Abstract
Background
The aim of this study was to provide a scoping review of the impact of pharmacist-led interventions on medication adherence and clinical outcomes in patients with hypertension and hyperlipidemia.
Methods
A scoping review was conducted using pre-defined search terms in three scientific databases, including Google Scholar, ScienceDirect, and PubMed. A multi-stage screening process that considered relevancy, publication year (2009–2019), English language, and article type (original research) was followed. Review articles, meta-analysis studies, and conference proceedings were excluded. Data charting was done in an iterative process using a study-specific extraction form.
Results
Of the initially identified 681 studies, 17 studies with 136,026 patients were included in the review. Of these, 16 were randomized controlled trials, while the remaining study was a retrospective cohort study. The majority of pharmacist-led interventions were face-to-face counseling sessions (n=8), followed by remote- or telephone-based interventions (n=5) and multi-faceted interventions (n=4). The majority of the studies (n=7) used self-reported adherence measures and pharmacy refill records (n=8) to measure the rate of adherence to prescribed medications. Eleven of the included studies reported a statistically significant (P<0.05) impact on medication adherence. Overall, twelve studies assessed the effect of the interventions on the clinical outcome measures; of these, only four studies were associated with significant impact.
Conclusion
Pharmacist-led interventions were associated with improved patients’ adherence to their medications but were less likely to be consistently associated with the attainment of clinical outcomes. Face-to-face counseling was the most commonly used intervention; while, the multi-faceted interventions were more likely to be effective in improving the overall outcome measures. The rigorous design of targeted interventions with more frequent follow-ups, careful consideration of the involved medications, and patients’ characteristics could increase the effectiveness of these interventions.
Keywords: adherence, hyperlipidemia, antihypertensive, pharmacists, intervention, pharmacy services
Introduction
Cardiovascular diseases (CVD) are considered a leading cause of death worldwide. It is estimated that in 2030, almost 23.6 million people will die from CVD.1 The risk factors of developing CVD can be further classified into modifiable and non-modifiable. Examples of modifiable risk factors include tobacco smoking, raise blood lipid levels, hypertension, physical inactivity, unhealthy diet, and obesity. A family history of CVD, age, gender, and socioeconomic status is considered as non-modifiable risk factors.1 Although evidence recommends guidelines-based pharmacotherapies for reducing the risk of CVD, adjunctive lifestyle modification is equally important in reducing the risk of repeated cardiovascular events.2
Typical examples of important cardiovascular medications include statins, antihypertensives, and antiplatelet drugs.3,4 Adherence to medication regimen; the extent to which people take medications as prescribed by their healthcare providers; is essential to attaining successful clinical outcomes.5 Adherence is used interchangeably with compliance; however, the motivational level seems to be varied between them, where adherence denotes better patients’ engagement with the instructions of healthcare providers.6 Unfortunately, nonadherence to cardiovascular medications constitutes a major problem that leads to treatment failure and poor clinical outcomes.7
Pharmacists are considered the most accessible healthcare team members, among other healthcare professionals.8 The role of pharmacists had extended beyond the traditional role of dispensing medications to provision of patient counseling on lifestyle modifications, medication therapy management, disease state management, and ensuring optimal medication adherence.9 According to the 2019 policy statement by the International Pharmaceutical Federation regarding the role of pharmacists in noncommunicable diseases, pharmacists contribute effectively to the appropriate management of CVD through provision of pharmaceutical care, medication reviews, and promoting medication adherence.10 However, little is known about the type and effectiveness of pharmacists’ intervention in improving medicine adherence by patients with hypertension and hyperlipidemia. This study was, therefore, conducted to characterize the types of pharmacists’ interventions based on their level of impact on medicine adherence by patients. Furthermore, it aimed to provide insights into the correlation between pharmacist interventions, adherence levels, and achievement of the desired clinical outcomes.
Methods
The general methodological framework for conducting scoping studies that was proposed by H. Arksey & L. O’Malley and enhanced further by Levac et al was followed as the basis for conducting this review.11,12
Identifying the Research Questions
This review focussed on studying the pharmacists-led interventions in promoting medication adherence among patients with CVD, particularly hypertension and hyperlipidemia. The following research questions guided the procedure of including studies, extract and summarize the data type, assessment, and impact of the designed interventions:
What are the characteristics of pharmacists-led interventions used in the included studies?
What methods were used to measure the impact of interventions on medication adherence and clinical outcomes among patients with hypertension and hyperlipidemia?
What was the overall effect of these interventions on medication adherence and clinical outcomes?
