Abstract
Background
During curfew, patients are self-isolated at home and worried. Patient–doctor interactions may be disrupted and therefore need to be replaced by alternative effective communication methods.
Purpose
To describe the preferences of cancer patients with respect to communication methods and the use of patient-accessible electronic health records (PAEHRs). To record the impact on cancer patients during the COVID-19 pandemic and the knowledge and attitude of the patients towards it.
Patients and Methods
We created a self-administered electronic survey that was piloted and evaluated for its clinical relevance. Using convenient sampling methods, we surveyed the cancer patients in our Oncology Center.
Results
We received 385 responses between April 15 and April 30, 2020. The preferred method for communication was a phone call with a 92% response rate followed by the electronic patient portal, mobile application, telemedicine and text message in 75%, 76%, 73%, and 72%, respectively. The majority (97%) preferred the use of PAEHRs for appointments, 95% for drug delivery and to view laboratory tests, and 92% in requesting medical reports. In our survey, 22% of patients with cancer reported that their medical cancer care had not been affected by COVID-19. They reported that trusted sources of information during COVID-19 included the Ministry of Health with 98% and doctors with 94%. Sixty-one percent know that they are more susceptible to COVID-19 infection and 91% of respondents supported the notion of digital transformation in the caring of cancer patients.
Conclusion
Our study revealed a general acceptance of patients to telecommunication as substitute to in-person interaction with their physicians. Interaction between cancer patients and health care providers should not be disrupted but should be augmented with more effective platforms to improve health care outcomes.
Keywords: patient preference, e-health, patient online access, health disparities, cancer, COVID-19
Introduction
Cancer patients encounter challenges and dilemmas in the face of the COVID-19 pandemic, they need direct communication with oncologists to ensure they follow precautionary measures and to pass on the correct information regarding practice modifications in light of the restrictions related to the COVID-19 pandemic.1,2
During curfew, telemedicine “virtual” or “e-health” allowed patients and doctors to discuss the patients care plan utilizing communication technologies. Mclean et al showed no differences in outcomes between tele-health-care and standard practices.3 Barsom et al looked into videoconference consultation among patients with colon cancer and reported that, based on patients' preferences, videoconference is equal to face-to-face consultation in terms of patient satisfaction and perceived quality of care.4
Electronic patient portals offer the potential to enhance the patient and health care workers' communication and improve clinical care beyond the office visit.5 When utilized effectively patient portals can empower patients to access medical records and interact with their care teams although Chan et al demonstrated low portal use in their patient populations, highlighting its infancy as a communication tool.6 Linde et al examined the effectiveness of one-way text messages and found that they did not improve the attendance rate to follow up among patients with cervical cancer.7
The desire to increase cancer knowledge was associated with a higher likelihood of utilizing a mobile application (OR 261.53;95% CI:10.13–6748.71).8 Mobile health applications improved goal adherence for breast cancer survivors by providing real-time feedback and accountability with the health care team.9
Digital transformation is the integration of digital technology with patients, healthcare providers and regulators.10 Healthcare transformation will add an opportunity to translate new data into actionable information, allowing earlier diagnosis and precise treatment options.11 This integration of innovative technologies will improve the patients’ experience.12
Supportive services are a critical component in managing cancer patients and lack of supportive communication methods between patients and health care workers results in poorer outcomes.13 There are a limited number of studies to guide oncologists on how to effectively communicate during the COVID-19 pandemic. In this survey, we aim to describe the preferences of cancer patients with respect to communication methods and the use of patient-accessible electronic health records (PAEHRs). Consequently, we aim to record the impact of the COVID-19 pandemic on the patient as well as their knowledge and attitude towards it. This could help stakeholders to conduct future studies to optimize interactions and information delivery to cancer patients utilizing the most appropriate technology platforms.
Materials and Methods
We utilized a convenient sampling method. To identify the target population, we contacted the patients’ affairs department and the outpatient administrations to provide a list of all the cancer patients attending the oncology center at King Abdullah Medical City (KAMC), Makkah, Saudi Arabia to participate in the survey.
