Abstract
Background.
With increasing emphasis on readmissions as an important quality metric, there is an interest in regionalization of care to high-volume centers. As a result, care of readmitted cardiac surgery patients may be fragmented if readmission occurs at a nonindex hospital. This study characterizes the frequency, risk factors, and outcomes of nonindex hospital readmission after cardiac surgery.
Methods.
In this multicenter, population-based, nationally representative sample, we used weighted 2010–2015 National Readmission Database claims to identify all US adult patients who underwent 2 of the major cardiac surgeries, isolated coronary artery bypass grafting (CABG) or isolated surgical aortic valve replacement (SAVR), during their initial hospitalization. We examined characteristics, predictors, and outcomes after non-index readmission.
Results.
Overall, 1,070,073 procedures were included (844,206 CABG and 225,866 SAVR). Readmission at 30 days was 12.8% for CABG and 14.5% for SAVR. Nonindex readmissions accounted for 23% and 26% at 30 days; these were primarily noncardiac in etiology. The proportion of nonindex readmissions did not change significantly from 2010 to 2015. For CABG and SAVR, in-hospital mortality (adjusted odds ratios of 1.26 and 1.37, respectively) and major complications (odds ratios of 1.17 and 1.25, respectively) were significantly higher during nonindex versus index readmission, even after adjusting for patient risk profile, case mix, and hospital characteristics. Older age, higher income, and increased comorbidity burden were all independent predictors of nonindex readmission.
Conclusions.
A considerable proportion of patients readmitted after cardiac surgery are readmitted to non-index hospitals. This fragmentation of care may account for worse outcomes associated with nonindex readmissions in this complex population.
Hospital readmissions represent a major financial burden and have been shown to compromise quality of care among surgical patients, especially in the immediate postoperative period.1–3 To combat this problem, the Centers for Medicare and Medicaid Services (CMS) instituted the Hospital Readmission Reduction Program (HRRP) in 2012 for select target medical conditions and procedures,4 assigning financial penalties to hospitals with higher than expected readmission rates.5–8 According to the CMS, hospital readmission is any admission to an acute care hospital within 30 days of discharge from the same or another acute care hospital. With promising initial results of the HRRP, the program was expanded to other procedures including coronary artery bypass grafting (CABG) in 2017.9
Although existing efforts across various levels of health care provision (ie, federal, state, hospital) have led to substantial reductions in hospital readmissions, understanding patterns of readmissions, especially in the context of care fragmentation, is of growing interest among policy-makers, clinicians, and patients. Fragmentation in services may lead to adverse care quality as a result of incomplete integration of patient medical records across institutions, inadequate transitions of care, and lack of standardized patient care pathways among the different health care providers and institutions.10–14 Understanding the impact of care fragmentation in the cardiac surgery population is particularly relevant because readmission rates are known to be as high as 20%.15 Furthermore, because cardiovascular care is often regionalized, specialized, and multidisciplinary in nature, readmissions that occur to facilities other than the hospital in which the initial (index) procedure was performed (ie, nonindex readmission) may increase the risk for medical errors, complications, and unnecessary testing, which ultimately increases hospitalization costs.16
Prior work in other high-risk, noncardiac surgical disciplines found nonindex readmissions to be associated with increased rates for morbidity and mortality.17–21 However, limited data exist characterizing the location of readmission among the cardiac surgery population. The introduction of the National Readmissions Database (NRD) has made nationally representative assessment of hospital readmissions possible. The aim of the current study was to characterize the frequency, risk factors, and implications of nonindex readmissions for patients undergoing 2 of the most commonly performed cardiac surgeries, CABG and surgical aortic valve replacement (SAVR), across the United States.
Patients and Methods
Data Source
This population-based, nationally representative study retrospectively analyzed the NRD. This is a unique and powerful database that allows a national assessment of hospital inpatient stays and readmission across for patients of all ages and across all payers and the uninsured population. Although the NRD contains verified patient identifiers to track individuals across hospital admissions within and across a state’s hospitals,22 this database contains completely deidentified data (ie, no social security numbers or patient specific identifiers), using unique patient keys that are tracked by the state. The NRD is drawn from the Agency for Healthcare Research and Quality’s state inpatient databases from 21 geographically dispersed states, with a variety of sizes and population densities, which account for 49.3% of the total US resident population and 49.1% of all US hospitalizations. Thus, the database contains data from approximately 17 million discharges each year, when unweighted, and roughly 36 million discharges, when weighted. Because the NRD is a publicly available, deidentified database, this study was exempt from review by our institutional review board.
Patient Selection
All US adult patients who were admitted for isolated CABG or isolated SAVR between January 1, 2010 and November 31, 2015 were selected from the NRD. Patients who died or underwent concomitant procedures during the index hospital admission were excluded. Those with missing discharge disposition or follow-up data were also excluded from this analysis. Per CMS methodology, all patients discharged alive were considered for readmission regardless of the potential for receipt of postdischarge care (eg, long-term care facility). For patients who had multiple readmissions within 30 days, only the first readmission was included. Transfer to another hospital was not considered as a readmission because it was already accounted for as a nonindex readmission. Patient selection is outlined in the study Consolidated Standards of Reporting Trials diagram (Figure 1).
Figure 1.
