Abstract
Purpose of the study
The Coronavirus disease 2019 (COVID-19) pandemic has had profound effects on healthcare system including medical training and education in India. The study was aimed to evaluate the impact of COVID-19 on post-graduate teaching and learning amongst candidates pursuing higher qualification in orthopaedics, in the Delhi-National Capital Region in India.
Design
An online cross-sectional survey of 29 questions was circulated amongst post-graduate students pursuing higher orthopaedics degree to evaluate (i) Impact on PG teaching (ii) Impact on surgical training (iii) Impact on Dissertation (iv) Future implications on PG training programme (v) Mental wellbeing.
Results
138 (77.5) PG trainees contributed in the survey, and 65.1% of them stated that no clinical classes are being held presently. The majority (94%) confirmed that COVID-19 has affected their surgical and clinical training. A large number (71.6%) had problems in completing their dissertations and 96% had concerns about mental health.
Conclusion
COVID-19 pandemic has severely disrupted the education and training of the Orthopaedic PG students, in Delhi-NCR region and perhaps elsewhere similarly too. The Government and Teaching organisations should take serious consideration of the plights of PGs and devise satisfactory mechanisms to overcome their problems and provide reasonable solutions also.
Keywords: COVID-19, Coronavirus, Pandemics, Orthopaedics, Education, Medical, Interactive learning environments
1. Introduction
The World Health Organization (WHO) declared Coronavirus disease 2019 (COVID-19) as pandemic on 11th March 2020.1 To contain and prevent the pandemic, Government of India announced many steps such as nationwide lockdown on March 25, 2020, promoting social distancing and infection control guidelines including the use of masks, personal protective equipment (PPE).2,3 The stringent ‘Lockdown’ restrictions has disrupted daily life, also affecting the field of orthopaedics including orthopaedic surgeons and trainees.4,5 Routine out-patient department (OPD) services and elective surgeries have been cancelled which has decreased orthopaedic patient influx to hospitals. Institutes and hospitals have re-organised orthopaedic services with cancellation of face to face lectures, clinical rounds, seminars, and similar academic and teaching activities.6 This has affected post-graduate (PG) teaching and learning in an unprecedented manner. The PG teaching in orthopaedics is going through difficult times during COVID-19 pandemic.
We have conducted an online survey among currently pursuing PG students of orthopaedics in Delhi- National Capital Region (Delhi-NCR) area to find out the impact of COVID-19 on PG teaching and learning. Difficulties and problems faced by them during the pandemic in terms of the progress in dissertation, lectures, seminars, clinical case discussions, surgical training, re-deployment challenges and the effect on mental health were enquired.
2. Material and methods
Study design: This cross-sectional study (online survey) was conducted from June 11, 2020 to June 15, 2020, to study the problems faced by PG students in orthopaedics in Delhi-NCR area. A questionnaire of 29 questions was created and was circulated among students pursuing post-graduation (MS and DNB), in orthopaedics in Delhi-NCR area of all governments and private hospitals using online website available at https://www.surveymonkey.com/ (Appendix 1: Questionnaire regarding Impact of COVID-19 on Post graduate teaching of orthopaedics).
Inclusion criteria: The target population for this study are PG students who are currently pursuing Masters in Orthopaedic Surgery (MS Ortho.), primary Diplomate National Board (DNB) (Orthopaedics), secondary DNB (Orthopaedics), from teaching institutions within the Delhi-NCR area.
Data collection: The responses submitted were checked for duplication, pooled, analysed, and summarised.
Evaluation: The survey focussed on following points
-
1.
Impact on PG teaching and its current status
-
2.
Impact on surgical training.
-
3.
Impact on Dissertation
-
4.
Future implications on PG training programme
-
5.
Mental wellbeing.
2.1. Statistical analysis
Data was entered in SPSS (Statistical product and service solutions) version 26 (IBM Corp) for statistical analysis. Frequencies/percentages were summarised for all categorical variables and Chi square test, Fisher’s exact test or Monte-Carlo simulation were used as appropriate. We have used Wilcoxon sign rank rest for pre (2019) and post COVID (2020) data in the same months for number of classes and cross tabulation and chi square tests for other variables for testing association. All results are described in percentage. A two-sided P value < 0.05 was considered as significant.
3. Results
3.1. General characteristics
The survey was sent to the most (178) orthopaedic PG students, who could be traced in Delhi-NCR region. A total of 143 responses were collected in the survey. Responses were checked for duplication and there were five responses from participants which were found repeated. These responses were deleted and finally 138 responses were included in the final analysis of results, with a 77.5% response rate.
72.65% respondents were pursuing MS (Orth) course, whereas 27.35% were DNB (Orthopaedics) students. 61.5% were postgraduate students at the government institutions and the majority respondents (55.5%) were in their third year of PG course.