A web-based questionnaire was designed and sent via text message to cancer patients who are on follow-up or currently receiving anti-cancer treatments under the care of the medical oncologists or malignant hematologists during the COVID-19 outbreak (Jan 1 – April 15, 2020). Non-oncology patients were excluded.
Development of the Instrument
We generated our survey instrument using rigorous survey development and testing methods.14 Items were selected based on literature review, cancer patients’ interviews and telephone correspondence. Five experts in the field of oncology and hematology extensively discussed the topics and reviewed items.
Items were nominated then ranked by expert oncologists to reach a consensus on which items should be selected for inclusion. Review by methodology and content experts to eliminate redundant items using binary responses (exclude and include) was also performed.
We aimed to have a survey that is simple and easy to understand by cancer patients. During the construction of the survey, we grouped the items into the domains we wanted to explore and then refined the questions.15 The self-administered survey consisted of 16 items that focused on four domains: characteristics of patients, characteristics of the tumor, impact of the COVID-19 pandemic and cancer patients’ preferences (Appendix 1).
The structured response format used in this survey included binary response (yes/no) nominal and ordinal. Other options were also allowed such as: undetermined, other and any other comments with free text to capture unanticipated responses.
Testing of the Instrument
During pre-testing and pilot testing, questions were reviewed by five experienced specialists; two experienced nurses, information technology (IT) specialist, patients affairs specialist and a patients experience specialist to check for the consistency and appropriateness of the questions designed by investigators,16,17 it was then reviewed by a non-expert colleague to assess the dynamics, flow and accessibility. Fifteen cancer patients carried out pilot testing of the instrument with appropriate modifications being made accordingly.
We conducted a clinical sensibility assessment to evaluate the comprehensiveness, clarity, and face validity of our instrument on a scale of 1–5. We invited five colleagues with research methodology and oncology expertise in addition to 15 patients with cancer to pilot the survey. Results of the clinical sensibility testing using mean scores on the 5-point scale suggested that the instrument had discriminability (4.3), face validity (4.7), content validity (4.8) and clarity (5).
Administration of the Instrument
The King Abdullah Medical City Institutional Review Board (IRB) approved the study and the IRB number is 20–614. Respondents received electronic links accompanied with concise instructions, a cover letter describing the background, objectives, target population and the request to participate voluntarily as their answers will be anonymized. Consent was obtained from the respondents prior to study commencement.
Study Duration/Study Timeline
On April 15, 2020, we sent an embedded link to the web-based survey on SurveyMonkey and sent reminders one and two weeks later; we then closed the survey on April 30, 2020.
Statistical Analysis
Descriptive statistics were used to summarize the data, synthesize the information and report patients’ preferences. Description of the data included proportions, frequencies, means and standard deviation for the continuous variables where appropriate.
Results
Of 3600 eligible patients, 385 completed the survey yielding a response rate of 11%. Table 1 presents the demographics of the respondents. There were higher proportion of female participants (61%, n=235), the mean age for study participants was 50 ± 15.1 years, majority (30%) were educated to a university level and living in the Makkah region (83%).
Table 1.
Characteristics of Respondents, n (%)
| Male | 150 (39) |
|---|---|
| Female | 235 (61) |
| Age, years, mean ± SD | 50 ± 15.1 |
| Level of Education | |
| Higher Degrees | 32 (8) |
| University | 116 (30) |
| High School | 77 (20) |
| Intermediate School | 31 (8) |
| Primary School | 42 (11) |
| Less than primary school | 66 (17) |
| Prefer not to answer | 21 (5) |
| Region of Living | |
| Makkah region | 320 (83) |
| Albaha region | 15 (4) |
| Aseer region | 15 (4) |
| Jazan region | 13 (4) |
| Madinah region | 8 (2) |
| Tabuk region | 4 (1) |
| Riyadh region | 4 (1) |
| Others | 6 (2) |
Note: This table shows the patients’ profile of the 385 surveyed respondents.
Concerning clinical characteristics, breast cancer was the most common tumor type (35%) followed by colorectal cancer (11%) and lymphoma (10%). Half of the respondents (48%) were on active surveillance. The most common treatment was chemotherapy in 30% of the respondents (Table 2)
Table 2.
