Highlights
-
•
The first case report of a 27 years follow up congenital insensitivity of pain in Indonesia.
-
•
Unrecognizing of the clinical pictures in the past, misleads to a late diagnosis and management.
-
•
Both patients suffered from debilitating consequence of amputation and death of the male patient.
-
•
Open reduction and internal fixations of metaphyseal fractures may eventually lead to non-union.
-
•
Diaphyseal fractures more likely result in bony unions with casting immobilization.
Keywords: Congenital insensitivity of pain, Anhidrosis, Hyperpyrexia, Case report
Abstract
Introduction
Congenital insensitivity to pain with anhidrosis (CIPA; OMIM 256,800) is a rare autosomal recessive disease. Although the clinical symptoms are known, the consensus of CIPA treatment has not been recognized. This is the first report of CIPA in Indonesia, a case of two siblings, male and female, whom we followed-up for 27 years.
Presentation of case
After a series of multiple fractures from an early age, both patients who lived wheelchair-bound with their parents had been suffering from a recurrent debilitating infection on their lower extremities. The male patient eventually died from sepsis due to bronchopneumonia, years after the nonunion of both legs. The female patient underwent double above knee amputation.
Discussion
Observation showed that fracture in joint and metaphysis treated with open reduction ultimately end in disastrous outcomes like infection and non-union. On the contrary, the diaphyseal fracture has a better expectation to unite with casting immobilization.
Conclusion
Unrecognizing of the clinical pictures of CIPA and minimal literature references in the past, misleads to late diagnosis and management. Genetic evaluation should be done for infants with unknown causes of high fever, anhidrosis combined with insensitivity to pain. Surgical intervention of metaphyseal fractures should be avoided due to tendencies of implants loosening, metal failures, recurrent infections followed with non-union, and instability.
1. Introduction
Congenital insensitivity to pain with anhidrosis (CIPA; OMIM 256,800), is a rare autosomal recessive disease characterized by recurrent episodes of unexplained fever, anhidrosis, lack of response to noxious stimuli, recurrent bone fractures, infection, and mental retardation.
Besides the apparent "brittle bone", the children could not tolerate warm weather, did not perspire at all, had episodes of extremely high body temperatures, and had insensitivity of the pain as well as habitually bit their fingers, lips, and tongue (Fig. 1, Fig. 2). Physical examinations revealed small stature, chronic eczematous skin, non-healing ulcers, and a slow learner.
Fig. 1.
Hand shows ulcer and fingertip loss of the male patient age 28.
Fig. 2.
Scars and irreguler tounge tip of the female patient age 15.
The presence of multiple long bone fractures resemble osteogenesis imperfecta together with the initial unawareness of CIPA, led to chronic joint destruction with debilitating consequences as non-union and limb amputation.
With the rare incidence of 1:25.000 [1], the consensus of CIPA treatment has not been recognized.
This is the first report of CIPA in Indonesia, a case of two siblings whom we followed-up for 27 years. The orthopedic problem wast first presented in 1992. The diagnosis of CIPA was confirmed by genomic DNA investigation 21 years later in the year 2013. This case report has been reported in line with the SCARE criteria [5].
2. Case report
Their parents were asymptomatic and non-consanguineous, had three children with one asymptomatic normal appearance eldest son. They have no history of developmental delay during the newborn period and no other family history with similar problems.
2.1. The first case is a boy, the second child in the family, born in 1987
A 5 years old boy was brought to an orthopedic clinic in 1992 with fever, painless swelling and surgical wound discharge in the right elbow after underwent K-wires fixation due to supracondylar humerus by a senior orthopedic surgeon in another hospital one week before. The boy had implants removal, debridement, and casting all done by the first author, a senior orthopedic surgeon. Subsequently, there was recurrent infected wound so the bone failed to unite resulting in pseudoarthrosis of the distal humerus. History of previous recurrent episodes of high fever mimicking sepsis with no perspiration since newborn was reported.
We recorded serial fractures of this patient: right tibia at 8 years old, right patella at 9, right femur at 11, left tibia, and left femur at 15 years old. All were treated conservatively with plaster casts. This condition was associated with a periodontal problem that caused spontaneous tooth loss from the age of 7 until a complete loss at the age of 10. The patient had slower learning abilities and never attended formal education.
Recurrent joint swelling was existed until the age of 26 years and and shows improvement when treated by antibiotics, a low dose of corticosteroid, and necessary aspiration. The support of calcium and vitamin D3 was continued. At the latest X-rays, in 2013 by the age of 26, showed complete lysis of both epiphyses of the right femoral and tibial side with malunion of the left diaphysis of femur and tibia as sequelae of previous fractures (Fig. 3). The patient lived a relatively normal life with the full assistance of the daily activities of his parents.
