies had lacunas of either small patient population, lack of double blinding or placebo control and so on. Due to this, a well-organized meta-analysis is probably not possible.[19] Also, not to forget about the significant side-effects of the HCQ like prolonged QT interval, retinopathy or cardiomyopathy. Hence, it is important for no one to use HCQ without medical advice and supervision.
• Monoclonal antibodies/IL-6 pathway inhibitors: Interleukin (IL)-6 receptor inhibitors (Tocilizumab, sarilumab and siltuximab) have successfully shown their clinical usefulness in many inflammatory diseases and many cancers. Tocilizumab has a licensed indication for use in cytokine release syndrome (CRS). Recent data on COVID-19 have shown critically ill patients to have variable degree of CRS (mild or severe) that could lead to a pro-inflammatory phenomenon, capillary leak reaction with fluid shift into the alveoli, resulting in respiratory distress and even ARDS.[20] Based on this, China has approved use of tocilizumab in COVID-19 pneumonia cases (ChiCTR2000029765). The ongoing randomized, double-blind, placebo-controlled phase II/III clinical trials are studying the safety and efficacy of tocilizumab (NCT04320615) and sarilumab (NCT04315298) in severe COVID-19 pneumonia.
• Cell and biological therapy
Mesenchymal stem cells (MSCs) have been studied for their comprehensive and robust immunomodulatory function. Significant studies so far have been done on immune mediated disorders like systemic lupus erythematosus and graft-versus-host disease. Len et al. have studied the immunomodulatory influence of MSCs in patients with COVID-19 pneumonia. They gave 1 million MSCs per kilogram body weight to 7 patients and demonstrated a notable clinical improvement in all patients with no adverse effects.[21] Based on this observation, a clinical trial (NCT04315987) is underway to study the efficacy of ACE2-MSC transplantation in COVID-19 pneumonia.
Role of Family Physicians during COVID-19 Pandemic
Family physicians have always been the backbone of health care and clinical practice. A family physician owns a professional responsibility to provide comprehensive health care service and holds a broad array of capabilities. COVID-19 pandemic poses a great challenge within the primary care and mandates family physicians to be abreast of the newest updates, preventive measures, latest epidemiological trends, and available treatment modalities to guide their patients and to clarify the immediate concerns of other care givers.[22,23,24,25] Apart from COVID-19, family physicians must be extremely alert not to miss the ongoing endemic diseases based on the local disease epidemiology. Lam et al. recently discussed the challenges faced by family physicians in Singapore during a dual outbreak of COVID-19 pandemic combined with dengue endemic.[25] Nowadays, through various telecom services like Skype, Facetime etc., it is possible for the family physicians to engage with the patients via telemedicine for both COVID and non-COVID related issues. Concerning symptoms like high grade fever, shortness of breath and cough can be easily discussed over phone or video call and patient can be guided directly to COVID-19 testing center thereby avoiding unwarranted personal visits to doctors office, long waiting in the queue, travelling to hospital and so on.[24] This not only prioritizes the diagnosis and treatment, but also prevent the community transmission to other healthy individuals. Upgradation of the existing community health centers to advanced Public Health Preparedness Clinics is an innovative way to provide one stop health service for consulting, testing, treating and referring COVID-19 suspects. This concept is currently successfully being implemented by the countries like Singapore, one of the few countries who have successfully contained the community transmission SARS-CoV-2 virus.
Conclusion
There is a pressing need but a narrow window of opportunity to address the gaps in global preparedness for a second wave of COVID-19. Definitive medical countermeasures are not expected to roll in the market for general public utilization for at least 1-2 years. Hence, till then, the non-pharmacological measures hold the prime importance to prevent further waves of COVID-19. Other sections that simultaneously might need attention are social harmony, political unpredictability, economic slowdown, poverty, other viral outbreaks and food scarcity. This COVID-19 pandemic seems devastating, but in reality, every human being can help hold up its the spread.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sahu KK, Mishra AK, Lal A. COVID-2019: Update on epidemiology, disease spread and management. Monaldi Arch Chest Dis. 2020:90. doi: 10.4081/monaldi.2020.1292. doi: 104081/monaldi20201292. [DOI] [PubMed] [Google Scholar]