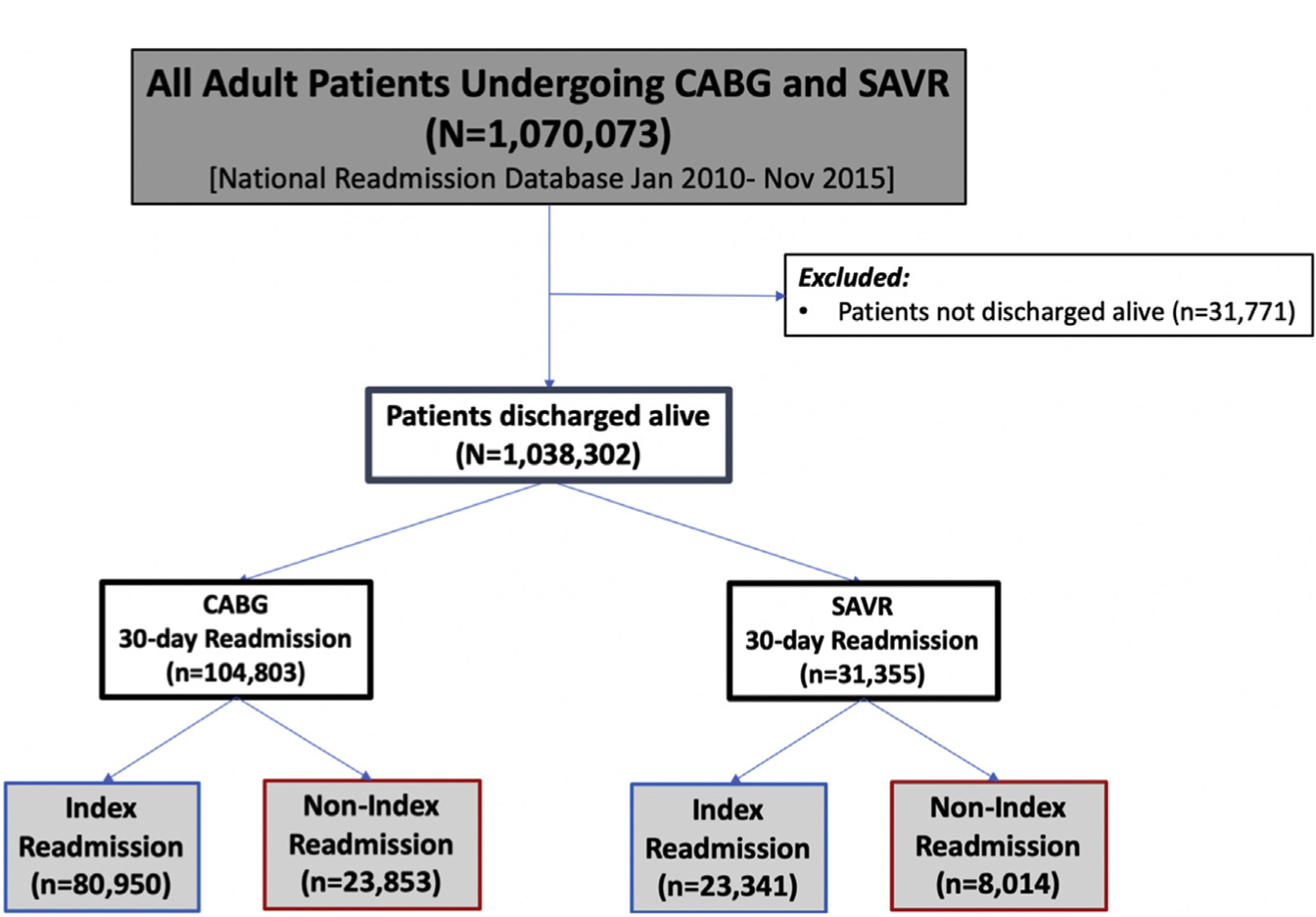
Study Consolidated Standards of Reporting Trials diagram. (CABG, coronary artery bypass grafting; SAVR, surgical aortic valve replacement.)
Variables and Outcomes of Interest
International Classification of Disease, Ninth Edition, Clinical Modifications codes were used to identify patient baseline characteristics, in-hospital procedures (eg, coronary angiography, percutaneous coronary intervention, and mechanical circulatory support), and outcomes (Supplemental Table 1). Primary outcomes were in-hospital mortality, major complications, and annual trends and proportion of index and nonindex readmissions at 30 days for each procedure. Nonindex readmission was defined as readmission to any hospital other than the hospital where the procedure was performed. We defined major complications as a composite of pneumonia, pulmonary embolism, renal failure, cerebrovascular accident, myocardial infarction, cardiac arrest, adult respiratory distress syndrome, sepsis and septic shock.23 Secondary outcome variables were readmission length of stay (LOS) and causes of readmissions. Causes of readmissions were classified as cardiac (eg, heart failure, arrhythmias, conduction disorders) and noncardiac (eg, respiratory, infectious, bleeding, trauma).
Statistical Analysis
Descriptive analyses were performed for 30-day readmission and categorized by index and nonindex readmission hospital status. The NRD time to readmission variable and the primary admission LOS were used to calculate the number of days to readmission.18 Normally distributed continuous variables are expressed as mean and SD and were compared using Student t tests with Levene’s test for homogeneity of variance. Kruskal-Wallis (nonparametric) 1-way analysis of variance was used to compare nonnormally distributed continuous variables. Categorical variables are presented as numbers and percentages and were compared using chi-square or Fisher exact tests, depending on distribution. Survey data analysis tools were employed to generate weighted national estimates and variances that accounted for weighting, clustering of outcomes within hospitals, and sampling variation across strata (region and year).
