1. Introduction
The COVID-19 (SARS-CoV-2) pandemic has changed the social environment in which people live and work, as well as the social systems they rely on.39,88 To contain the spread of coronavirus and to prepare for a dramatic increase in demand for limited hospital/medical facilities and resources, societies have enforced physical distancing measures. Consequently, there have been limitations on the use of public transportation, public spaces, and work, education, and recreational facilities. Furthermore, access to vital, but nonurgent, healthcare services (including pain management services) has been restricted. These changes have affected the way people connect with each other, manage their health and wellbeing, and fulfil their social roles. For some, these changes may present opportunities (eg, increased time with family, normalisation of flexible working, and reduced demand for travel). For others, however, these social changes can also represent significant threats to health and wellbeing.
The negative impact of social changes prompted by the COVID-19 crisis may disproportionately affect individuals living with long-term painful conditions. Living with chronic pain can threaten an individuals' fundamental social needs for autonomy (agency or independence), belonging (social connection), and justice (fairness). In turn, for some, experiencing heightened social threat can maintain and exacerbate chronic pain.48 In this review, we draw attention to the potential for social and systemic changes associated with attempts to contain the spread of COVID-19 to precipitate, maintain, and exacerbate pain by increasing the social threats faced by individuals with chronic pain (Fig. 1). We also suggest strategies for mitigating the social impact of COVID-19 on those living with chronic pain, for instance by learning from the resilience demonstrated by people in pain who have found ways to deal with social threat. Finally, we suggest several time-critical, high-impact research questions for further investigation (Fig. 1).
Figure 1.
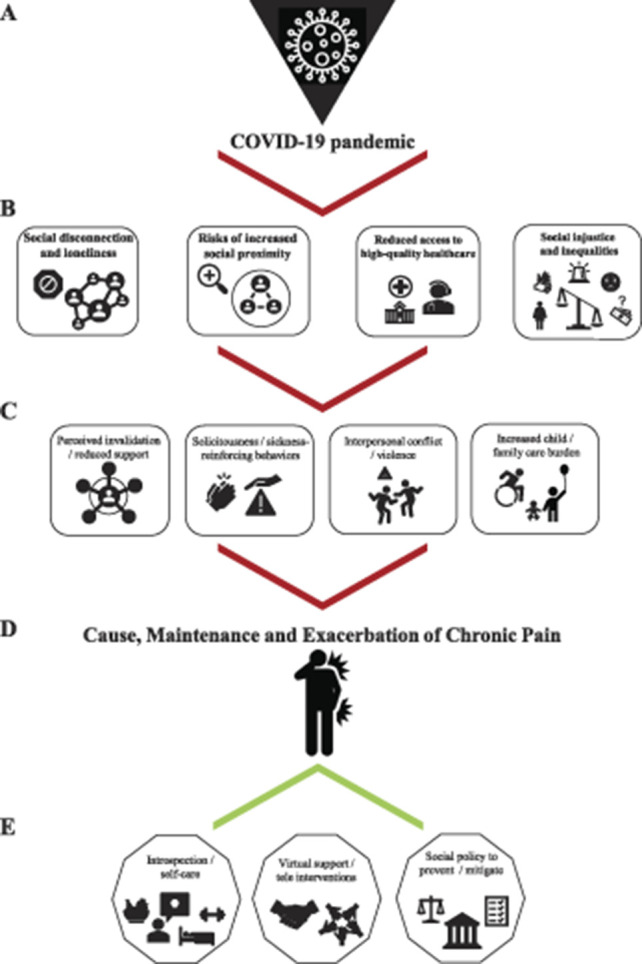
Schematic representation of how the COVID 19 pandemic (A) exacerbates existing levels of social threat (B), thereby inducing several social challenges (C) for people with chronic pain, and ultimately increasing the risk for the development, maintenance, and exacerbation of chronic pain complaints (D). Possible protecting processes and interventions countering the effects of the pandemic are portrayed as well (E).
2. Social threats posed by the COVID-19 pandemic
1.1. Social disconnection and loneliness
One of the most immediate effects of the pandemic on our social lives is the introduction of physical distancing measures and restriction of travel. It is well known that spontaneous social interactions with others and participation in social roles can build and maintain a generalised sense of trust in others (social capital), promote feelings of wellbeing,76 provide protection from the harmful effects of stress,95 promote social connectedness, and reduce pain sensitivity.91 Conversely, social isolation is associated with loneliness, higher levels of depression and anxiety, poorer health behaviours, poorer sleep, higher blood pressure, poorer immune function, and pain.40,42
Chronic pain conditions place individuals at an increased risk of social isolation, smaller social network size, and reduced social role functioning,37,38,78 all of which have negative implications for pain interference and pain intensity over time.7,31,47 Indeed, disruption to social roles and relationships is one of the most distressing aspects of living with chronic pain.81 Physical distance from others and reduced participation in work and social activities can cause people to feel lonely or socially distanced from others,73 and there are concerns that the COVID-19 pandemic will lead to a steep rise in the prevalence of loneliness.5,22,35,39 People living with chronic pain, who may have entered the pandemic with fewer social resources than others, may be particularly vulnerable to feelings of loneliness and social disconnection at this time. Unless individuals have the ability and means to maintain meaningful connections with others despite physical distancing measures, being physically isolated from others threatens to exacerbate pain and associated disability.