3.2. Impact on teaching
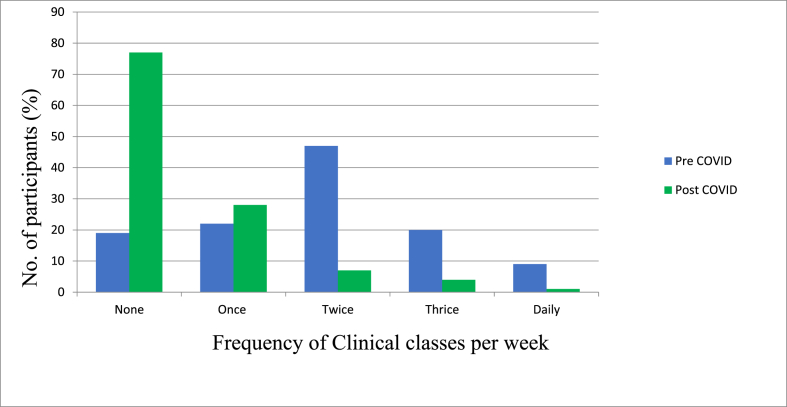
Prior to COVID-19 pandemic, the majority of students were attending PG classes twice or thrice in a week (57.26%). However, some respondents (16.24%) said that they did not have any regular classes at their institution. During the COVID-19 pandemic, the number of PG classes have been significantly reduced to none as reported by 65.81%, remained twice or thrice a week by 9.4% and once a week by 23.9% (P < 0.001) (Fig. 1).
Fig. 1.
Pattern of teaching classes during and before COVID 19 pandemic.
During COVID-19 pandemic, the majority of classes and case presentations are being conducted virtually (89.09%); mostly on the ZOOM platform (51.82%), followed by Cisco WebEx (15.45%), and Microsoft Teams (9.09%). However, only 27.27% PG students were satisfied with the virtual classes; 40.9% were not satisfied and 31.8% were satisfied only to some extent. (P < 0.001).
3.3. Impact on PG training and dissertation
The majority (84.5%) felt that their basic skills in various common orthopaedic procedures such as cast application, skin, and skeletal traction application, local and intra articular injections, wound care and dressings are severely affected during COVID-19 pandemic. This feeling was significantly associated with feelings of overall decrease in clinical and surgical learning during PG course due to COVID 19(P < 0.001) and feeling of lack of competency to work in independent practice after PG completion (P < 0.001).
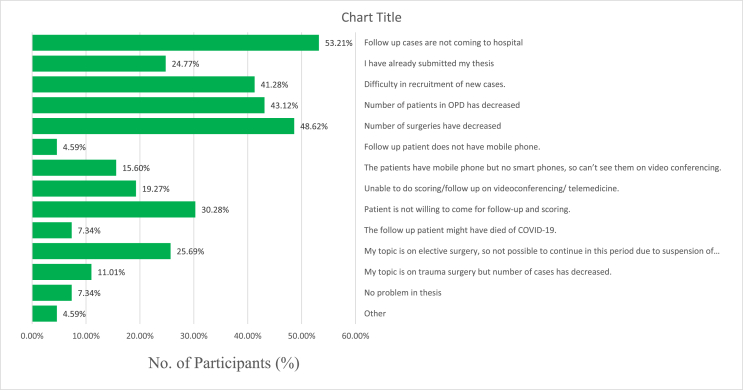
Only 28.4% students had completed their dissertation and the majority remaining were struggling with the completion of their research and dissertation work, due to several reasons. Major reasons being follow up patients which were part of their study are not coming to the hospital (53.2%) followed by decrease in number of surgeries (48.6%), decrease in number of OPD cases (43.1%) and difficulty in recruitment of new cases (41.2%) (Fig. 2).
Fig. 2.
Problems faced by PG students regarding their dissertation.
Almost all the student felt the lack of clinical teaching (96%) on the ward rounds and case presentations (91%). These feelings (lack of clinical teaching and lack of case presentation) were significantly associated with feelings of COVID-19 having an overall negative effect on passing the PG final examination (P < 0.001).
3.4. Problems and difficulties faced by PG students
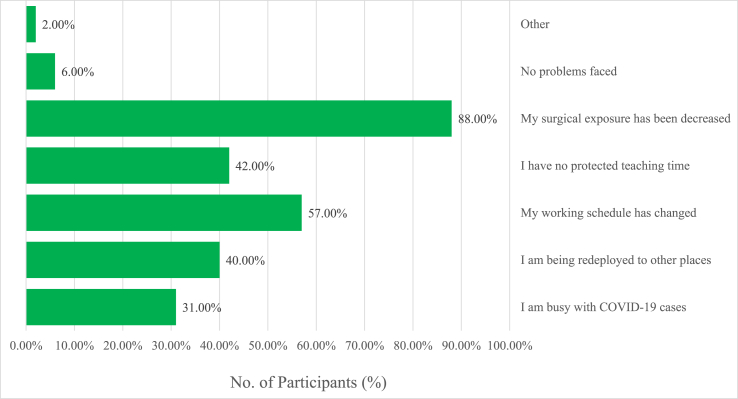
Major difficulties faced by PG students in training were decrease in surgical exposure (88%), change in working schedule (57%), decrease in teaching time (42%) and redeployment to other places (40%) (Fig. 3).
Fig. 3.