We performed multivariable regression analysis to determined adjusted outcome differences between the 2 hospital categories. Multivariable logistic regression was also used to identify factors present on the primary admission that were associated with readmission to a nonindex hospital. These risk-adjusted models were calculated using inverse probability of treatment weighting based on calculated propensity scores for a priori defined variables: age, gender, income, operative emergency, Charlson comorbidity index, hospital size, hospital teaching status, and patient residential population. The resultant models, which also accounted for the stratified single-stage cluster sampling design of the NRD, were confirmed not to be significantly different from the complete models (inclusive of all terms shown in Supplemental Table 2) based on a comparison of the ln(likelihoods) for the full and reduced nested models. Quintile regression was used to test differences in LOS. In addition, annual trends and causes of readmission at index versus nonindex readmission were determined. All analyses were conducted using STATA software (version 13.1, StataCorp LP, College Station, TX) with 2-sided P greater than or equal to .05 as the criterion for significance.
Results
Nonindex Readmission After CABG
Overall, 1,070,073 procedures met inclusion criteria, including 844,206 CABG and 225,866 SAVR procedures. Among the CABG patients who were discharged alive (N = 822,257), the 30-day readmission rate was 12.7% (104,803 patients). We also observed an overall decreasing trend for 30-day readmissions, which was more pronounced after the implementation of HRRP policies in 2012 (Figure 2). Although the proportion of nonindex readmissions at 30 days was considerable (22.7%) and increased at 90 days (relative increase of 12.3%), they remained relatively unchanged over time +(Figure 3). Furthermore, more than half of these nonindex readmissions (53.1%) were because of noncardiac causes (53.1%), primarily due to respiratory etiologies (17.3%) (Table 1).
Figure 2.
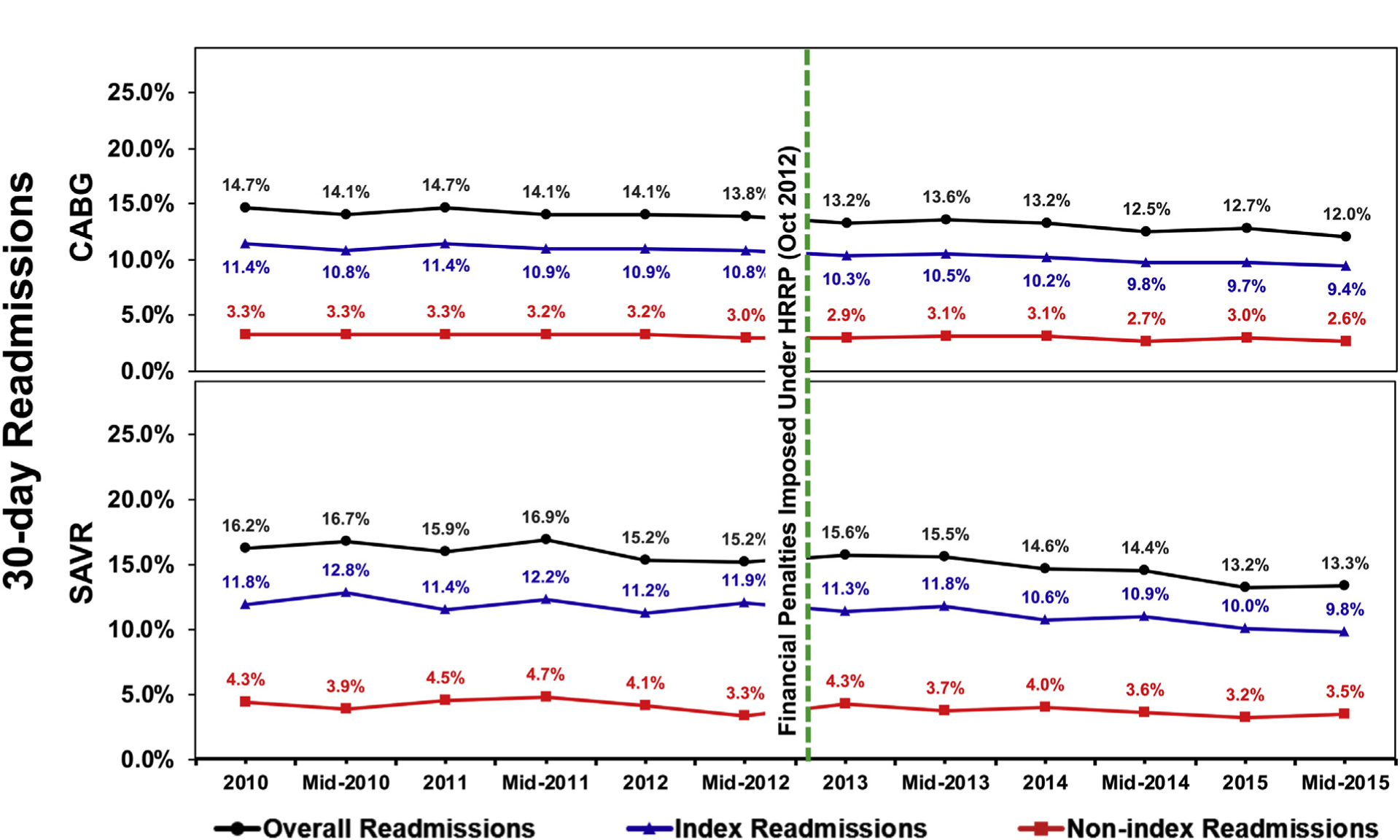
Temporal trends in overall, index, and nonindex 30-day readmission rates after coronary artery bypass grafting (CABG) and surgical aortic valve replacement (SAVR). Green dashed line depicts timing of financial penalties imposed under Hospital Readmission Reduction Program (HRRP).
