Abstract
Objective
Describe the early impact of the COVID-19 pandemic on general surgery residency training nationwide.
Design
A 31-question electronic survey was distributed to general surgery program directors. Qualitative data underwent iterative coding analysis. Quantitative data were evaluated with summary statistics and bivariate analyses.
Participants
Eighty-four residency programs (33.6% response rate) with representation across US geographic regions, program affiliations, and sizes.
Results
Widespread changes were observed in the surgical training environment. One hundred percent of programs reduced the number of residents on rounds and 95.2% reduced the size of their in-hospital resident workforce; on average, daytime staffing decreased by nearly half. With telehealth clinics (90.5%) and remote inpatient consults (26.2%), both clinical care and resident didactics (86.9%) were increasingly virtual, with similar impact across all program demographics. Conversely, availability of some wellness initiatives was significantly higher among university programs than independent programs, including childcare (51.2% vs 6.7%), housing (41.9% vs 13.3%), and virtual mental health services (83.7% vs 53.3%).
Conclusions
Changes in clinical care delivery dramatically reduced in face-to-face learning opportunities for surgical trainees during the COVID-19 pandemic. While this effect had equal impact across all program types, sizes, and geographies, the same cannot be said for wellness initiatives. Though all programs initiated some strategies to protect resident health, the disparity between university programs and independent programs may be cause for action.
Key words: graduate medical education, general surgery, coronavirus, COVID-19, resident wellness, virtual education
COMPETENCIES: Systems-Based Practice, Interpersonal and Communication Skills, Patient Care
Introduction
In December 2019, a novel coronavirus (SARS-CoV-2) spread rapidly in China, resulting in a devastating and often lethal disease, termed COVID-19.1 By January 20, 2020, the first confirmed case was documented within the United States.2 Over the following weeks, government officials and healthcare organizations began bracing for what ultimately would be declared a pandemic by the World Health Organization (WHO) on March 11, 2020. The effect on the global medical community was unparalleled and will likely define a generation of medical professionals. However, the impact on surgical residency programs in the United States and their trainees is only beginning to be understood.
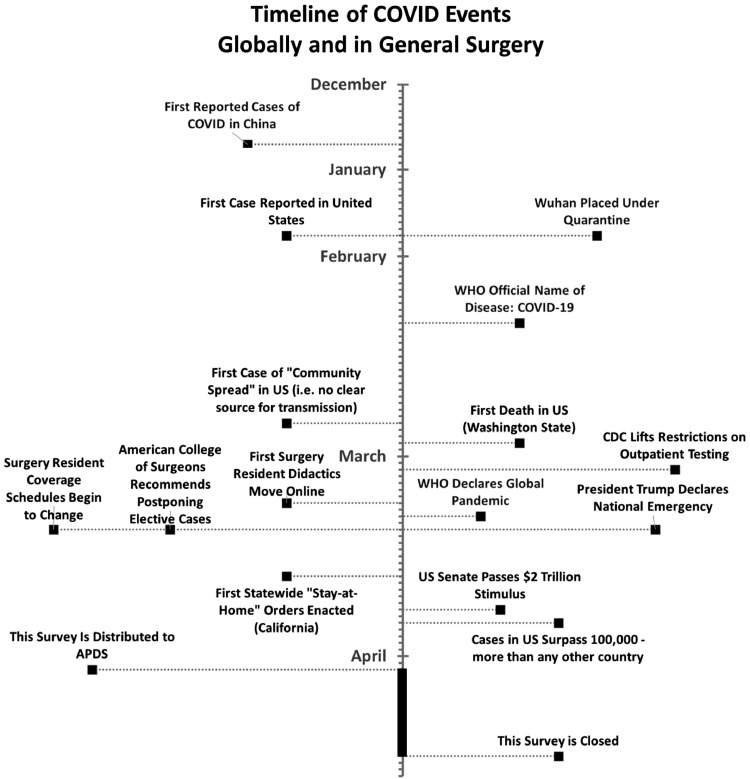
The US surgical community responded to the pandemic swiftly (Fig. 1 ). At the national level, recognizing the need to make limited resources available for the care of COVID-19 patients, the American College of Surgeons (ACS) recommended cancellation of elective surgical cases.3 Individually, hospitals drafted and began to implement response plans including perioperative COVID-19 infection control,4 sourcing Personal Protective Equipment (PPE),5 allocation of ventilators and critical care beds,6 and changing the roles of residents.7
FIGURE 1.