Difficulties faced in PG training during COVID-19 Pandemic.
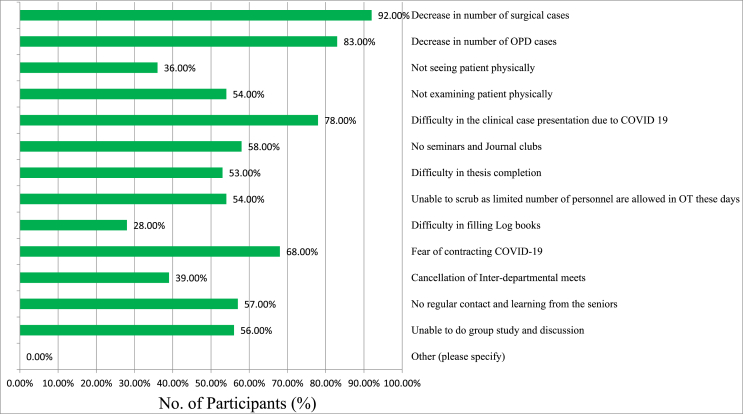
As a PG student, major problems faced by PG students were significant decreased load in the surgical cases (92%), lesser OPD cases (83%), difficulty in clinical case presentation (78%), fear of contracting COVID-19 (68%), and cessation of seminar and journal clubs (58%), amongst others (Fig. 4).
Fig. 4.
Problems faced as a PG student in COVID-19 pandemic.
The vast majority of the PG students (94%) confirmed that COVID-19 pandemic has overall decreased their clinical and surgical training and this was significantly associated with (around 70% students) the feeling that it has negatively affected their chances of passing the final PG exit exam (P < 0.001).
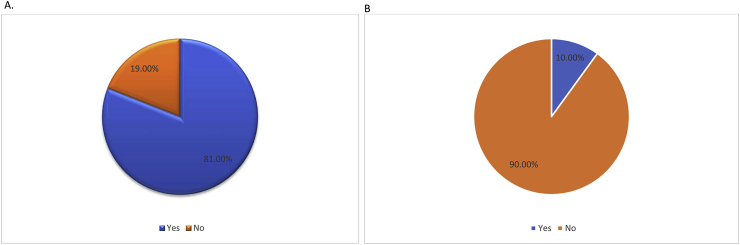
Majority of the PG students (71.56%) were redeployed for other non-orthopaedic duties, related to the management of COVID-19 patients and 81% of them had come in contact with the COVID-19 patients, during their clinical duties (Fig. 5A). 10% of the trainees were also infected with COVID-19 (Fig. 5B).
Fig. 5.
Exposure with or treatment of any COVID-19 patients by PG students (A); PG students contracted or acquired COVID-19 infection while performing duties (B).
The risk of contracting COVID infection was significantly associated with redeployment for Screening in OPDs, COVID wards, ICU’s, or other places in the hospital, and with history of exposure to COVID positive patients during the course of treatment (P < 0.001).
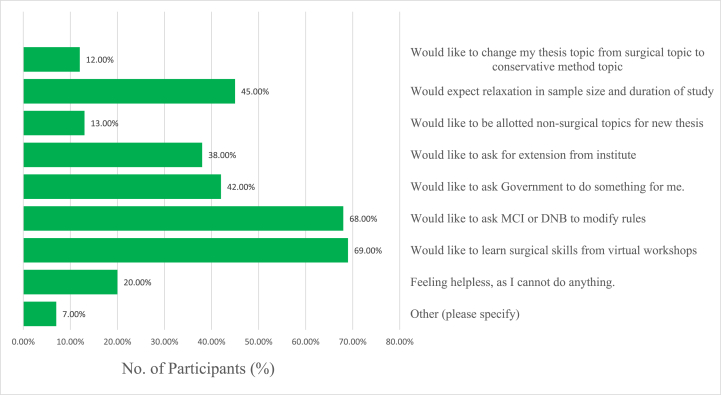
3.5. Future implications of COVID-19 on PG training programme
If the COVID-19 crisis is prolonged then the majority student (68%) were of the opinion that they should approach the government and educational bodies to help them out, by modifying the rules of their training and exit exam. 69% of the respondents are of opinion that they would like to learn surgical skills from virtual workshops. Around one-third (38%) trainees would like to ask extension in training period from institute (Fig. 6).
Fig. 6.
Suggestions for alleviating problems faced by PG students suppose if this COVID-19 crisis continues for another 6 months as given by PG students.
83% participants were of the view that the Medical Council of India (MCI) criteria of presenting poster and paper in conference are not possible in this time, due to COVID-19 pandemic during their PG tenure.
89% participants were confused in their choice of virtual classes and seminars with so many being conducted across the country. Significant association was seen with anxiety about difficulty in poster and paper presentations (83%) and confusion about choosing appropriate virtual seminars and classes (89%).