Figure 3.
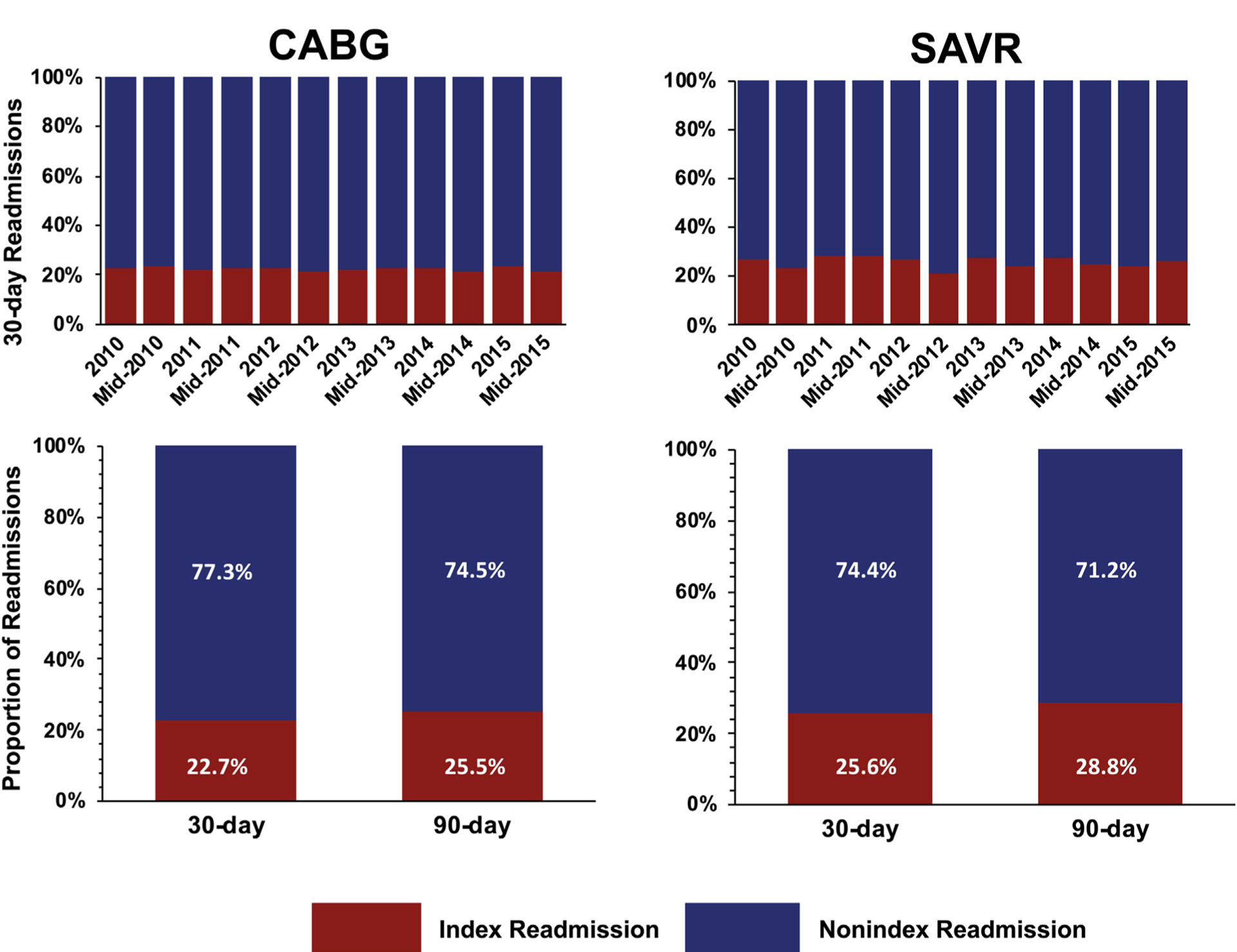
Temporal trends and changes in proportion of index versus nonindex readmission for coronary artery bypass grafting (CABG) and surgical aortic valve replacement (SAVR).
Table 1.
Major Causes of Readmission at Nonindex Versus Index Hospital at 30 d After Coronary Artery Bypass Grafting: Nationally Weighted Resultsa
| Cause of Readmission | Nonindex Readmission at 30 d (n = 23,853) | Index Readmission at 30 d (n = 80,950) | P |
|---|---|---|---|
| Cardiac | 7013 (29.4%) | 22,504 (27.8%) | .031 |
| Heart failure | 3077 (12.9%) | 7852 (9.7%) | <.001 |
| Arrhythmias | 1455 (6.1%) | 5262 (6.5%) | .303 |
| Conduction disorders | 24 (0.1%) | 162 (0.2%) | .206 |
| Valve disorders | 143 (0.6%) | 567 (0.7%) | .183 |
| Hypertension | 48 (0.2%) | 162 (0.2%) | .519 |
| Pericarditis | 119 (0.5%) | 1457 (1.8%) | <.001 |
| Coronary artery disease | 477 (2.0%) | 1538 (1.9%) | .589 |
| Acute myocardial infarction | 358 (1.5%) | 1781 (2.2%) | .002 |
| Chest pain | 763 (3.2%) | 1943 (2.4%) | <.001 |
| Syncope | 215 (0.9%) | 648 (0.8%) | .481 |
| Other | 310 (1.3%) | 1295 (1.6%) | .113 |
| Noncardiac | 12,666 (53.1%) | 46,303 (57.2%) | <.001 |
| Respiratory | 4127 (17.3%) | 13,114 (16.2%) | .054 |
| Infectious | 2719 (11.4%) | 14,004 (17.3%) | <.001 |
| Bleeding | 668 (2.8%) | 2105 (2.6%) | .434 |
| Peripheral vascular disease | 883 (3.7%) | 5343 (6.6%) | <.001 |
| Renal/genitourinary | 644 (2.7%) | 2105 (2.6%) | .653 |
| Gastrointestinal | 859 (3.6%) | 2509 (3.1%) | .032 |
| Transient ischemic attack/stroke | 572 (2.4%) | 1781 (2.2%) | .082 |
| Trauma | 191 (0.8%) | 486 (0.6%) | .015 |
| Endocrine/metabolic | 787 (3.3%) | 2,024 (2.5%) | .001 |
| Neuropsychiatric | 406 (1.7%) | 971 (1.2%) | .011 |
| Hematological/neoplasm | 310 (1.3%) | 729 (0.9%) | .001 |
| Other | 453 (1.9%) | 1214 (1.5%) | .044 |
Tabulated results are based on primary diagnosis codes on readmission. Codes are presented in Supplemental Table 1. Two-sided P values were taken from chi-square tests.