Clinical Characteristics, n (%)
| Primary Tumor Site | |
|---|---|
| Breast | 133 (35) |
| Colorectal | 43 (11) |
| Lymphoma | 40 (10) |
| Leukemia | 36 (9) |
| Gynecologic | 35 (9) |
| Urologic | 23 (6) |
| Gastroesophageal | 15 (4) |
| Unknown | 11(3) |
| Head & neck | 9 (2) |
| Lung | 10 (3) |
| Pancreatic-hepatobiliary | 9 (2) |
| CNS | 8 (2) |
| Sarcoma | 8 (2) |
| Thyroid | 5 (1) |
| Stage | |
| Non-metastatic | 232 (60) |
| Metastatic | 153 (40) |
| Treatment | |
| Chemotherapy | 115 (30) |
| Hormonal therapy | 96 (25) |
| Targeted therapy | 50 (11) |
| Immunotherapy | 20 (5) |
| On follow up only | 183 (48) |
Note: This table shows the tumor profile, stage and treatment of 385 surveyed respondents, selection of more than one option allowed.
Abbreviation: CNS, central nervous system.
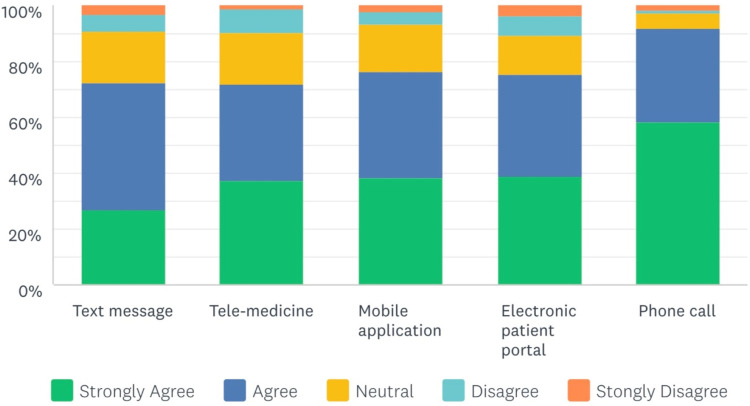
Respondents indicated that the preferred method for communication during COVID-19 was a phone call with a 92% response rate. Proportions of the respondents who preferred the electronic patient portal, mobile application, telemedicine and text messages were 75%, 76%, 73%, 72%, respectively (Figure 1).
Figure 1.
Respondents’ reported preferences of communication methods during the COVID-19 pandemic. This figure shows patients’ responses when asked about their preferred communication methods.
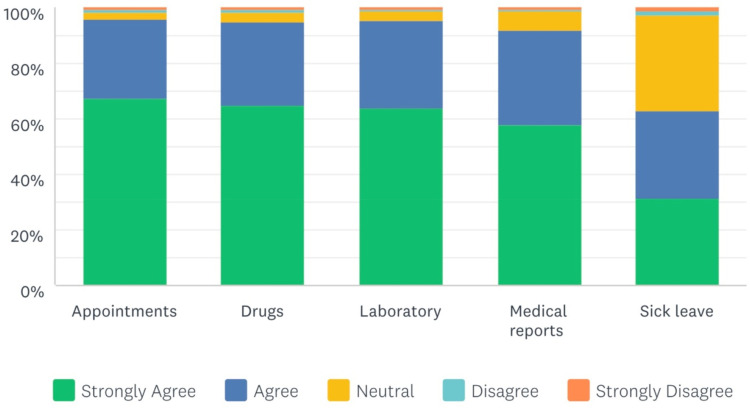
With regard to the preferred use of patient-accessible electronic health records (PAEHRs), the vast majority of respondents (97%) preferred the use of PAEHRs for booking an appointment and rescheduling existing appointments. Drug request/delivery and laboratory results viewing had an equal response of 95%, 92% preferred the PAEHR for medical report requests and 62% for sick leave requests (Figure 2).
Figure 2.