1.2. Risk of increased social proximity
The paradox of COVID-19 is that being physically isolated from one's community can mean living in closer proximity to one's household members. People living with chronic pain conditions may benefit from more frequent contact with family members because closer proximity offers more opportunity to improve social bonds. However, enforced close-proximity living could also bring challenges to autonomy and independence. Although social support can help buffer against pain,14,15,18,56 an increase in solicitous behaviours in such close proximity might unintentionally contribute to the chronicity of pain.34,43,72 For example, in households where a child is in pain, increased social proximity could lead to increased exposure to protective parental behaviours and reductions in child autonomy and activity. Conversely, family members could become desensitised to the pain of others, or even become avoidant, risking further isolation for individuals living with pain. Those living with pain may experience increased feelings of guilt in response to increased support, especially if they perceive themselves to be a burden.50,75 Alternatively, fear of rejection could lead to masking pain from others in shared living spaces, preventing individuals with pain from asking for help to meet their needs.13,65
There is also a risk that for people living with chronic pain, living in close proximity and enclosed environments could increase exposure to interpersonal conflict,63,69 which is known to amplify pain and disability.11,26,36,61 For some, COVID-19 has brought about increased risks of conflict among household members, as they deal with the stresses associated with unexpected financial pressures, job insecurity, and unemployment.21 Many people are struggling to juggle multiple social roles and responsibilities—supporting children with schoolwork, working from home, and parenting—leading to emotional exhaustion. Women, in particular, are likely to carry a greater social burden and greater responsibility for childcare during COVID-19.1,92 Critically, domestic abuse has increased during the COVID-19 lockdown,10 which has also been shown to contribute to chronic pain.2,60
1.3. Reduced access to high-quality pain management
COVID-19 potentially poses a significant challenge for patients seeking to access pain management. Although pain management is a fundamental right,23 the health system responses to mitigate the impact of COVID-19 may significantly affect access for patients with complex medical conditions (eg, people with comorbid mental health conditions and addiction) and widen existing inequities in relation to pain management for socially disadvantaged populations.90 For some people with chronic pain, the pandemic might bring life stressors that result in pain flare-ups, and increase the need for pain services.77 Furthermore, individual pain experiences may not be considered as immediately important when compared to the need to treat life-threatening symptoms associated with COVID-19,12 leading to less help-seeking and psychological distress.
Pain management during this pandemic for clinicians involves balancing access to care with minimising safety risk from exposure to COVID-19 for vulnerable patients and clinicians themselves.79 Cancelled elective surgeries, closure of pain management services, and redeployment of clinicians to other areas of care all result in limited access to high-quality care. Consequently, the increased burden on healthcare workers may result in a greater focus on biomedical management (eg, opioid prescribing), rather than psychological and interdisciplinary treatment approaches. Although this may be deemed necessary in the context of the pandemic due to heightened needs from patients for pain relief, clinicians and patients may not agree on opioid prescription/deprescription.66 In addition, the individual assessment required to address the risks and benefits of opioid use and the monitoring of its use85 may be complicated by a lack of access to face-to-face pain services.