Compared with patients readmitted to index hospitals after CABG, those readmitted to nonindex hospitals were significantly older, had higher burden of comorbidities, and had a higher tendency for nonhome discharge after the initial hospitalization (all P < .001) (Supplemental Table 2).
In-hospital mortality (3% versus 2.4%; adjusted odds ratio [AOR] = 1.26; 95% confidence interval [CI], 1.07–1.50) and major complications (41.8% versus 37.8%; AOR = 1.17; 95% CI, 1.11–1.24) were significantly higher during nonindex readmission (both P < .001) (Table 2). On multivariable analysis, factors more likely to be associated with 30-day nonindex readmission were older age (AOR = 1.43 for age 75–84 years; AOR = 1.48 for age > 84 years), higher income (AOR = 1.21), living in rural or suburban areas (AOR =1.22), higher comorbidity scores (AOR = 1.50), and metropolitan teaching status of the hospital (AOR = 1.19) (Table 3).
Table 2.
Outcome Differences During Nonindex Versus Index 30-d Readmission After Coronary Artery Bypass Grafting: Nationally Weighted Resultsa
| Mortality | 716 (3.0%) | 1943 (2.4%) | 1.27 (1.07–1.50) | 1.26 (1.07–1.49) |
| Major complication(s) | 9971 (41.8%) | 30,599 (37.8%) | 1.18 (1.11–1.25) | 1.17 (1.11–1.25) |
| In-hospital outcome(s) | ||||
| Complete heart block | 95 (0.4%) | 405 (0.5%) | 0.85 (0.52–1.37) | 0.86 (0.54–1.39) |
| Pacemaker placement | 167 (0.7%) | 729 (0.9%) | 0.70 (0.50–0.98) | 0.70 (0.50–0.97) |
| TIA/stroke | 1431 (6.0%) | 4452 (5.5%) | 1.10 (0.97–1.24) | 1.09 (0.97–1.24) |
| Acute myocardial infarction | 2528 (10.6%) | 10,362 (12.8%) | 0.81 (0.73–0.89) | 0.81 (0.73–0.90) |
| Cardiac arrest | 334 (1.4%) | 890 (1.1%) | 1.25 (0.98–1.59) | 1.23 (0.96–1.57) |
| Acute kidney injury | 3960 (16.6%) | 13,842 (17.1%) | 0.97 (0.89–1.05) | 0.96 (0.89–1.04) |
| Major bleeding | 143 (0.6%) | 324 (0.4%) | 1.47 (1.02–2.11) | 1.47 (1.02–2.11) |
| Vascular complications | 72 (0.3%) | 324 (0.4%) | 0.81 (0.50–1.32) | 0.80 (0.49–1.32) |
| Further readmissions required | 10,471 (43.9%) | 32,137 (39.7%) | 1.18 (1.12–1.25) | 1.18 (1.12–1.25) |
| Readmission length of stay, d | ||||
| 50th percentileb | 4 | 5 | +1.00 (+0.80 to +1.20) | +1.00 (+0.76 to +1.24) |
| 75th percentileb | 6 | 7 | +2.00 (+1.50 to +2.50) | +2.00 (+1.70 to +2.30) |
Risk-adjusted models were calculated using inverse probability of treatment weighting based on calculated propensity scores for a priori defined: age, gender, income, resident, operative emergency, Charlson Comorbidity Index, hospital size, hospital teaching status, patient residential population, hypertension, heart failure, and prior TIA/stroke. Major complications were defined to include pneumonia, pulmonary embolism, renal failure, cardiovascular accident, myocardial infarction, cardiac arrest, acute respiratory distress syndrome, sepsis, and severe sepsis.
Results of quantile regression showing the differences in length of stay at the indicated percentile.
CI, confidence interval; OR, odds ratio; TIA, transient ischemic attack.
Table 3.