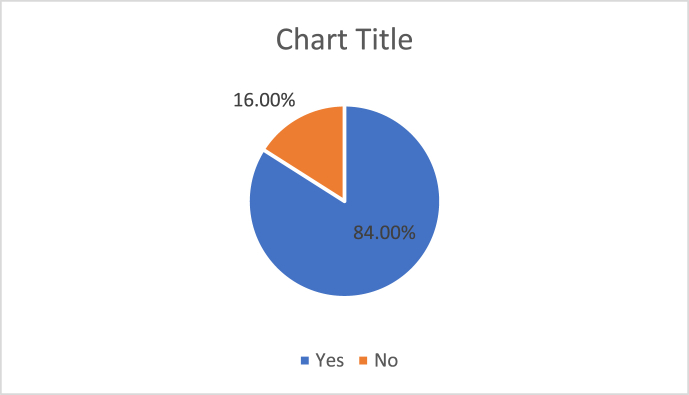
As the number of surgeries are going down significantly in hospitals 84% feel that teaching on simulators may be helpful during COVID-19 pandemic (Fig. 7). More than half (55%) trainees felt that due to decreased surgical experience, their confidence in doing independent practice after completing their post-graduation was significantly reduced.
Fig. 7.
Usefulness of simulator techniques in COVID-19 pandemic for learning.
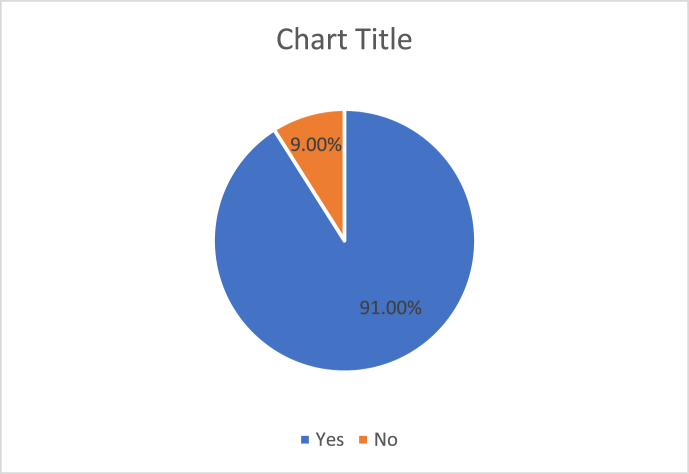
Around two-thirds students were in the favour of continuing their learning by virtual teaching and workshops during the pandemic, although the majority (91%) confirmed that the virtual teaching cannot replace the face-to-face teaching (Fig. 8). About 3/4 respondents were still in favour of face to face examinations instead of virtual examination for PG exit exam.
Fig. 8.
Importance of face to face teaching in relation to virtual teaching especially for clinical case discussions.
3.6. Mental well being
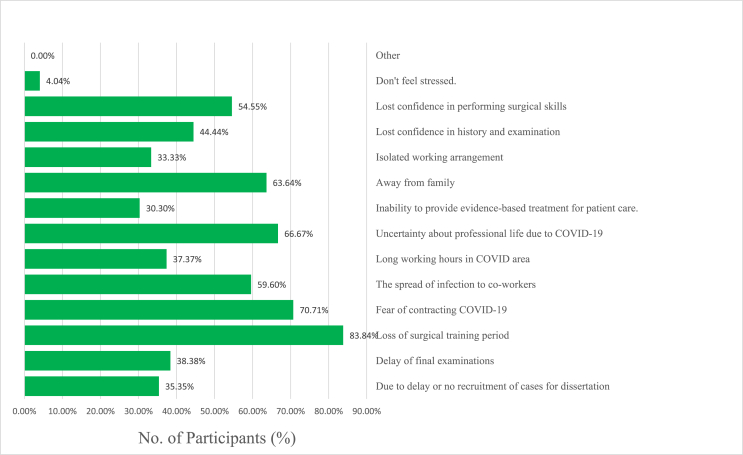
96% of orthopaedic residents feel stressed during COVID pandemic times. Major reasons were the loss of surgical training period (83.8%), fear of contracting COVID-19 (70.7%), uncertainty about professional life due to COVID-19 (66.6%), being away from family (63.64%), spread of infection to co-workers (59.6%) and have lost confidence in acquiring surgical skills (54.5%), amongst the others (Fig. 9).
Fig. 9.
Reason (s) for PG students to feel stress during COVID-10 pandemic.
Association between different variables and their significance is summarised in Table 1.
Table 1.
Association between different variables and their significance.