- 2.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China? N Engl J Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gu J, Han B, Wang J. COVID-19: Gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. 2020;158:1518–9. doi: 10.1053/j.gastro.2020.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tian Y, Rong L, Nian W, He Y. Review article: Gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51:843–51. doi: 10.1111/apt.15731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Santarpia JL, Rivera DN, Herrera V, Morwitzer MJ, Creager H, Santarpia GW, et al. Transmission potential of SARS-CoV-2 in viral shedding observed at the University of Nebraska Medical Center. medRxiv. 2020 (published online Mar 26) doi: 101101/2020032320039446. [Google Scholar]
- 6.Van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–7. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sahu KK, Mishra AK, Lal A. A twin challenge to handle: COVID-19 with pregnancy. J Med Virol. 2020 doi: 10.1002/jmv.25784. doi: 101002/jmv25784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sahu KK, Jindal V, Siddiqui AD. Managing COVID-19 in patients with cancer: A double blow for oncologists. JCO Oncol Pract. 2020;16:223–5. doi: 10.1200/OP.20.00167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ebrahim SH, Ahmed QA, Gozzer E, Schlagenhauf P, Memish ZA. Covid-19 and community mitigation strategies in a pandemic. BMJ. 2020;368:m1066. doi: 10.1136/bmj.m1066. [DOI] [PubMed] [Google Scholar]
- 10.Orso D, Federici N, Copetti R, Vetrugno L, Bove T. Infodemic and the spread of fake news in the COVID-19-era. Eur J Emerg Med. 2020 doi: 10.1097/MEJ.0000000000000713. doi: 101097/MEJ0000000000000713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tambyah PA, Lye DC. Responding to the new influenza A (H1N1) 2009 pandemic: Moving forward together. Singapore Med J. 2009;50:554–5. [PubMed] [Google Scholar]
- 12.Lin RJ, Lee TH, Lye DCB. From SARS to COVID-19: The Singapore journey. Med J Aust. doi: 10.5694/mja2.50623. Published online: 6 April 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eubank S, Eckstrand I, Lewis B, Venkatramanan S, Marathe M, Barrett CL, Ferguson, et al. “Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand”. Bull Math Biol. 2020;82:52. doi: 10.1007/s11538-020-00726-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kassem AM. COVID-19: Mitigation or suppression? Arab J Gastroenterol. 2020;21:1–2. doi: 10.1016/j.ajg.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grein J, Ohmagari N, Shin D, Diaz G, Asperges E, Castagna A, et al. Compassionate use of remdesivir for patients with severe Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMoa2007016. doi: 101056/NEJMoa2007016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shen C, Wang Z, Zhao F, Yang Y, Li J, Yuan J, et al. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma. JAMA. 2020 doi: 10.1001/jama.2020.4783. doi: 101001/jama 20204783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferrara G, Zumla A, Maeurer M. Intravenous immunoglobulin (IVIg) for refractory and difficult-to-treat infections. Am J Med. 2012;125:1036e1–8. doi: 10.1016/j.amjmed.2012.01.023. [DOI] [PubMed] [Google Scholar]
- 18.Cao W, Liu X, Bai T, Fan H, Hong K, Song H, et al. High-dose intravenous immunoglobulin as a therapeutic option for deteriorating patients with coronavirus disease 2019. Open Forum Infect Dis. 2020;7:ofaa102. doi: 10.1093/ofid/ofaa102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah S, Das S, Jain A, Misra DP, Negi VS. A systematic review of the prophylactic role of chloroquine and hydroxychloroquine in coronavirus disease-19 (COVID-19) Int J Rheum Dis. 2020 doi: 10.1111/1756-185X.13842. doi: 101111/1756-185X13842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang C, Wu Z, Li JW, Zhao H, Wang GQ. The cytokine release syndrome (CRS) of severe COVID-19 and Interleukin-6 receptor (IL-6R) antagonist Tocilizumab may be the key to reduce the mortality? Int J Antimicrob Agents. 2020:105954. doi: 10.1016/j.ijantimicag.2020.105954. doi: 10.1016/j.ijantimicag. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leng Z, Zhu R, Hou W, Feng Y, Yang Y, Han, et al. Transplantation of ACE2 (-) mesenchymal stem cells improves the outcome of patients with COVID-19 pneumonia. Aging Dis. 2020;11:216–28. doi: 10.14336/AD.2020.0228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Sutter A, Llor C, Maier M, Mallen C, Tatsioni A, van Weert H. Family medicine in times of ‘COVID-19': A generalists’ voice. Eur J Gen Pract. 2020;26:58–60. doi: 10.1080/13814788.2020.1757312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sexton S. AFP's approach to COVID-19. Am Fam Physician. 2020;101:518. [PubMed] [Google Scholar]
- 24.Sahu KK, Mishra AK, Martin K, Chastain I. COVID-19 and clinical mimics Correct diagnosis is the key to appropriate therapy. Monaldi Arch Chest Dis. 2020:90. doi: 10.4081/monaldi.2020.1327. doi: 104081/monaldi20201327. [DOI] [PubMed] [Google Scholar]
- 25.Lam LTM, Chua YX, Tan DHY. Roles and challenges of primary care physicians facing a dual outbreak of COVID-19 and dengue in Singapore. Fam Pract. 2020 doi: 10.1093/fampra/cmaa047. pii: cmaa047 doi: 101093/fampra/cmaa047. [DOI] [PMC free article] [PubMed] [Google Scholar]