Independent Predictors of Nonindex Hospital Versus Index Hospital 30-d Readmission After CABG and SAVR: Nationally Weighted Resultsa
| Categorical age, y | ||
| 18–44 | 1.00 (reference) | 1.00 (reference) |
| 45–54 | 1.13 (0.92–1.39) | 1.09 (0.84–1.43) |
| 55–64 | 1.18 (0.97–1.43) | 1.34 (1.03–1.74) |
| 65–74 | 1.31 (1.08–1.59) | 1.45 (1.14–1.84) |
| 75–84 | 1.43 (1.17–1.75) | 1.85 (1.44–2.38) |
| >84 | 1.48 (1.17–1.88) | 2.16 (1.65–2.85) |
| Female | 1.00 (0.94–1.06) | 1.11 (1.00–1.24) |
| Median income quartile | ||
| Ql (lowest) | 1.00 (reference) | 1.00 (reference) |
| Q2 | 1.11 (1.01–1.21) | 1.17 (1.00–1.37) |
| Q3 | 1.17 (1.07–1.29) | 1.15 (0.98–1.35) |
| Q4 (highest) | 1.21 (1.08–1.36) | 1.26 (1.06–1.48) |
| Patient residential population | ||
| Urban, metro area ≥ 1 million | 1.00 (reference) | 1.00 (reference) |
| Suburban, metro area ≥ 1million | 1.22 (1.15–1.28) | 1.15 (0.96–1.36) |
| 250,000–999,999 | 0.80 (0.75–0.85) | 0.91 (0.76–1.08) |
| <250,000 | 1.28 (1.20–1.36) | 1.12 (0.88–1.43) |
| Operative urgency | ||
| Emergent/urgent | 1.00 (reference) | 1.00 (reference) |
| Elective | 0.93 (0.87–1.01) | 1.13 (1.02–1.27) |
| Charlson Comorbidity Index | ||
| 0 (lowest) | 1.00 (reference) | 1.00 (reference) |
| 1 | 1.05 (0.96–1.16) | 1.07 (0.93–1.24) |
| 2 | 1.15 (1.04–1.26) | 1.13 (0.96–1.33) |
| 3 | 1.18 (1.06–1.31) | 1.11 (0.94–1.32) |
| 4 | 1.31 (1.17–1.47) | 1.28 (1.04–1.59) |
| ≥5 (highest) | 1.50 (1.33–1.69) | 1.51 (1.17–1.93) |
| Hospital bed size | ||
| Small | 1.00 (reference) | 1.00 (reference) |
| Medium | 0.66 (0.53–0.87) | 0.71 (0.55–0.90) |
| Large | 0.70 (0.57–0.86) | 0.78 (0.64–0.95) |
| Hospital teaching status | ||
| Metropolitan nonteaching | 1.00 (reference) | 1.00 (reference) |
| Metropolitan teaching | 1.19 (1.07–1.32) | 1.43 (1.24–1.65) |
| Nonmetropolitan hospital | 0.26 (0.20–0.34) | 0.46 (0.27–0.78) |
| Patient residential population | ||
| Urban, metro area ≥1 million | 1.00 (reference) | 1.00 (reference) |
| Suburban, metro area ≥1 | 1.20 (1.06–1.36) | 1.15 (0.96–1.36) |
| million | ||
| 250,000–999,999 | 0.74 (0.64–0.84) | 0.90 (0.75–1.08) |
| <250,000 | 0.83 (0.70–0.99) | 1.12 (0.88–1.43) |
| Specific comorbidities | ||
| Hypertension | 1.21 (0.83–1.77) | 1.03 (0.56–1.90) |
| Heart failure | 0.84 (0.51–1.38) | 1.01 (0.67–1.52) |
| Prior transient ischemic attack/stroke | 1.23 (1.13–1.35) | 1.21 (1.01–1.45) |
Risk-adjusted model was calculated using inverse probability of treatment weighting based on calculated propensity scores for a priori defined age, gender, income, operative emergency, CCI, hospital size, hospital teaching status, and patient residential population. The resultant model was confirmed not to be significantly different from the complete models (inclusive of all terms shown in Supplemental Table 1) based on comparison of the ln(likelihoods) for the full and reduced nested models.
CABG, coronary artery bypass grafting; CI, confidence interval; OR, odds ratio; Q, quartile; SAVR, surgical aortic valve replacement.
Nonindex Readmission After SAVR
Among the 31,355 SAVR patients who were readmitted, 8,014 (25.6%) were readmitted to a non-index hospital, primarily for noncardiac causes (Supplemental Table 3). This proportion increased to 28.8% at 90 days (relative increase of +12.5%). Like CABG, trends in 30-day readmissions for SAVR decreased but the proportion of nonindex readmissions remained relatively stable over time (Figures 2, 3). Similarly, patients readmitted to nonindex hospitals were older with greater comorbidity (Supplemental Table 4) and their readmission was associated with higher risk-adjusted odds of mortality (AOR = 1.37; 95% CI, 1.06–1.77) and major complications (AOR = 1.25; 95% CI, 1.13–1.39). Predictors of nonindex hospital readmission were similar to those after CABG (Table 3).
Comment
Understanding the implications of location of short-term readmissions after cardiac surgery is relevant in the current era of HRRP and regionalization of complex cardiac surgery. In this large, nationally representative, contemporary, multicenter analysis of over 1 million index procedures, approximately one quarter of readmissions after cardiac surgery were to hospital systems other than the hospital in which the initial procedure was performed (no-index readmission). Despite longitudinal improvements in total annual readmissions under the HRRP, the proportion of nonindex readmissions has remained stagnant. Most nonindex readmissions were due to noncardiac etiologies. Risk-adjusted in-hospital mortality and rates of major complications were consistently worse during nonindex readmissions across both targeted (ie, CABG) and nontargeted procedures (ie, SAVR) under the HRRP, even after risk adjustment. The HRRP for CABG was installed in 2017, after the study period of this analysis, which may not have influenced the outcome. Nonetheless, this study comprehensively highlighted the persistence of care fragmentation after cardiac surgery and calls for concerted efforts to identify the mechanisms to decrease the potential adverse implications of these nonindex readmissions.