Fig. 3.
Lower extremeties of the male patient A, B) X-ray at age 26 showing non-union of supracondylar right femur and lysis of tibial plateau with varus union of the left femur and tibial diaphysis. C) clinical appearance at age 29 showed leg length discrepancies of 7 cm and varus left leg.
The patient refused the suggestion of above-knee amputation for the flail right knee. He was unable to perform normal gait and wheelchair-bound. At the age of 30 in 2017, the patient suffered from persistent high fever and soon after died with high suspicion of sepsis due to bronchopneumonia at home.
2.2. The second case is a girl, the third child in the family, born in 2000
In 2007, fifteen years after the boy first appeared in our clinic, his 7 years old sister came with complaints of continuous painless swelling, surgical wound discharge and wire exposure (Figs. 4a-c) after underwent K-wire fixation and splinting for dislocated ankle fracture two months prior in another hospital in another hospital by a senior orthopedic surgeon.. We performed a thorough debridement, wires removal, and splinting of the heavily damaged right ankle.
Fig. 4.
Right ankle of the female patient after ankle fracture dislocation: A) X-ray at age 7 two months after kirschner wire fixation B) X-ray showed right ankle destruction 5 years after surgery C) clinical appearance at age 15 with flail ankle.
The painless sensation was first noticed when she was 5 years old after a minor trauma resulted in right ankle contusion. She also had a history of recurrent unknown high fever and no perspiration since her newborn period, like her brother had, but in a lower degree of severity.
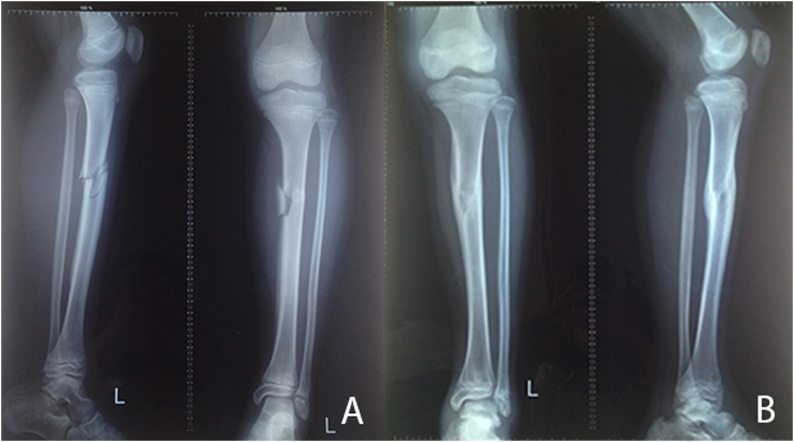
Afterward, we recorded multiple fractures and dislocations of this patient: a right hip dislocation at age 7, a minimal epiphysiolysis fracture of the left distal radius and left diaphyseal tibial fracture (Figs. 5a and b) at the age of 12, and a left knee dislocation at the age of 13, all caused by minor trauma. Conservative treatment with cast splinting, joint aspiration, antibiotic, and low dose corticosteroids, along with supportive calcium, vitamin D3, and high intake of protein were applied. Patients feel comfortable with splinting although the painless sensation allowed her to still perform a movement regardless of the cast.
Fig. 5.
Lower left leg of the female patient A) X-ray showed tibial shaft fracture at age 12 and B) bone union after 6 months of casting.
Follow-up radiologic examination by the age of 12 showed total damaged and flail right ankle (Fig. 4d) surprisingly associated with normal bony healing of the left diaphyseal tibia (Fig. 5c).
These clinical signs led to differential diagnosis of CIPA in 2010. The genomic DNA approach was suggested by the pediatrician in our team to confirm the type of CIPA. Dry blood spots of the whole family were sent to Taipei City Hospital in Taiwan when the girl was 13 years old.
The diagnosis of CIPA was definitively established after DNA mapping: The primer sequence for exons 1–17 was obtained. Two mutations were detected by comparing published DNA and genomic sequences for the normal TRKA gene. There were mutations in exon 1: c.253C>A (R85S) from the mother and in exon 13:c.2074C>T (R692C) from the father. These mutations were found in both patients, as they inherited them from each parent. The eldest son inherited only one mutation from his father. (Fig. 6).
Fig. 6.
All mutations in the NTRK1 gene in patients with CIPA. Red letters indicate the novel mutations found in this study.
At the age of 16, two months after the death of her brother, she underwent a right below-knee amputation due to continuous infection of the flail ankle. Unfortunately, her left knee further deteriorated due to overused pressure from crawling. The X-ray showed chondrolysis and instability. In 2018, a "cold" abscess from her left knee urged us to perform above-knee leg amputation.
