At present, SARS-CoV-2 infection rates among UK oncology health care workers are unknown. The COVID-19 Serology in Oncology Staff (CSOS) study is a multicentre UK study investigating oncology staff SARS-CoV-2 exposure following 2 months of the UK national pandemic lockdown. Participants are patient-facing staff working in secondary care oncology departments during the COVID-19 pandemic. Samples are being collected at multiple time points and analysed for SARS-CoV-2 antibodies (blood-based tests) as well as antigens (nasopharyngeal swab test). To increase accuracy, two different methods are being used to detect SARS-CoV-2 IgG antibodies.
The study's primary objective is to measure the prevalence of SARS-CoV-2 IgG antibodies in oncology staff following 2 months of national pandemic lockdown. Secondary outcomes comprise the rate of persistent asymptomatic SARS-CoV-2 antigen positivity over time, the proportion of previously symptomatic and asymptomatic SARS-CoV-2 IgG seropositivity and the proportion of those who do not become antibody-positive following a positive antigen polymerase chain reaction (PCR) result. Here, we summarise the initial results from our pilot study [1].
Pilot Data
Seventy health care workers (from a total of 82 eligible staff; 85.4%) were recruited from the oncology department at the Queen Elizabeth Hospital in Kings Lynn – a 515-bed district general hospital in the East of England serving a population of about 331 000 people. Samples were collected during the first week of June 2020 from both oncology and haemato-oncology staff: antibodies were assayed using a rapid point of care (POC) test (manufacturer reported sensitivity 98.5% and specificity 97.9%), as well as a laboratory-based Luminex test (sensitivity 84% and specificity 100%); antigen status was measured by PCR. Most of the participants were nurses (45/70; 64.3%), followed by doctors (15/70; 21.2%) and patient-facing administrative staff (10/70; 14.3%). Prior symptoms were reported in 25/70 (35.7%) participants, with the highest incidence in nurses (17/45; 37.7%). Symptom duration was similar across all staff groups (median and mean 11 days; range 1–35 days). Eleven of the 25 (44%) who reported previous symptoms reported undergoing PCR nasopharyngeal swab testing when symptomatic: of these, 4/11 (36.4%) tested positive. Only 5/17 (29.4%) previously symptomatic nurses received a prior PCR test (2/5; 40% were positive), in contrast to 4/5 (80%) previously symptomatic doctors (2/4; 50% were positive). The mean time from resolution of reported previous symptoms to the CSOS study sample collection date was 48.4 days (95% confidence interval 39.3–57.46). Most participants (45/70; 64.3%) reported no prior symptoms during the pandemic, which was similar across all groups.
All tested participants were nasopharyngeal swab PCR negative for SARS-CoV-2 antigen. A positive SARS-CoV-2 IgG was detected in 15/70 (21.4%) of participants using the Luminex test, and in 10/70 (14.3%) using the rapid POC test. All participants positive using the rapid POC test were positive using the Luminex test. Due to its ability to detect lower antibody concentration levels (because of the assay type), the results from the Luminex assay were used as the final result. Nurses had the highest percentage of SARS-CoV-2 antibodies (13/45; 28.9%). The percentage prevalence in doctors was less than half that in nurses (2/15; 13.3%), although this difference was not significant (Fischer's exact test P = 0.3). No SARS-CoV-2 antibodies were detected in the receptionists. All participants with a positive nasopharyngeal PCR result prior to the study tested positive for antibodies (4/4; 100%).
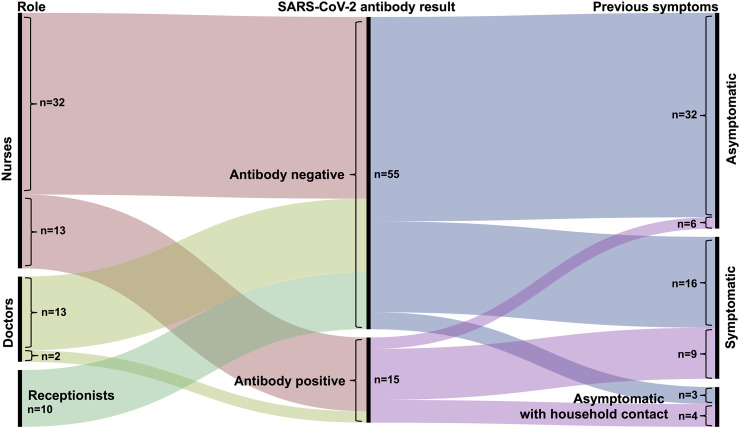
Sixty per cent (9/15) of antibody-positive participants reported previous symptoms, consistent with SARS-CoV-2 infection during the pandemic: a 3.6-fold higher odds than antibody-negative participants (16/55; 29.1%) (Fischer's exact test P = 0.03). Of the total number of previously symptomatic participants, 9/25 (36%) had detectable SARS-CoV-2 antibodies. In those who reported no prior symptoms during the pandemic, 6/45 (13.3%) had antibodies, indicating asymptomatic prior infection. Of seven participants who had no prior symptoms but had been exposed to a suspected infected household member, 4/7 (57.1%) had positive antibodies. See Figure 1 for the results.