Series of significant pandemic-related events December to mid-April in the surgical community, the United States, and abroad.
Many have opined that the COVID-19 pandemic has had, and will continue to have, a dramatic effect on resident education.8 , 9 On March 13, 2020, the Accreditation Council for Graduate Medical Education (ACMGE) announced relaxations of many common and specialty specific requirements to allow for flexibility in resident allocation in response to the pandemic.10 Likewise, the American Board of Surgery recognized the impact of reduced operative volume on surgical training and addended the resident requirements for graduate case volumes.11
While some general surgery residency programs have published reports of their own responses and restructuring plans,12 , 13 there have been little data regarding the impact of COVID-19 on surgical residency programs nationwide. This study presents a nationwide survey of surgical program directors that aims to elucidate how surgical training programs were impacted during the initial weeks of the pandemic and whether program characteristics such as size, geographic location, and academic affiliations had any bearing on response time and resource allocation. It was hypothesized that during this period, surgical residency programs had already begun to dramatically transform their clinical and educational training paradigms.
Methods
Survey Design and Distribution
A 31-question survey was designed to evaluate several domains of interest in surgical education (didactic education, clinical workflow, occupational health, and resident wellness). Questions were initially designed by study authors based on local experience, then piloted among a group of medical and surgical educators and general surgery residents from within the same geographic region. The survey was then distributed by the Association of Program Directors in Surgery to their program director mailing list. Potential participants, representing approximately 250 nonmilitary programs, received via e-mail an anonymous survey link, administered through the Qualtrics Survey Software platform. An initial invitation was emailed on April 3, 2020 with a follow-up reminder sent on April 7, 2020. The survey remained open for a total period of 14 days. This study received exemption status following Institutional Review Board review (Protocol ID #20000027745).
Quantitative Data Analysis
Data were analyzed using summary statistics, stratified by program affiliation, geographic region, and program size to evaluate for possible differences in pandemic response. For categorical responses, Fisher's exact test or chi-square statistical testing was used, while ANOVA, 2-sample t tests, and paired t tests were employed for most continuous data. Event dates were analyzed using log-rank survival analysis. The specific test used for each comparison is reported alongside results.
Given the potentially sensitive nature of some questions, near complete survey responses (>70% of questions answered) were included in analysis. The variation in denominator for these survey items is reported in the results. Some survey questions asked respondents to identify specific event dates and provided a clickable calendar widget. Analysis required specific calendar dates; however, some responses were found to be contextual (e.g., “three weeks ago”) or unrealistic (e.g., future date/wrong month). Where possible, incomplete data were imputed based on the response. If no date could be easily imputed, the response was excluded from analysis.
Qualitative Data Analysis
Qualitative data from open-ended questions were collated into a list of individual statements and analyzed using an iterative grounded theory approach. Three investigators (EMW, MPS, and ACE) independently analyzed the data using open coding. Their independently developed codes were then compared and honed to develop a consensus codebook. The data were then independently re-coded using the shared codebook. The 3 analyses were then collated into a single unified data set and sorted according to thematic categories.
Results
Program Demographics
Ninety-two participants answered the survey, of which 8 were excluded due to insufficient completion or ineligibility (3 submissions were from nongeneral surgery residency programs). Responses from 84 general surgery programs were included in the analysis, reflecting 33.6% of programs represented by membership in the Association of Program Directors in Surgery. Specific response rates across program demographics are displayed in Table 1 . About half of respondents were from university programs (51.2%, 43/84) and the Northeast (39.3%, 33/84) which was expected given known population demographics. The response rate among independent programs was 55.5% (15/27). There was a visible correlation between type of program and size of resident cohort; the median independent program was reported as 10 to 19 residents, while the median university affiliated program was 20 to 29 residents, and median university program was 40 to 49 residents.
TABLE 1.
