Abstract
Rheumatoid Arthritis (RA) is a form of arthritis characterized by joint pain, stiffness, swelling and deformity. There has been plethora of researches in the area of rheumatoid arthritis which focused on immune system, genetic predisposition and newer treatment modalities. Researchers have also examined the cognitive decline, physical deficits and their interrelationship in patients with RA. Among several psychological aspects depression, anxiety and stress emerge as significant psychological co morbidity. RA is a multifactorial, chronic, inflammatory disease primarily affects physical functioning as well as psychological aspects. Pain, fatigue, duration of disease, disease activity and functional disability are very common in rheumatoid arthritis which is leading cause of psychological distress and functional disability. Various types of neuropsychological battery were used to assess the decline in specific areas like attention, executive functioning, visuo-spatial learning, verbal learning/memory etc. These functions were compared with other type of arthritis disease. Also, various other factors like depression, cardiovascular diseases, other systemic and chronic disease and concomitant drugs intake etc. also affected cognitive functioning in Rheumatoid Arthritis patients. The objective of this review was to identify and explore the rates and types of cognitive impairment in RA. This present review paper systematically examines and summarizes the cognition related decrement in arthritis patients. Multiple research articles between 1990 to 2018 were searched. These reviews were evaluated and synthesized using a narrative and descriptive approach.
Keywords: Attentional functioning, cognitive impairment, pain, rheumatoid arthritis, Yoga
Introduction
Rheumatoid arthritis (RA)
Rheumatoid arthritis (RA) is a systemic disease that involves systems/organs other than the bones and joint alone.[1] RA is an autoimmune disease wherein white blood cells attack the organism's own tissues, cause symmetrical joint pain associated with swelling, stiffness, and deformity. It is the most common rheumatic disorder among connective tissue disorders. It is a persistent and progressive inflammatory process, which begins with the synovial membrane and ends with the destruction, deformation, and impairment of articular tissues and articulatory function.[2] Etiology is unclear. However, various factors like climate, race, diet, psychosomatic disorders, trauma, endocrine dysfunction, biochemical disorders, hereditary influences, disturbances in the autoimmunity, and infection have been found to initiate the rheumatoid process. The symptoms and progression of RA vary widely from person to person. It tends to strike during the most productive years of adulthood, between the ages of 20 and 40, and is a chronic disabling condition often causing pain and deformity. Women are affected more than men in a ratio of 3:1.[1]
There is no cure for RA, but medical treatments are useful for reducing pain at a normal level. Medical treatment is aimed at the reduction of symptoms by attacking the inflammation and prevention of joint damage. Medical management of RA involves the use of analgesics, non-steroid anti-inflammatory agents (NSAIDs) and corticosteroids. Besides medical treatments, physical exercise, yoga, and cognitive behavior therapies enhance the functional ability, quality of life, well-being as well as physical and mental health.
Clinical features of RA
The disease involves several organs and synovial tissues with various systemic manifestations. The involvement of the synovial lining of tendon sheaths and ligaments gives rise to pain, swelling, increased redness, and stiffness. The involvement of ligaments in the cervical region may produce subluxation with pain and neurological signs. The involvement of articular surfaces of the joints and its surrounding soft tissues produces cardinal joint symptoms that eventually are responsible for the crippling disorganization of the concerned joint. The extent of physical disability is directly proportional to these changes. They begin with pain, tenderness, warmth, erythema, and effusion. If not controlled, they progress to stiffness, cartilage wear and tear, and osteoporosis resulting in joint subluxation and dislocation. In the majority of patients the wrist, metacarpophalangeal and knee joints are involved early as compared to the other joints. Progressive weakness of the muscle groups further complicates the patient's situation.[1]
RA: Pain and cognitive functioning
Pain is a subjective, multidimensional experience that can have a marked impact on both the physiological and psychological state of an individual. Chronic pain has bio psychosocial implications, affecting relationships, capacity for work, mood, quality of life, and disabling limitations on physical function.[3,4] Studies suggested that pain severity negatively associated with cognitive task performance.[5,6,7]
Cognitive functioning is thought to be affected in chronic pain (pain persisting for 3-6 months or longer) patients. It is hypothesized that because neural systems involved in cognition and pain processing are closely linked, they may modulate one another reciprocally. Cognition has been described as the brain's acquisition, processing, storage, and retrieval of information.[8] Co-morbid affective disorders (such as depression, stress, and anxiety), and the effects of fatigue and sleep disturbance and medication use are sometimes, but not always, considered as important factors affecting cognition in RA.