Respondents’ reported preferred use of patient-accessible electronic health records (PAEHRs). This figure shows patients’ responses when asked about preferred use of patient-accessible electronic health records (PAEHRs) to book appointments, request/delivery of drugs, view laboratory tests, view/request medical reports and sick leave.
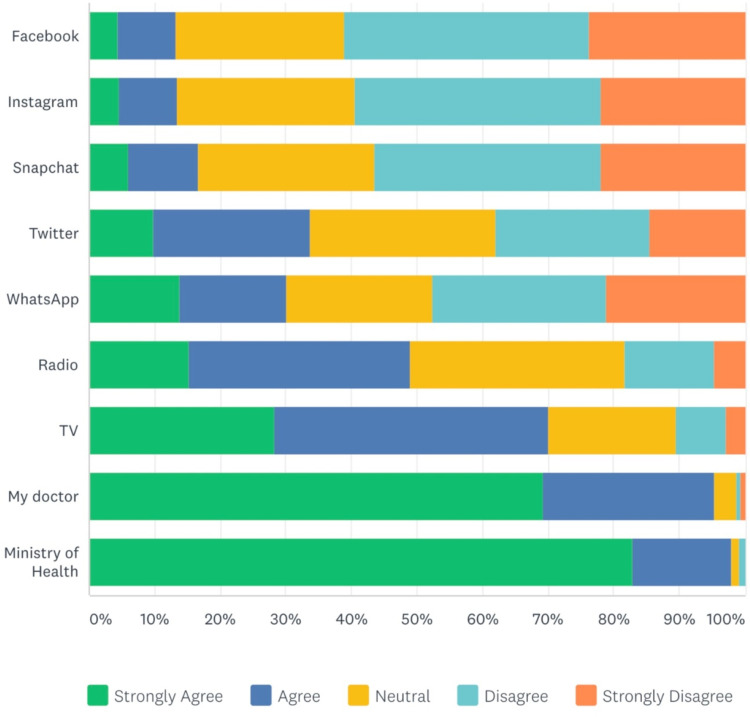
In terms of the impact of COVID-19 pandemic on cancer patients, only 22% reported they were not affected, this means 78% of cancer patients were affected in some way (Table 3). Respondents were asked about which source of information they most trusted during the COVID-19 pandemic, the vast majority (98%) trusted the Ministry of Health (MOH) and doctors with a 94% response rate. In contrast, the minority trusted WhatsApp, Twitter, Snapchat, Instagram and Facebook with confidence percentages of 13%, 34%, 17%, 14%, 13%, respectively (Figure 3).
Table 3.
Impact of COVID-19 on Cancer Patients
| Respondents | n (%) |
|---|---|
| My anti-cancer treatments continued | 157 (41) |
| Unable to attend the clinic due to curfew | 145 (38) |
| I was not affected | 86 (22) |
| My doctor advised me not to come | 78 (20) |
| I was worried about catching COVID-19 in the hospital | 64 (17) |
| My anti-cancer treatments stopped or were delayed | 41 (11) |
| Unable to attend due to transportation issues | 26 (7) |
| News and social media have impacted me | 21 (5) |
| I have asked to stop or hold treatment | 11 (2) |
| My family has asked me not to attend | 5 (1) |
| Other | 62 (16) |
Note: This table shows the impact of the COVID-19 pandemic on cancer patients, selection of more than one option allowed.
Figure 3.
Respondents’ preferred trusted source of COVID-19 information. This figure shows patients’ responses when asked about their preferred trusted source of information during the COVID-19 pandemic, selection of more than one option allowed. TV = Television.
With respect to knowledge, 61% of respondents know that cancer patients are more susceptible to COVID-19 infection compared to 35% who claimed not to know.