Demographics of Programs Responding to Study Survey
| Affiliation | Number of Respondents | Proportion of Respondents | Response Rate |
|---|---|---|---|
| University | 43 | 51.2% | 27.5% (43/156) |
| University affiliated | 26 | 31.0% | 38.8% (26/67) |
| Independent | 15 | 17.9% | 55.5% (15/27) |
| Region | Number of Respondents | Proportion of Respondents | Response Rate |
| Midwest | 24 | 28.6% | 40.7% (24/59) |
| Northeast | 33 | 39.3% | 40.7% (33/81) |
| Pacific | 5 | 6.0% | 19.2% (5/26) |
| Rocky mountain | 1 | 1.2% | 20.0% (1/5) |
| Southeast | 16 | 19.0% | 27.1% (16/59) |
| Southwest | 5 | 6.0% | 25.0% (5/20) |
| Program Size | Number of Respondents | Proportion of Respondents | N/A |
| 10-19 | 17 | 20.2% | |
| 20-29 | 19 | 22.6% | |
| 30-39 | 17 | 20.2% | |
| 40-49 | 16 | 19.0% | |
| 50-59 | 6 | 7.1% | |
| 60+ | 9 | 10.7% | |
| Number of Hospitals | Number of Respondents | Proportion of Respondents | |
| 1 | 8 | 9.5% | |
| 2 | 13 | 15.5% | |
| 3 | 19 | 22.6% | |
| 4 | 17 | 20.2% | |
| 5+ | 27 | 32.1% |
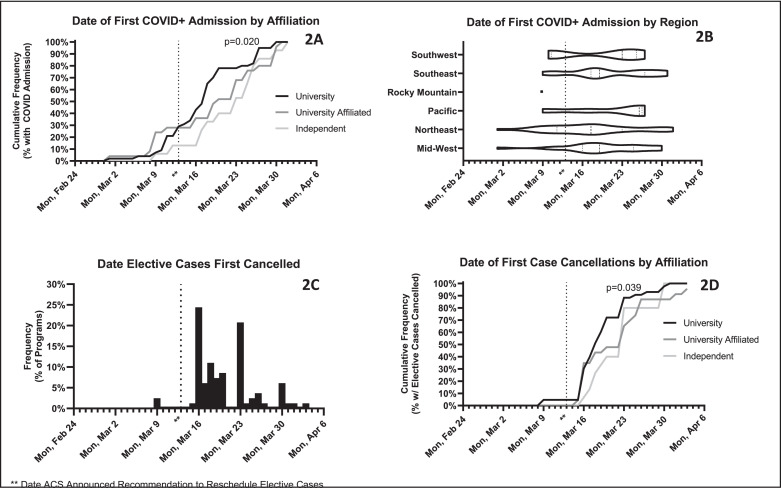
The timing of initial COVID-19 admissions was evaluated as an additional demographic feature among participating programs. All participants reported COVID-19 patients had been admitted to at least one of their training sites. The date of first COVID-19 admission showed a significantly earlier arrival at university programs as compared to university affiliated and independent program (p = 0.020, log-rank test) with no clear geographic pattern (Fig. 2 ).
FIGURE 2.
Dates of COVID events reported at participant institutions. By April 1, all participants reported the presence of COVID patients at their training sites, as demonstrated here by affiliation (A) and geographic region (B). Elective case cancellations are shown as a distribution of the first date seen by each respondent (C) as well as by affiliation (D). The distributions of these events trended toward earlier at university programs compared to university affiliated and independent programs by log-rank survival analysis.
Qualitative Data Analysis
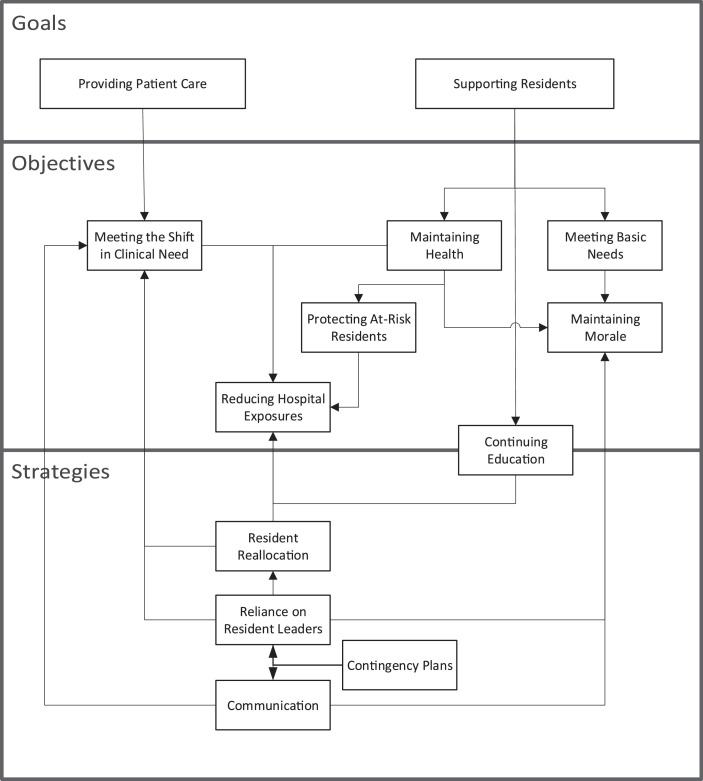
Thematic analysis revealed a model of primary drivers behind initiatives implemented by general surgery residency programs with 2 tertiary goals (Fig. 3 ). First, respondents described the need to provide patient care within a dynamic clinical environment, where changes in surgical patient volume and care delivery necessitated the reallocation of resident roles and responsibilities. Second, they described a mission to protect resident health and wellness; in large part their objective was to limit the direct effects of COVID-19 on the health of their resident workforce, but many expressed a holistic view which also included meeting basic needs outside the hospital and maintaining resident morale.