In recent years, an increasing number of studies have examined the frequency and impact of nonindex readmission after surgery. Although all of these studies have been in noncardiac surgery, 2 consistent theme emerged. First, a considerable proportion of patients are readmitted to nonindex hospitals after discharge. Second, these patients tend to have worse morbidity and mortality leading to higher hospitalization costs, readmission LOS, and, in some cases, worse quality of care.14,17–21,24,25 Zafar and colleagues18 found that nonindex readmissions were associated with 27% higher odds of morbidity and 31% higher odds of mortality compared with readmissions to index hospitals after major cancer surgery. Consistent with these previous experiences, we found that both CABG and SAVR had higher odds of mortality and major complication during nonindex readmission compared with index readmission.
We observed a decreasing trend in 30-day readmission rates across all procedures between 2010 and 2015. This finding is encouraging, but trends appeared to be driven by longitudinal reductions in readmissions to index facilities; the proportion of nonindex readmission was unchanged over the study period for both CABG and SAVR. Nonetheless, the proportion of nonindex readmission was still substantial at 30 days and considerably increased at 90 days for both CABG and SAVR. This suggest that near-term issues were more likely to be managed by the index hospital system as opposed to late-presenting complications from medical issues. Furthermore, index hospitals where cardiac procedures are performed tend to be large academic centers in urban communities. These hospitals were found to be more sensitive to the effects of HRRP overall and may already have instituted global measures to reduce all readmissions, especially because these are closely tied to reimbursement claims.26 This is consistent with previous literature on the HRRP, which suggests a possible spillover effect in which readmissions of nontarget conditions also declined owing to hospital-wide efforts to reduce both index and nonindex readmissions.7,8
This study has important practice implications. First, it appeared that patient-related factors (eg, age, medical complexity, insurance status) predicted the likelihood of nonindex readmission after cardiac surgery. However, we also suspect that socioeconomic predilection may have had a notable role in influencing the pattern of readmission. For instance, higher incomes and living in rural or suburban areas appeared to increase the likelihood of nonindex readmissions. Second, most readmissions to nonindex hospitals resulted from to noncardiac etiologies, specifically respiratory and infectious causes, which emphasizes the need to establish best practices to address comprehensive aspects of perioperative care through a multidisciplinary team approach. Some of these readmissions may be preventable by investing in adequate home health, encouraging the use of visiting nurse services, and instituting routine home monitoring of postoperative patients through either Web-based applications or virtual visits. Recent studies on the use of enhanced recovery after surgery pathways have been promising and should be encouraged.27 Enhancing transitions of care from inpatient to outpatient settings and improving overall communication systems could also help reduce negative outcomes associated with nonindex readmission. Most important, these data call for more integrated cardiac surgery systems of care in which readmissions are triaged based on severity of illness, care needs, and local capacities. To date, there appears to be a mismatch in patient profile and readmission location, because older and sicker patients are more frequently readmitted to nonindex hospitals. Improved interhospital communication through a hub-and-spoke model may be especially important for complex cardiac surgery. Our findings provide an important framework to help understand the realities of existing care fragmentation, because there is growing interest in regionalization of care for complicated patients in the context of HRRP.
Limitations
This analysis has several limitations. First, these administrative data do not contain the granularity of data required to make inferences about specific surgical techniques or causes of readmission. Irregularities in coding practices may introduce some uncertainty over time. Despite the strengths of the database, it may not capture all readmissions. Thus, our overall assumptions and findings may be greatly overestimated. Second, we were unable to confirm affiliations between index and nonindex hospitals, which would reduce some elements of fragmentation of health care. Hospital volume was unavailable in the recent NRD version, and hence the impact of hospital volume in relation to index versus nonindex readmissions could not be elucidated. Likewise, we were unable to delineate reasons for hospital transfers. Finally, we could not examine long-term outcomes or the impact of patients who were discharged to extended care facilities beyond the follow-up period. These are different yet important questions to address and warrant additional studies.
Conclusion
A major proportion of patients undergoing isolated CABG or SAVR are readmitted to nonindex hospitals. This fragmentation of care may account for worse outcomes associated with nonindex readmissions in this complex population, although medical complexity and socioeconomic predilection may have had a large role in influencing outcomes. Nonindex readmissions after cardiac surgery represent an enduring, residual target for future health policies to reduce health care fragmentation.
Supplementary Material
Acknowledgments
Dr Zogg is supported by NIH Medical Scientist Training Program Training Grant T32GM007205. Dr Vaduganathan is supported by the KL2/Catalyst Medical Research Investigator Training award from Harvard Catalyst (National Institutes of Health/National Center for Advancing Translational Sciences Award UL 1TR002541) and participates on clinical end point committees for studies sponsored by Novartis and the National Institutes of Health. Dr Kaneko is a speaker for Edwards Life Sciences, Medtronic, Abbott and Baylis Medical and is a consultant for 4C Medical.
Footnotes
Presented at the Poster Session of the Fifty-fifth Annual Meeting of The Society of Thoracic Surgeons, San Diego, CA, Jan 26–29, 2019.
Dr Vaduganathan discloses a financial relationship with Amgen, AstraZeneca, Bayer AG, Novartis, and Baxter Healthcare; Dr Kaneko with Edwards Life Sciences and Medtronic.