Cognitive impairment is described as difficulty in remembering, learning new things, problem-solving, concentrating, or making decisions. Previous studies also reported that cognitive functioning is also affected by RA. Bartolini et al. observed that cognitive dysfunction was common in RA patients with prevalence rates ranging from 38% (divided/sustained attention and mental flexibility) to 71% (visuo-spatial and planning functions).[9]
The study by Dick et al. on attentional functioning in RA and its comparison with fibromyalgia (FM) and musculoskeletal (MSK) pain patients revealed that impaired cognitive functioning existed in all the groups.[10] This study supports previous findings by reporting that many chronic pain patients have significant attentional dysfunction. Ziarko et al. revealed that pain intensity, coping strategies, and ego resiliency depend on the severity of anxiety and depression.[11] In another study, Dick and Rashiq examined the disruption in attention and memory processes accompanied by chronic pain and found that 2/3 of participants with chronic pain had impaired attention and significantly greater difficulties in maintaining a memory trace during a challenging test of working memory.[12]
Brown et al. revealed that RA patients with pain and depression performed poorly on the cognitive task. However, the effects of pain on cognition were no longer found when depression was entered as a mediated variable.[13] Another study also reported a negative association between arthritis pain and performance on a task requiring selective attention, inhibition, and working memory was found.[14]
Bilgici et al. compared three groups, i.e. healthy controls, RA, and FM patients on measures of cognitive functions (global attention/working memory, language, visual and verbal memory, visuospatial process, and executive function) and observed that FM and RA patients performed poorly on most of the measures of cognitive functions compared with healthy controls.[15] However, differences in cognitive functions between patients with FM and RA were found non-significant except for the measure of executive functions. Although cognitive symptoms may be exacerbated by the presence of fatigue, sleep problems, and pain, the relationship of these factors to cognitive problems in FM patients is unclear.
A recent study of three groups of patients (acute pain, regularly recurrent pain, and persistent pain) on three measures of cognitive functions (sustained attention, cognitive control, and psychomotor ability) was found that patients with constant pain lead to a decline in performance on sustained attention and psychomotor functions as compared to healthy controls. Patients with acute pain have a significant relationship with psychomotor ability; this reduced the performance on psychomotor ability. The individuals who have regularly current pain have a major impact on decrementing the performance in sustained attention.[16] Brain parts such as the prefrontal cortex, anterior cingulate cortex, and secondary somatosensory cortex have a major role in controlled and higher-order cognitive processing which involves attention, cognitive control, and certain psychomotor abilities.[17,18]
Moore et al. found that experimentally induced thermal pain affected task switching, dual attention, and attentional span.[19] It clearly suggests that tasks requiring higher-orderr processes, particularly executive control are susceptible to pain interference.[20] Using neuropsychological tests battery, Simos et al. found that 20% of RA patients were cognitively impaired. It is assumed that cognitive impairment leads to decrease in performance in physical activity and other executive functioning.[21]
Low cognitive function was significantly associated with the subsequent loss of physical function in daily activities with a significant relationship between cognitive function and functional limitation, especially in older adults.[22] Shin et al. investigated the relationship between cognitive function and physical function in RA, using 12 standardized neuropsychological measures and found that cognitive impairment was significantly associated with greater functional limitations in patients with RA and this decrement was associated with performance-based and self-reported measures.[23] Cognitive difficulties in RA may have enough impact on daily functioning treatment management and adaption to illness.[23,24] The above studies have shown that RA is a disease having pain and physical symptoms but there is a psychological aspect regarding this disease. This pain affects work, sleep, daily activities and negatively impacts an individual's quality of life.[25] The following summary in Table 1 shows some previous research studies of RA with different psychological variables.
Table 1.
Summary of research studies
| Author | N (sample) | Measures/Variables | Outcomes |
|---|---|---|---|
| Dick, Eccleston and Crombez (2002)[10] | FM=20 RA=20 MSK=20 And 20 pain-free controls | Attentional functioning: selective attention, sustained attention, attentional switching, and auditory-verbal working memory | Pain patients had impaired cognitive functioning on an ecological sensitive neuropsychological test of everyday attention. |
| Attentional deficits in the patients’ group were significant on tasks of selective and sustained attention and auditory-verball working memory. | |||
| FM patients showed a significantly higher level of anxiety than the other 3 groups. | |||
| Dick and Rashiq (2007)[12] | 24 participants | Pain, pain catastrophizing, attentional functioning | 2/3 of participants with chronic pain had found impaired on attentional task and they had significantly greater difficulties in maintaining a memory trace during a challenging test of working memory. |
| Shin, Katz, Wallhagen and Julian (2012)[26] | 115 subjects | Cognitive function (verbal learning, short delay, immediate delay, long delay recall, inhibition, switching condition) and covariates (sociodemographic and disease characteristics), blood test, depression | Proportion of persons who were classified as cognitively impaired on each test ranged from 8-29%. |