Identifying Relevant Studies
We included original research articles published between 2009 and 2019 that reported the impact of pharmacist interventions on medication adherence. The searches were limited to the last ten years to provide a review of the most recently published evidence. Review articles, meta-analysis studies, book chapters, and conference proceedings were excluded. Google Scholar, PubMed, and ScienceDirect databases were searched to retrieve studies of interest using relevant pre-defined terms. The search terms included (“adherence”), (“compliance”), (“cardiovascular disease preventive medication”), (“hyperlipidemia”), (“anti-hypertensive”), (“pharmacist role”), (“pharmacist intervention”), and (“pharmacy services”).
Study Selection
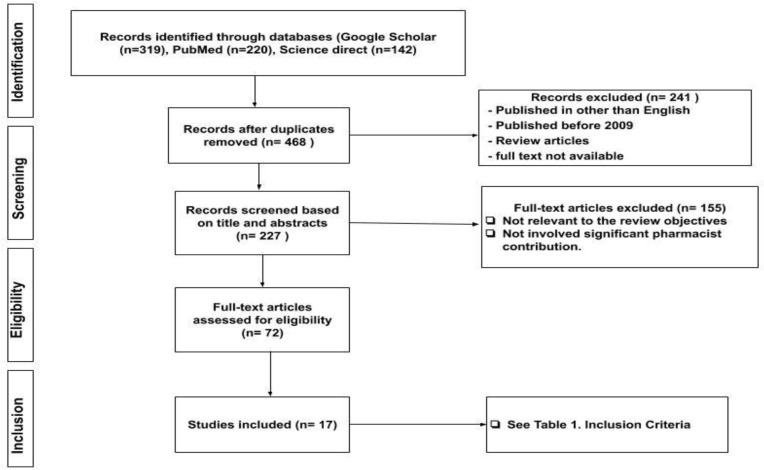
At this stage, two reviewers (ME, NR) independently identified the included studies according to the pre-defined inclusion criteria presented in Table 1. As per the followed methodological framework, meetings were conducted three times: at the start, middle, and end of the selection stage. Furthermore, two independent reviewers met at regular intervals during the study selection stage to resolve any conflicts or discrepancies between them. Finally, full-text articles published in the last ten years that met the inclusion criteria were considered for inclusion (see Figure 1).
Table 1.
Inclusion Criteria
| Category | Inclusion Criteria |
|---|---|
| Language of publication | English |
| Year of publication | 2009–2019 |
| Publication type | Original research articles |
| Outcomes measures | Medication Adherence and Clinical outcomes either as primary or secondary outcomes |
| Methodology | Studies assessing pharmacist’s interventions on outcome measures for hypertension and/or hyperlipidemia were eligible for inclusion |
| Pharmacist role | Pharmacists have to perform a leading role in designing and/or executing the interventions. |
| Patients | Adult patients aged 18 years old or above who were receiving cardiovascular medications. |
Figure 1.
PRISMA flowchart for selecting the studies according to the systematic scoping review methodology.
Charting the Data
Data charting was done in an iterative process using a study-specific extraction form that was aligned with the research question. The included variables were study author, publication year, study design, study population, type of intervention, adherence measurement, and key findings. Two independent researchers completed the data extraction of the first five studies. A meeting was then conducted to discuss the extent of consistency of data extraction against the study-specific extraction form.
Collating, Summarizing, and Reporting the Results
A descriptive analysis of the extracted data was conducted. Reporting of the key findings was done consistent with the study outcome measures. For hyperlipidemia, the clinical outcome measured was lipid profile where total cholesterol and LDL-cholesterol were taken into account. A summary of the methods of the main types of pharmacists’ interventions, methods of measuring medication adherence, and their impact on patients’ adherence was provided. Pharmacists’ interventions were characterized and tabulated into two categories based on the level of impact on medicine adherence. Studies reporting statistically significant improvement in medicine adherence (P< 0.05) and studies with non-significant or no improvement in adherence (P> 0.05). The included variables included study design, study population, type of intervention, outcome measures, method of adherence measurement, and key results.
Results
Characteristics of the Included Studies
Of the initially identified 681 studies, 17 studies with 136,026 patients were included in the review. Of the 17 included studies, 16 were Randomized Controlled Trials (RCTs), while the remaining study was a retrospective cohort study. Eight studies reported the impact of pharmacist interventions on adherence to antihypertensive medications, while five studies focused on adherence to medications for high cholesterol. The remaining four studies assessed the adherence to both hypertension and hyperlipidemia medications. Regarding the location of the included studies, ten studies were conducted in the U.S.; three studies were in the Netherlands and one study for each of Denmark, India, Portugal, Spain, Australia, Hong Kong, and the United Kingdom.