FIGURE 3.
Thematic analysis of qualitative data revealed as model of primary drivers behind restructuring of general surgery residencies. Changes were made to achieve 2 primary goals, with a number of specific objectives identified as important to these goals. Strategies or resources available to achieve these objectives were also described.
Because these themes were also captured by quantitative survey items, this study predominantly focuses on quantitative results. However, open-ended responses allowed us to capture additional changes that had not been anticipated by our closed-ended questions, so qualitative data are also provided where complementary.
Changes in Clinical Training Environment
On Thursday, March 13, the ACS announced a new recommendation for postponing or cancelling elective cases in order to avoid exposure to patients and reduce use of limited PPE. Prior to this recommendation, only 2.5% of programs (2/80) had adopted such a policy, but that following Monday, March 16, saw the largest single day increase in adoption of this policy when nearly a quarter of institutions began cancelling elective cases (23.8%, 19/80). On March 17, a second set of guidelines detailing how to triage elective cases was released by the ACS, and the following Monday another large wave of adoptions occurred (21.3%, 17/80). At the time of this study, only 1 program reported that elective cases were still being performed at their institution (1.2%, 1/84). Most programs were still performing semielective cases (64.35%, 54/84), and the vast majority were still performing urgent (97.6%, 2/84) and emergent cases (98.8%, 83/84).
In addition to cancelling cases, many other changes in care delivery were observed (Table 2 ). When operative cases did happen, attendings were often operating without resident assistance (44.0%, 37/84). Most respondents (90.5%, 76/84) reported the adoption of telehealth to see clinic patients and 26.2% (22/84) reported that inpatient consults were being seen remotely when possible as well. Hundred percent of respondents reported decreasing the number of providers participating in rounds.
TABLE 2.
Numerous Changes Were Experienced and Implemented by General Surgery Training Programs. These Included Changes to the Clinical Learning Environment (A) As Well As Strategies to Protect Resident Health and Wellness (B).
| A. Clinical Learning Environment | Overall (n = 84*) | University (n = 43*) | University Affiliated (n = 26*) | Independent (n = 15) | p Value |
|---|---|---|---|---|---|
| Attendings operating without resident assistance | 44.0% (37) | 46.5% (20) | 50.0% (13) | 26.7% (4) | 0.326 |
| Reducing number of providers on rounds | 100.0% (84) | 100.0% (43) | 100.0% (26) | 100.0% (15) | NA |
| Conducting inpatient consults remotely | 26.2% (22) | 34.9% (15) | 23.1% (6) | 6.7% (1) | 0.100 |
| Telehealth clinic visits | 90.5% (76) | 93.0% (40) | 84.6% (22) | 93.3% (14) | 0.608 |
| Virtual handoffs | 46.4% (39) | 51.2% (22) | 46.2% (12) | 33.3% (5) | 0.491‡ |
| Conducting EMR work at home | 54.8% (46) | 60.5% (26) | 57.7% (15) | 33.3% (5) | 0.180‡ |