References
- 1.Lucas DJ, Pawlik TM. Readmission after surgery. Adv Surg. 2014;48:185–199. [DOI] [PubMed] [Google Scholar]
- 2.Mao J, Redberg RF, Carroll JD, et al. Association between hospital surgical aortic valve replacement volume and transcatheter aortic valve replacement outcomes. JAMA Cardiol. 2018;3:1070–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kolte D, Khera S, Sardar MR, et al. Thirty-day readmissions after transcatheter aortic valve replacement in the united states: insights from the nationwide readmissions database. Circ Cardiovasc Interv. 2017;10:e004472. [DOI] [PubMed] [Google Scholar]
- 4.Ibrahim AM, Nathan H, Thumma JR, Dimick JB. Impact of the hospital readmission reduction program on surgical readmissions among medicare beneficiaries. Ann Surg. 2017;266:617–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bradley EH, Curry L, Horwitz LI, et al. Hospital strategies associated with 30-day readmission rates for patients with heart failure. Circ Cardiovasc Qual Outcomes. 2013;6:444–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bradley EH, Curry L, Horwitz LI, et al. Contemporary evidence about hospital strategies for reducing 30-day readmissions: a national study. J Am Coll Cardiol. 2012;60:607–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Desai NR, Ross JS, Kwon JY, et al. Association between hospital penalty status under the hospital readmission reduction program and readmission rates for target and nontarget conditions. JAMA. 2016;316:2647–2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta A, Allen LA, Bhatt DL, et al. Association of the hospital readmissions reduction program implementation with readmission and mortality outcomes in heart failure. JAMA Cardiol. 2018;3:44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weber SM, Greenberg CC. Medicare hospital readmission reduction program: what is the effect on surgery? Surgery. 2014;156:1066–1068. [DOI] [PubMed] [Google Scholar]
- 10.McAlister FA, Youngson E, Kaul P. Patients with heart failure readmitted to the original hospital have better outcomes than those readmitted elsewhere. J Am Heart Assoc. 2017;6:e004892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Havens JM, Olufajo OA, Tsai TC, et al. Hospital factors associated with care discontinuity following emergency general surgery. JAMA Surg. 2017;152:242–249. [DOI] [PubMed] [Google Scholar]
- 12.Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297:831–841. [DOI] [PubMed] [Google Scholar]
- 13.Adler-Milstein J, Jha AK. Health information exchange among U.S. Hospitals: who’s in, who’s out, and why? Healthc (Amst). 2014;2:26–32. [DOI] [PubMed] [Google Scholar]
- 14.Tsai TC, Orav EJ, Jha AK. Care fragmentation in the post-discharge period: surgical readmissions, distance of travel, and postoperative mortality. JAMA Surg. 2015;150:59–64. [DOI] [PubMed] [Google Scholar]
- 15.Iribarne A, Chang H, Alexander JH, et al. Readmissions after cardiac surgery: experience of the National Institutes of Health/Canadian Institutes of Health Research Cardiothoracic Surgical Trials Network. Ann Thorac Surg. 2014;98:1274–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holmes DR, Rich JB, Zoghbi WA, Mack MJ. The heart team of cardiovascular care. J Am Coll Cardiol. 2013;61:903–907. [DOI] [PubMed] [Google Scholar]
- 17.Beal EW, Bagante F, Paredes A, et al. Index versus non-index readmission after hepato-pancreato-biliary surgery: where do patients go to be readmitted? J Gastrointest Surg. 2019;23: 702–711. [DOI] [PubMed] [Google Scholar]
- 18.Zafar SN, Shah AA, Channa H, Raoof M, Wilson L, Wasif N. Comparison of rates and outcomes of readmission to index vs nonindex hospitals after major cancer surgery. JAMA Surg. 2018;153:719–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zheng C, Habermann EB, Shara NM, et al. Fragmentation of care after surgical discharge: non-index readmission after major cancer surgery. J Am Coll Surg. 2016;222:780–789.e782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kothari AN, Loy VM, Brownlee SA, et al. Adverse effect of post-discharge care fragmentation on outcomes after readmissions after liver transplantation. J Am Coll Surg. 2017;225: 62–67. [DOI] [PubMed] [Google Scholar]
- 21.Brooke BS, Goodney PP, Kraiss LW, Gottlieb DJ, Samore MH, Finlayson SRG. Readmission destination and risk of mortality after major surgery: an observational cohort study. Lancet. 2015;386:884–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project (HCUP). Introduction to the HCUP Nationwide Readmissions Database (NRD), 2013. Available at: https://www.hcup-us.ahrq.gov/db/nation/nrd/NRD_Introduction_2013.jsp. Accessed June 20, 2019.
- 23.Zogg CK, Olufajo OA, Jiang W, et al. The need to consider longer-term outcomes of care: racial/ethnic disparities among adult and older adult emergency general surgery patients at 30, 90, and 180 days. Ann Surg. 2017;266:66–75. [DOI] [PubMed] [Google Scholar]
- 24.Graboyes EM, Kallogjeri D, Saeed MJ, Olsen MA, Nussenbaum B. Postoperative care fragmentation and thirty-day unplanned readmissions after head and neck cancer surgery. Laryngoscope. 2017;127:868–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Walraven C, Oake N, Jennings A, Forster AJ. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract. 2010;16:947–956. [DOI] [PubMed] [Google Scholar]
- 26.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the hospital readmissions reduction program. JAMA. 2013;309:342–343. [DOI] [PubMed] [Google Scholar]
- 27.Williams JB, McConnell G, Allender JE, et al. One-year results from the first US-based enhanced recovery after cardiac surgery (ERAS Cardiac) program. J Thorac Cardiovasc Surg. 2019;157:1881–1888. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


