Key Points
Question
Is the risk factor burden of cardiovascular disease, as assessed by atherosclerotic cardiovascular disease risk score, associated with coronary plaque progression and the development of adverse plaque characteristics?
Findings
In this cohort study of 1005 adult patients from an international multicenter registry who underwent serial coronary computed tomographic angiography, the progression of coronary atherosclerotic plaque volume and the development of adverse plaque characteristics was greater in patients with a high atherosclerotic cardiovascular disease risk score.
Meaning
The study findings suggest that the overall cardiovascular disease risk burden is associated with the progression of coronary atherosclerosis; the progression of fibrofatty plaque and low-attenuation plaque and the development of adverse plaque characteristics appear to be accelerated in patients with a high risk of atherosclerotic cardiovascular disease.
Abstract
Importance
Several studies have reported that the progression of coronary atherosclerosis, as measured by serial coronary computed tomographic (CT) angiography, is associated with the risk of future cardiovascular events. However, the cumulative consequences of multiple risk factors for plaque progression and the development of adverse plaque characteristics have not been well characterized.
Objectives
To examine the association of cardiovascular risk factor burden, as assessed by atherosclerotic cardiovascular disease (ASCVD) risk score, with the progression of coronary atherosclerosis and the development of adverse plaque characteristics.
Design, Setting, and Participants
This cohort study is a subgroup analysis of participant data from the prospective observational Progression of Atherosclerotic Plaque Determined by Computed Tomographic Angiography Imaging (PARADIGM) study, which evaluated the association between serial coronary CT angiography findings and clinical presentation. The PARADIGM international multicenter registry, which includes 13 centers in 7 countries (Brazil, Canada, Germany, Italy, Portugal, South Korea, and the US), was used to identify 1005 adult patients without known coronary artery disease who underwent serial coronary CT angiography scans (median interscan interval, 3.3 years; interquartile range [IQR], 2.6-4.8 years) between December 24, 2003, and December 16, 2015. Based on the 10-year ASCVD risk score, the cardiovascular risk factor burden was classified as low (<7.5%), intermediate (7.5%-20.0%), or high (>20.0%). Data were analyzed from February 8, 2019, to April 17, 2020.
Exposures
Association of baseline ASCVD risk burden with plaque progression.
Main Outcomes and Measures
Noncalcified plaque, calcified plaque, and total plaque volumes (mm3) were measured. Noncalcified plaque was subclassified using predefined Hounsfield unit thresholds for fibrous, fibrofatty, and low-attenuation plaque. The percent atheroma volume (PAV) was defined as plaque volume divided by vessel volume. Adverse plaque characteristics were defined as the presence of positive remodeling, low-attenuation plaque, or spotty calcification.
Results
In total, 1005 patients (mean [SD] age, 60 [8] years; 575 men [57.2%]) were included in the analysis. Of those, 463 patients (46.1%) had a low 10-year ASCVD risk score (low-risk group), 373 patients (37.1%) had an intermediate ASCVD risk score (intermediate-risk group), and 169 patients (16.8%) had a high ASCVD risk score (high-risk group). The annualized progression rate of PAV for total plaque, calcified plaque, and noncalcified plaque was associated with increasing ASCVD risk (r = 0.26 for total plaque, r = 0.23 for calcified plaque, and r = 0.11 for noncalcified plaque; P < .001). The annualized PAV progression of total plaque, calcified plaque, and noncalcified plaque was significantly greater in the high-risk group compared with the low-risk and intermediate-risk groups (for total plaque, 0.99% vs 0.45% and 0.58%, respectively; P < .001; for calcified plaque, 0.61% vs 0.23% and 0.36%; P < .001; and for noncalcified plaque, 0.38%vs 0.22% and 0.23%; P = .01). When further subclassified by noncalcified plaque type, the annualized PAV progression of fibrofatty and low-attenuation plaque was greater in the high-risk group (0.09% and 0.02%, respectively) compared with the low- to intermediate-risk group (n = 836; 0.02% [P = .02] and 0.001% [P = .008], respectively). The interval development of adverse plaque characteristics was greater in the high-risk group compared with the low-risk and intermediate-risk groups (for new positive remodeling, 73 patients [43.2%] vs 151 patients [32.6%] and 133 patients [35.7%], respectively; P = .02; for new low-attenuation plaque, 26 patients [15.4%] vs 44 patients [9.5%] and 35 patients [9.4%]; P = .02; and for new spotty calcification, 37 patients [21.9%] vs 52 patients [11.2%] and 54 patients [14.5%]; P = .002). The progression of noncalcified plaque subclasses and the interval development of adverse plaque characteristics did not significantly differ between the low-risk and intermediate-risk groups.
Conclusions and Relevance
Progression of coronary atherosclerosis occurred across all ASCVD risk groups and was associated with an increase in 10-year ASCVD risk. The progression of fibrofatty and low-attenuation plaques and the development of adverse plaque characteristics was greater in patients with a high risk of ASCVD.
This cohort study analyzes data from the Progression of Atherosclerotic Plaque Determined by Computed Tomographic Angiography Imaging study to explore the association of cardiovascular risk factor burden with progression of coronary atherosclerosis and development of adverse plaque characteristics.
Introduction
Coronary computed tomographic (CT) angiography allows quantitative measurement of multiple components of coronary atherosclerotic plaque and assessment of adverse plaque characteristics.1,2,3,4 In addition, the development and progression of coronary atherosclerotic plaque across the entire coronary tree can be evaluated using serial coronary CT angiography scans.5,6 Serial assessment of coronary artery plaques through coronary CT angiography provides clinical information regarding the progression of disease and the risk of experiencing future adverse cardiovascular events.7,8
Although several studies have reported an association between individual cardiovascular disease (CVD) risk factors and plaque progression,9,10,11,12 the cumulative consequences of multiple risk factors for plaque progression and the development of adverse plaque characteristics have not been well characterized. Current guidelines recommend the application of the 10-year atherosclerotic CVD (ASCVD) risk score,13 a validated model that incorporates age, sex, and traditional CVD risk factors to estimate the likelihood of cardiovascular events over 10 years.14 We aimed to explore the association of CVD risk factor burden, as measured by the 10-year ASCVD risk score, with coronary plaque progression and the development of adverse plaque characteristics in a large international longitudinal cohort using serial coronary CT angiography.