| Clinical schedule changes | |||||
| Reducing size of in-hospital resident workforce | 95.2% (80) | 97.7% (42) | 88.5% (23) | 100.0% (15) | 0.170 |
| Limit residents switching between hospitals | 68.4% (52/76†) | 65.9% (27/41†) | 75.0% (15/20†) | 66.7% (10) | 0.761‡ |
| Postponing/cancelling resident vacations | 36.9% (31) | 41.9% (18) | 34.6% (9) | 26.7% (4) | 0.541 |
| Didactics | |||||
| Cancelled in-person didactics | 92.9% (78) | 95.3% (41) | 88.5% (23) | 93.3% (14) | 0.635 |
| Virtual resident didactics | 86.9% (73) | 90.7% (39) | 76.9% (20) | 93.3% (14) | 0.266 |
| Virtual grand rounds | 83.3% (70) | 88.4% (38) | 73.1% (19) | 86.7% (13) | 0.279 |
| B. Resident Health and Wellness | Overall (n = 84*) | University (n = 43*) | University Affiliated (n = 26*) | Independent (n = 15) | p Value |
|---|---|---|---|---|---|
| COVID-19 testing available | 93.8% (76/81*) | 92.9% (39/42*) | 95.8% (23/24*) | 93.3% (14) | 1.000 |
| Asymptomatic testing available | 2.4% (2) | 2.3% (1) | 3.8% (1) | 0.0% (0) | 1.000 |
| COVID+ residents | 23.5% (19/81*) | 32.6% (14) | 17.4% (4/23*) | 6.7% (1) | 0.101 |
| Prequarantining residents | 46.4% (39) | 55.8% (24) | 30.8% (8) | 46.7% (7) | 0.130‡ |
| Wearing PPE 24/7 | 78.6% (66) | 76.7% (33) | 76.9% (20) | 86.7% (13) | 0.824 |
| Reusing PPE | 82.1% (69) | 79.1% (34) | 84.6% (22) | 86.7% (13) | 0.801 |
| Tracking provider contacts for COVID-suspected patients | 26.2% (22) | 20.9% (9) | 34.6% (9) | 26.7% (4) | 0.455 |
| Wellness resources provided | |||||
| Childcare | 38.1% (32) | 51.2% (22) | 34.6% (9) | 6.7% (1) | 0.006 |
| Housing | 27.4% (23) | 41.9% (18) | 11.5% (3) | 13.3% (2) | 0.011 |
| Additional meal stipends | 29.8% (25) | 27.9% (12) | 26.9% (7) | 40.0% (6) | 0.630‡ |
| Virtual mental health services | 72.6% (61) | 83.7% (36) | 65.4% (17) | 53.3% (8) | 0.046‡ |
| Financial support | 6.0% (5) | 7.0% (3) | 7.7% (2) | 0.0% (0) | 0.702 |
Bold values significance in P values <0.05.
Variations in denominator reflect inclusion of near complete responses.
Hospitals with only 1 clinical site were excluded from this analysis.
p values marked with this superscript are the result of chi-square analyses; all others reflect a Fisher's exact test.
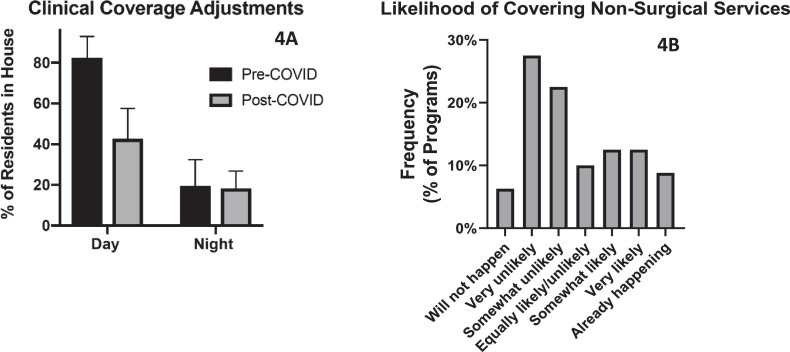
The vast majority of programs (95.2%, 80/84) reported restructuring coverage schedules to reduce the number of residents working in-hospital. On average, the proportion working in-hospital on a typical day decreased by almost half: prior to the pandemic, programs estimated that 82.4% (s.d. 10.5%) of residents would be working in-hospital on a typical day, but as of mid-April, this was reduced to 42.7% (s.d. 14.9%, p < 0.001, paired t test). For in-hospital night coverage, the size of the workforce was essentially unchanged (18.7% ± 11.1% to 18.3% ± 8.5%, p = 0.701, paired t test); however, 51.2% (40/77) had changed the types of coverage shifts (i.e., 24-hour shifts vs night float) and were relying more frequently on a night float system (p = 0.001, Wilcoxon signed-rank test).