Measurement of the Impact of Pharmacists’ Interventions
All the included studies reported measures for medication adherence. Fourteen studies reported the adherence measures as primary outcome meanwhile only three studies reported the adherence as a secondary outcome measure.13–15 A total of five studies did not report the assessment of clinical outcomes and reported only the adherence measures.16–20 Twelve studies included the assessment of clinical outcomes either as secondary (N=8) or primary outcome measures (N=4). Almost half of the assessment of the clinical outcomes were reported for hypertension (N=6); meanwhile, three studies reported clinical outcomes for hyperlipidemia and the remaining three studies considered clinical outcomes for both conditions simultaneously. Of these, only four studies showed a significant impact of the interventions on the clinical outcomes of hypertension (N=3) and hyperlipidemia (N=1). Four different methods of measuring medication adherence were identified across the included studies. These included Morisky Medication Adherence Scale (MMAS) and its related scales (n=7), pharmacy refill records adherence (n=8), prescription abandonment (n=1), and manual pill count (n=1). If there was more than one method used to assess medication adherence in a single study, we considered the method identified as a primary outcome measure as the basis of classifying the impact of the intervention. Table 2 describes the frequency of adherence measurement methods and their relevant characteristics.
Table 2.
Medicine Adherence Measurement Methods and Their Characteristics Reported in the Included Studies
| Adherence Measurement Method | Self-Reported Adherence (MMAS and Its Related Scales) N=7 | Refill Record-Based Adherence N=8 | Prescription Abandonment N=1 | Manual Pill Count N=1 |
|---|---|---|---|---|
| Main Characteristics |
|
-The proportion of days covered (PDC)
|
|
|
Abbreviations: MMAS, Morisky Medication Adherence Scale; PDC, proportions of days covered; MPR, medication possession ratio.
Types of Pharmacists’ Interventions
The classification of the implemented interventions was referring to the nature of executing the main intervention sessions, not merely on the name of the used tools. For example, studies with counseling sessions as the main interventions that have used telephone reminders in the follow-up period were classified under the “counseling” class of interventions.21 Overall, conventional face-to-face counseling was the most frequently used intervention in the included studies (n=8), where patients were provided counseling on disease management, adverse effects, strategies to improve medicine adherence, and advice on lifestyle modifications. All studies conducted follow-up counseling sessions; however, the structure, frequency, and duration of the follow-up sessions were variable across the studies (see Tables 3 and 4). Telephone-based or remotely conducted interventions were used in five studies. As reported in the face-to-face counseling, there was considerable variability in the delivery of these interventions. For example, one study implemented behavioral interviewing as a part of a multicomponent remote intervention.22 Another example was the use of successive series of telephone calls in specified intervals.14 Furthermore, one study tested the impact of electronic reminders alone or with counseling in a comparative context.19 Additionally, four studies used multi-faceted interventions that consisted of well-structured multicomponent interventions including pre-assessment of individual’s adherence level, counseling sessions, medication review, collaboration with physicians, and telephone calls.20,23-25 In almost all multi-faceted interventions, the pharmacists were leading the interventions in the multidisciplinary collaborative care models that involved physicians or general practitioners to help in determining patients’ eligibility, patients’ referral, and as feedback receiver of the outcomes of the intervention to be integrated into the subsequent patient care process.
Table 3.