| More than 20% of subjects were found to be cognitively impaired in executive function (28% on the design fluency test and 21% on the trail making test).29% and 18% of subjects were cognitively impaired in visuospatiall learning and verbal learning/memory, respectively. | |||
| Shin, Julian and Katz (2013)[23] | 122 subjects | Cognitive function: verbal learning, short delay, immediate delay, and long delay recall, executive functioning, inhibition, switching conditions, and depression Physical function: functional limitation, functional disability | Nearly one-third of subjects were classified as cognitively impaired on 4 or more out of 16 subtests. About 20-30% of subjects were found to be cognitively impaired in executive function; specifically, 29% in the nonverbal fluency test and 21% in the sequencing and set-shifting test. 20% and 29% of subjects were impaired in verbal learning/memory and visuospatial learning/memory, respectively. |
| Melo and Silva (2012)[27] | FM=13 RA=13 SLE=11 (age range=30 to 80 years) | Memory, language, executive function | FM and SLE group showed significantly higher means of the neuropsychiatric symptoms of anxiety, irritability, and hallucinations than the RA group in the neuropsychiatric inventory. Young adults performed better in all tests as compared with the elderly. |
| Bilgici, Terzi, Guz and Kuro (2014)[15] | FM=16 RA=15 Health controls=15 | cognitive performance (global attention/working memory, language, visual and verbal memory, visuospatial process and executive function) | FM and RA patients performed poorly on most cognitive measurements compared with healthy controls and much similar to each other in performance except for the executive functions. No significant differences were found between FM and RA patients on the attention, memory, word fluency and visuospatial tasks. RA and FM patients performed poorly on verbal memory tests when compared with control groups. |
| Simos et al. (2016)[21] | 100 consecutive RA patients aged 28-67 years (90% woman) | Verbal short- term and working memory, verbal episodic memory, executive function (set-shifting and verbal fluency), visuomotor processing speed, Premorbid verbal capacity, premorbid nonverbal ability, nonverbal reasoning and problem-solving ability, pain severity, anxiety and depression | 20% of RA patients were cognitively impaired. Deficient performances were noted on tests of verbal short-term memory, immediate and short-delay verbal episodic recall, verbal working memory and phonemic fluency. Pain severity and anxiety and depression symptomatology jointly accounted for a small (not significant) proportions of variance in each of the cognitive indices measured in the study. |
| Gunnarsson, Grahn, Agerstrom (2016)[16] | 3 pain groups: acute pain (n=38), regularly recurrent pain (n=58), persistent pain (n=54) and healthy control group (n=51) | Sustained attention, cognitive control, psychomotor ability | Patients with persistent pain showed significantly worse on sustained attention and psychomotor ability compared with healthy controls. The acute pain group showed a significant decrement in psychomotor ability and regularly current pain group showed a decrement in sustained attention. |
MSK: Musculoskeletal, SLE: Systemic Lupus Erythematosus, FM: Fibromyalgia, RA: Rheumatoid Arthritis
Factors Affecting Cognitive Functioning in Rheumatoid Arthritis
Various factors are responsible for cognitive impairment in RA. Previous research has professed that chronic pain in arthritis disrupts attention and that this breakdown can lead to significant functional impairment and decreased quality of life. Prevalence studies indicate that as much as 44% of the population experience pain regularly and that in one-quarter of this group the pain is severe.[28,29] It is clear that many individuals who suffer from chronic pain experience attentional and other deficits.
Pain serves as a negative indication and warning of actual or potential harm.[13] Patients with chronic pain experience disruption of attention and memory.[2] Chronic pain affects the ability to work, sleep, and daily life activities and these changes generally worsen over time. Eccleston and Crombez documented that patients with chronic pain who reported higher levels of both pain and somatic awareness showed significant performance decrements on an attentionally demanding switching task compared with other chronic pain patients.[30] The mechanism underlying the interaction between pain and attention/cognitive function is not understood but likely involves some common cortical elements because pain involves similar attentional resources as other cognitive processes.
Brown et al. documented the negative impact of pain on measures of processing speed, reasoning, working memory, and verbal episodic memory, which were largely mediated by depressive symptomatology.[13] Disease symptoms such as chronic pain and psychological distress have been linked to cognitive impairment.[31] Thus, pain being central to arthritis plays a crucial role among arthritis patients during their cognitive performances.
Drugs, which are used for treating pain in RA has also their effect on cognition. Such as corticosteroid responsible for their effects on cognitive abilities, like memory. Wolkowitz et al. (1990) also found that even a single dose (1 mg dose of dexamethasone) or short - term use of corticosteroids (80 mg dose of prednisone for 5 days) was significantly related to memory problems.[32]
Shin et al. found possible predictors through their study that persons with lower education, lower income, oral glucocorticoid use, and increased cardiovascular disease (CVD) risk factors were more likely to be cognitively impaired. Demographic factors, medical comorbities, and steroid treatment were identified in studies as potential risk factors for cognitive dysfunction.