Qualitative data provided additional details about how in-hospital coverage was drawn down. Some described pulling “all residents brought back from away rotations” or “only covering essential services (acute care, pediatrics, trauma).” Others described scheduling blocks of several days at a time where residents were kept out of the hospital such as “7 days on, 7 days off, and alternating days/nights” or “each resident does 2, 5-day blocks and then has a 5-day block [off-service].” When outside of the hospital, residents were often expected to work on other “scholarly activities” such as online didactic education or to assist the in-house team with “clerical duties such as telephone follow ups, documentation, [and] ‘seeing’ consults that can be answered remotely.”
The survey also explored whether residents may be re-assigned to nonsurgical services. The majority of programs did not expect surgical residents would be called upon to cover services they would not typically cover (Fig. 4 b); however, 25% of respondents stated it was likely to happen, and 8.3% stated it was already occurring. Qualitative data demonstrated that the reality might be more nuanced. For example, some programs reported “more surgical residents are covering ICU patients under surgical ICU attending.” While this scenario did not explicitly describe residents being re-assigned to, for example, a medicine service, it did represent a change from their prepandemic surgical patient care responsibilities.
FIGURE 4.
Changes to resident clinical coverage included a decrease in size of the in-hospital cohort (A), on average 82.4% (s.d. 10.5%) of residents worked in-hospital during days prepandemic, down to 42.7% (s.d. 14.9%) postpandemic with no significant change to overnight staffing. The expectation that surgical residents would need to cover nontypical service rotations was variable (B).
Also based on qualitative data, the shift in resident responsibilities appeared inconsistent across PGY level. It was apparent from free text responses that many programs were very reliant on senior residents. Some described a shift in administrative responsibilities where “resident leaders, mostly the chiefs, are playing a huge role coordinating schedules and restructuring coverage.” Others described how senior residents shouldered an increased responsibility of care for COVID-19 patients, for example: “senior residents provide a line service for COVID-19 patients” and “limiting OR participation on COVID+ or suspected patients to senior residents (4&5) only.”
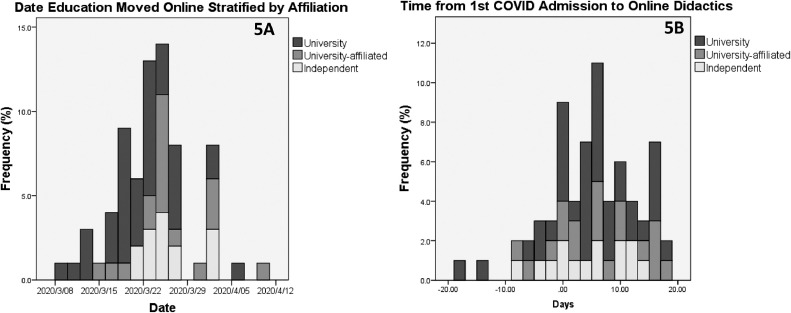
In addition to decreasing in-person clinical time, the pandemic reduced formal face-to-face didactic education time, with 91.7% (77/84) of programs reporting cancelled in-person didactics. Of these, 90.4% (66/77) had converted didactics online (Fig. 5 ). Likewise, 83.3% (70/84) of departments moved Grand Rounds to a virtual platform. Initial analysis showed the timing to start online didactics varied significantly by program affiliation, with university programs reporting their mean first date of online didactics as March 21, while both university affiliated and independent programs started on average 4 days later (p = 0.039, log-rank test). However, adjusting for the timing of first COVID-19 admission, which was disproportionately earlier among university programs, effectively eliminated this difference, with independent programs potentially having a more rapid transition to online didactics (3.857 days, s.d. 7.49) compared to university programs (4.28 days, s.d. 7.74) and university affiliates (3.94 days, s.d. 7.80, p = 0.685, ANOVA).
FIGURE 5.
The majority (86.9%) of programs transitioned resident didactics to a virtual platform. By date, the first programs to do so were university programs (A). However, to assess programs’ response rates in the context of local COVID risk, a comparison of days between when the first COVID patient was admitted and when didactics were moved online showed no trend (B).
Resident Health and Wellness
While many of the changes in clinical volume and scheduling were largely designed to reduce both patient and healthcare exposures, programs also described additional precautions being taken to decrease transmission and protect resident health (Table 2). Most respondents reported policies for mandatory PPE use for the entirety of each clinical shift (78.6%, 66/84), though the majority also had a policy for PPE reuse (82.1%, 69/84). Relatively few institutions implemented any method of documenting which providers had directly cared for COVID-19 positive or suspected patients (26.2%, 22/84) in order to track potential exposures and spread.