Studies Reporting Significant Improvement (P<0.05) in Medicine Adherence (N=11)
| Author, Year, Country | Study Design and Population | Pharmacist Intervention | Comparator, Follow-Up and Outcome Measures | Key Findings |
|---|---|---|---|---|
| Ho et al, 201423 (USA) | RCT involved 241 patients admitted with ACS and then discharged. | Multi-faceted intervention comprising medication reconciliation, patient education, collaborative care, and voice messaging. | Comparator: usual care. Follow-up: 12 months. Outcomes: Primary (refill adherence >0.8, % of adherent patients), Secondary (% of patients achieved BP and LDL-C targets). |
The intervention increased adherence to statin (93.2 vs. 71.3%) (p=<0.001) and ACEI/ARB regimens (93.1% vs. 81.7%), (p=0.03) significantly. There was no significant changes in percentage of target BP or LDL-C levels attainments. |
| Lyons et al 201627 (UK) | RCT involved 677 T2DM patients prescribed with LLT. | Two telephone-based Intervention, with medicine chart reminder. | Comparator: standard care. Follow-up: 6 months. Outcomes: Primary (self-reported nonadherence), Secondary (LDL-C levels). |
The intervention group has less percentage of nonadherence compared to control group (10.6% vs. 19.6%, p=0.010). There was no associated significant difference in the clinical outcomes. |
| Taitel et al 201216 (USA) | Retrospective cohort study included 2056 patients who were newly initiated on statin medications. | Two Face-to-face counselling session including a motivational interview | Comparator: control group. Follow-up: 12 months. Outcomes: medication adherence (MPR ≥80%). |
The statin adherence has improved in the intervention group compared to control group is (61.8% vs. 56.9%, p<0.01). There was no assessment for clinical outcomes. |
| Choudhry et al, 201822 (USA) | A Pragmatic cluster RCT involved 4078 patients’ non-adherent to their hypertension and hyperlipidemia medications. | Telephone-based behavioral interviewing, text messaging, and progress reports. | Comparator: usual care. Follow-up: 12 months. Outcomes: Primary (medication adherence, % of covered days), Secondary (LDL-C & SBP). |
The intervention showed a significant improvement of 4.7% (95% CI, 3.0–6.4%) in medication adherence. There were no significant changes in the overall assessment of clinical outcomes. |
| Hedegaard et al, 201521 (Denmark) | RCT included 532 patients prescribed with AHT and LLT. | Tailored medication review, patient interview, followed by telephone reminders. | Comparator: control group. Follow-up: 12 months. Outcomes: Primary (medication adherence, MPR ≥80%), Secondary (BP & hospital admission). |
Nonadherence was higher in the control group (30.2% vs. 20.3%, p=0.01) as compared to the intervention group. There were no significant differences in the evaluated clinical outcomes. |
| Ramanath et al, 201226 (India) | RCT involved 52 patients on AHT. | Counseling sessions using patient information leaflets and telephone reminders. | Comparator: control group. Follow-up: 1 month (twice). Outcomes: Primary (self-reported adherence, MMAS & MARS), Secondary (BP control). |
The overall adherence increased significantly in the intervention group compared to the control group. There was no significant impact on BP control. |
| Morgadoet al 201113 (Portugal) | RCT included 197 patients receiving AHT. | Counseling and educational sessions. | Comparator: usual care. Follow-up: 9 months. Outcomes: Primary (BP control), Secondary (self-reported medication adherence. |
There was a statistically significant improvement in blood pressure control (66% vs. 41.7%, p = 0.0008) and medication adherence (74.5% vs. 57.6%, p = 0.012) between intervention and control groups. |
| Benbrahim et al 201317 (Spain) | RCT included 176 patients on AHT. | Face-to-face (written and oral) tailored educational intervention. | Comparator: usual care. Follow-up: 6 months. Outcomes: medication adherence (pills count). |
The adherence was increased significantly to 95.5% (baseline 86%) in the intervention group compared to 86.5% (baseline 85.4%) in the control group (p=0.011). There was no assessment for clinical outcomes. |
| Fischer et al, 201418 (USA) | RCT included 124 131 patients with newly prescribed cardiovascular medications. | Live telephone calls with tailored educational messages | Comparator: control group. Follow-up: 30 days following index date. Outcomes: Primary medication adherence (prescription abandonment). |
The live pharmacy-based interventions decreased primary medication adherence by 4.8% (P< 0.0001) compared to control group. There was no assessment for clinical outcomes. |
| Stewart et al, 201424 (Australia) | Cluster RCT involved 395 patients who were taking at least one AHT. | Multi-faceted intervention consisted of motivational interviews, refill reminders, training on BP monitoring and medication reviews. | Comparator: control group. Follow-up: 6 months. Outcomes: Primary (self-reported adherence), Secondary (BP control) |
No significant difference in % of adherent patients between control (57.2% vs. 63.6%) and intervention (60% vs. 73.5%) groups at baseline and 6 months, respectively. Non-adherence decreased from 61.8% at baseline to 39.2% at 6 months in the intervention group (P = 0.007). There was a significant SBP reduction in the intervention group (p=0.01). |
| Svarstad et al, 201325 (USA) | Cluster RCT included 567 patients taking one or more AHT. | Team Education and Adherence Monitoring program involved tailored counselling and education using take-home toolkit, leaflets and medication box. | Comparator: control (only patient information). Follow-up: 6 and 12 months. Outcomes: adherence (refill ≥80%) and BP control. |
Participants in the intervention group had better adherence (60% vs 34%, p<0.001) and BP control (50% vs. 36%, p=0.01) compared to the control group. |
Abbreviations: ACS, acute coronary syndrome; RCT, randomized controlled trial; LLT, lipid-lowering therapy; SBP, systolic blood pressure; T2DM, type 2 diabetes mellitus; AHT, antihypertensive; LDL-C, low-density lipoprotein cholesterol.