Methods
Study Population
The study population was acquired using data from the Progression of Atherosclerotic Plaque Determined by Computed Tomographic Angiography Imaging (PARADIGM) study. The PARADIGM registry has been previously described.15 In brief, the registry is a prospective international multicenter dynamic observational database designed to evaluate the association between serial coronary CT angiography findings and clinical presentation. Baseline data for the PARADIGM registry represent adult participants who received serial coronary CT angiography scans between December 24, 2003, and December 16, 2015, with follow-up through November 24, 2016. A total of 2252 consecutive adult participants underwent serial coronary CT angiography scans at an interval of 2 or more years at 1 of 13 centers in 7 countries (Brazil, Canada, Germany, Italy, Portugal, South Korea, and the US). Participating medical centers included the Montreal Heart Institute (Montreal, Quebec, Canada); Hospital da Luz (Lisbon, Portugal); the University of California, Los Angeles; the Institute for Research, Hospitalization and Healthcare (IRCCS; Milan, Italy), St.Paul’s Hospital (Vancouver, British Columbia, Canada); the University of Munich (Munich, Germany); Casa de Saúde (São José, Brazil); Severance Cardiovascular Hospital (Seoul, South Korea); Pusan University Hospital (Busan, South Korea); Seoul National University Hospital (Seoul, South Korea); Gangnam Severance Hospital (Seoul, South Korea); Seoul National University Bundang Hospital (Sungnam, South Korea); and Inje University Ilsan Paik Hospital (Goyang, South Korea). The study protocol was approved by the institutional review boards at all participating sites, and patients provided written informed consent. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cohort studies.
Among 2252 consecutive participants, we excluded 754 patients with coronary CT angiography images that were inadequate for quantitative plaque analysis of the entire coronary tree, 282 patients who had a previous coronary revascularization, 133 patients who experienced an adverse cardiovascular event (defined as a myocardial infarction or revascularization) between serial coronary CT angiography scans, and 78 patients for whom the ASCVD risk score could not be calculated. After exclusions, 1005 patients were included in the current analysis. Baseline demographic characteristics, including age, sex, smoking status, and presence of hypertension, diabetes, or dyslipidemia, were collected at the baseline and follow-up coronary CT angiography scans. The 10-year ASCVD risk score, which was calculated using the pooled cohort equation13 based on information obtained at baseline coronary CT angiography, was used to assess CVD risk factor burden. Participants’ risk factor burdens were categorized as low (<7.5%), intermediate (7.5%-20.0%), or high (>20.0%).14
Coronary CT Angiography
All testing, data acquisition, and image postprocessing for coronary CT angiography were performed in accordance with the Society of Cardiovascular Computed Tomography guidelines.16 The coronary CT angiography scans were acquired in all centers using a scanner with 64 or more detector rows. Baseline and follow-up data sets from each center were transferred to an offline workstation for analysis using semiautomated plaque analysis software (QAngio CT Research Edition, version 2.1.9.1; Medis Medical Imaging Systems) with manual correction as needed. Independent blinded readers who were experienced with coronary CT angiography (Core Cardiovascular Training Statement [COCATS] level 3 certification) analyzed all images. Segments were matched between baseline and follow-up coronary CT angiography scans using branch points as landmarks. For longitudinal comparisons of coronary CT angiography images, both baseline and follow-up coronary segments were coregistered using fiduciary landmarks, including distance from ostia or branch vessel takeoffs.
Plaques were qualitatively assessed for adverse characteristics, including positive remodeling, low-attenuation plaque, or spotty calcification. A remodeling index was defined as the maximal lesion vessel diameter divided by the proximal reference vessel diameter. Positive remodeling was defined as a remodeling index greater than 1.1, and low-attenuation plaque was defined as any voxel less than 30 Hounsfield units (HUs) within an individual coronary plaque.7,17 An intralesion calcific plaque less than 3 mm in length that composed less than 90 degrees of the lesion circumference was defined as spotty calcification.17 Development of adverse plaque characteristics was defined as the presence of a new lesion with adverse plaque characteristics on the follow-up coronary CT angiography scan or the development of adverse plaque characteristics from a lesion without adverse plaque characteristics on the baseline coronary CT angiography scan.
Plaque volumes (measured in mm3) of all coronary segments were obtained and summed to generate the total plaque volume on a per-patient level. Atherosclerotic plaque volume was further subclassified by composition, employing predefined intensity cutoff values in HU, including low-attenuation plaque (−30 to 30 HU), fibrofatty plaque (31-130 HU), fibrous plaque (131-350 HU), and calcified plaque (>350 HU).18,19 Percent atheroma volume (PAV) was defined as total plaque volume divided by vessel volume.2 The PAV was also calculated for each subtype of plaque composition. Rapid plaque progression was defined as an increase from baseline total PAV of more than 0.59% per year (the mean value of total PAV progression in the study population) on the follow-up coronary CT angiography scan.
Statistical Analysis
Continuous variables were reported as mean (SD) or median (interquartile range [IQR]) and were compared using a t test or a Wilcoxon rank sum test (as appropriate) for 2-group comparisons and 1-way analysis of variance or a Kruskal-Wallis test (as appropriate) for comparisons of more than 2 groups. Categorical variables were reported as numbers and percentages and compared using the Pearson χ2 test. The association between ASCVD risk score and plaque progression was assessed using linear regression analyses and reported as correlation coefficient (β). All statistical tests were 2-sided and performed on independent or unpaired groups, with P < .05 considered statistically significant. All statistical analyses were performed using Stata software, version 13 (StataCorp LLC). Data were analyzed from February 8, 2019, to April 17, 2020.