In the absence of the availability of face-to-face contact, telehealth is increasingly being recommended as a first line of care for patients,19 including those with chronic pain.29 The rapid transition to telehealth in response to physical distancing regulations allows people to access high-quality care without travelling, potentially increasing patient access to care. It also opens up new opportunities and enables us to think about new ways of delivering pain management. However, this mode of delivery may be particularly challenging for vulnerable groups due to poor health status and low technological literacy.71 Even when services are delivered through telehealth, the fear of sharing confidential information from home and juggling multiple social responsibilities, particularly for women, pose further barriers to engaging in high-quality care.64 In the context of delivery, practical challenges in conducting multidisciplinary treatment through telehealth77 may lead to a prioritising of individual over multidisciplinary approaches. This is despite evidence that care delivered through telehealth can be as effective as face-to-face care for people experiencing pain conditions.55
1.4. Exacerbation of social injustice and social inequalities
COVID-19 is exacerbating existing social injustices and inequalities. Extreme events such as terrorist attacks and natural disasters32,44,96 are known to undermine the fundamental belief that the world is just, stable, orderly, and predictable,52 with ramifications for perceived life control, future prospects, and wellbeing.67,86 This is particularly relevant to chronic pain because commitment to the belief in a just world can buffer against its adverse effects.57 A pandemic-initiated violation of just-world beliefs could exacerbate perceived injustices associated with pain.16 For example, physical distancing policies could further increase social isolation and potentially worsen perceived injustices,80 while disrupting social networks that are sources of justice and support74 may heighten perceptions of invalidation among those with pain, driven by the sense that one does not matter to others.17
Variation in the effect of COVID-19 illustrates social inequalities around pain, and health care more generally. There are known individual differences in pain associated with social identities, including sex, ethnicity, and age.6,33 There are also social inequalities and biases, which can affect pain burden25 and access to pain care.24,82 Structural and individual biases towards minority and marginalized groups that are heightened by uncertainty, stress, and fear49 are likely to be exacerbated by COVID-19. Discrimination experienced by marginalized groups can affect peripheral and central processes, including immune functioning,20,28,83 thus compounding the negative effects associated with the stigmatization of chronic pain.26
Those living in poorer and/or more remote communities have higher rates of chronic pain and comorbidities60,62 and limited access to health care, which can lead to greater unmanaged pain and disability.3,4 Reduced access to health care, higher costs, and language might form additional barriers to pain management in these communities (eg, refugees). For example, disabling chronic pain can be more prevalent in Indigenous populations, who are also less likely to access support services.3,4,8 Travel restrictions imposed to limit the spread of COVID-19 into remote communities are likely to disrupt the provision of nonessential services, further limiting access to pain care. Socioeconomic disadvantage also increases vulnerability to disease, including COVID-19, through many potential pathways including lower social support,89 overcrowding, poorer sanitation, neighbourhood, and housing conditions, and poorer health behaviours (eg, smoking, diet, alcohol consumption, and reduced exercise).9,70 Furthermore, although people from lower socioeconomic backgrounds are overrepresented in “essential” employment sectors, which have been largely spared from COVID-19-related redundancies, many of these employees are now facing longer working hours under more demanding conditions. All these factors could not only lead to increased risk of exposure to COVID-19, but also, if left untreated, exacerbate other conditions, including chronic pain. In short, COVID-19 has disproportionately affected socially disadvantaged groups, and the ensuing global economic fallout could magnify these inequalities in pain further.90 The concern is that the most economically disadvantaged will be most likely to be exposed to the hazard, most susceptible to harm from it, and most likely to experience negative outcomes from it.88
3. Responding to social threats posed by COVID-19
The wide range of social threats that COVID-19 brings to those in pain means that no one response will address all these issues. However, by identifying such threats, we can start to think of more focused and targeted approaches. For example, just as some treatments have moved online, it may also be possible to mitigate some of the impacts of physical distancing and social isolation using technology. Social media platforms, due to their wide reach and penetration, can help disseminate key information about COVID-19, providing virtual support to enhance social connectedness.58 People with pain already report using digital peer-support groups to connect with similar others and derive benefits from feeling validated and heard.59 Online peer-support could potentially be used to help reduce felt social distance while maintaining physical distance. Increasing digital social connectedness might afford people with chronic pain more social contact and accessibility than is possible face-to-face because it does not require physical mobility. However, we also need to ensure that the use of social platforms is beneficial, and do not increase risk (eg, due to the exposure to poor-quality health information that reinforces disability or propagating unproven and potentially harmful approaches).27 Even so, the pandemic has provided an opportunity to understand how social media might be better used as a tool to develop a sense of community and reduce isolation.
Online technology can be used to facilitate the delivery of healthcare interventions, under the guidance of healthcare professionals. For example, cognitive behavioural therapies for loneliness delivered online can decrease loneliness and improve mental wellbeing.45,46 Online pain management programs seem to hold promise,29 particularly when patients have contact with healthcare providers, albeit remotely.54 Online resources can disseminate pain education, and online training programs on pain self-management can be developed for healthcare professionals, those with pain, and their close others.30,41,84 However, these novel digital interventions might not be accessible for all and may even put up new barriers to those who require them the most (eg, socially disconnected individuals with limited digital literacy).
We also need to think beyond technology. The COVID-19 pandemic served to highlight the upstream social determinants of health, many of affect chronic pain directly. Historic social inequalities and unequal access to resources shape individual-level risk factors, which in turn produce and perpetuate health disparities.53 These structural problems require structural solutions51,93 with the aim to improve population health, for instance by bolstering social welfare systems, public health funding, and improved global cooperation.68,87,94 At the local level, online technologies could mitigate the social threat of existing social inequalities and injustices, providing access to relatively inexpensive, location-independent treatment, and social connection. Coupled with systemic interventions such as increased government funding to telehealth services, reducing the costs and barriers to internet access, and making computers and mobile devices available to those who otherwise might not have access to them can further reduce these disparities.97
4. Conclusions and future directions
The current pandemic has exacerbated existing sources of social threat for people with chronic pain. To prevent a population-level increase in the severity and impact of chronic pain, it is critical to devote scientific attention to the assessment, mitigation, and prevention of sources of social threat for people with chronic pain. Table 1 outlines several high-impact areas for research to this end. Crucially, COVID-19 should not only be regarded as a challenge but also as a unique opportunity for researchers and clinicians to develop new ways to deliver social support and pain management, as well as understand the impact of social adjustment among individuals with chronic pain.