Table 4.
Studies with Non-Significant or No Improvement in Medicine Adherence (N=6)
| Author, Year, Country | Study Design and Population | Pharmacist Intervention | Comparator, Follow-Up and Outcome Measures | Key Findings |
|---|---|---|---|---|
| Eussen et al, 201029 (Netherlands) | A multicentre, open-label RCT included 899 patients on statin medications. | Five structured counselling sessions over a year. | Comparator: usual care. Follow-up: 6 and 12 months. Outcomes: Primary (adherence, 1-year discontinuation rate), Secondary (6 months discontinuation rate, ≥90% MPR and LDL-C levels). |
The intervention showed a lower discontinuation rate of that was significant only at 6 months but not significant at 1 year. Median MPR was not significantly different between groups (99.5% vs. 99.2%, p=0.14). Adherent patients were more likely to achieve target LDL-c levels at 6 months (74% vs. 50%, p=0.01). |
| Kooy et al 201319 (Netherlands) | RCT included 299 elderly patients (65 years or above) who had started statins at least one year. | Electronic reminder device (ERD) with or without counselling sessions. | Comparator: control group. Follow-up: 360 days. Outcomes: adherence (refill ≥80%). |
Overall, refill adherence was not significantly improved with counselling with ERD (69.25, p=0.55), ERD only (72.4%, p=0.18) compared to control group (64.8%). There was no assessment for clinical outcomes. |
| Ma et al, 201014 (USA) | RCT involved 689 patients with underlying CHD who had an LLT prescription. | Five Telephone counselling calls. | Comparator: usual care. Follow-up: 12 months. Outcomes: Primary (% patients achieved LDL-C levels), Secondary (adherence, continuous multiple-interval (CMA) from pharmacy records). |
The intervention did not show significant improvement in statin adherence (0.88 vs. 0.90, p=0.51). It had no significant impact on clinical outcomes (65% vs. 60%, p=0.29). |
| Gums et al, 201520 (USA) | Cluster RCT included 593 patients who had at least one AHT. | Physician-pharmacist collaboration management (PPCM) | Comparator: usual care. Follow-up: 9 months. Outcomes: Primary (Adherence, self-reported questionnaire), Secondary (medication changes). |
There was no significant difference in the measures of medication adherence between the groups. Patients in the intervention group experienced higher medication changes compared to control group (4.9 vs. 1.1, p=0.003). There was no assessment for clinical outcomes. |
| Wong et al, 201315 (Hong Kong) | RCT included 274 patients taking at least one long-term AHT and having suboptimal compliance | Counselling sessions with structured patient education and provision of pillboxes and medication knives. | Comparator: usual care (brief drug advice). Follow-up: 3 and 6 months. Outcomes: Primary (BP control), Secondary (adherence, self-reported) |
Overall, both percentage of patients with optimal adherence and BP control were improved throughout study period. However, there were no significant differences between the groups in both outcome measures. |
| Van der Laan et al, 201828 (Netherlands) | RCT included 170 patients who were on AHT. | Two face-to-face consultation (3 months apart). | Comparator: usual care. Follow-up: 9 months. Outcomes: Primary (self-reported adherence), Secondary (BP control). |
There were no significant differences between intervention and control groups in both outcome measures. |
Impact of Pharmacists’ Interventions on Medicines Adherence and Clinical Outcomes
Eleven studies reported a significant impact of the pharmacist interventions on medication adherence by patients (see Table 3). Of these, five studies included patients with hypertension,13,17,24-26 two studies included patients with hyperlipidemia,16,27 and four studies reported impact among patients receiving medications for both conditions.18,21-23 On the other hand, six studies reported insignificant impact of the interventions on the outcome measures with respect to the comparable groups (see Table 4). Of these, three studies were conducted among patients with hypertension;15,20,28 meanwhile, the remaining three studies were carried out among patients receiving medications for hyperlipidemia.14,19,29 Almost half of the interventions associated with improvement in adherence involved direct pharmacist-patient counseling sessions. A multi-faceted pharmacist intervention was employed in three studies, while three studies relied on involving remote reminders or telephone-designed interventions. The non-significant improvement in medicine adherence was reported in two telephone-based interventions, three face-to-face counseling sessions, and one multi-faceted intervention. In addition, of the twelve studies that assessed the impact of the interventions on the clinical outcome measures, only four studies had been associated with significant impact for the pharmacists’ interventions on the overall assessment of clinical outcome measures. Of these, three studies were involving antihypertensive medications and only one study involved lipid-lowering therapy.