A study of Smedstad et al. RA symptoms were of great impact on psychiatric illnesses but mediated also between inflammation and stress.[33] Similarly, Covic et al. found that the degree of fatigue, as well as pain, can predict depression.[34] Contrary to this result, Huyser et al. could only confirm an interrelation between RA-fatigue and - pain and problematic moods.[35] Zautra et al. could detect that a past episode of depression could have the effect that pain at baseline was higher than in people without a depression history.[36] Further in this study, social distress had a strengthening effect on this relation. Other studies wherein psychosocial factors had an impact on the relation between RA symptomatic and mood problems were of Covic et al. who detected that helplessness not only affects depression but also increases pain perception[37] and mediate the relationship between depression and pain and Chaney et al. who found that internal attributions as helplessness enforce pain perception and depression.[38] Also, Frantom et al. could relate several psychosocial factors like stress and self-efficacy directly to pain.[39]
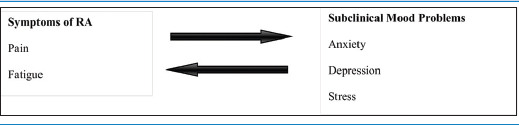
Anxiety and depression both are common constructs and are seen as distinctly different, anxiety being motivated by fear while depression by sadness.[40] Some studies show a higher prevalence rate of anxiety than depression in RA, whereas others do not.[41,42] According to the tripartite model[43], it is possible that anxiety manifests through physical arousal, increased sensitivity to pain, and interpretation of sensation as painful. However, depressive symptoms can be increase vulnerability to pain sensation at a time of stress.[44] So, Table 2 presents a conceptual model of relations between symptoms of RA and subclinical mood problems.
Table 2.
Conceptual model of relations between demanded variables
RA can be accompanied by cognitive dysfunction yet there is very limited literature on their dynamics. To assess cognitive impairment, deficits have been noted on short - term memory, visuospatial processing, episodic memory, and executive tasks.[9,45] Shin et al. also have worked on the same topic and revealed that the proportion of persons who were classified as cognitively impaired on each test ranged from 8-29%. More than 20% of subjects were found to be cognitively impaired in executive functions (28% on the design fluency test and 21% on the trail making test). A total of 29% and 18% of subjects were cognitively impaired in visuospatial learning and verbal learning/memory, respectively.[26] These deficits are because of lower levels of socioeconomic status (e.g., education and income), so it is well-known risk factors for poorer performance on cognitive tasks.[46,47]
It is estimated that the prevalence of depression in RA between 14% and 62% and the level of anxiety stands with a prevalence of between 21% and 70%. Brown et al. found that pain was positively related to depression and negatively related to cognitive functioning and that depression mediated the relationship between pain and cognitive functioning, suggesting that pain leads to depression, which leads to poorer cognitive functioning.[13] Studies have reported that executive and attentional functions are affected in chronic pain patients and it challenged attentional demands of chronic pain.[30,48,49] Yilmaz et al. concluded their findings as psychological stress and mood status are independent factors for relapse periods among RA and contribute to disease flare. RA patients also have increased functional disability, and decreased quality of life with higher disease activity.[50] Patients who suffer from excessive pain has also decreased health-relatedd quality of life. Brandstetter et al. also explained in their study that social support was found to be inversely associated with depressive symptoms in RA.[51]
Mechanism of Cognitive Decline in RA
There are number of factors for cognitive decline in RA and have some mechanisms involved in it. Studies show that the mechanism of systemic inflammation and CVD are linked with this type of impairment in the general population and have particular relevance for RA. In addition, the influence of glucocorticoid use and CVD may be interconnected, with some studies suggesting that glucocorticoid use may also confer a direct risk for CVD in RA.[52]
The mechanism for the deterioration of attention and executive function in chronic pain patients remains largely unclear. However, it has been suggested that patients have an attentional bias toward painful sensation, which may cause distraction from other stimuli. The experience of pain may reduce the capacity to attend to another stimulus because it captures attentional resources itself. It is also expected that increasing task demands on cognitive task performance decreases in chronic pain patients to a greater extent.[17] Earlier research found that people with RA had more trouble with tests of memory, speaking ability, and attention. More recent theories suggest that attention is a system of anomalous networks including alerting, orienting, and selection.[53]
So, through literature review, it has been clearly identified that RA patients get affected on various aspects of cognitive functioning and pain is a major factor involved in the decrement of performance. This work will provide a beneficial psychological outlook for the RA patients in a clinical setting.