Table 1.
Priorities for research on social factors resulting from the COVID-19 pandemic.
| 1. Demographic and longitudinal studies on the social consequences of the pandemic for people with chronic pain. |
| a. Assess nature and cohesion of family and wider social support networks and emotional connectedness of people with chronic pain during physical distancing. |
| b. Assess how minority and marginalised groups with chronic pain are accessing pain support during the pandemic, identifying possible facilitators and barriers. |
| c. Assess different forms of social threat for people with chronic pain such as loneliness, experiences of injustice, victimization, and invalidation. |
| d. Examine the effects of social distancing measures in the workplace, and on job prospects after the COVID-19 pandemic for employees with chronic pain. |
| 2. Fundamental research on biological, psychological, and/or social working mechanisms on the bidirectional relationship between social factors and pain. |
| a. Assess the immediate and long-term effects of physical distancing on relevant pain outcomes and pain management strategies. |
| b. Investigate whether pain-related stigma, discrimination, social isolation, or perceptions of injustice increase vulnerability to COVID-19 infection or affect risk-related behaviour. |
| c. Investigate the role of social learning in times of uncertainty and the effect on pain behaviour. |
| 3. Clinical and fundamental research on digital social support for chronic pain. |
| a. Study the potential limitations (eg, less physical activity, lower quality of social relationships) and strengths (eg, lower threshold for engagement) of digital social support compared to face-to-face social support on pain outcomes. |
| b. Conduct theory-based studies on mediators that influence the effectiveness of online social support for chronic pain complaints. |
| 4. Clinical research on the effectiveness of digital pain management interventions for chronic pain. |
| a. Clinical trials comparing the effectiveness of digital vs face-to-face interventions. |
| b. Research on the quality of social relationships, communication and trust between professionals delivering online interventions and chronic pain patients. |
| c. Identify barriers and facilitators for access to online treatments, especially for marginalized populations with chronic pain. |
| 5. Research into possible individual resilience mechanisms (eg, increased social cohesions, revaluation of values and priorities, increased uptake of online pain management) buffering against the effects of the pandemic on chronic pain. |
| 6. Systemic research on the effects of multilevel social determinants of health on chronic pain and policies to address them (eg, labour relations, income inequality, neighbourhood deprivation, racism, sexism, ageism, access to health care, etc.), to strengthen population resilience to the impact of heightened social threats on chronic pain. |
| a. Research into integrated methods of intervention or analysis (eg, dynamic systems modelling) across micro (ie, families, partnerships), meso (ie, community, city, organizations), and macro (ie, nations, civilizations) levels of the social system. |
Conflict of interest statement
The authors have no conflicts of interest to report.
Supplemental video content
A video abstract associated with this article can be found at http://links.lww.com/PAIN/B141.
Acknowledgements
K. Karos is a postdoctoral researcher supported by the Research Foundation, Flanders, Belgium (grant 1244820N). F.P. Kapos is a PhD candidate who is supported by the Patrick-Beresford Fellowship in Social Epidemiology and the P.E.O. International Peace Scholarship. H. Devan is a Postdoctoral Fellow supported by the Centre for Health, Activity and Rehabilitation Research (CHARR) Postdoctoral Fellowship at the School of Physiotherapy, University of Otago, New Zealand. This review was an initiative of the Social Aspects in Pain Special Interest Group (SocSIG) of the International Association of Pain (IASP).
