Data science and artificial intelligence (AI) have the potential to transform the delivery of health care. Health care as a sector, with all of the longitudinal data it holds on patients across their lifetimes, is positioned to take advantage of what data science and AI have to offer. The current COVID-19 pandemic has shown the benefits of sharing data globally to permit a data-driven response through rapid data collection, analysis, modelling, and timely reporting.
Despite its obvious advantages, data sharing is a controversial subject, with researchers and members of the public justifiably concerned about how and why health data are shared. The most common concern is privacy; even when data are (pseudo-)anonymised, there remains a risk that a malicious hacker could, using only a few datapoints, re-identify individuals. For many, it is often unclear whether the risks of data sharing outweigh the benefits.
A series of surveys over recent years indicate that the public holds a range of views about data sharing.1, 2 Over the past few years, there have been several important data breaches and cyberattacks.3 This has resulted in patients and the public questioning the safety of their data, including the prospect or risk of their health data being shared with unauthorised third parties.4
We surveyed people across the UK and the USA to examine public attitude towards data sharing, data access, and the use of AI in health care. These two countries were chosen as comparators as both are high-income countries that have had substantial national investments in health information technology (IT) with established track records of using data to support health-care planning, delivery, and research. The UK and USA, however, have sharply contrasting models of health-care delivery, making it interesting to observe if these differences affect public attitudes.
Data from 3194 respondents (aged >18 years) across the UK (n=2080) and the USA (n=1114) were used from an online 2018 YouGov survey that we developed (appendix p 1). YouGov is a widely used research platform that develops nationally representative surveys through active sampling, ensuring a nationally representative pool; the final responses are statistically weighted (by the UK Office for National Statistics and the US Census Bureau) to the national profile of each country for adults aged 18 years or older.
Although most respondents were aware of electronic health records (EHRs), their use was not widespread in either country, especially in the UK (14·3% vs 44·5% in the USA). Women and older patients were slightly more likely to report access to their EHRs, suggesting EHR access might be associated with relative health-service use (figure ).
Figure.
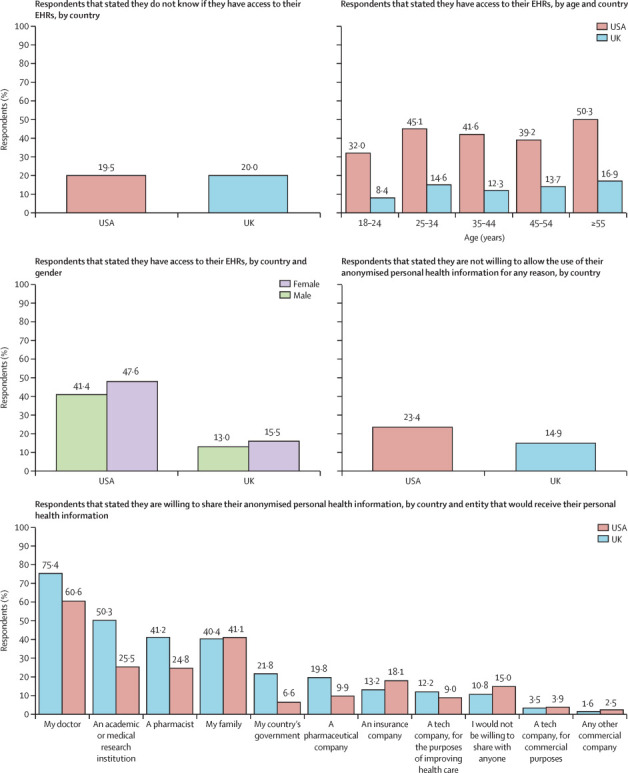
Citizens' awareness of access to their EHRs and willingness to share their anonymised personal health information
95% CIs for all estimates are provided in the appendix (pp 4–5). EHR=electronic health record.
Willingness to share anonymised personal health information varied across receiving bodies (figure). The more commercial the purpose of the receiving institution (eg, for an insurance or tech company), the less often respondents were willing to share their anonymised personal health information in both the UK and the USA. Older respondents (≥35 years) in both countries were generally less likely to trust any organisation with their anonymised personal health information than younger respondents (<35 years).
Despite low numbers of access, many UK (59·0%, 95% CI 56·9–61·1) and US (70·1%, 67·4–72·8) respondents regarded access to their medical records as useful (appendix pp 2, 4).
In both countries, more respondents were happy to receive advice from their doctor or nurse without assistance from AI than with it (58·2% [95% CI 56·1–60·3] vs 54·8% [52·7–56·9] in the UK and 51·8% [48·8–51·2] vs 38·2% [35·4–64·6] in the USA; appendix pp 3, 5). By contrast with US respondents, a small majority of UK respondents were happy to receive care from AI software as long as it was there to support a doctor or nurse (appendix pp 3, 5). Younger respondents (≤44 years) were more willing to receive advice from independent AI than older respondents (>44 years) in both the USA and the UK (appendix pp 3, 5).