Fig 1.
Summary of the relationship between role, previous symptoms and antibody result. All participants were nasopharyngeal swab SARS-COV-2 polymerase chain reaction negative at the time of SARS-COV-2 antibody testing.
Comment
To the best of our knowledge, this is the first UK study specifically investigating SARS-CoV-2 exposure in patient-facing oncology staff who were at work within a secondary care non-surgical oncology department during the COVID-19 pandemic between March and the start of June 2020. Nearly a quarter of oncology staff assessed were SARS-CoV-2 antibody-positive, suggesting a substantial past infection rate, although we found that no participants were SARS-CoV-2 PCR positive at the time of sampling. Although only 6% (9/150) of the patients admitted to the pilot site's oncology in-patient ward during the first 3 months of the UK lockdown were found to be PCR positive, by the nature of the hospital admission process it is possible that some of the infections among staff (both previously symptomatic and asymptomatic) could have arisen from exposure to these patients, especially as earlier on during the pandemic, personal protective equipment was less readily available within the National Health Service.
Nurses were the staff group with the highest percentage of positive SARS-CoV-2 antibodies (double that of doctors, although this difference was not statistically significant at this sample size), which if borne out in a larger sample size, may be the result of a higher frequency and duration of physical contact between nurses and patients by the nature of their work. That none of the receptionist group were antibody positive fits with this hypothesis. A higher proportion of those who reported prior symptoms suggestive of SARS-CoV-2 infection were antibody positive. This emphasises the correlation between symptoms and SARS-CoV-2 serology and highlights the importance of SARS-CoV-2 testing. The National Health Service has now begun to initiate large-scale SARS-CoV-2 testing in staff (using multiple different assays), which will be invaluable in determining exposure rates. Until a vaccine or functional treatment becomes available, serial testing of both oncology staff and patients is likely to be clinically useful, especially when taking into account managing immunocompromised oncology and haemato-oncology patients.
Our finding of a 13.3% previous asymptomatic infection rate (evidenced by positive antibodies and a negative PCR) is higher than reported elsewhere in health care workers [for example: 3/230 (1.3%) in a French study and 11/578 (1.9%) in a Spanish Study] [2,3]. However, it remains unclear whether such antibodies are protective against future repeat SARS-CoV-2 infection. New data in this regard appear promising [4].
Two different antibody assays were used in order to limit the possibility of erroneous results. The rapid POC antibody test was reported by the manufacturer to have high sensitivity and specificity and not to cross-react with the four other main coronavirus types, whereas the Luminex test was able to detect antibodies at a lower concentration level (by the nature of the method). This was evidenced by a previously SARS-CoV-2 PCR-positive participant, who was confirmed to be low level anti-SARS-CoV-2 (IgG)-positive by the Luminex test, but not by the rapid POC method. If we had used the rapid test only, the overall positive antibody percentage would have been 8% lower. Although there is the possibility that some of our study participants were recently SARS-CoV-2 infected and thus were not yet producing SARS-CoV-2 IgG or had fully seroconverted, the mean time from the reported resolution of previous symptoms to the start of the study was 1.5 months. This is something that will be explored with additional sample collection at a later time point.
This study is ongoing and will be collecting further samples at later time points from both our pilot site as well as other National Health Service hospitals. We report these interim results in the expectation that they will be of importance for planning UK national guidance on SARS-CoV-2 testing of patients due to start or having started anticancer non-surgical treatments, as well as the oncology staff treating them.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgement
This study was funded by the Oncology Department Charity Fund at the Queen Elizabeth Hospital Kings Lynn NHS Foundation Trust, the Oncology Department Research Fund at Peterborough City Hospital, North West Anglia NHS Foundation Trust, and the Addenbrooke's Charitable Trust.
References
- 1.Favara D.M., Cooke A., Doffinger R., Houghton S., Budriunaite I., Bossingham S. First results from the UK COVID-19 Serology in Oncology Staff study (CSOS) medRxiv. 2020 doi: 10.1101/2020.06.22.20136838. [DOI] [Google Scholar]
- 2.Solodky M.L., Galvez C., Russias B., Detourbet P., N’Guyen-Bonin V., Herr A.L. Lower detection rates of SARS-COV2 antibodies in cancer patients vs healthcare workers after symptomatic COVID-19. Ann Oncol. 2020 doi: 10.1016/j.annonc.2020.04.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garcia-Basteiro A.L., Moncunill G., Tortajada M., Vidal M., Guinovart C., Jimenez A. Seroprevalence of antibodies against SARS-CoV-2 among health care workers in a large Spanish reference hospital. medRxiv. 2020 doi: 10.1101/2020.04.27.20082289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sekine T., Perez-Potti A., Rivera-Ballesteros O., Strålin K., Gorin J.-B., Olsson A. Robust T cell immunity in convalescent individuals with asymptomatic or mild COVID-19. bioRxiv. 2020 doi: 10.1101/2020.06.29.174888. [DOI] [PMC free article] [PubMed] [Google Scholar]