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
K. Karos and J.L. McParland contributed equally to this work.
References
- [1].Alon TM, Doepke M, Olmstead-Rumsey J, Tertilt M. The impact of COVID-19 on gender equality. Cambridge, 2020. Available at: https://www.nber.org/papers/w26947. [Google Scholar]
- [2].Anda R, Tietjen G, Schulman E, Felitti V, Croft J. Adverse childhood experiences and frequent headaches in adults. Headache 2010;50:1473–81. [DOI] [PubMed] [Google Scholar]
- [3].Australian Institute of Health and Welfare. The burden of musculoskeletal conditions in Australia: a detailed analysis of the Australian Burden of Disease Study 2011. Canberra, Australia: AIHW, 2017. [Google Scholar]
- [4].Barnabe C, Hemmelgarn B, Jones CA, Peschken CA, Voaklander D, Joseph L, Bernatsky S, Esdaile JM, Marshall DA. Imbalance of prevalence and specialty care for osteoarthritis for first nations people in Alberta, Canada. J Rheumatol 2015;42:323–8. [DOI] [PubMed] [Google Scholar]
- [5].Berg-Weger M, Morley JE. Editorial: loneliness and social isolation in older adults during the COVID-19 pandemic: implications for gerontological social work. J Nutr Health Aging 2020;24:456–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Blyth FM, March LM, Brnabic AJ, Jorm LR, Williamson M, Cousins MJ. Chronic pain in Australia: a prevalence study. PAIN 2001;89:127–34. [DOI] [PubMed] [Google Scholar]
- [7].Boehm A, Eisenberg E, Lampel S. The contribution of social capital and coping strategies to functioning and quality of life of patients with fibromyalgia. Clin J Pain 2011;27:233–9. [DOI] [PubMed] [Google Scholar]
- [8].Bolen J, Schieb L, Hootman JM, Helmick CG, Theis K, Murphy LB, Langmaid G. Differences in the prevalence and severity of arthritis among racial/ethnic groups in the United States, National Health Interview Survey, 2002, 2003, and 2006. Prev Chronic Dis 2010;7:A64. [PMC free article] [PubMed] [Google Scholar]
- [9].Booher L. The impact of low socioeconomic status in adults with chronic pain: an integrative review. Orthop Nurs 2019;38:381–9. [DOI] [PubMed] [Google Scholar]
- [10].Bradbury-Jones C, Isham L. The pandemic paradox: the consequences of COVID-19 on domestic violence. J Clin Nurs 2020;29:2047–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Burns JW, Peterson KM, Smith DA, Keefe FJ, Porter LS, Schuster E, Kinner E. Temporal associations between spouse criticism/hostility and pain among patients with chronic pain: a within-couple daily diary study. PAIN 2013;154:2715–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Buunk BP, Ybema JF. Social comparisons and occupational stress: the identification-contrast model. In: Buunk BP, Gibbons FX, editors. Health, coping, and well-being: perspectives from social comparison theory: Lawrence Erlbaum Associates, Inc, 1997:359–88. [Google Scholar]
- [13].Cano A, Goubert L. What's in a name? The case of emotional disclosure of pain-related distress. J Pain 2017;18:881–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Cano A, Leong LE, Williams AM, May DK, Lutz JR. Correlates and consequences of the disclosure of pain-related distress to one's spouse. PAIN 2012;153:2441–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Cano A, Williams AC. Social interaction in pain: reinforcing pain behaviors or building intimacy? PAIN 2010;149:9–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Carriere JS, Donayre Pimentel S, Yakobov E, Edwards RR. A systematic review of the association between perceived injustice and pain-related outcomes in individuals with musculoskeletal pain. Pain Med 2020;21:1449–63. [DOI] [PubMed] [Google Scholar]
- [17].Casale S, Flett GL. Interpersonally-based fears during the COVID-19 pandemic: reflections on the fear of missing out and the fear of not mattering constructs. Clin Neuropsychiatry 2020;17:88–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Che X, Cash R, Ng SK, Fitzgerald P, Fitzgibbon BM. A systematic review of the processes underlying the main and the buffering effect of social support on the experience of pain. Clin J Pain 2018;34:1061–76. [DOI] [PubMed] [Google Scholar]
- [19].Cohen SP, Baber ZB, Buvanendran A, McLean L, Chen Y, Hooten WM, Laker SR, Wasan WAD, Kennedy DJ, Sandbrink F, King L, Fowler C, Stojanovic MP, Hayek SM, Phillips C. Pain management best practices from multispecialty organizations during the COVID-19 pandemic and public health crises. Pain Med 2020;21:1331–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Cole SW, Kemeny ME, Taylor SE. Social identity and physical health: accelerated HIV progression in rejection-sensitive gay men. J Personal Soc Psychol 1997;72:320–35. [DOI] [PubMed] [Google Scholar]
- [21].Cook AK. I've got my own problems: the impact of parental stressors on parental anger. J Juvenile Justice 2015;4:57–70. [Google Scholar]
- [22].Courtet P, Olié E, Debien C, Vaiva G. Keep socially (but not physically) connected and carry on: preventing suicide in the age of COVID-19. J Clin Psychiatry 2020;81:20com13370. [DOI] [PubMed] [Google Scholar]
- [23].Cousins MJ, Lynch ME. The Declaration Montreal: access to pain management is a fundamental human right. PAIN 2011;152:2673–4. [DOI] [PubMed] [Google Scholar]