Discussion
To the authors’ knowledge, this is the first study that has characterized the types of pharmacists’ interventions based on their level of impact on both medicine adherence and clinical outcomes. Previous research highlighted that pharmacist-led interventions were associated with improvement in the rational use of hyperlipidemia medications.30 Approximately 65% of the studies included in this review reported a significant impact of the pharmacist interventions on medication adherence by patients. Three studies were assessing medication adherence as secondary outcome measures. Of these, two studies did not show a significant change in the adherence following the pharmacists’ intervention. The overall success rate of pharmacists’ interventions aimed at improving medicine adherence was reported as 75% for multi-faceted interventions, 62.5% for face-to-face counseling, and 60% for telephone-based interventions. These findings suggest that the direct involvement of the pharmacists in multi-faceted care models that had a multidisciplinary collaborative component showed the highest potential to improve medication adherence.
Concerning the medications involved in the interventions, the findings showed that almost half of the total studies were dedicated to improving the adherence of the antihypertensive medications, while five studies were for lipid-lowering therapy. In the remaining four studies, both medications were included. It is important to highlight that almost all studies that assessed both medications were associated with significant improvement in the adherence outcome measures.18,21-23 Furthermore, five out of eight studies that only targeted improvement in the adherence outcome measures for antihypertensive drugs reported significant results.13,17,24-26 Finally, only two out of five studies aimed to enhance the adherence to lipid-lowering therapy reported a positive impact of the implemented pharmacist interventions.16,27 In a study that reported the overall good impact of the intervention on medication adherence, it was underpinned that the adherence measures for antihypertensive were more positively affected by the intervention compared to lipid-lowering therapy.18 Moreover, among studies that failed to show the overall impact of pharmacist intervention on the adherence measures, it was highlighted that women, particularly, were able to attain a significant impact on adherence to lipid-lowering therapy for secondary prevention compared to the control group.19 The findings suggest the potential importance of the customization of the implemented interventions to consider the medications and the patients’ demographics carefully.
Twelve studies assessed the impact of pharmacists’ interventions on clinical outcomes including hypertension and hyperlipidemia. Of these, four studies were designed primarily to assess the impact of pharmacists’ interventions on the clinical outcomes of blood pressure control or achievement of target LDL-C levels.13–15,25 However, only three studies reported significant improvement in clinical outcomes following pharmacists’ interventions with two of them being multi-faceted. It is also important to highlight that studies that assessed both outcome measures for both antihypertensive and lipid-lowering therapy were less likely to have a significant impact on the clinical outcomes despite their significant impact on medicine adherence.
Majority of the included studies used pharmacy-refill records either as medication possession ratio (MPR) or the proportion of days covered (PDC) to measure the adherence level of patients. The MPR calculates medicine adherence as the days’ sum supply of the medications during the observation period divided by the total days during that period.16 The PDC, on the other hand, takes into account the covered days, which is calculated as the proportion of days covered of the 360 days following the index date divided by the total days’ supply by the number of the study period.19 Both methods are calculative measures not subjected to a bias imposed by self-reporting. However, the interpretation of adherence differed within studies with some studies regarding adherence as MPR ≥ 90%, while some regarded adherence as MPR ≥ 80%. The other most popular method of measuring adherence was the Morisky Medication Adherence Scale (MMAS) that has also been a basis for developing derived scales.13,20 This adherence measurement method has widely been used in measuring adherence to antihypertensive medications due to its simplicity, ease of administration, and low cost.15 However, this method has limitations, including an overestimation of the adherence level induced by the self-reporting. Consequently, the improvement in adherence to the self-reporting component might be less valid compared to other quantitative methods.
Pharmacist-led interventions were associated with improved patients’ adherence to their medications but were less likely to be consistently associated with the attainment of clinical outcomes. The findings of this study seem to be influenced by the variations in the type and design of the intervention, control group, decision on primary and secondary outcomes, and tools for assessing adherence. Most of the studies measured clinical outcomes as secondary outcomes following the assessment of medication adherence as primary outcomes. Measurement of clinical outcomes was missing in some studies that made it challenging to investigate the association between adherence and clinical outcomes.17
The findings of this suggested that interventions with frequent follow-ups,13 the use of a variety of verbal and written materials,17 and interventions implemented with several subsequent components were more likely to achieve positive intervention outcomes.24 Future studies involving pharmacists’ interventions should involve frequent contact with patients as better-structured multicomponent interventions are more likely to achieve optimal adherence levels. Furthermore, future studies should focus on delivering interventions to patients who are more likely to benefit from the intervention. Thus, it is essential to recruit patients who are experiencing adherence issues at baseline to make efficient use of the available human and financial resources.25 Also, it would be critical to investigate the individual patients’ level characteristics such as gender that have the potential to affect the overall outcomes of the implemented interventions.19
This study has some limitations. Quality assessment of the included studies was not conducted. The searches were confined to three databases that may have limited the opportunity to identify further eligible studies published in other relevant databases. Furthermore, since our work was limited to the inclusion of published literature only, publication bias is probable. However, it can be argued that a significant number of the included studies were not necessarily reporting positive findings. Nevertheless, the review employed a comprehensive, transparent, and rigorous method to identify studies.