Results
Baseline Characteristics
In total, 1005 patients (mean [SD] age, 60 [8] years; 575 men [57.2%]) were included in the analysis. The mean (SD) 10-year ASCVD risk score was 11.3 (9.9). The baseline characteristics of the study population according to 10-year ASCVD risk groups are shown in Table 1. A total of 463 patients (46.1%) had low 10-year ASCVD risk scores (low-risk group), 373 patients (37.1%) had intermediate 10-year ASCVD risk scores (intermediate-risk group), and 169 patients (16.8%) had high 10-year ASCVD risk scores (high-risk group). Patients with high ASCVD risk scores were older (mean [SD] age, 69 [6] years) compared with patients with low risk scores (mean [SD] age, 54 [6] years) and intermediate risk scores (mean [SD] age, 63 [6] years); and a greater proportion of patients with high ASCVD risk scores was male (124 patients [73.4%] vs 204 patients [44.1%] with low risk scores and 247 patients [66.2%] with intermediate-risk scores). Atypical chest pain was present in 694 patients (69.1%) at the baseline coronary CT angiography scan, and clinical symptom status did not significantly differ across ASCVD risk groups (Table 1). The prevalence of hypertension (115 patients [68.0%] in the high-risk group vs 188 patients [40.6%] in the low-risk group and 202 patients [54.2%] in the intermediate-risk group; P < .001), diabetes (84 patients [49.7%] in the high-risk group vs 45 patients [9.7%] in the low-risk group and 69 patients [18.5%] in the intermediate group; P < .001), and current smoking (54 patients [32.0%] in the high-risk group vs 46 patients [9.9%] in the low-risk group and 81 patients [21.7%] in the intermediate-risk group; P < .001) was greater in patients with higher 10-year ASCVD risk scores (Table 1).
Table 1. Baseline Characteristics Based on 10-Year Atherosclerotic Cardiovascular Disease Risk Score.
| Characteristic | No. (%) | P value | |||
|---|---|---|---|---|---|
| All | Low risk | Intermediate risk | High risk | ||
| Total No. | 1005 | 463 | 373 | 169 | |
| Age, mean (SD), y | 60 (8) | 54 (6) | 63 (6) | 69 (6) | <.001 |
| Male sex | 575 (57.2) | 204 (44.1) | 247 (66.2) | 124 (73.4) | <.001 |
| BMI, mean (SD) | 25.3 (3.1) | 24.9 (2.9) | 25.5 (3.1) | 25.7 (3.3) | .009 |
| Clinical symptoms | .26 | ||||
| Asymptomatic | 135 (13.4) | 53 (11.4) | 53 (14.2) | 29 (17.2) | .15 |
| Shortness of breath | 53 (5.3) | 16 (3.5) | 25 (6.7) | 12 (7.1) | .06 |
| Atypical chest pain | 694 (69.1) | 332 (71.7) | 249 (66.8) | 113 (66.9) | .24 |
| Noncardiac chest pain | 80 (8.0) | 41 (8.9) | 31 (8.3) | 8 (4.7) | .26 |
| Typical chest pain | 37 (3.7) | 18 (3.9) | 13 (3.5) | 6 (3.6) | .95 |
| Hypertension | 505 (50.2) | 188 (40.6) | 202 (54.2) | 115 (68.0) | <.001 |
| Diabetes | 198 (19.7) | 45 (9.7) | 69 (18.5) | 84 (49.7) | <.001 |
| Dyslipidemia | 396 (39.4) | 162 (35.0) | 151 (40.5) | 63 (37.3) | .24 |
| Current smoker | 181 (18.0) | 46 (9.9) | 81 (21.7) | 54 (32.0) | <.001 |
| Medications at baseline | |||||
| Aspirin | 350 (34.8) | 117 (25.2) | 153 (41.0) | 80 (47.3) | <.001 |
| β-Blocker | 232 (23.1) | 64 (13.8) | 113 (30.3) | 55 (32.5) | <.001 |
| ACE inhibitor/ARB | 266 (26.5) | 93 (20.1) | 102 (27.3) | 71 (42.0) | <.001 |
| Statin use | 363 (36.1) | 136 (29.4) | 156 (41.8) | 71 (42.0) | <.001 |
| ASCVD risk score | 11.3 (9.9) | 3.9 (1.9) | 12.6 (3.5) | 28.7 (9.6) | <.001 |
Abbreviations: ACE, angiotensin-converting enzyme; ARB, angiotensin II receptor blocker; ASCVD, atherosclerotic cardiovascular disease; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Coronary artery plaques were present in 760 patients (75.6%) at the baseline coronary CT angiography scan (Table 2). At the baseline scan, 300 patients (64.8%) in the low-risk group, 307 patients (82.3%) in the intermediate-risk group, and 153 patients (90.5%) in the high-risk group had coronary artery plaques (P < .001). Quantitative measurements of each type of plaque volume were significantly greater in patients with high 10-year ASCVD risk scores. For example, the median total plaque volume was 105.1 mm3 (IQR, 47.6-228.9 mm3) in the high-risk group compared with 23 mm3 (IQR, 0-85.9 mm3) in the low-risk group and 45.8 mm3 (IQR, 11.1-128.0 mm3) in the intermediate-risk group (P < .001) (Table 2).