- [24].Craig KD, Holmes C, Hudspith M, Moor G, Moosa-Mitha M, Varcoe C, Wallace B. Pain in persons who are marginalized by social conditions. PAIN 2020;161:261–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Dahlhamer JM, Galinsky AM, Joestl SS, Ward BW. Barriers to health care among adults identifying as sexual minorities: a US national study. Am J Public Health 2016;106:1116–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].De Ruddere L, Craig KD. Understanding stigma and chronic pain: a-state-of-the-art review. PAIN 2016;157:1607–10. [DOI] [PubMed] [Google Scholar]
- [27].Devan H, Godfrey HK, Perry MA, Hempel D, Saipe B, Hale L, Grainger R. Current practices of health care providers in recommending online resources for chronic pain self-management. J Pain Res 2019;12:2457–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav 2013;17:1785–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Eccleston C, Blyth FM, Dear BF, Fisher EA, Keefe FJ, Lynch ME, Palermo TM, Reid MC, Williams ACC. Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services. PAIN 2020;161:889–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].European Pain Federation EFIC. Pain Curricula, 2020. Available at: https://europeanpainfederation.eu/education/pain-curricula/. Accessed July 7, 2020. [Google Scholar]
- [31].Evers AW, Kraaimaat FW, Geenen R, Jacobs JW, Bijlsma JW. Pain coping and social support as predictors of long-term functional disability and pain in early rheumatoid arthritis. Behav Res Ther 2003;41:1295–310. [DOI] [PubMed] [Google Scholar]
- [32].Ferguson N, Kamble SV. The role of revenge, denial, and terrorism distress in restoring just world beliefs: the impact of the 2008 Mumbai attacks on British and Indian students. J Soc Psychol 2012;152:687–96. [DOI] [PubMed] [Google Scholar]
- [33].Fillingim RB. Individual differences in pain: understanding the mosaic that makes pain personal. PAIN 2017;158(suppl 1):S11–s18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Fordyce WE. Behavioral methods in chronic pain and illness. St Louis: Mosby, 1976. [Google Scholar]
- [35].Galea S. Well: what we need to talk about when we talk about health. New York: Oxford University Press, 2019. [Google Scholar]
- [36].Gauthier LR, Rodin G, Zimmermann C, Warr D, Librach SL, Moore M, Shepherd FA, Gagliese L. The communal coping model and cancer pain: the roles of catastrophizing and attachment style. J Pain 2012;13:1258–68. [DOI] [PubMed] [Google Scholar]
- [37].Gold DT, Roberto KA. Correlates and consequences of chronic pain in older adults. Geriatr Nurs 2000;21:270–3. [DOI] [PubMed] [Google Scholar]
- [38].Harris RA. Chronic pain, social withdrawal, and depression. J Pain Res 2014;7:555–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Cohen Silver R, Everall I, Ford T, John A, Kabir T, King K, Madan I, Michie S, Przybylski AK, Shafran R, Sweeney A, Worthman CM, Yardley L, Cowan K, Cope C, Hotopf M, Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 2020;7:547–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci 2015;10:227–37. [DOI] [PubMed] [Google Scholar]
- [41].International Association for the Study of Pain. IASP Curricula, 2020. https://www.iasp-8pain.org/Education/CurriculaList.aspx. Accessed July 7, 2020. [Google Scholar]
- [42].Jaremka LM, Andridge RR, Fagundes CP, Alfano CM, Povoski SP, Lipari AM, Agnese DM, Arnold MW, Farrar WB, Yee LD, Carson WE, III, Bekaii-Saab T, Martin EW, Jr, Schmidt CR, Kiecolt-Glaser JK. Pain, depression, and fatigue: loneliness as a longitudinal risk factor. Health Psychol 2014;33:948–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Jensen MP, Moore MR, Bockow TB, Ehde DM, Engel JM. Psychosocial factors and adjustment to chronic pain in persons with physical disabilities: a systematic review. Arch Phys Med Rehabil 2011;92:146–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Kaiser CR, Vick SB, Major B. A prospective investigation of the relationship between just-world beliefs and the desire for revenge after September 11, 2001. Psychol Sci 2004;15:503–6. [DOI] [PubMed] [Google Scholar]
- [45].Käll A, Backlund U, Shafran R, Andersson G. Lonesome no more? A two-year follow-up of internet-administered cognitive behavioral therapy for loneliness. Internet Interv 2020;19:100301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Käll A, Jägholm S, Hesser H, Andersson F, Mathaldi A, Norkvist BT, Shafran R, Andersson G. Internet-Based cognitive behavior therapy for loneliness: a pilot randomized controlled trial. Behav Ther 2020;51:54–68. [DOI] [PubMed] [Google Scholar]
- [47].Karayannis NV, Baumann I, Sturgeon JA, Melloh M, Mackey SC. The impact of social isolation on pain interference: a longitudinal study. Ann Behav Med 2019;53:65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Karos K, Williams ACC, Meulders A, Vlaeyen JWS. Pain as a threat to the social self: a motivational account. PAIN 2018;159:1690–5. [DOI] [PubMed] [Google Scholar]
- [49].Kite ME, Whitley BE., Jr Psychology of prejudice and discrimination. New York, NY: Psychology Press, 2016. [Google Scholar]