Conclusions
Based on previous studies, it has been observed that the cognitive functioning of RA patients got affected by RA induced pain. There are multiple factors involved in cognitive impairment, which negatively affect mental health along with physical health. Psychological treatment using patient education and cognitive-behavioral therapy is effective for patients with chronic pain.[54] Multiple aspects of cognition covered by attention and executive function domains, which were reported in earlier findings. However, there are many parts of executive function that remains unclear such as working memory and set shifting.[55] Studies reported that pain, fatigue, poor sleep, and depression may be attentional distractions, and in turn affect cognitive processes and influence daily life activities.[56] People with more depression and greater pain respectively perform less well on tests of cognitive function and this cognitive function is subsequently impaired by pain and depression both.[57] Meade et al. reviewed and revealed that age, education, disease activity, and depression were associated with cognitive impairment.[58] Pain is known to affect cognition, particularly mental flexibility and attention. This is because of the attention-occupying nature of chronic pain and due to overlap between brain regions, which involve pain and cognition.[59]
Therefore, there is a need to examine the various other psychological factors that decreases the performances of patients with RA. To understand the effect of arthritis pain on attention and its other dimensions like alerting, orienting, and executive control should be also measured in RA and other arthritis patients. Further studies are also needed to confirm and explore the prevalence rates and examine the potential mechanism. Also, the management of psychological symptoms in such kind of patients should be multidisciplinary and should include psychoeducational programs.
Relevance of the study for the practice of family physicians
RA is the most common rheumatic disorder with persistent pain. A person suffering from RA experiences numerous somatic symptoms like deformation of joints, fever, fatigue, pain, sleep disturbances, and weight loss along with various psychological issues such as anxiety, depression, stress, feeling of loss, and other social difficulties, which might be related to changes in fulfilling their social roles and responsibilities.[60] From the earlier studies, it is assumed that pain is one of the most distressing symptoms of RA and it has a major role in influencing and exaggerating negative emotions like anxiety and depression. So, medication would be better work with a combination of yoga asanas, psychoeducational programs, and awareness programs.
Yoga might be considered as an ancillary treatment for RA. Yoga asanas have shown significant improvement in handgrip strength[61] and reduction in the symptoms of anxiety, depression[62], and oxidative stress[63] and also relieve tensions leading to better relaxation and concentration.[27,64] Systematic reviews have shown that yoga seems to be a safe and effective intervention for patients with arthritis.
The practice of yoga can lead to significant improvements in physical, mental as well as spiritual health. Medicine would work better in patients' bodies if their psychological problems would be identified and healed together with the treatment. Thus, these intervention programs were very beneficial in decreasing disability and enhancing functionality to improve cognition and mental health.
Financial support and sponsorship
Funding for this work was provided by University Grant Commission, National Eligibility Test- Junior Research Fellowship (NET-JRF) in science, humanities, and social science (UGC - Ref. No.: 308/NET-DEC. 2014).
Conflicts of interest
There are no conflicts of interest.
References
- 1.Joshi J, Kotwal P. Essential of Orthopedics and Applied Physiotherapy. 2nd ed. New Delhi: A division of Reed Elsevier India Private limited; 2011. pp. 352–3. [Google Scholar]
- 2.Małdyk P. Reumatoidalne zapalenie stawów. In: Sz. Gazzdzik T, editor. Ortopedia I Traumatologia. Warszawa, Poland: Wydawnictwo Lekarskie PZWL; 2008. pp. 510–7. [Google Scholar]
- 3.Hart RP, Martelli MF, Zasler ND. Chronic pain and neuropsychological functioning. Neuropsychol Rev. 2000;10:131–49. doi: 10.1023/a:1009020914358. [DOI] [PubMed] [Google Scholar]
- 4.Van Dijk GM, Veenhof C, Lankhorst GJ, Dekker J. Limitations in activities in patients with osteoarthritis of the hip or knee: The relationship with body functions, comorbidity and cognitive functioning. Disabil Rehabil. 2009;31:1685–91. doi: 10.1080/09638280902736809. [DOI] [PubMed] [Google Scholar]