Conclusion
Pharmacist-led interventions were associated with improved patients’ adherence to their medications but were less likely to be consistently associated with the attainment of clinical outcomes. Face-to-face counseling provided by pharmacists was found to be the most widely used; meanwhile, the multi-faceted interventions were more likely to be effective in improving the overall outcome measures. The rigorous design of targeted interventions with more frequent follow-ups, careful consideration of the involved medications, and patients’ characteristics could increase the effectiveness of these interventions.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organization. Cardiovascular Diseases (CVDs) Fact Sheet. Key Facts; 2017. Available from: https://www.who.int/cardiovascular_diseases/about_cvd/en/. Accessed July 12, 2020. doi: 10.1016/B978-1-4377-0660-4.00020-X [DOI] [Google Scholar]
- 2.Ministry of Health Malaysia. Primary & Secondary Prevention of Cardiovascular Disease 2017; 2017. [Google Scholar]
- 3.Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2016;37(29):2315–2381. doi: 10.1093/eurheartj/ehw106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Prevention of cardiovascular disease guidelines for assessment and management of cardiovascular risk WHO library cataloguing-in-publication data. 2007. Available from: www.inis.ie. Accessed February26, 2020.
- 5.Robinson JH, Callister LC, Berry JA, Dearing KA. Patient-centered care and adherence: definitions and applications to improve outcomes. J Am Acad Nurse Pract. 2008;20(12):600–607. doi: 10.1111/j.1745-7599.2008.00360.x [DOI] [PubMed] [Google Scholar]
- 6.Glynn L, Fahey T. Cardiovascular medication: improving adherence. Clin Evid. 2011;4(220). Available from: https://www.researchgate.net/publication/51040145. Accessed February 26, 2020. [PMC free article] [PubMed] [Google Scholar]
- 7.Kolandaivelu K, Leiden BB, O’Gara PT, Bhatt DL. Nonadherence to cardiovascular medications. Eur Heart J. 2014;35(46):3267–3276. doi: 10.1093/eurheartj/ehu364 [DOI] [PubMed] [Google Scholar]
- 8.Elnaem MH, Jamshed SQ, Elkalmi RM. The future of pharmaceutical care in Malaysia: pharmacy students ’ perspectives. Pharm Educ. 2017;17(1):215–222. [Google Scholar]
- 9.Albrecht S. The pharmacist’s role in medication adherence. US Pharm. 2011;36(5):45–48. [Google Scholar]
- 10.FIP - International Pharmaceutical Federation. Fip Statement of Policy - the Role of Pharmacist in Non- Communicable Diseases; 2019. [Google Scholar]
- 11.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol Theory Pract. 2005;8(1):19–32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 12.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(69):1–9. doi: 10.1017/cbo9780511814563.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morgado M, Rolo S, Castelo-Branco M. Pharmacist intervention program to enhance hypertension control: a randomised controlled trial. Int J Clin Pharm. 2011;33(1):132–140. doi: 10.1007/s11096-010-9474-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ma Y, Ockene IS, Rosal MC, Merriam PA, Ockene JK, Gandhi PJ. Randomized trial of a pharmacist-delivered intervention for improving lipid-lowering medication adherence among patients with coronary heart disease. Cholesterol. 2010;2010:1–11. doi: 10.1155/2010/383281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong MCS, Liu KQL, Wang HHX, et al. Effectiveness of a pharmacist-led drug counseling on enhancing antihypertensive adherence and blood pressure control: a randomized controlled trial. J Clin Pharmacol. 2013;53(7):753–761. doi: 10.1002/jcph.101 [DOI] [PubMed] [Google Scholar]
- 16.Taitel M, Jiang J, Rudkin K, Ewing S, Duncan I. The impact of pharmacist face-to-face counseling to improve medication adherence among patients initiating statin therapy. Patient Prefer Adherence. 2012;6:323–329. doi: 10.2147/PPA.S29353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fikri-Benbrahim N, Faus MJ, Martínez-Martínez F, Sabater-Hernández D. Impact of a community pharmacists’ hypertension-care service on medication adherence. The AFenPA study. Res Soc Adm Pharm. 2013;9(6):797–805. doi: 10.1016/j.sapharm.2012.12.006 [DOI] [PubMed] [Google Scholar]