Qualitative data revealed even more strategies aimed at protecting resident health, such as “extra [disinfectant solution] for offices,” “UV phone sterilizers for masks and stethoscope parts and phones,” and “increased cleaning of call rooms.” A few programs also described additional precautions to protect residents perceived as particularly high risk. They reported having “completely benched high risk residents (immunosuppressed, pregnant)” and “changed high risk residents to clinic only and moved admin responsibilities to them.”
Care for resident health was not isolated to physical well-being. Some respondents referenced “building on some of SECOND Trial domains,” “talks…about resilience and positive psychology,” hosting a “virtual happy hour,” and developing a “buddy system… to check in with each other.” Quantitatively, the survey asked about some specific wellness services. Providing access to virtual mental health resources was the most widely adopted initiative (72.6%, 61/84); however, the availability of these services was not equal among programs when stratified by affiliation: 83.7% (36/43) of university programs provided this, compared to only 53.3% (8/15) of independent programs (p = 0.046). Additional support resources, including childcare and housing, were also more commonly offered among university programs (Table 2). Additional resources such as financial support or meal stipends were variably provided with no significant difference based on affiliation.
Discussion
As the prevalence of COVID-19 rapidly increased in the United States, the medical community was forced to respond expeditiously. This study depicts the response as of early April 2020 within the surgical education community to the evolving COVID-19 pandemic. By this point, COVID-19 was widespread across the country. Universally, the surgical community was challenged by this new occupational hazard, with every responding program reporting at least 1 COVID-19 admission within their hospitals, and, in most cases, major changes to the surgical training environment.
In light of diminished surgical volume and an effort to reduce COVID-19 exposures, there was a dramatic restructuring of resident clinical teams. This study demonstrated a universal reduction of the number of residents involved in rounds (100% of programs), and a near universal adoption of reduced in-hospital resident teams (95.2% of programs), resulting a decrease of daytime staffing by nearly half. Programs compensated with a rapid adoption of virtual didactics (86.9%); however, in considering the multitude of changes to clinical care delivery—the use of telehealth clinics (90.5%), remote inpatient consults (26.2%), and attendings operating without resident assistance (44.0%)—this study demonstrates a significant decrease in trainee interaction with both attendings and patients, representing a multitude of lost face-to-face learning opportunities.
These changes to the clinical learning environment seemed to be equally shared across all programs regardless of size or university affiliation. However, there was a disproportionate distribution of wellness resources made available to residents, including childcare, housing, and access to virtual mental health services, with increased availability observed at universities compared to independent programs. The nature of this disparity was not immediately obvious. While this may be the result of having close ties with university resources, it should be noted that university programs tend to be larger than independent programs; it may be that large programs have larger resources to draw on, irrespective of university affiliation. Alternatively, having a larger group of residents with inherently more diverse needs may require more resources, whereas smaller programs may be better able to tailor wellness needs to their small group without providing the full range of services queried in this study. In any case, with the effects of the pandemic expected to last for many more months, and the well-documented physical and emotional toll of the COVID-19 pandemic on healthcare workers,8 , 14 , 15 these findings deserve to be addressed at the national level of graduate medical education leadership. Just as the ACS has made access to online education resources available broadly,16 there may be a need for additional wellness resources to be directed toward trainees who are at risk due to either personal or situational circumstances.
Limitations
As with any survey study, data are susceptible to bias. In the midst of a crisis, with a range of competing priorities, it is conceivable that survey participant selection may have been influenced by the crisis itself. Likewise, the data may be subject to response bias, for example: with respect to the query of adherence to the ACS guidelines, it is conceivable that respondents provided answers that reflected their wish to comply rather than their actual functional level of compliance.
At the time this survey was being conducted, it was not yet known which geographic regions would be hardest hit, and the broad geographic data collected here was insufficiently granular to determine whether or not programs were located in what became known as “hot zones.” Future retrospective studies will be necessary to elucidate the longer term effects of the pandemic on surgical education. The authors advocate conducting that work in a way that provides specific local epidemiological context.