- 5.Eccleston C. Chronic pain and distraction: An experimental investigation into the role of sustained and shifting attention in the processing of chronic persistent pain. Behav Res Ther. 1995;33:391–405. doi: 10.1016/0005-7967(94)00057-q. [DOI] [PubMed] [Google Scholar]
- 6.Weiner DK, Rudy TE, Morrow L, Slaboda J, Lieber S. The relationship between pain, neuropsychological performance, and physical function in community-dwelling older adults with chronic low back pain. Pain Med. 2006;7:60–70. doi: 10.1111/j.1526-4637.2006.00091.x. [DOI] [PubMed] [Google Scholar]
- 7.Oosterman JM, Derksen LC, Van Wijck AJ, Kessels RP, Veldhuijzen DS. Executive and attentional functions in chronic pain: Does performance decrease with increasing task load? Pain Res Manag. 2012;17:159–65. doi: 10.1155/2012/962786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lawlor PG. The panorama of opioid related cognitive dysfunction in patients with cancer: A critical literature appraisal. Cancer. 2002;94:1836–53. doi: 10.1002/cncr.10389. [DOI] [PubMed] [Google Scholar]
- 9.Bartolini M, Candela M, Brugni M, Catena L, Mari F, Pomponio G, et al. Are behaviour and motor performances of rheumatoid arthritis patients influenced by subclinical cognitive impairments? A clinical and neuroimaging study. Clin Exp Rheumatol. 2002;20:491–8. [PubMed] [Google Scholar]
- 10.Dick B, Eccleston C, Crombez G. Attentional functioning in fibromyalgia, rheumatoid arthritis, and musculoskeletal pain patients. Arthritis Rheum. 2002;47:639–44. doi: 10.1002/art.10800. [DOI] [PubMed] [Google Scholar]
- 11.Ziarko M, Siemiątkowska K, Sieński M, Samborski W, Samborska J, Mojs E. Mental health and rheumatoid arthritis: Toward understanding the emotional status of people with chronic disease. BioMed Res Int. 2019;2019:1473925. doi: 10.1155/2019/1473925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dick BD, Rashiq S. Disruption of attention and working memory traces in individuals with chronic pain. Anesth Analg. 2007;104:1223–9. doi: 10.1213/01.ane.0000263280.49786.f5. [DOI] [PubMed] [Google Scholar]
- 13.Brown SC, Glass JM, Park DC. The relationship of pain and depression to cognitive function in rheumatoid arthritis patients. Pain. 2002;96:279–84. doi: 10.1016/S0304-3959(01)00457-2. [DOI] [PubMed] [Google Scholar]
- 14.Abeare CA, Cohen JL, Axelrod BN, Leisen JC, Mosley-Williams A, Lumley MA. Pain, executive functioning, and affect in patients with rheumatoid arthritis. Clin J Pain. 2010;26:683–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Bilgici A, Terzi M, Güz H, Kuru Ö. Comparison of the cognitive performance between healthy controls, rheumatoid arthritis and fibromyalgia patients without depression. J Clin Anal Med. 2014;5:216–21. [Google Scholar]
- 16.Gunnarsson H, Grahn B, Agerström J. Impaired psychomotor ability and attention in patients with persistent pain: A cross-sectional comparative study. J Pain Res. 2016;9:825–35. doi: 10.2147/JPR.S114915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Babiloni C, Vecchio F, Bares M, Brazdil M, Nestrasil I, Eusebi F, et al. Functional coupling between anterior prefrontal cortex (BA10) and hand muscle contraction during intentional and imitative motor acts. Neuroimage. 2008;39:1314–23. doi: 10.1016/j.neuroimage.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 18.Chen TL, Babiloni C, Ferretti A, Perrucci MG, Romani GL, Rossini PM, et al. Human secondary somatosensory cortex is involved in the processing of somatosensory rare stimuli: An fMRI study. Neuroimage. 2008;40:1765–71. doi: 10.1016/j.neuroimage.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 19.Moore DJ, Keogh E, Eccleston C. The interruptive effect of pain on attention. Q J Exp Psychol A. 2012;65:565–86. doi: 10.1080/17470218.2011.626865. [DOI] [PubMed] [Google Scholar]
- 20.Moore DJ, Keogh E, Eccleston C. The effect of threat on attentional interruption by pain. Pain. 2013;154:82–8. doi: 10.1016/j.pain.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 21.Simos P, Ktistaki G, Dimitraki G, Papastefanakis E, Kougkas N, Fanouriakis A, et al. Cognitive deficits early in the course of rheumatoid arthritis. J Clin Exp Neuropsychol. 2016;38:820–9. doi: 10.1080/13803395.2016.1167173. [DOI] [PubMed] [Google Scholar]