- 18.Fischer MA, Choudhry NK, Bykov K, et al. Pharmacy-based interventions to reduce primary medication nonadherence to cardiovascular medications. Med Care. 2014;52(12):1050–1054. doi: 10.1097/mlr.0000000000000247 [DOI] [PubMed] [Google Scholar]
- 19.Kooy MJ, Van Wijk BLG, Heerdink ER, De Boer A, Bouvy ML. Does the use of an electronic reminder device with or without counseling improve adherence to lipid-lowering treatment? The results of a randomized controlled trial. Front Pharmacol. 2013;4(MAY(May)):1–11. doi: 10.3389/fphar.2013.00069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gums TH, Uribe L, Vander Weg MW, James P, Coffey C, Carter BL. Pharmacist intervention for blood pressure control: medication intensification and adherence. J Am Soc Hypertens. 2015;9(7):569–578. doi: 10.1016/j.jash.2015.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hedegaard U, Kjeldsen LJ, Pottegård A, et al. Improving medication adherence in patients with hypertension: a randomized trial. Am J Med. 2015;128(12):1351–1361. doi: 10.1016/j.amjmed.2015.08.011 [DOI] [PubMed] [Google Scholar]
- 22.Choudhry NK, Isaac T, Lauffenburger JC, et al. Effect of a remotely delivered tailored multicomponent approach to enhance medication taking for patients with hyperlipidemia, hypertension, and diabetes the STIC2IT cluster randomized clinical trial. JAMA Intern Med. 2018;178(9):1190–1198. doi: 10.1001/jamainternmed.2018.3189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ho PM, Lambert-kerzner A, Carey EP, et al. Multi-faceted intervention to improve medication adherence and secondary prevention measures after acute coronary syndrome hospital discharge a randomized clinical trial. JAMA. 2014;80220(2):186–193. doi: 10.1001/jamainternmed.2013.12944 [DOI] [PubMed] [Google Scholar]
- 24.Stewart K, George J, Mc Namara KP, et al. A multi-faceted pharmacist intervention to improve antihypertensive adherence: a cluster-randomized, controlled trial (HAPPy trial). J Clin Pharm Ther. 2014;39(5):527–534. doi: 10.1111/jcpt.12185 [DOI] [PubMed] [Google Scholar]
- 25.Svarstad BL, Kotchen JM, Shireman TI, et al. Improving refill adherence and hypertension control in black patients: wisconsin TEAM trial. J Am Pharm Assoc. 2013;53(5):520–529. doi: 10.1331/JAPhA.2013.12246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ramanath KV, Balaji DBSS, Nagakishore CH, Mahesh Kumar S, Bhanuprakash M. A study on impact of clinical pharmacist interventions on medication adherence and quality of life in rural hypertensive patients. J Young Pharm. 2012;4(2):95–100. doi: 10.4103/0975-1483.96623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lyons I, Barber N, Raynor DK, Wei L. The Medicines Advice Service Evaluation (MASE): a randomised controlled trial of a pharmacist-led telephone based intervention designed to improve medication adherence. BMJ Qual Saf. 2016;25(10):759–769. doi: 10.1136/bmjqs-2015-004670 [DOI] [PubMed] [Google Scholar]
- 28.van der Laan DM, Elders PJM, Boons CCLM, Nijpels G, van Dijk L, Hugtenburg JG. Effectiveness of a patient-tailored, pharmacist-led intervention program to enhance adherence to antihypertensive medication: the CATI study. Front Pharmacol. 2018;9. doi: 10.3389/fphar.2018.01057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eussen SRBM, Van Der Elst ME, Klungel OH, et al. A pharmaceutical care program to improve adherence to statin therapy: a randomized controlled trial. Ann Pharmacother. 2010;44(12):1905–1913. doi: 10.1345/aph.1P281 [DOI] [PubMed] [Google Scholar]
- 30.Elnaem MH, Nik Mohamed MH, Huri HZ. Pharmacist-led academic detailing improves statin therapy prescribing for Malaysian patients with type 2 diabetes: quasi- experimental design. PLoS One. 2019;14(9):e0220458. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- World Health Organization. Prevention of cardiovascular disease guidelines for assessment and management of cardiovascular risk WHO library cataloguing-in-publication data. 2007. Available from: www.inis.ie. Accessed February26, 2020.