Table 2. Baseline Coronary Computed Tomographic Angiography Measures Based on 10-Year Atherosclerotic Cardiovascular Disease Risk Score.
| Measure | No. (%) | ||||
|---|---|---|---|---|---|
| All | Low risk | Intermediate risk | High risk | P value | |
| Total No. | 1005 | 463 | 373 | 169 | |
| Presence of any plaque | 760 (75.6) | 300 (64.8) | 307 (82.3) | 153 (90.5) | <.001 |
| Plaque volume, median (IQR), mm3 | |||||
| Total plaque | 43.1 (3.9-127.0) | 23 (0-85.9) | 45.8 (11.1-128.0) | 105.1 (47.6-228.9) | <.001 |
| Calcified plaque | 5.3 (0-32.6) | 1.2 (0-16.4) | 7.8 (0.1-37.2) | 31.3 (3.8-75.3) | <.001 |
| Noncalcified plaque | 28.8 (1.0-85.9) | 14.8 (0-61.4) | 30.5 (5.9-89.4) | 66.3 (23.8-149.2) | <.001 |
| Fibrous plaque | 20.3 (0.7-56.5) | 10.3 (0-41.6) | 22.3 (4.6-55.8) | 46.3 (20.7-96.3) | <.001 |
| Fibrofatty plaque | 3.5 (0-22.1) | 1.0 (0-17.3) | 4.6 (0.1-19.6) | 11.7 (1.8-34.6) | <.001 |
| Low-attenuation plaque | 0 (0-1.5) | 0 (0-0.8) | 0 (0-1.6) | 0.3 (0-2.8) | <.001 |
| Adverse plaque characteristics | |||||
| Any APC | 688 (68.5) | 260 (56.2) | 280 (75.1) | 148 (87.6) | <.001 |
| Positive remodeling | 662 (65.9) | 250 (54.0) | 268 (71.8) | 144 (85.2) | <.001 |
| Low-attenuation plaque | 213 (21.2) | 88 (19.0) | 76 (20.4) | 49 (29.0) | .02 |
| Spotty calcification | 194 (19.3) | 68 (14.7) | 78 (20.9) | 48 (28.4) | <.001 |
Abbreviations: APC, adverse plaque characteristic; IQR, interquartile range.
The prevalence of any adverse plaque characteristics at the baseline coronary CT angiography scan was 260 patients (56.2%) in the low-risk group, 280 patients (75.1%) in the intermediate-risk group, and 148 patients (87.6%) in the high-risk group (P < .001) (Table 2). The prevalence of positive remodeling, low-attenuation plaque, and spotty calcification was significantly higher in patients with a high ASCVD risk score (144 patients [85.2%], 49 patients [29.0%], and 48 patients [28.4%], respectively) compared with patients with a low ASCVD risk score (250 patients [54.0%], 88 patients [10.0%], and 68 patients [14.7%], respectively) or an intermediate ASCVD risk score (268 patients [71.9%], 76 patients [20.4%], and 78 patients [20.9%], respectively; P < .001 for positive remodeling, P = .02 for low-attenuation plaque, and P < .001 for spotty calcification).
Plaque Progression and ASCVD Risk
The median interval between coronary CT angiography scans was 3.3 years (IQR, 2.6-4.8 years), with no significant difference in interval across ASCVD risk groups (median, 3.3 years [IQR, 2.5-4.8 years] for the low-risk group, 3.4 years [IQR, 2.6-4.8 years] for the intermediate-risk group, and 3.4 years [IQR, 2.7-4.9 years] for the high-risk group; P = .57). The annual progression of PAV for total plaque, calcified plaque, and noncalcified plaque was weakly correlated with ASCVD risk (r = 0.26 for total plaque, 0.23 for calcified plaque, and 0.11 for noncalcified plaque; P < .001) (eFigure in the Supplement). The annualized progression of total plaque, calcified plaque, and noncalcified plaque was significantly greater in the high-risk group compared with the low-risk and intermediate-risk groups (for total plaque, 0.99% vs 0.45% and 0.58%, respectively; P < .001; for calcified plaque, 0.61% vs 0.23% and 0.36%; P < .001; and for noncalcified plaque, 0.38% vs 0.22% and 0.23%; P = .01). The results of linear regression analyses for the association between the annualized PAV progression of total plaque and the ASCVD risk score are shown in Table 3. In the multivariate analysis, the ASCVD risk score was significantly correlated with the annualized PAV progression of total plaque (β = 0.108; SE = 0.238; P < .001) after adjusting for statin use, PAV, and the presence of adverse plaque characteristics at the baseline coronary CT angiography scan.
Table 3. Linear Regression Analysis for the Association of Clinical and Plaque Characteristics With Plaque Progression.
| Variable | Univariate | Multivariate | ||
|---|---|---|---|---|
| β (SE) | P value | β (SE) | P value | |
| Statin use | 0.139 (0.056) | <.001 | 0.012 (0.046) | .67 |
| Diameter stenosis | 0.302 (0.001) | <.001 | 0.006 (0.133) | .84 |
| Baseline PAV | 0.540 (0.409) | <.001 | 0.445 (0.509) | <.001 |
| Positive remodeling | 0.347 (0.054) | <.001 | 0.105 (0.055) | .001 |
| Low-attenuation plaque | 0.228 (0.065) | <.001 | 0.044 (0.059) | .12 |
| Spotty calcification | 0.209 (0.067) | <.001 | 0.005 (0.061) | .86 |
| ASCVD risk score | 0.259 (0.264) | <.001 | 0.108 (0.238) | <.001 |
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; PAV, percent atheroma volume.