| Variables | P value < 0.05 |
|---|---|
| Effect on basic clinical skills (for e.g., Slab and cast application, skeletal and skin traction application, local and intra-articular injections, wound care) in COVID-19 pandemic. AND Decrease in clinical and surgical learning during PG course in COVID-19 pandemic. | Yes |
| Effect on ward round clinical teaching COVID-19 pandemic. AND Negative effect of COVID-19 on chances of passing the PG final examination. | Yes |
| Decrease in case presentation, physically, during this COVID-19 period after March 25, 2020 to till date. AND Negative effect of COVID-19 on chances of passing the PG final examination. | Yes |
| Confusion about choosing appropriate virtual classes and seminars. AND Difficulty in presenting poster and paper presentation in conferences. | Yes |
| Redeployment for duties for Screening in OPDs, COVID wards, ICU’s or other places in the Hospital.AND Exposure with or treatment of any COVID-19 patients and risk of contracting COVID-19. | Yes |
| Effect on basic clinical skills (for e.g., Slab and cast application, skeletal and skin traction application, local and intra-articular injections, wound care) in COVID-19 pandemic. AND Redeployment for duties for Screening in OPDs, COVID wards, ICU’s or other places in the Hospital. | Yes |
4. Discussion
In India, the PG teaching in Orthopaedics is usually offered through different courses; MS, DNB, and Diploma in Orthopaedics (D.Orth).7,8 The purpose of PG course in Orthopaedics is to create professionals who can impart high quality and specialized health care services at different level of health centres. COVID-19 has caused unprecedented changes to orthopaedic training. As orthopaedic residents continue to perform necessary patient care during the COVID-19 crisis, they will unquestionably face both daily challenges to personal health and long-term questions about their training experience.9 Our survey demonstrated that problems in the training of PG students are significantly increased due to COVID-19 pandemic.
4.1. Impact on teaching
Lectures and theoretical classes have been cancelled in the teaching hospitals and institutions to prevent and contain the spread of COVID-19.10 Seminars and Journal clubs have also taken a hit as reported by 58% respondents. Inter-departmental academic meets such as with radiology, pathology, physiotherapy, and nursing departments to discuss important and unique cases have also been cancelled, as of now as reported by 39% participants.
But the real difficulty lies with the clinical classes and physical examinations by the PG students. As this survey shows that 65.81% respondents claim that no clinical classes have been conducted in their institutes. There is statistically significant decrease in frequency of clinical classes conducted at different institutes (P < 0.001).
Many Institutes have shifted to virtual classes and clinical case presentations through online video platforms such as Zoom, Cisco Webex, Microsoft teams etc.11 However, the satisfaction rate of use of these platforms is not high. Palan et al. have reported their exposure of conducting virtual learning systems and ‘virtual’ journal clubs. There are both advantages and disadvantages of virtual learning methods. Advantages being: a) easy accessibility of the educational content, b) facility of attaching images and radiographs to web-based platforms (which can provide more valuable information and stimulate discussion), c) no risk of exposure to COVID-19 and d) confer utilisation of time at home. However, the disadvantages include: a) no compulsion to attend the classes online, b) the virtual classes are time bound (the educators need to finish lecture and discussion with stipulated time), c) lack of two ways discussion, in many such lectures, d) the infrastructure remains a potential hurdle for successful implementation of virtual learning platforms, and e) the success largely depends upon the consultant and faculty participation and input that guides and control the discussion.12 Institutes and hospitals across the country should collaborate and share their experience and educational material with others.
The education and training of PGs is consolidated by high volume of patients encountered in the out-patients department (OPD). A disease can present with variety of manifestations and high patient exposure allows PG students to understand atypical presentations of common diseases, rare diseases, and diversity of disease pathologies. History taking and physical examination can only be learned and excelled when it is done in person. Online videos or tutorials can show PG students how to take history and perform a test, but it is difficult to get feel of signs on virtual platforms and this places students at a significant disadvantage. Almost all the trainees in this survey felt the lack of clinical teaching (96%) on the ward rounds and case presentations (91%).
There are lot of webinars being hosted on various topics. This provides PG students an opportunity to learn from the best of the field. But this also creates confusion in their mind as reflected in this survey. There should be proper coordination among the various orthopaedic societies and organizers to streamline such issues. State medical councils could give accreditation to these academic activities as Continued Medical Education activities which would work favourably for PG students.
4.2. Impact on PG training and dissertation
Routine OPD and elective non urgent surgeries have also been suspended at most places.10 The reduced patient load has affected the demonstration of many clinical skills such as slab and cast application, skeletal and skin traction application, local and intra-articular injections, wound care, and dressings as reflected in this survey also. Decrease in number of cases for clinical discussions could be dealt with the use of card cases and other tools such as virtual classes. In case, it is essential to examine the patient in face to face clinic the student must wear full Personal Protective Equipment (PPE), which may not be feasible in most places.13
Video conferencing facilities could be used for demonstration of technical procedures and other small procedures if feasible. Faculty members may use instructional videos to teach PG students and discuss with them online11
Surgery is an art and it can be learned and mastered at a place, where it is performed. While the number of elective orthopaedic surgeries such as arthroplasty, arthroscopy, spine, and other specialized surgeries has been reduced, the opportunity for PG student to observe, assist and perform the surgery has also been lost during the pandemic. This is the major difficulty faced by almost 92% of PG students. Decrease in surgical and clinical learning was causally related to the effect of COVID-19 on basic clinical skills (P < 0.001).