- 22.Greiner PA, Snowdon DA, Schmitt FA. The loss of independence in activities of daily living: The role of low normal cognitive function in elderly nuns. Am J Public Health. 1996;86:62–6. doi: 10.2105/ajph.86.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shin SY, Julian L, Katz P. The relationship between cognitive function and physical function in rheumatoid arthritis. J Rheumatol. 2013;40:236–43. doi: 10.3899/jrheum.120871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dunlop DD, Semanik P, Song J, Manheim LM, Shih V, Chang RW. Risk factors for functional decline in older adults with arthritis. Arthritis Rheum. 2005;52:1274–82. doi: 10.1002/art.20968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shifren K, Park DC, Bennett JM, Morrell RW. Do cognitive processes predict mental health in individuals with rheumatoid arthritis.? J Behav Med. 1999;22:529–47. doi: 10.1023/a:1018782211847. [DOI] [PubMed] [Google Scholar]
- 26.Shin SY, Katz P, Wallhagen M, Julian L. Cognitive impairment in persons with rheumatoid arthritis. Arthritis Care Res. 2012;64:1144–50. doi: 10.1002/acr.21683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Melo LF, Da-Silva SL. Neuropsychological assessment of cognitive disorders in patients with fibromyalgia, rheumatoid arthritis, and systemic lupus erythematosus. Rev Bras Reumatol. 2012;52:181–8. [PubMed] [Google Scholar]
- 28.Birse TM, Lander J. Prevalence of chronic pain. Can J Public Health. 1998;89:129–31. doi: 10.1007/BF03404405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith BH, Elliott AM, Chambers WA, Smith WC, Hannaford PC, Penny K. The impact of chronic pain in the community. Fam Pract. 2001;18:292–9. doi: 10.1093/fampra/18.3.292. [DOI] [PubMed] [Google Scholar]
- 30.Eccleston C, Crombez G. Pain demands attention: A cognitive–affective model of the interruptive function of pain. Psychol Bull. 1999;125:356–66. doi: 10.1037/0033-2909.125.3.356. [DOI] [PubMed] [Google Scholar]
- 31.Hart RP, Wade JB, Martelli MF. Cognitive impairment in patients with chronic pain: The significance of stress. Curr Pain Headache Rep. 2003;7:116–26. doi: 10.1007/s11916-003-0021-5. [DOI] [PubMed] [Google Scholar]
- 32.Wolkowitz OM, Reus VI, Weingartner H, Thompson K, Breier A, Doran A, et al. Cognitive effects of corticosteroids. Am J Psychiatry. 1990;147:1297–303. doi: 10.1176/ajp.147.10.1297. [DOI] [PubMed] [Google Scholar]
- 33.Smedstad LM, Mourn T, Vaglum P, Kvien TK. The impact of early rheumatoid arthritis on psychological distress. Scand J Rheumatol. 1996;25:377–82. doi: 10.3109/03009749609065649. [DOI] [PubMed] [Google Scholar]
- 34.Covic T, Tyson G, Spencer D, Howe G. Depression in rheumatoid arthritis patients: Demographic, clinical, and psychological predictors. J Psychosom Res. 2006;60:469–76. doi: 10.1016/j.jpsychores.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 35.Huyser BA, Parker JC, Thoreson R, Smarr KL, Johnson JC, Hoffman R. Predictors of subjective fatigue among individuals with rheumatoid arthritis. Arthritis Rheum. 1998;41:2230–7. doi: 10.1002/1529-0131(199812)41:12<2230::AID-ART19>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 36.Zautra AJ, Parrish BP, Van Puymbroeck CM, Tennen H, Davis MC, Reich JW, et al. Depression history, stress, and pain in rheumatoid arthritis patients. J Behav Med. 2007;30:187–97. doi: 10.1007/s10865-007-9097-4. [DOI] [PubMed] [Google Scholar]
- 37.Covic T, Adamson B, Spencer D, Howe G. A biopsychosocial model of pain and depression in rheumatoid arthritis: A 12-month longitudinal study. Rheumatology. 2003;42:1287–94. doi: 10.1093/rheumatology/keg369. [DOI] [PubMed] [Google Scholar]
- 38.Chaney JM, Mullins LL, Wagner JL, Hommel KA, Page MC, Doppler MJ. A longitudinal examination of causal attributions and depression symptomatology in rheumatoid arthritis. Rehabil Psychol. 2004;49:126. [Google Scholar]
- 39.Frantom CG, Parker JC, Smarr KL, Slaughter JR, Hewett JE, Hewett JE, et al. Relationship of psychiatric history to pain reports in rheumatoid arthritis. Int J Psychiatry Med. 2006;36:53–67. doi: 10.2190/2QGP-WWGJ-67PX-LF0W. [DOI] [PubMed] [Google Scholar]
- 40.Watson D, Clark LA, Weber K, Assenheimer JS, Strauss ME, McCormick RA. Testing a tripartite model: II. Exploring the symptom structure of anxiety and depression in student, adult, and patient samples. J Abnorm Psychol. 1995;104:15–25. doi: 10.1037//0021-843x.104.1.15. [DOI] [PubMed] [Google Scholar]
- 41.El-Miedany YM, El Rasheed AH. Is anxiety a more common disorder than depression in rheumatoid arthritis? Joint Bone Spine. 2002;69:300–6. doi: 10.1016/s1297-319x(02)00368-8. [DOI] [PubMed] [Google Scholar]
- 42.Isik A, Koca SS, Ozturk A, Mermi O. Anxiety and depression in patients with rheumatoid arthritis. Clin Rheumatol. 2007;26:872–8. doi: 10.1007/s10067-006-0407-y. [DOI] [PubMed] [Google Scholar]