- [50].Kowal J, Wilson KG, McWilliams LA, Péloquin K, Duong D. Self-perceived burden in chronic pain: relevance, prevalence, and predictors. PAIN 2012;153:1735–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Krieger N. Measures of racism, sexism, heterosexism, and gender binarism for health equity research: from structural injustice to embodied harm-an ecosocial analysis. Annu Rev Public Health 2020;41:37–62. [DOI] [PubMed] [Google Scholar]
- [52].Lerner M, Miller D. Just world research and the attribution process: looking back and ahead. Psychol Bull 1978;85:1030–51. [Google Scholar]
- [53].Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav 1995;Spec No:80–94. [PubMed] [Google Scholar]
- [54].Mariano TY, Wan L, Edwards RR, Jamison RN. Online teletherapy for chronic pain: a systematic review. J Telemed Telecare 2019. doi:10.1177/1357633X19871746 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [55].Martorella G, Boitor M, Berube M, Fredericks S, Le May S, Gélinas C. Tailored web-based interventions for pain: systematic review and meta-analysis. J Med Internet Res 2017;19:e385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Matos M, Bernardes SF, Goubert L, Beyers W. Buffer or amplifier? Longitudinal effects of social support for functional autonomy/dependence on older adults' chronic pain experiences. Health Psychol 2017;36:1195–206. [DOI] [PubMed] [Google Scholar]
- [57].McParland J, Eccleston C. “It's not fair”. Social justice appraisals in the context of chronic pain. Curr Dir Psychol Sci 2013;22:484–9. [Google Scholar]
- [58].Merchant RM, Lurie N. Social media and emergency preparedness in response to novel coronavirus. JAMA 2020;323:2011–12. [DOI] [PubMed] [Google Scholar]
- [59].Merolli M, Gray K, Martin-Sanchez F. Therapeutic affordances of social media: emergent themes from a global online survey of people with chronic pain. J Med Internet Res 2014;16:e284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth 2019;123:e273–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Mohammadi S, Chambers CT, Rosen NO. Expression of pain behaviors and perceived partner responses in individuals with chronic pain: the mediating role of partner burden and relationship quality. Clin J Pain 2018;34:927–35. [DOI] [PubMed] [Google Scholar]
- [62].Nakad L, Booker S, Gilbertson-White S, Shaw C, Chi NC, Herr K. Pain and multimorbidity in late life. Curr Epidemiol Rep 2020;7:1–8. [Google Scholar]
- [63].Neff LA, Karney BR. Acknowledging the elephant in the room: how stressful environmental contexts shape relationship dynamics. Curr Opin Psychol 2017;13:107–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].New Zealand Telehealth. Equity & improving access with Telehealth Webinar, 2020. Available at: https://www.telehealth.org.nz/health-provider/webinars/#webinar2. Accessed July 7, 2020. [Google Scholar]
- [65].Newton-John TR, Williams AC. Chronic pain couples: perceived marital interactions and pain behaviours. PAIN 2006;123:53–63. [DOI] [PubMed] [Google Scholar]
- [66].Nichols VP, Toye F, Eldabe S, Sandhu HK, Underwood M, Seers K. Experiences of people taking opioid medication for chronic non-malignant pain: a qualitative evidence synthesis using meta-ethnography. BMJ Open 2020;10:e032988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Nudelman G, Otto K, Dalbert C. Can belief in a just world buffer mood and career prospects of people in need of risk protection? First experimental evidence. Risk Anal 2016;36:2247–57. [DOI] [PubMed] [Google Scholar]
- [68].Obstfeld M, Posen AS, Blanchard OJ. How the G20 can hasten recovery from COVID-19, 2020. Available at: https://www.piie.com/publications/piie-briefings/how-g20-can-hasten- recovery-covid-19. Accessed July 7, 2020. [Google Scholar]
- [69].Organisation for Economic Co-operation and Development. COVID-19: Protecting people and societies, 2020. Available at: http://www.oecd.org/coronavirus/policy-responses/covid-19- protecting-people-and-societies-e5c9de1a/. Accessed July 7, 2020. [Google Scholar]
- [70].Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annu Rev Sociol 2010;36:349–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Parker S, Prince A, Thomas L, Song H, Milosevic D, Harris MF. Electronic, mobile and telehealth tools for vulnerable patients with chronic disease: a systematic review and realist synthesis. BMJ Open 2018;8:e019192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Romano JM, Jensen MP, Turner JA, Good AB, Hops H. Chronic pain patient-partner interactions: further support for a behavioral model of chronic pain. Behav Ther 2000;31:415–50. [Google Scholar]
- [73].Savikko N, Routasalo P, Tilvis RS, Strandberg TE, Pitkälä KH. Predictors and subjective causes of loneliness in an aged population. Arch Gerontol Geriatr 2005;41:223–33. [DOI] [PubMed] [Google Scholar]
- [74].Scott W, McEvoy A, Garland R, Bernier E, Milioto M, Trost Z, Sullivan M. Sources of injustice among individuals with persistent pain following musculoskeletal injury. Psychol Inj Law 2016;9:6–15. [Google Scholar]
- [75].Serbic D, Pincus T, Fife-Schaw C, Dawson H. Diagnostic uncertainty, guilt, mood, and disability in back pain. Health Psychol 2016;35:50–9. [DOI] [PubMed] [Google Scholar]
- [76].Shankar A, Rafnsson SB, Steptoe A. Longitudinal associations between social connections and subjective wellbeing in the English Longitudinal Study of Ageing. Psychol Health 2015;30:686–98. [DOI] [PubMed] [Google Scholar]