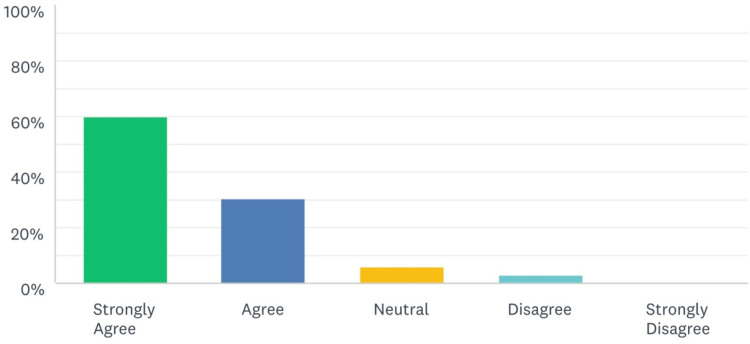
Overall, 91% of respondents supported the notion of digital transformation for improving the care of cancer patients during the COVID-19 pandemic (Figure 4).
Figure 4.
Respondents’ reported support of digital transformation in cancer care? This Figure shows patients’ responses when asked if they support the notion of digital transformation for caring of cancer patients.
Discussion
During curfew, a significant number of patients are self-isolated at home and worried about the exposure to incorrect information. Patient–doctor interaction may be disrupted; therefore, needs to be replaced by alternative effective communication methods to guide patients on the correct precautionary measures and pass on accurate information regarding oncology practice modifications.
To the best of our knowledge, the preferred communication methods during COVID-19 pandemic for cancer patients had not been described before in our patient population. Identification of the preferred communication methods will facilitate the development and implementation of such interventions to improve early diagnosis, precise treatment and improve access to care even during times of international pandemic. Our self-administered survey completed by cancer patients demonstrated that the preferred method for communication is phone call compared to other methods such as the availability of an electronic patient portal, mobile applications, telemedicine and text message (Figure.1).
The likely explanation of why patients preferred a phone call is related to the already established professional relationship with their oncologist that makes the patients feel accommodated and taken care of during these unprecedented times.18 A phone conversation can answer directly any patients’ concerns whilst providing support and instant guidance. It is known that electronic patient portals improved clinical care beyond the office visit,5 despite this fact our results are consistent with Chan et al findings demonstrating low patient-portal use in our population.6 The utilization of Mobile applications is associated with increased cancer knowledge8 and provides real-time feedback.9 Similarly, telemedicine via videoconference is equal in patient satisfaction and perceived quality of care.4 Surprisingly in our study (mobile application and telemedicine) were not the preferred method and this is likely due to similar technology-specific reasons described by Scott Kruse et al,19 and we need better ways to assess the quality and effectiveness of mobile health applications.20 Linde et al examined the effectiveness of one-way text messages7 and similar to our finding, it is not a preferred communication method.
Our study shows that the vast majority of responders preferred to use patient-accessible electronic health records (PAEHRs); and the rates found in our study are higher than those reported by Zanaboni et al.21 These results suggest that our cancer patients are willing to use new technologies to enhance patients experience and access to care.
In our study, we described the impact of COVID-19, from the cancer patients’ perspective, which has not been reported previously to our knowledge. Only 22% claimed to have not been affected, this indicates that 78% of cancer patients were affected in some way by the COVID-19 pandemic.
Our results also demonstrate that the trusted source of information during COVID-19, in the vast majority of cancer patients is the MOH and doctors. This emphasizes the need for direct patient to doctor communication during any crisis. Sixty-one percent of respondents know that cancer patients are more susceptible to COVID-19 infection and overall, 91% of respondents supported the notion of digital transformation for caring of cancer patients. Interestingly, these results confirm the unmet need to transform the current standard of healthcare into fast, simple and effective digital health care.
Our study has several strengths. Firstly, we described the preferred communication methods during the COVID-19 pandemic among cancer patients, which had not been reported before. Secondly, we have used a rigorous methodology for our instrument development, validation and administration as no validated instrument currently exists. Thirdly, we have focused on optimizing the interactions of cancer patients during COVID-19, integrated with preferred communications, PAEHRs, information source, all of which comes from the patients’ perspectives.