The girl is now 19 years old and lived with her parents. She is wheelchair-bound, has a subaverage intellectual ability, and needs full assistance in daily living activities. Her amputee stump suffered from recurrent swelling every time it is overused because of crawling.
3. Discussion
CIPA is a rare autosomal recessive disease. Dearborn described first in 1932 as "Congenital pure analgesia". They are collectively termed "hereditary sensory and autonomic neuropathies" [2].
Although it is a neurological condition, many of the manifestations are orthopedic. Symptoms started as children became active in early childhood. The lack of pain leads to many injuries as the child cannot control the strength of the movement. The children in our case series presented with fractures, joint dislocations, infection, and Charcot arthropathies.
Cases with CIPA have never been reported before in our country. We got the absolute diagnosis of CIPA 21 years later after the first patient was first brought to our clinic. At first, the patients were suspected to have osteogenesis imperfecta-like brittle bones with delayed healing. Unrecognizing of the clinical pictures and minimal literature references in the past, misleads to late diagnosis and management.
In this case, we observed that the joint and metaphyseal fracture treated with surgical intervention would finally end in disastrous outcomes like infections and non-union. On the contrary, we found out that the diaphyseal injury has a better expectation to unite with conservative treatment of cast immobilization.
It is unlikely that patients with CIPA have an intrinsic abnormality of the bone [3]. Rather the failure of joint healing is mostly because of the response from the stubborn movement of the joint caused by the lack of pain. The risk of infection and non-union are reduced with non-surgical treatment.
It should also be noted that high fever in children could lead to febrile seizure and promote the long term risk of epilepsy, psychiatric disorder, and mortality [4].
4. Conclusion
Genetic evaluation for CIPA should be considered as soon as possible for an infant with an unknown cause of high fever and anhidrosis and combined with insensitivity to pain without other significant clinical and laboratory changes. Early diagnosis may save the life of neonates and infants from the debilitating complications and protect them from the fractures due to exposure to various self-harming activities.
Open reduction and internal fixations for the metaphyseal fractures localized adjacent to joints may lead to implants loosening, metal failures and recurrent infections followed with non-union, instability, and severe leg-length discrepancy and the subsequent high cost of care. In contrast, diaphyseal fractures more likely result in bony unions following conservative casting immobilization.
Finally, without consensus treatment protocols available for this condition, early diagnosis and wise fracture management are crucial to limit complications leading to permanent disabilities.
Declaration of Competing Interest
The authors have no conflict of interest to declare.
Funding
There is no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Approval to publish case report is waived by the institution.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Franky Hartono: the manuscript design and writing, the literature review and data collection.
Daniel P Marpaung: the literature review.
Karina E Besinga: the literature review
Conny Tanjung: the literature review
Tessi Ananditya: the manuscript design and writing and data collection.
Andrew Budiartha Budisantoso: the manuscript writing
Registration of research studies
This is not a first in man studies.
-
1.
Name of the registry:-
-
2.
Unique identifying number or registration ID:-
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked):-
Guarantor
Franky Hartono.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Contributor Information
Franky Hartono, Email: hartono_franky@yahoo.com.
Conny Tanjung, Email: mfconnytanjung@yahoo.com.
Karina E Besinga, Email: kembesinga@gmail.com.
Daniel Marpaung, Email: dpm2211@gmail.com.
Tessi Ananditya, Email: t.ananditya@gmail.com.
Andrew Budiartha Budisantoso, Email: andrew.b_12@hotmail.com.
References
- 1.Sasnur A.H., Sasnur P.A., Ghaus-Ul R.S. Congenital insensitivity and anhidrosis. Indian J. Orthop. 2011;45:269–271. doi: 10.4103/0019-5413.80047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sezg B., Bolgül N., Hamamci N. Congenital insensitivity to pain: a case report with dental implications. HK J. Paediatr. 2010;15:234. [Google Scholar]
- 3.Krettek C., Gluer S., Therman H. Non-union of the ulna in a ten-month-old child who had Type-IV hereditary sensory neuropathy. A case report. J. Bone Joint Surg. Am. 1997;79(August (8)):1232–1234. doi: 10.2106/00004623-199708000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Dreier J.W., Li J., Sun Y., Christensen J. Evaluation of long-term risk of epilepsy, psychiatric disorders, and mortality among children with recurrent febrile seizures: a national cohort study in Denmark. JAMA Pediatr. 2019;173(12):1164–1170. doi: 10.1001/jamapediatrics.2019.3343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]