Surgical simulation techniques are rapidly evolving field and would be powerful and important tool for teaching osteo-synthesis and arthroscopic surgeries to PG students which would provide them valuable experience and meet the surgical training demand.14,15 This technology can improve the surgeon’s confidence. However, this is costly and requires infrastructure space which may be a concern for many hospitals. It has to be noted though only a few surgical procedures can be learnt using simulation techniques.16
To prevent the spread of COVID-19 and following the norms of social distancing, the number of personnel in OT has to be kept to minimum and may thus influence their participation in all the surgical procedures. Similar recommendations have also been provided by other authors.11
PG students who have a dissertation to submit are finding themselves in a difficult situation. Patients who are the part of their clinical studies have not been able to come to the hospital for follow up because of lockdown, travel restrictions and migration to home states from big cities. It is difficult to recruit new patients for those PG students who have dissertation topics related to non-urgent elective surgeries as elective surgeries and OPD have been shut down. Some patients don’t want to come to the hospital for follow up because of risk of contracting COVID-19. Even for those students, whose topics are related to trauma surgeries, the number of patients has decreased considerably. Most of the operated patients are followed up by the surgical team through telemedicine or remote consultations (e.g. telephone or video consultation), so as to avoid their hospital visit and face-to-face interaction with the doctor and other hospital staff.17 Gathering information about outcome scores and follow-up radiographs is difficult in this scenario. This has caused great inconvenience for the PG students and faculty members.
4.3. Problems and difficulties faced by PG students
PG students have difficulty in presenting clinical cases, are not able to examine patients physically and there is no face to face interactions with patients. Some hospitals are being converted to COVID-19 hospital. This has changed the working schedule of PG students, decreased the time available to study, completely ceased any possibility of orthopaedic elective work to be done in that hospital and increased the chance of infection of COVID-19. Redeployment of orthopaedic trainees has been found up to 71.56% as per this survey. They have been redeployed to other areas of hospital such as Screening OPDs, COVID wards, ICU’s etc. which is necessary as redistribution of available resources is required to fight COVID-19 pandemic. However, this is impacting on the PG students as they are busy in work other than their specialized orthopaedic work. Redeployment to other areas was also significantly associated with feelings of decreased exposure to basic skills (P < 0.001).
The focus of the PGs has now shifted to COVID-19 due to redeployment and 40% respondents are finding it difficult. If this paradigm shift continues for too long, the orthopaedic PGs may lose skills in managing a broad range of orthopaedic surgical pathologies.18 Social distancing norms have prevented group study and discussion among PG students.
Logbooks need to be signed by faculty members as part of academic curriculum. As the patient load has been reduced and there is redeployment of PG students to non-orthopaedic work, students would find it hard to fill the details of surgical procedures performed or assisted. This problem has been reported by 28% of respondents.
The majority of PG students have come in contact with the COVID-19 patients during their clinical duties and 10% of these students have contracted COVID-19 which should be a cause of concern. Redeployment was related to the risk of contracting COVID-19 (P < 0.001).
4.4. Future implications of COVID-19 on PG training programme
It is desirable as a part of curriculum for PG students to present poster and paper at conferences and attend at least 2 conferences or workshops or continued medical education (CME) activities during their tenure. However, this is not possible now as reported by 83% of participants of this survey. Students face difficulties as academic conferences and workshops have been cancelled and it is unclear when these academic activities would restart.
Connecting with experts in field of orthopaedics face-to-face is most valuable opportunities during live conferences for future research, publication and receiving expert advice in their practice. Virtual meetings do not replicate face-to-face interaction at such meetings. Thus, PG students will lose this opportunity to network with experts in their desired fields in virtual meetings.
PG students who were due to appear for their final examination have faced a lot of uncertainty and anxiety. Many institutes have delayed their PG examinations and are waiting for guidelines from universities. 70% feel that COVID-19 pandemic has negatively affected their chances of passing their exit examination and it is related to the decrease in the ward round clinical teaching (P < 0.001) and decrease in the clinical case presentation (P < 0.001).
It is not known that how long COVID-19 pandemic is going to stay. What PG students would like to change in the current scenario if similar situation continues for another 6 months? Majority would like to approach government and higher bodies to modify rules for PG training and would like to learn from virtual workshops.
As all PG courses are of fixed tenure there is loss of precious time of approximately 2–3 months for teaching and learning. It is anticipated that these residents may graduate and become specialist/consultant without achieving proficiency in essential surgical procedures.18 Similar finding has been brought out during our survey where 55% participants don’t feel competent enough to work independently after PG completion.
4.5. Mental well being
Orthopaedic PG students are exposed to stressful life and COVID-19 pandemic has added to it. COVID-19 pandemic has effect on mental health and wellbeing according to World health Organization (WHO).19 Mental well-being is often overlooked. COVID-19 has impacted the surgical training period. And there is lot of uncertainty regarding future prospects. They expose not only themselves but their family members too through them to COVID-19. Some are not able to visit their families because of lockdown measures. Saddik B et al. also reported mild to severe anxiety in medical students during COVID-19 pandemic which decreased after the introduction of online teaching programmes.20 Institutions should be aware of this fact and should be proactive in providing the necessary counselling services required for the sound mental well-being of the students.