- [77].Shanthanna H, Strand NH, Provenzano DA, Lobo CA, Eldabe S, Bhatia A, Wegener J, Curtis K, Cohen SP, Narouze S. Caring for patients with pain during the COVID-19 pandemic: consensus recommendations from an international expert panel. Anaesthesia 2020;75:935–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Smith T. “On their own”: social isolation, loneliness and chronic musculoskeletal pain in older adults. Qual Ageing Old Adults 2017;18:87–92. [Google Scholar]
- [79].Song XJ, Xiong DL, Wang ZY, Yang D, Zhou L, Li RC. Pain management during the COVID-19 pandemic in China: lessons learned. Pain Med 2020;21:1319–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Sturgeon JA, Carriere JS, Kao MJ, Rico T, Darnall BD, Mackey SC. Social disruption mediates the relationship between perceived injustice and anger in chronic pain: a collaborative health outcomes information registry study. Ann Behav Med 2016;50:802–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Sturgeon JA, Dixon EA, Darnall BD, Mackey SC. Contributions of physical function and satisfaction with social roles to emotional distress in chronic pain: a Collaborative Health Outcomes Information Registry (CHOIR) study. PAIN 2015;156:2627–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Tait RC, Chibnall JT. Racial/ethnic disparities in the assessment and treatment of pain: psychosocial perspectives. Am Psychol 2014;69:131–41. [DOI] [PubMed] [Google Scholar]
- [83].Thames AD, Irwin MR, Breen EC, Cole SW. Experienced discrimination and racial differences in leukocyte gene expression. Psychoneuroendocrinology 2019;106:277–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Thompson K, Johnson MI, Milligan J, Briggs M. Twenty-five years of pain education research-what have we learned? Findings from a comprehensive scoping review of research into pre-registration pain education for health professionals. PAIN 2018;159:2146–58. [DOI] [PubMed] [Google Scholar]
- [85].Toye F, Seers K, Tierney S, Barker KL. A qualitative evidence synthesis to explore healthcare professionals' experience of prescribing opioids to adults with chronic non-malignant pain. BMC Fam Pract 2017;18:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Ucar GK, Hasta D, Malatyali MK. The mediating role of perceived control and hopelessness in the relation between personal belief in a just world and life satisfaction. Pers Individ Differ 2019;143:68–73. [Google Scholar]
- [87].United Nations. The secretary-general's UN response and recovery fund, 2020. Available at: https://unsdg.un.org/resources/secretary-generals-un-covid-19-response-and-recovery-fund. Accessed July 7, 2020. [Google Scholar]
- [88].Van Bavel JJ, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, Crockett MJ, Crum AJ, Douglas KM, Druckman JN, Drury J, Dube O, Ellemers N, Finkel EJ, Fowler JH, Gelfand M, Han S, Haslam SA, Jetten J, Kitayama S, Mobbs D, Napper LE, Packer DJ, Pennycook G, Peters E, Petty RE, Rand DG, Reicher SD, Schnall S, Shariff A, Skitka LJ, Smith SS, Sunstein CR, Tabri N, Tucker JA, Linden SV, Lange PV, Weeden KA, Wohl MJA, Zaki J, Zion SR, Willer R. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav 2020;4:460–71. [DOI] [PubMed] [Google Scholar]
- [89].Vonneilich N, Jöckel KH, Erbel R, Klein J, Dragano N, Siegrist J, von dem Knesebeck O. The mediating effect of social relationships on the association between socioeconomic status and subjective health—results from the Heinz Nixdorf Recall cohort study. BMC Public Health 2012;12:285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Webster F, Connoy L, Sud A, Pinto AD, Katz J. Grappling with chronic pain and poverty during the COVID-19 pandemic. Can J Pain 2020;4:125–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Weinstein D, Launay J, Pearce E, Dunbar RI, Stewart L. Singing and social bonding: changes in connectivity and pain threshold as a function of group size. Evol Hum Behav 2016;37:152–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Wenham C, Smith J, Morgan R. COVID-19: the gendered impacts of the outbreak. Lancet 2020;395:846–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Williams DR, Cooper LA. Reducing racial inequities in health: using what we already know to take action. Int J Environ Res Public Health 2019;16:606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].World Health Organization. COVID 19 strategy update. Geneva, 2020. Available at: https://www.who.int/publications-detail/covid-19-strategy-update---14-april-2020. Accessed July 7, 2020. [Google Scholar]
- [95].Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 Days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Monit 2020;26:e923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Xie X, Liu H, Gan Y. Belief in a just world when encountering the 5/12 Wenchuan earthquake. Environ Behav 2011;43:566–86. [Google Scholar]
- [97].Yip PSF, Chau PH. Physical distancing and emotional closeness amidst COVID-19. Crisis 2020;41:153–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A video abstract associated with this article can be found at http://links.lww.com/PAIN/B141.