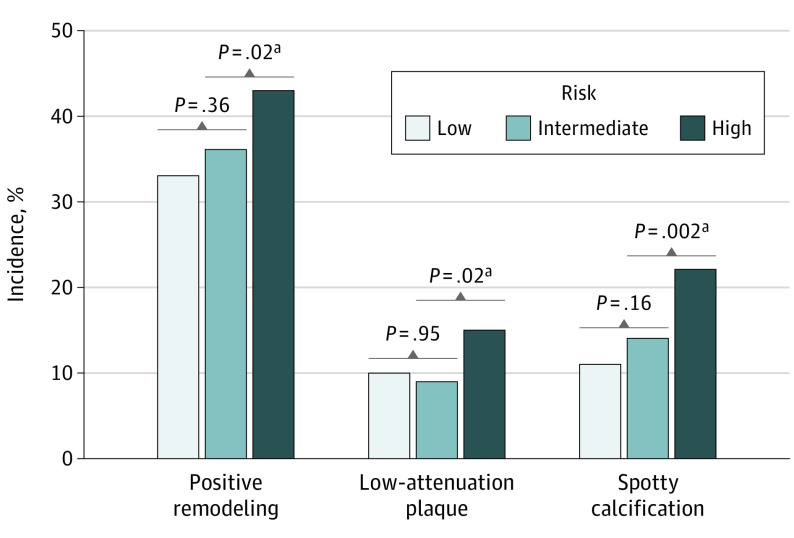
The annualized PAV progression according to plaque components is described in Figure 1 and eTable 1 in the Supplement. The annualized progression of PAV for total plaque and calcified plaque increased as ASCVD risk increased (Figure 1A). The annualized PAV progression of noncalcified plaque was significantly greater in the high-risk group (0.38%) compared with the low- to intermediate-risk group (n = 836; 0.22%; P = .01) (Figure 1A). When we further subclassified noncalcified plaque, the annualized PAV progression of fibrofatty plaque and low-attenuation plaque was significantly greater in the high-risk group (0.09% and 0.02%, respectively) compared with the low- to intermediate-risk group (n = 836; 0.02%; P = .02 and 0.001%; P = .008, respectively) (Figure 1B). No significant differences between the low-risk and intermediate-risk groups were found in the progression of annualized PAV for noncalcified plaque subclasses.
Figure 1. Annualized Plaque Progression .
A, Total, calcified, and noncalcified plaque. B, Noncalcified plaque component. Plaque progression according to atherosclerotic cardiovascular disease risk score. PAV indicates percent atheroma volume.
aComparison between high-risk group vs low- to intermediate-risk group (n = 836).
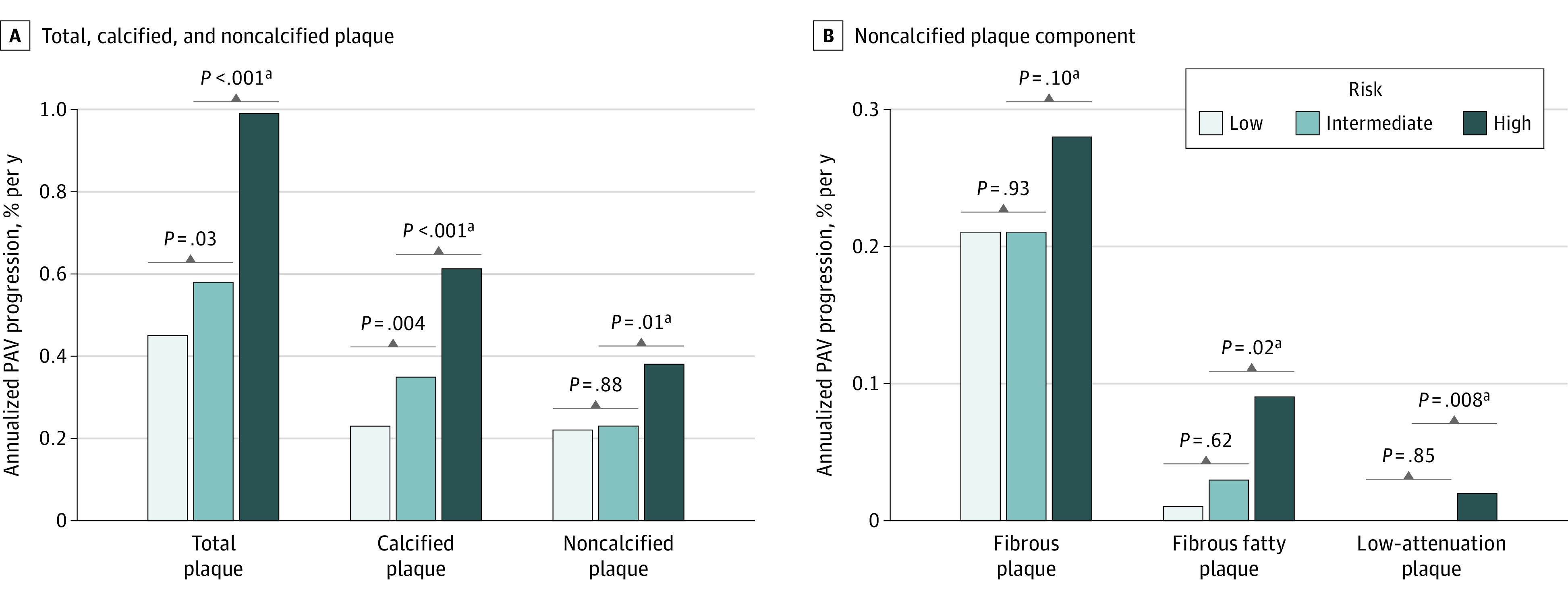
The incidence of new adverse plaque characteristics in the follow-up coronary CT angiography scan according to ASCVD risk groups are described in Figure 2 and eTable 1 in the Supplement. The development of new positive remodeling, new low-attenuation plaque, and new spotty calcification on the follow-up coronary CT angiography scan was greater in the high-risk group (73 patients [43.2%], 26 patients [15.4%], and 37 patients [21.9%] of 169 total patients, respectively) compared with the low-risk group (151 patients [32.6%], 44 patients [9.5%], and 52 patients [11.2%] of 463 total patients, respectively) and the intermediate-risk group (133 patients [35.7%], 35 patients [9.4%], and 54 patients [14.5%] of 373 total patients, respectively; P = .02 for new positive remodeling, P = .02 for new low-attenuation plaque, and P = .002 for new spotty calcification) (Figure 2). The incidence of adverse plaque characteristics did not significantly differ between the low-risk and intermediate-risk groups.
Figure 2. Newly Developed Adverse Plaque Characteristics in Follow-up Coronary Computed Tomographic Angiography .
Adverse plaque characteristics according to atherosclerotic cardiovascular disease risk groups.
aComparison between high-risk group vs low- to intermediate-risk group (n = 836) and intermediate-risk group to low-risk group.