Adequate sleep and rest are essential to those who are working in COVID-19 area for long hours. The orthopaedic training for post-graduates during this phase must essentially include daily updated information on the nature of pandemic, the rationale behind the use PPE, social distancing, safe surgical skills, and other essential things to prevent them from contracting COVID-19. This can be through video lectures or through social media such as WhatsApp, Facebook, and Twitter over smartphone.21
Possible solutions or Recommendations for PG teaching programme during COVID-19 pandemic is summarised in Table 2.
Table 2.
Recommendations and possible solutions for PG teaching programme during COVID-19 pandemic.
| S.No. | Problems | Recommendations and possible solutions |
|---|---|---|
| 1. | Decrease in OPD cases | Use of Telehealth OPD services |
| 2. | Decrease in Surgery cases | Use of Simulator techniques Waiver by MCI for the minimum number of procedures required by trainee |
| 3. | Decrease in Academic activities (Clinical case presentations, Journal clubs, Seminars, Inter departmental meets etc.) |
|
| ||
| ||
| ||
| ||
| 4. | Examination issues |
|
| ||
| 6. | Dissertation issues |
|
| ||
| 7. | Conferences/Workshops/CME |
|
| ||
| ||
| ||
| 8. | Mental wellbeing | Counselling |
The COVID-19 pandemic has also been learning opportunity and appears to have been a catalyst for new, innovative ways delivering teaching and training.22 In these COVID-19 times, clinicians have more time compared to the regular days. Hence, they have the opportunity to update themselves as well. This in turn is helping them impart their up to date knowledge via webinars, virtual meets and paper writing. Hence, improving the quality of learning and the participants also has a chance to ask one to one questions and clarify. The virtual learning environment results in increased trainee participation and consultant input in the virtual journal club and case-based discussions. As we develop innovative ways to support and provide teaching in all fields of life with virtual learning platforms, focus on patient centred care still remains the core responsibility of all health care professionals.
4.6. Limitations of the study
This survey was based on the data known to us and some of the PG students might have been missed out due to non-availability of their contact details. However, we believe that this survey has included majority of the PG students and their response rate of 77.5% has been satisfactory. Further this survey was open for all postgraduates. The 1st and 2nd year PGs are usually busier in the hospital work and have different priorities, as compared to the 3rd year PGs and therefore more participation of the 3rd year PGs, in this survey could be a possible source of bias. We did not calculate the proportion of postgraduate responders in each collage separately, as it was not known how many were working in each collage in the orthopaedic department, and finding the later would involve administrative issues. As we have not asked the name of institutes from participants, there may be a possibility that many PG students from a single medical college/hospital have responded. Such surveys are based on the perception and response of the participants, who may not be honest in replying to all the questions correctly. Lastly COVID 19 has undoubtedly created unique difficulties for all academic orthopaedic setups, and this is highly likely to affect moods of the participants. Varying moods and circumstances may lead to variability in survey participation, and may also affect responses.
5. Conclusion
COVID-19 pandemic has severely disrupted the education and training of the Orthopaedic PG students, in the capital of India. No such study has yet analysed, in depth, about the problems faced by these young trainees. There has been a significant reduction in the PG classes, clinical and practical training. Significant reduced flow of patients to the hospital, and has directly affected the training of the PGs, through much lesser attendance in the OPDs, in patients, and surgical work. The PGs also have serious problems in completing their dissertations and learning from attending the workshops and conferences. In addition, the trainees have increased mental stress and many feel that they may not pass the exit exam and practice independently after their PG course, due to inadequate training. 10% of these students have also acquired COVID, during their hospital duties. This paper clearly outlines the changes in orthopaedic academic environment in India due to COVID 19, as perceived by postgraduate students, and may provide insights for responsible stakeholders involved in orthopaedic education in the country. The Government and Teaching organisations should take serious note of the plights of PGs and devise satisfactory mechanisms to overcome their problems and provide reasonable solutions also.
Authors statements
Author’s Contributions: GU and VJ involved in Conceptualization, literature search, manuscript writing and editing. KPI, AV and MKP in Literature search, methodology, Data curation, manuscript review and editing. VJ supervised overall submission and approved final draft. All authors read and agreed the final draft submitted.
Funding statement
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Statement of ethics
All our clinical procedures were fully compliant with the ethical standards in accordance with the local consenting and ethics guidelines. The current submitted article is not a clinical study and does not involve any patients.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2020.07.018.
Contributor Information
Gaurav Kumar Upadhyaya, Email: drgkupadhyaya@yahoo.in.
Vijay Kumar Jain, Email: drvijayortho@gmail.com.
Karthikeyan P. Iyengar, Email: kartikp31@hotmail.com.
Mohit Kumar Patralekh, Email: mohitkumarpatralekh@gmail.com.
Abhishek Vaish, Email: drabhishekvaish@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Who Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 accessed on.
- 2.COVID-19 India. https://www.mohfw.gov.in accessed on.