The ambition both in the USA and the UK is to enable patient access to EHRs; however, our results suggest access and use is not widespread. This might partly be explained by relative health-care consumption rather than a lack of information or support. Yet, there are also many barriers to accessing health records, such as poor usability and interoperability, language barriers, overall mistrust in the health system, or concerns about insurance eligibility. A previous study in the USA found that ethnic minority and lower income patients adopt EHRs less often than white and higher income patients,5 suggesting further research is needed to tackle inequity in digital health. Patient involvement in the design of digital applications might be imperative to appropriately respond to rapidly evolving expectations of digital services—especially for those who have grown up with technology.6 Young adults now extensively use digital resources to access health information, digital health tools, and peer support7 and this presents an important opportunity for health-care provision amid the COVID-19 crisis.
A key finding from this work was the importance of trust. Although the majority of respondents in both countries were willing to share their data with their doctor, it is worrying that in the USA more than a third are not. The fact that distrust in the USA, which has a largely privatised system, was higher than in the UK, which has a socialised single-payer system, might indicate that patients are concerned that data might not be protected from commercial end-use.8 This is supported by our findings comparing willingness to share across public (eg, government, research institution) and commercial end-users (eg, insurance and tech companies). When institutions are likely to use data for commercial purposes, respondents were less willing to share their data, especially in the case of tech organisations. Our findings indicate a sharp shift in public opinion compared with a Wellcome Trust survey in 2016 in which half of UK respondents were willing to share data with commercial organisations.9 This suggests that the growing commodification of patient data, and recent tech scandals such as Cambridge Analytica in 2018, have increased public awareness of the risks and consequences of sharing data with commercial and tech industries.10 This pattern is also reflected in a 2018 survey done by RockHealth in the USA, showing a substantial decline in the number of individuals willing to share their health data with tech companies.1
The data analysed here were obtained through a YouGov survey, which results in some limitations. No ethnic demographic data were obtained, the survey was conducted in English, and all participants needed to have IT access—all factors that highlight potential biases of the survey data.
Despite the benefits of big data and technology in health care, our findings suggest that the rapid development of novel technologies has been received with concern. Growing commodification of patient data has increased awareness of the risks involved in data sharing. There is a need for public standards that secure regulation and transparency of data use and sharing and support patient understanding of how data are used and for what purposes.4
The implications of our findings amid the COVID-19 pandemic remain unclear. While the urgency of data science and AI is becoming increasingly evident as the COVID-19 outbreak grows globally, the crisis also imposes new risks to public privacy and data security. Further work needs to be done to understand how this catastrophic public health emergency will affect public views on data sharing.
Acknowledgments
We declare no competing interests. This work was supported by the World Innovation Summit for Health (WISH) which is hosted by the Qatar Foundation. AD is a National Institute for Health Research (NIHR) Senior Investigator. The views expressed in this Comment are those of the author(s) and not necessarily those of the NIHR, or the Department of Health and Social Care. Infrastructure support for this research was provided by the NIHR Imperial Biomedical Research Centre. All data are anonymised and are in the public domain through YouGov as part of a wider survey (UK and USA), and are also available by contacting the corresponding author.
Supplementary Material
References
- 1.Day S, Zweig M, Evans B, McGuinness D. Beyond wellness for the healthy: digital health consumer adoption 2018. Rock Health. https://rockhealth.com/reports/beyond-wellness-for-the-healthy-digital-health-consumer-adoption-2018
- 2.Curved Thinking Understanding public expectations of the use of health and care data. July, 2019. https://understandingpatientdata.org.uk/sites/default/files/2019-07/Understanding%20public%20expectations%20of%20the%20use%20of%20health%20and%20care%20data.pdf
- 3.Ghafur S, Fontana G, Martin G, Grass E, Goodman J, Darzi A. Imperial College London; London: 2019. Improving cyber security in the NHS. [Google Scholar]
- 4.Ghafur S, Fontana G, Halligan J, O'Shaughnessy J, Darzi A. Imperial College London; London: 2020. NHS data: maximising its impact on the health and wealth of the United Kingdom. [Google Scholar]
- 5.Yamin CK, Emani S, Williams DH. The digital divide in adoption and use of a personal health record. Arch Intern Med. 2011;171:568–574. doi: 10.1001/archinternmed.2011.34. [DOI] [PubMed] [Google Scholar]
- 6.Pew Research Center Internet & technology. Mobile fact sheet. June 12, 2019. https://www.pewresearch.org/internet/fact-sheet/mobile/
- 7.Rideout V, Fox S. Hopelab & Well Being Trust; San Francisco, CA: 2018. Digital health practices, social media use, and mental well-being among teens and young adults in the US. [Google Scholar]
- 8.Ham C. Money can't buy you satisfaction. BMJ. 2005;330:597–599. doi: 10.1136/bmj.330.7491.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wellcome Trust Public attitudes to commercial access to health data. 2016 [cited 2019 Nov 11] https://wellcome.ac.uk/sites/default/files/public-attitudes-to-commercial-access-to-health-data-summary-wellcome-mar16.pdf
- 10.Gostin LO, Halabi SF, Wilson K. Health data and privacy in the digital era. JAMA. 2018;320:233–234. doi: 10.1001/jama.2018.8374. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