Our study has several weaknesses, an important caveat for interpreting our study is the nature of an online survey, no reward incentives were offered, and only 385 responses were obtained from a single institution. One inherent weakness of this study is its restricted participation to single geographical site limiting the inferences that can be drawn from the data. Ideally, we would obtain responses from other geographical locations for synthesis and comparison on a global scale. Another important limitation is that there were differences in the respondents’ demographic make-up, the majority of respondents were females with breast cancer and living in one region, we tried to manage this bias by inviting more respondents to participate. Lastly, the nature of web-based survey could exclude certain demographic groups, with little technological advancements, in particular, low socioeconomic status and the elderly. Understanding the weaknesses due to non-response could be explained by the nature of the web-based survey or due to loss of follow up, death or change in the contact number as we sent the survey via text message. We have invited all potential target populations so they have an equal chance to respond; however, engagement was less than anticipated and we have tried to overcome this by sending reminders and personalized invites during clinic visits.
Future research could be conducted with a more balanced participation in relation to gender, tumor types and geographic distributions in addition to other groups who lack technological advancements who might not be comfortable with novel communication methods.
Our study adds to the previous knowledge that from the cancer patients’ perspective, a phone call is the most preferred method of communication and the vast majority of responders preferred to use patient-accessible electronic health records (PAEHRs) for follow up. Both of these approaches would help with the reduction of COVID-19 transmission, improve access to information and ensure continuity of cancer care. Our results also confirm that cancer patients were impacted by the COVID-19 pandemic and already have the appropriate knowledge received from trusted sources that they are more susceptible to COVID-19 infection consistent with evolving literature.1 Oncologists are the main source of trusted information by cancer patients hence the interaction between cancer patients and their oncologists should not be disrupted.
Many questions remain to be addressed concerning the implications on privacy, ethics, cost, and infrastructures as these novel technologies are not clearly available in all institutions. Finally, an important unanswered question is how to integrate patients’ perspectives with respect to communication methods, use of PAEHRs and health care system functions into one platform to provide better health care outcomes. These are possible avenues for future research to understand how these factors translate into an improvement of cancer care.
Innovative methods to optimize the interaction of cancer patients during pandemics is evolving, if developed and implemented in the appropriate venues they will improve health care outcomes, encourage early diagnosis, and provide precise treatment plans which will reflect positively on the patients experience and reduce the health care burden on health care providers.
Conclusion
Our survey revealed a general acceptance of patients to telecommunication as a substitute to face-to-face in-person interaction with their physicians during a pandemic, the phone call is the most preferred method of communication and the vast majority preferred to use patient-accessible electronic health records (PAEHRs). Both would help with the reduction of COVID-19 transmission, improve access to information and ensure continuity of cancer care. Our results also confirm that cancer patients have been impacted by COVID-19; they know they are more susceptible to COVID-19 infection and have received information from trusted sources. Interactions between cancer patients and health care providers should not be disrupted but augmented with more effective platforms to improve health care outcomes.
Acknowledgments
We thank all patients who participated in this survey. Also, we would like to thank Lawrence, Myer who provided language editing and proofreading. The publication fee for this article was supported by TrakCare, Electronic Medical Record System, InterSystems.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Shankar A, Saini D, Roy S, et al. Cancer care delivery challenges amidst coronavirus disease 19 (COVID-19) outbreak: specific precautions for cancer patients and cancer care providers to prevent spread. Asian Pac J Cancer Prev. 2020;21(3):569–573. doi: 10.31557/APJCP.2020.21.3.569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Shamsi HO, Alhazzani W, Alhuraiji A, et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID19) pandemic: an international collaborative group. Oncologist. 