- 3.Ministry of Health and Family Welfare Government of India (MOHFW) eSanjeevani- an integrated telemedicine solution. https://esanjeevani.in/
- 4.Haleem Abid, Mohd Javaid, Raju Vaishya, VaishAbhishek Effects of COVID-19 pandemic in the field of orthopaedics. J Clin Orthop Trauma. 2020;11 doi: 10.1016/j.jcot.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jain V.K., Vaishya R. COVID-19 and orthopaedic surgeons: the Indian scenario [published online ahead of print, 2020 Apr 21] Trop Doct. 2020 doi: 10.1177/0049475520921616. 49475520921616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lal H., Sharma D.K., Patralekh M.K., Jain V.K., Maini L. Outpatient Department practices in orthopaedics amidst COVID-19: the evolving model [published online ahead of print, 2020 May 18] J Clin Orthop Trauma. 2020 doi: 10.1016/j.jcot.2020.05.009. 10.1016/j.jcot.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Postgraduate-Medical-Education-Regulations-2000. Available at: https://www.mciindia.org/CMS/rules-regulations/p-g-medical-education-regulations-2000. Accessed on.
- 8.Guidelines for competency based training programme in DNB- ORTHOPEDICS. https://nbe.edu.in/mainpdf/curriculum/Orthopedics.pdf Available at: Accessed on.
- 9.An T.W., Henry J.K., Igboechi O. How are orthopaedic surgery residencies responding to the COVID-19 pandemic? An assessment of resident experiences in cities of major virus outbreak [published online ahead of print, 2020 Jun 1] J Am Acad Orthop Surg. 2020 doi: 10.5435/JAAOS-D-20-00397. 10.5435/JAAOS-D-20-00397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Circulars for COVID-19/ministry of home affairs/GOI. Available at: https://www.mha.gov.in/notifications/circulars-covid-19. Accessed on.
- 11.Chick R.C., Clifton G.T., Peace K.M. Using technology to maintain the education of residents during the COVID-19 pandemic. J Surg Educ. 2020 Apr 3;77(4):729–732. doi: 10.1016/j.jsurg.2020.03.018. Epub ahead of print. PMID: 32253133; PMCID: PMC7270491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Palan J., Roberts V., Bloch B., Kulkarni A., Bhowal B., Dias J. The use of a virtual learning environment in promoting virtual journal clubs and case-based discussions in trauma and orthopaedic postgraduate medical education: the Leicester experience. J Bone Joint Surg Br. 2012;94:1170–1175. doi: 10.1302/0301-620X.94B9.28780. [DOI] [PubMed] [Google Scholar]
- 13.Iyengar K.P., Jain V.K., Vaish A., Vaishya R., Maini L., Lal H. Post COVID-19: planning strategies to resume orthopaedic surgery -challenges and considerations [published online ahead of print, 2020 May 4] J Clin Orthop Trauma. 2020;11:S291-S295. doi: 10.1016/j.jcot.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blyth P., Stott N.S., Anderson I.A. A simulation-based training system for hip fracture fixation for use within the hospital environment. Injury. 2007;38(10):1197-1203. doi: 10.1016/j.injury.2007.03.031. [DOI] [PubMed] [Google Scholar]
- 15.Gomoll A.H., O’Toole R.V., Czarnecki J., Warner J.J. Surgical experience correlates with performance on a virtual reality simulator for shoulder arthroscopy. Am J Sports Med. 2007;35(6):883-888. doi: 10.1177/0363546506296521. [DOI] [PubMed] [Google Scholar]
- 16.Plancher K.D., Shanmugam J.P., Petterson S.C. The changing face of orthopaedic education: searching for the new reality after COVID-19. Arthrosc Sports Med Rehabil. 2020 Apr 27 doi: 10.1016/j.asmr.2020.04.007. Epub ahead of print. PMID: 32342048; PMCID: PMC7183965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kogan M., Klein S.E., Hannon C.P., Nolte M.T. Orthopaedic education during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28(11):e456–e464. doi: 10.5435/JAAOS-D-20-00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Edigin E., Eseaton P.O., Shaka H., Ojemolon P.E., Asemota I.R., Akuna E. Impact of COVID-19 pandemic on medical postgraduate training in the United States. Med Educ Online. 2020;25(1):1774318. doi: 10.1080/10872981.2020.1774318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mental health and psychosocial considerations during the COVID-19 outbreak. https://www.who.int/docs/default-source/coronaviruse/mental-health-consid erations.pdf Accessed on. [PubMed]
- 20.Saddik B., Hussein A., Sharif-Askari F.S. Increased levels of anxiety among medical and non-medical university students during the COVID-19 pandemic in the United Arab Emirates. MedRxiv. 2020 doi: 10.1101/2020.05.10.20096933. 05.10.20096933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iyengar K., Upadhyaya G.K., Vaishya R., Jain V. COVID-19 and applications of smartphone technology in the current pandemic [published online ahead of print, 2020 May 26] Diabetes Metab Syndr. 2020;14(5):733-737. doi: 10.1016/j.dsx.2020.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iyengar K., Mabrouk A., Jain V.K., Venkatesan A., Vaishya R. Learning opportunities from COVID-19 and future effects on health care system [published online ahead of print, 2020 Jun 20] Diabetes Metab Syndr. 2020;14(5):943–946. doi: 10.1016/j.dsx.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.