- 43.Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. J Abnorm Psychol. 1991;100:316–36. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- 44.Smith BW, Zautra AJ. The effects of anxiety and depression on weekly pain in women with arthritis. Pain. 2008;138:354–61. doi: 10.1016/j.pain.2008.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Appenzeller S, Bertolo MB, Costallat LT. Cognitive impairment in rheumatoid arthritis. Methods Find Exp Clin Pharmacol. 2004;26:339–44. doi: 10.1358/mf.2004.26.5.831324. [DOI] [PubMed] [Google Scholar]
- 46.Lynch JW, Kaplan GA, Shema SJ. Cumulative impact of sustained economic hardship on physical, cognitive, psychological, and social functioning. N Engl J Med. 1997;337:1889–95. doi: 10.1056/NEJM199712253372606. [DOI] [PubMed] [Google Scholar]
- 47.Cagney KA, Lauderdale DS. Education, wealth, and cognitive function in later life. J Gerontol B Psychol Sci Soc Sci. 2002;57:163–72. doi: 10.1093/geronb/57.2.p163. [DOI] [PubMed] [Google Scholar]
- 48.Grisart JM, Plaghki LH. Impaired selective attention in chronic pain patients. Eur J Pain. 1999;3:325–33. doi: 10.1053/eujp.1999.0138. [DOI] [PubMed] [Google Scholar]
- 49.Moriarty O, McGuire BE, Finn DP. The effect of pain on cognitive function: A review of clinical and preclinical research. Prog Neurobiol. 2011;93:385–404. doi: 10.1016/j.pneurobio.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 50.Yılmaz V, Umay E, Gündoǧdu İ, Karaahmet ZÖ, Öztürk AE. Rheumatoid Arthritis: Are psychological factors effective in disease flare.? Eur J Rheumatol. 2017;4:127. doi: 10.5152/eurjrheum.2017.16100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brandstetter S, Riedelbeck G, Steinmann M, Ehrenstein B, Loss J, Apfelbacher C. Pain, social support and depressive symptoms in patients with rheumatoid arthritis: Testing the stress-buffering hypothesis. Rheumatol Int. 2017;37:931–6. doi: 10.1007/s00296-017-3651-3. [DOI] [PubMed] [Google Scholar]
- 52.Mazzantini M, Talarico R, Doveri M, Consensi A, Cazzato M, Bazzichi L, et al. Bombardieri S. Incident comorbidity among patients with rheumatoid arthritis treated or not with low-dose glucocorticoids: A retrospective study. J Rheumatol. 2010;37:2232–6. doi: 10.3899/jrheum.100461. [DOI] [PubMed] [Google Scholar]
- 53.Fan J, Mc Candliss BD, Sommer T, Raz A, Posner MI. Testing the efficiency and independence of attentional networks. J Cogn Neurosci. 2002;14:340–7. doi: 10.1162/089892902317361886. [DOI] [PubMed] [Google Scholar]
- 54.Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain. 1999;80:1–3. doi: 10.1016/s0304-3959(98)00255-3. [DOI] [PubMed] [Google Scholar]
- 55.Lezak MD, Howieson DB, Loring DW, Fischer JS. Neuropsychological Assessment. USA: Oxford University Press; 2004. [Google Scholar]
- 56.Akdoǧan S, Ayhan FF, Yıldırım Ş, Borman P. Impact of fatigue on cognitive functioning among premenopausal women with fibromyalgia syndrome and rheumatoid arthritis: The controlled study. J Musculoskelet Pain. 2013;21:135–46. [Google Scholar]
- 57.James RJ, Ferguson E. The dynamic relationship between pain, depression and cognitive function in a sample of newly diagnosed arthritic adults: A cross-lagged panel model. Psychol Med. 2019;7:1–9. doi: 10.1017/S0033291719001673. [DOI] [PubMed] [Google Scholar]
- 58.Meade T, Manolios N, Cumming SR, Conaghan PG, Katz P. Cognitive impairment in rheumatoid arthritis: A systematic review. Arthritis Care Res. 2018;70:39–52. doi: 10.1002/acr.23243. [DOI] [PubMed] [Google Scholar]
- 59.Attal N, Masselin-Dubois A, Martinez V, Jayr C, Albi A, Fermanian J, et al. Does cognitive functioning predict chronic pain? Results from a prospective surgical cohort. Brain. 2014;137:904–17. doi: 10.1093/brain/awt354. [DOI] [PubMed] [Google Scholar]
- 60.Ziarko M. Zmaganie Sie Ze Stresem Choroby Przewleklej. Poznan, Poland: Wydawnictwo Naukowe Wydzialu Nauk Spolecznych UAM; 2014. [Google Scholar]
- 61.Dash M, Telles S. Improvement in hand grip strength in normal volunteers and rheumatoid arthritis patients following yoga training. Indian J Physiol Pharmacol. 2001;45:355–60. [PubMed] [Google Scholar]
- 62.Woolery A, Myers H, Sternlieb B, Zeltzer L. A yoga intervention for young adults with elevated symptoms of depression. Altern Ther Health Med. 2004;10:60–3. [PubMed] [Google Scholar]
- 63.Yadav RK, Ray RB, Vempati R, Bijlani RL. Short communication effect of a comprehensive effect of a yoga-based lifestyle modification program on lipid peroxidation. Indian J Physiol Pharmacol. 2005;49:358–62. [PubMed] [Google Scholar]
- 64.Kulmatycki L. Yoga Nidra Relaxation Art Warsaw: Publishing House Book and Knowledge. 2004:90. [Google Scholar]