2020;25. doi: 10.1634/theoncologist.2020-0213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McLean S, Sheikh A, Cresswell K, et al. The impact of telehealthcare on the quality and safety of care: A systematic overview. PLoS One. 2013;8(8):e71238. doi: 10.1371/journal.pone.0071238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barsom EZ, Jansen M, Tanis PJ, et al. Video consultation during follow up care: effect on quality of care and patient- and provider attitude in patients with colorectal cancer. Surg Endosc. 2020. doi: 10.1007/s00464-020-07499-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ralston JD, Rutter CM, Carrell D, Hecht J, Rubanowice D, Simon GE. Patient use of secure electronic messaging within a shared medical record: A cross-sectional study. J Gen Intern Med. 2009;24(3):349–355. doi: 10.1007/s11606-008-0899-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan B, Lyles C, Kaplan C, Lam R, Karliner L. A comparison of electronic patient-portal use among patients with resident and attending primary care providers. J Gen Intern Med. 2018;33(12):2085–2091. doi: 10.1007/s11606-018-4637-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Linde DS, Andersen MS, Mwaiselage JD, Manongi R, Kjaer SK, Rasch V. One-way text messages versus no text messages on attendance to follow-up cervical cancer screening among HPV-positive Tanzanian women (Connected2Care): a parallel-group randomized controlled trial (Preprint). J Med Internet Res. 2019;22(4):e15863. doi: 10.2196/15863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Potdar R, Thomas A, DiMeglio M, et al. Access to internet, smartphone usage, and acceptability of mobile health technology among cancer patients. Support Care Cancer. 2020. doi: 10.1007/s00520-020-05393-1 [DOI] [PubMed] [Google Scholar]
- 9.Stubbins R, He T, Yu X, et al. A behavior-modification, clinical grade mobile application to improve breast cancer survivors’ accountability and health outcomes. JCO Clin Cancer Informatics. 2018;2:1–11. doi: 10.1200/CCI.18.00054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Why digital transformation for healthcare isn’t about technology qualtrics. Available from: https://www.qualtrics.com/blog/healthcare-digital-transformation/. Accessed April8, 2020.
- 11.Seyhan AA, Carini C. Are innovation and new technologies in precision medicine paving a new era in patients centric care? J Transl Med. 2019;17(1). doi: 10.1186/s12967-019-1864-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Transforming healthcare practices and patient care in the digital era - MedCity news. Available from: https://medcitynews.com/2020/01/transforming-healthcare-practices-and-patient-care-in-the-digital-era/. Accessed April8, 2020.
- 13.Hendren S, Chin N, Fisher S, et al. Patients’ barriers to receipt of cancer care, and factors associated with needing more assistance from a patient navigator. J Natl Med Assoc. 2011;103(8):701–710. doi: 10.1016/S0027-9684(15)30409-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Méndez LA. From lisp to fuzzy lisp. Stud Fuzziness Soft Comput. 2017;349(3):339–350. doi: 10.1007/978-3-319-48317-7_21 [DOI] [Google Scholar]
- 15.Passmore C, Dobbie AE, Parchman M, Tysinger J. Guidelines for constructing a survey. Fam Med. 2002;34(4):281–286. [PubMed] [Google Scholar]
- 16.llins D. Pretesting survey instruments: an overview of cognitive methods. Qual Life Res. 2003;12:229–238. doi: 10.1023/A:1023254226592 [DOI] [PubMed] [Google Scholar]
- 17.Woodward CA. Questionnaire construction and question writing for research in medical education. Med Educ. 1988;22(4):345–363. doi: 10.1111/j.1365-2923.1988.tb00764.x [DOI] [PubMed] [Google Scholar]
- 18.Jørgensen L, Jacobsen HR, Pedersen B, Uhrenfeldt L. Calling an oncological emergency telephone to seek advice. Cancer Nurs. 2019. doi: 10.1097/ncc.0000000000000778 [DOI] [PubMed] [Google Scholar]
- 19.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare. 2018;24(1):4–12. doi: 10.1177/1357633X16674087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McKay FH, Cheng C, Wright A, Shill J, Stephens H, Uccellini M. Evaluating mobile phone applications for health behaviour change: A systematic review. J Telemed Telecare. 2018;24(1):22–30. doi: 10.1177/1357633X16673538 [DOI] [PubMed] [Google Scholar]
- 21.Zanaboni P, Kummervold PE, Sørensen T, Johansen MA. Patient use and experience with online access to electronic health records in norway: results from an online survey. J Med Internet Res. 2020;22(2):e16144. doi: 10.2196/16144 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Why digital transformation for healthcare isn’t about technology qualtrics. Available from: https://www.qualtrics.com/blog/healthcare-digital-transformation/. Accessed April8, 2020.
- Transforming healthcare practices and patient care in the digital era - MedCity news. Available from: https://medcitynews.com/2020/01/transforming-healthcare-practices-and-patient-care-in-the-digital-era/. Accessed April8, 2020.