An additional potential limitation is that data were not collected from residents themselves regarding their experiences, perspectives, and outcomes. While it was observed that programs are mobilizing resources to support resident health and continue education in a dynamic clinical environment, it provides no insight into the efficacy of such strategies. As the United States reaches a plateau in the number of COVID-19 cases and surgical volumes begin to return to baseline levels, one hopes that efforts to protect the surgical workforce both physically and emotionally will pay dividends moving forward. This will be an important line of inquiry over the coming months, not only to provide ongoing support where it is needed, but as an opportunity to investigate and develop best practices for resident training in the future.
As one respondent commented: “The difficulty with this survey is that things are changing at such a rapid pace, that the answer at an institution one week will be different the next week.” The data from this survey indeed reflect a rapidly changing clinical environment which has affected all surgical trainees and will certainly continue to evolve in the coming months as the surgical community begins to define the “new normal.” With the dramatic decrease in surgical learning opportunities, surgical educators will need to consider how to strategically backfill resident education, or whether the increased time spent out of the hospital completing clinical work and education virtually is sufficient, and potentially even beneficial, for resident education and wellness. These conclusions will all require time, retrospective reflection, and ongoing discussion at both the local and national level.
Acknowledgments
Thank you to members of the Connecticut Chapter of the American College of Surgeons Resident Committee and the Yale School of Medicine Teaching and Learning Center who piloted the survey. We also acknowledge the Association of Program Directors in Surgery for distributing this survey.
References
- 1.Guo Y., Cao Q., Hong Z. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak—an update on the status. Military Med Res. 2020;7:11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holshue M.L., DeBolt C., Lindquist S. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Recommendations for management of elective surgical procedures. American College of Surgeons, 2020. Available at:https://www.facs.org/covid-19/clinical-guidance/elective-surgery. Accessed May 29, 2020.
- 4.Dexter F., Parra M.C., Brown J.R., Loftus R.W. Perioperative COVID-19 defense: an evidence-based approach for optimization of infection control and operating room management. Anesth Analg. 2020;131:37–42. doi: 10.1213/ANE.0000000000004829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Livingston E., Desai A., Berkwits M. Sourcing personal protective equipment during the COVID-19 pandemic. JAMA. 2020 doi: 10.1001/jama.2020.5317. [DOI] [PubMed] [Google Scholar]
- 6.White D.B., Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA. 2020 doi: 10.1001/jama.2020.5046. [published online ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Ross S.W., Lauer C.W., Miles W.S. Maximizing the calm before the storm: tiered surgical response plan for novel coronavirus (COVID-19) J Am Coll Surg. 2020;230:1080–1091. doi: 10.1016/j.jamcollsurg.2020.03.019. .e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ehrlich H., McKenney M., Elkbuli A. Protecting our healthcare workers during the COVID-19 pandemic. Am J Emerg Med. 2020;38:1527–1528. doi: 10.1016/j.ajem.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alvin M.D., George E., Deng F., Warhadpande S., Lee S.I. The impact of COVID-19 on radiology trainees. Radiology. 2020 doi: 10.1148/radiol.2020201222. [published online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.ACGME resident/fellow education and training considerations related to coronavirus (COVID-19). Accreditation Council for Graduate Medical Education, 2020. Available at: https://www.acgme.org/Newsroom/Newsroom-Details/ArticleID/10085/ACGME-Resident-Fellow-Education-and-Training-Considerations-related-to-Coronavirus-COVID-19. Accessed May 29, 2020
- 11.Modifications to Training Requirements. The American Board of Surgery, 2020. Available at: http://www.absurgery.org/default.jsp?news_covid19_trainingreq. Accessed May 29, 2020.
- 12.Nassar A.H., Zern N.K., McIntyre L.K. Emergency restructuring of a general surgery residency program during the coronavirus disease 2019 pandemic: the University of Washington Experience. JAMA Surg. 2020 doi: 10.1001/jamasurg.2020.1219. Published online. [DOI] [PubMed] [Google Scholar]
- 13.Bryan D.S., Benjamin A.J., Schneider A.B., Milner R., Matthews J.B., Roggin K.K. Nimble, together: A training program's response to the COVID-19 pandemic. Ann Surg. 2020 doi: 10.1097/SLA.0000000000003994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Montemurro N. The emotional impact of COVID-19: from medical staff to common people. Brain Behav Immun. 2020;87:23–24. doi: 10.1016/j.bbi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spoorthy M.S., Pratapa S.K., Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic—a review. Asian J Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Project quarantine: surgical education [RAS-ACS Hangouts web site]. 2020. Available at: https://www.facs.org/member-services/ras/hangout. Accessed March 25, 2020.