Rapid Plaque Progression
A total of 77 of 169 patients (45.6%) with a high risk of ASCVD experienced rapid plaque progression. Patients with high ASCVD risk and rapid plaque progression were more frequently men (50 of 77 patients [64.9%]) and had more clinical risk factors (59 patients [76.6%] had hypertension, 48 patients [62.3%] had diabetes, and 32 patients [41.6%] were current smokers) compared with those without rapid plaque progression (27 of 92 patients were men [29.3%]; P = .02; 56 patients [60.9%] had hypertension [P = .04], 36 patients [39.1%] had diabetes [P = .003], and 22 patients [23.9%] were current smokers [P = .01]) (eTable 2 in the Supplement). However, age and ASCVD risk score did not differ between patients with rapid progression compared with those without rapid progression (mean [SD] age, 69 [5] years vs 69 [6] years, respectively; P = .99; mean [SD] ASCVD risk score, 29.9 [10.6] vs 27.5 [8.5], respectively; P = .10).
Quantitative measurements of each type of plaque volume were significantly higher in patients with rapid progression (median volume for total plaque, 185.7 mm3 [IQR, 93.9-367.7 mm3]; median volume for calcified plaque, 56.7 mm3 [IQR, 23.4-129.2 mm3]; median volume for noncalcified plaque, 118.5 mm3 [IQR, 52.7-228.4 mm3]) compared with patients without rapid progression (median volume for total plaque, 57.8 mm3 [IQR, 20.5-120.3 mm3]; median volume for calcified plaque, 13.6 mm3 [IQR, 0-43.3 mm3]; median volume for noncalcified plaque, 38.9 mm3 [IQR, 10.4-85.3 mm3]; P < .001 for all comparisons). The prevalence of positive remodeling and low-attenuation plaque at the baseline coronary CT angiography scan was also significantly higher in patients with rapid progression (74 patients [96.1%] and 30 patients [39.0%], respectively) compared with those without rapid progression (70 patients [76.1%] and 19 patients [20.7%], respectively; P < .001 for positive remodeling and P = .009 for low-attenuation plaque) (eTable 2 in the Supplement). Notably, all patients with a high risk of ASCVD and rapid plaque progression had coronary plaques at the baseline coronary CT angiography scan.
Among 2252 patients in the PARADIGM registry, 754 patients were excluded due to image quality. Compared with the 1005 patients in the analysis group, the excluded patients were older (mean [SD] age, 60 [8] years vs 63 [10] years, respectively; P < .001), more frequently male (575 men [57.2%] vs 502 men [66.6%]; P < .001), and had more clinical risk factors (505 patients [50.3%] vs 485 patients [64.3%] had hypertension [P < .001], 198 patients [19.7%] vs 208 patients [27.6%] had diabetes [P < .001], and 376 patients [39.4%] vs 360 patients [47.8%] had dyslipidemia [P < .001]) (eTable 3 in the Supplement).
Discussion
In this study, we found that overall CVD risk burden was associated with the progression of coronary atherosclerosis. A high risk of ASCVD was associated with more rapid progression of coronary atherosclerosis, including calcified plaque, fibrofatty plaque, and low-attenuation plaque volumes, on serial coronary CT angiography scans as measured by the PAV. Furthermore, the incidence of new adverse plaque characteristics increased among patients who had a high risk of ASCVD compared with those who had a low to intermediate risk.
Previous studies of patients who underwent serial coronary CT angiography examinations have reported that clinical factors and laboratory values are associated with the rate of plaque progression.10,11,12 The presence of conventional risk factors, such as diabetes9,10 or high low-density lipoprotein cholesterol levels,11,12 are associated with accelerated plaque progression. Our findings expand on these earlier findings by indicating that patients with a higher CVD risk factor burden, assessed with a validated global risk score, have accelerated plaque progression compared with patients with a lower risk. Most patients with CVD do not present with a single CVD risk factor,20,21 and physicians typically integrate multiple conventional CVD risk factors in clinical practice.14,22 Therefore, the current findings provide practical insights on the development and evolution of atherosclerotic plaques based on a patient’s overall CVD risk burden as assessed by the ASCVD risk score.
A growing body of evidence suggests that noncalcified plaque components are more closely associated with CVD risk than calcified plaque components. The 2018 Incident Coronary Syndromes Identified by Computed Tomography (ICONIC) study observed that patients with acute coronary syndrome associated with coronary plaques had substantially larger noncalcified plaque volumes, most notably low-attenuation plaque volume, before they developed acute coronary syndrome compared with a similar degree of stenotic plaque in patients without acute coronary syndrome, while there was no difference in total plaque and calcified plaque volumes.21 In the current study, we found that although plaque progression occurred in patients with low to intermediate risk, the progression of high-risk noncalcified plaque components, including fibrofatty plaque and low-attenuation plaque volumes, was significantly accelerated in patients with a high CVD risk factor burden compared with patients with a low to intermediate risk factor burden. However, it is unknown whether interventions in these patients were associated with improvements in clinical outcomes.
Because coronary atherosclerosis is a dynamic process, with plaques gaining or losing adverse plaque characteristics over time, the development of adverse plaque characteristics may be an important step from subclinical atherosclerosis to an acute coronary syndrome event.7,23 In a study of 449 patients who underwent serial coronary CT angiography scans, the development of high-risk plaque features (ie, positive remodeling and low-attenuation plaque) was independently associated with acute coronary syndrome.7 In the current study, we observed that a high CVD risk factor burden indicated not only a high prevalence of adverse plaque characteristics at the baseline coronary CT angiography scan but also a significant acceleration in the development of new adverse plaque characteristics.
Although plaque progression has been reported to be associated with an increased risk of developing CVD, methods and thresholds to assess clinically significant plaque progression were inconsistent in previous investigations. Using serial intravascular ultrasound, Nicholls et al24 reported a prognostic significance of per-lesion–based plaque progression at an annualized PAV of more than 1%. With regard to coronary CT angiography, Motoyama et al7 reported prognostic significance of plaque progression for acute coronary syndrome, in which progression was defined as an increase in the degree of stenosis or a remodeling index of more than 1.1. In the current study, the rapid plaque progression was defined as an increase from the baseline total PAV of more than the mean value of total PAV progression in the study population because there is no established threshold for significant plaque progression as assessed by volumetric computed tomographic plaque quantification of the entire coronary tree. Future studies are warranted to establish a clinically relevant threshold of total coronary plaque progression by serial coronary CT angiography assessment.
The current study results indicated that up to two-thirds of low-risk patients (ie, those with <7.5%) had coronary artery plaques at the baseline coronary CT angiography scan. In addition, the progression of noncalcified plaque components and the incidence of high-risk plaque were only modestly different between the low and intermediate ASCVD risk groups. These findings suggest that the arbitrary cutoffs of 5.0% to 7.5% (borderline) or 7.5% to 20.0% (intermediate) of the 10-year ASCVD score are limited in their ability to accurately differentiate the actual ASCVD risk among individuals in the low-risk to intermediate-risk populations. This finding is consistent with the current guideline, which emphasizes the need for risk-enhancing factors to reclassify ASCVD risk in the borderline to intermediate-risk group.14 Noninvasive coronary imaging, such as coronary calcium scans or coronary CT angiography scans, may help to personalize risk assessment and shared decision-making regarding the intensity needed for the preventive strategy.25,26,27
Limitations
This study has several limitations. Although the PARADIGM registry is, to our knowledge, the largest serial coronary CT angiography study to date, there may be unmeasured confounding factors which have implications for the results of this study. We did not have detailed medication information or measures of patient adherence during the interval between scans, which could be used to perform a more refined analysis of the association of statin therapy with plaque progression. The ASCVD risk score was originally validated for 10-year outcomes in asymptomatic patients; therefore, the ASCVD risk score may not completely reflect risk in symptomatic patients who are referred for coronary CT angiography. We included patients who had coronary CT angiography scans with sufficient image quality to allow quantitative assessment of both the baseline and follow-up scans for the purpose of assessing plaque progression in the entire coronary tree. Compared with the excluded patients, the analyzed patients had a lower prevalence of cardiovascular risk factors and medication receipt (eTable 3 in the Supplement). Thus, the potential consequences of selection bias for the generalizability of the findings should be considered. Patients who underwent revascularization before their follow-up coronary CT angiography scan were excluded; thus, the study population consisted mainly of low-risk patients. As a result, the overall clinical event rate in our cohort is low, precluding us from exploring the potential associations between plaque progression, CVD risk factor burden, and adverse CVD outcomes.
Conclusions
The progression of coronary atherosclerosis occurs across all ASCVD risk groups, but the progression of overall PAV increases as the 10-year ASCVD risk score increases. The progression of fibrofatty and low-attenuation plaques and the development of adverse plaque characteristics was greater in patients with a high risk of ASCVD.
eTable 1. Annualized PAV Progression and Development of New APC According to ASCVD Risk Score
eTable 2. Baseline Characteristics of Patients With High ASCVD Risk According to Rapid Plaque Progression
eTable 3. Difference Between Analyzed and Excluded Patients Due to Image Quality
eFigure. Association Between ASCVD Risk Score and Annualized Plaque Progression
References
- 1.Motoyama S, Sarai M, Harigaya H, et al. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol. 2009;54(1):49-57. doi: 10.1016/j.jacc.2009.02.068 [DOI] [PubMed] [Google Scholar]
- 2.Nakazato R, Shalev A, Doh J-H, et al. Aggregate plaque volume by coronary computed tomography angiography is superior and incremental to luminal narrowing for diagnosis of ischemic lesions of intermediate stenosis severity. J Am Coll Cardiol. 2013;62(5):460-467. doi: 10.1016/j.jacc.2013.04.062 [DOI] [PubMed] [Google Scholar]
- 3.Park H-B, Lee BK, Shin S, et al. Clinical feasibility of 3D automated coronary atherosclerotic plaque quantification algorithm on coronary computed tomography angiography: comparison with intravascular ultrasound. Eur Radiol. 2015;25(10):3073-3083. doi: 10.1007/s00330-015-3698-z [DOI] [PubMed] [Google Scholar]
- 4.Dey D, Schepis T, Marwan M, Slomka PJ, Berman DS, Achenbach S. Automated three-dimensional quantification of noncalcified coronary plaque from coronary CT angiography: comparison with intravascular US. Radiology. 2010;257(2):516-522. doi: 10.1148/radiol.10100681 [DOI] [PubMed] [Google Scholar]
- 5.Lee S-E, Park H-B, Xuan D, et al. Consistency of quantitative analysis of coronary computed tomography angiography. J Cardiovasc Comput Tomogr. 2019;13(1):48-54. doi: 10.1016/j.jcct.2018.09.012 [DOI] [PubMed] [Google Scholar]
- 6.Lehman SJ, Schlett CL, Bamberg F, et al. Assessment of coronary plaque progression in coronary computed tomography angiography using a semiquantitative score. JACC Cardiovasc Imaging. 2009;2(11):1262-1270. doi: 10.1016/j.jcmg.2009.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Motoyama S, Ito H, Sarai M, et al. Plaque characterization by coronary computed tomography angiography and the likelihood of acute coronary events in mid-term follow-up. J Am Coll Cardiol. 2015;66(4):337-346. doi: 10.1016/j.jacc.2015.05.069 [DOI] [PubMed] [Google Scholar]
- 8.Yang J, Dou G, Tesche C, et al. Progression of coronary atherosclerotic plaque burden and relationship with adverse cardiovascular event in asymptomatic diabetic patients. BMC Cardiovasc Disord. 2019;19(1):39. doi: 10.1186/s12872-019-1016-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim U, Leipsic JA, Sellers SL, et al. Natural history of diabetic coronary atherosclerosis by quantitative measurement of serial coronary computed tomographic angiography: results of the PARADIGM study. JACC Cardiovasc Imaging. 2018;11(10):1461-1471. doi: 10.1016/j.jcmg.2018.04.009 [DOI] [PubMed] [Google Scholar]
- 10.Nakanishi R, Ceponiene I, Osawa K, et al. Plaque progression assessed by a novel semi-automated quantitative plaque software on coronary computed tomography angiography between diabetes and non-diabetes patients: a propensity–score matching study. Atherosclerosis. 2016;255:73-79. doi: 10.1016/j.atherosclerosis.2016.11.004 [DOI] [PubMed] [Google Scholar]
- 11.Tamarappoo B, Otaki Y, Doris M, et al. Improvement in LDL is associated with decrease in non-calcified plaque volume on coronary CTA as measured by automated quantitative software. J Cardiovasc Comput Tomogr. 2018;12(5):385-390. doi: 10.1016/j.jcct.2018.05.004 [DOI] [PubMed] [Google Scholar]
- 12.Shin S, Park H-B, Chang H-J, et al. Impact of intensive LDL cholesterol lowering on coronary artery atherosclerosis progression: a serial CT angiography study. JACC Cardiovasc Imaging. 2017;10(4):437-446. doi: 10.1016/j.jcmg.2016.04.013 [DOI] [PubMed] [Google Scholar]
- 13.Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25, pt B):2935-2959. doi: 10.1016/j.jacc.2013.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):e285-e350. doi: 10.1016/j.jacc.2018.11.003 [DOI] [PubMed] [Google Scholar]
- 15.Lee SE, Chang HJ, Rizvi A, et al. Rationale and design of the Progression of Atherosclerotic Plaque Determined by Computed Tomographic Angiography Imaging (PARADIGM) registry: a comprehensive exploration of plaque progression and its impact on clinical outcomes from a multicenter serial coronary computed tomographic angiography study. Am Heart J. 2016;182:72-79. doi: 10.1016/j.ahj.2016.09.003 [DOI] [PubMed] [Google Scholar]
- 16.Abbara S, Blanke P, Maroules CD, et al. SCCT guidelines for the performance and acquisition of coronary computed tomographic angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee: endorsed by the North American Society for Cardiovascular Imaging (NASCI). J Cardiovasc Comput Tomogr. 2016;10(6):435-449. doi: 10.1016/j.jcct.2016.10.002 [DOI] [PubMed] [Google Scholar]
- 17.Puchner SB, Liu T, Mayrhofer T, et al. High-risk plaque detected on coronary CT angiography predicts acute coronary syndromes independent of significant stenosis in acute chest pain: results from the ROMICAT-II trial. J Am Coll Cardiol. 2014;64(7):684-692. doi: 10.1016/j.jacc.2014.05.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Achenbach S, Moselewski F, Ropers D, et al. Detection of calcified and noncalcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multidetector spiral computed tomography: a segment-based comparison with intravascular ultrasound. Circulation. 2004;109(1):14-17. doi: 10.1161/01.CIR.0000111517.69230.0F [DOI] [PubMed] [Google Scholar]
- 19.de Graaf MA, Broersen A, Kitslaar PH, et al. Automatic quantification and characterization of coronary atherosclerosis with computed tomography coronary angiography: cross-correlation with intravascular ultrasound virtual histology. Int J Cardiovasc Imaging. 2013;29(5):1177-1190. doi: 10.1007/s10554-013-0194-x [DOI] [PubMed] [Google Scholar]
- 20.Stone GW, Maehara A, Lansky AJ, et al. ; PROSPECT Investigators . A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364(3):226-235. doi: 10.1056/NEJMoa1002358 [DOI] [PubMed] [Google Scholar]
- 21.Chang H-J, Lin FY, Lee S-E, et al. Coronary atherosclerotic precursors of acute coronary syndromes. J Am Coll Cardiol. 2018;71(22):2511-2522. doi: 10.1016/j.jacc.2018.02.079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Neth Heart J. 2008;16(6):191-196. doi: 10.1007/BF03086144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tian J, Dauerman H, Toma C, et al. Prevalence and characteristics of TCFA and degree of coronary artery stenosis: an OCT, IVUS, and angiographic study. J Am Coll Cardiol. 2014;64(7):672-680. doi: 10.1016/j.jacc.2014.05.052 [DOI] [PubMed] [Google Scholar]
- 24.Nicholls SJ, Hsu A, Wolski K, et al. Intravascular ultrasound-derived measures of coronary atherosclerotic plaque burden and clinical outcome. J Am Coll Cardiol. 2010;55(21):2399-2407. doi: 10.1016/j.jacc.2010.02.026 [DOI] [PubMed] [Google Scholar]
- 25.Nasir K, Bittencourt MS, Blaha MJ, et al. Implications of coronary artery calcium testing among statin candidates according to American College of Cardiology/American Heart Association cholesterol management guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2015;66(15):1657-1668. doi: 10.1016/j.jacc.2015.07.066 [DOI] [PubMed] [Google Scholar]
- 26.Han D, Beecy A, Anchouche K, et al. Risk reclassification with coronary computed tomography angiography–visualized nonobstructive coronary artery disease according to 2018 American College of Cardiology/American Heart Association cholesterol guidelines (from the Coronary Computed Tomography Angiography Evaluation for Clinical Outcomes: an International Multicenter Registry [CONFIRM]). Am J Cardiol. 2019;124(9):1397-1405. doi: 10.1016/j.amjcard.2019.07.045 [DOI] [PubMed] [Google Scholar]
- 27.Hwang I-C, Lee H, Yoon YE, et al. Risk stratification of non-obstructive coronary artery disease for guidance of preventive medical therapy. Atherosclerosis. 2019;290:66-73. doi: 10.1016/j.atherosclerosis.2019.09.018 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Annualized PAV Progression and Development of New APC According to ASCVD Risk Score
eTable 2. Baseline Characteristics of Patients With High ASCVD Risk According to Rapid Plaque Progression
eTable 3. Difference Between Analyzed and Excluded Patients Due to Image Quality
eFigure. Association Between ASCVD Risk Score and Annualized Plaque Progression