Supplemental Digital Content is Available in the Text.
Abstract
Background:
During the COVID-19 pandemic, telehealth modalities have come to prominence as a strategy for providing patient care when in-person care provision opportunities are limited. The degree of adoption by neuro-ophthalmologists has not been quantified.
Methods:
Telehealth utilization pre–COVID-19 and peri–COVID-19 was surveyed among practicing neuro-ophthalmologists in and outside the United States using an online platform. Demographics, perceived benefits, barriers, and utility for different neuro-ophthalmic conditions were collected. Data collection occurred over a 2-week period in May 2020.
Results:
Two hundred eight practicing neuro-ophthalmologists (81.3% United States, 50.2% females, age range <35 to >65, mode 35–44 years) participated in the survey. Utilization of all telehealth modalities increased from pre-COVID to peri-COVID (video visit 3.9%–68.3%, P < 0.0005, remote interpretation of testing 26.7%–32.2%, P = 0.09, online second opinion 7.9%–15.3%, P = 0.001, and interprofessional e-consult 4.4%–18.7%, P < 0.0005, McNemar). The majority selected access, continuity, and patient efficiency of care as benefits and data quality as a barrier. Telehealth was felt to be most helpful for conditions relying on history, external examination, and previously collected ancillary testing and not helpful for conditions requiring funduscopic examination.
Conclusions:
Telehealth modality usage by neuro-ophthalmologists increased during the COVID-19 pandemic. Identified benefits have relevance both during and beyond COVID-19. Further work is needed to address barriers in their current and future states to maintain these modalities as viable care delivery options.
Telehealth, the delivery of health care services where patients and providers are separated by distance and sometimes time, was historically a relatively small component of the entire health care delivery system. During the COVID-19 pandemic, when minimizing face-to-face contact became a primary strategy to reduce virus transmission, public health policy changes incentivized health care providers and systems to accelerate implementation and utilization of telehealth services (1,2). Although there are some universal benefits and challenges to the utilization of telemedicine, there are also specialty-specific nuances (3).
Before the COVID-19 pandemic, a minority of neuro-ophthalmologists used telehealth services to improve efficiency of and access to care. As part of the audience response questions at a recent telehealth symposium, planned pre-COVID and delivered on March 9, 2020, at the annual meeting of the North American Neuro-Ophthalmology Society (NANOS), 4% of attendees reported using telehealth video visits and 21% reported performing remote interpretation of testing as part of their clinical practice (T. Thebeau, BS, personal communication, NANOS). The goal of this study is to characterize changes in telehealth utilization by neuro-ophthalmologists during the COVID-19 pandemic as well as perceived benefits, barriers, and utility. Select synchronous and asynchronous telehealth methodologies were considered (Box 1).
Box 1. Definitions of Telehealth Modalities Included in This Study.
Video visits are real-time (synchronous) encounters between a provider and a patient separated by location. The provider is able to obtain a history from the patient, perform external examination, and review previous clinical data, then counsel the patient and make decisions for management of the patient's care. Regulations on patient and provider location, medical liability, and billing and reimbursement have evolved rapidly during the pandemic.
Remote interpretation of testing is where the patient obtains a test separately from a direct encounter with a provider; the provider interprets the test and provides a report to a referring provider separately. Relevant tests in neuro-ophthalmology including visual fields, ophthalmic photography, and electrophysiology. Excluded from this definition is the CPT/HCPCS code G2010 (remote review/interpretation of remote patient data), in which an established patient submits a photograph or video to a provider for review and interpretation to determine whether or not the patient needs to be seen in-person urgently.
Online second opinions are asynchronous encounters between the provider and a new patient (i.e., not previously seen in their in-person practice). Typically, they are administered through a third party vendor, are initiated by the patient, and consist of the provider's review of the patient's medical records and patient questions, followed by a written report to the patient (19,20).
E-consults (or interprofessional consults) are asynchronous and sometimes synchronous encounters between the consulting provider and a referring provider about new or established patients without any communication with the patient. These consults are requested by the referring provider (with patient consent) and consist of a review of the patient's medical records by the consulting provider and sometimes verbal discussion with the referring provider. The consulting provider then provides a written report to the referring physician. This definition is in accordance with the CPT/HCPCS codes 99446-99449 and 99451.
METHODS
This study is a survey of neuro-ophthalmologists in independent clinical practice. Exclusion criteria were nonindependent practice (e.g., resident, fellow-in-training, or student) or inactive clinical practice (e.g., retirement). The population was sampled in a nonrandom fashion through an email sent to members of NANOS, the largest organization in the world for the clinical subspecialty of neuro-ophthalmology, with 16% of members residing outside the United States. The study was deemed exempt by the Stanford Institutional Review Board. Participants were survey respondents who agreed to the parameters of the study and confirmed eligibility before proceeding with survey questions.
Survey Content
Demographic questions included country of residence, state of residence for US participants, age category, gender, and board certification(s) (neuro-ophthalmologists train initially in neurology and/or ophthalmology). Clinical practice questions included practice setting, proportion of income derived from clinical revenue, and electronic medical record (EMR) utilization, all of which were categorical.
Participants were asked about the use of synchronous (video visits) and asynchronous (remote interpretation of tests, second-opinion reviews, and e-consults) telehealth in their personal clinical practice before the COVID-19 pandemic (for US participants, before March 1, 2020), during the COVID-19 pandemic (March 1, 2020, through dates of survey May 1–15, 2020), and looking to the future. Telephone visits, virtual check-ins, and online patient portal communications were not included in this study.
Perceived benefits of synchronous telemedicine (video visits) were collected only from those who use it, whereas all participants were asked about barriers. Questions about benefits and barriers were presented as multiple-choice responses where multiple responses could be selected. Additional comments were collected as free text. Participants were asked for their opinion (helpful, somewhat helpful, or not helpful) on the utility of video visits in the evaluation and management of select neuro-ophthalmic conditions. See the online supplemental material for full survey questions (see Supplemental Digital Content, Supplement 1, http://links.lww.com/WNO/A433).
Survey Delivery
The survey was implemented on an electronic, web-based platform (SurveyMonkey, San Mateo, CA) and distributed through email to members of NANOS using the organization's member listserv on May 1, 2020. Two additional reminders were sent. The survey was open from May 1–15, 2020. No identifying information was collected.
Analysis
Responses to categorical survey questions are reported as proportions. Responses to numerical responses are reported as mean and 95% confidence interval (CI). Responses to free text questions are reported qualitatively. Country of residence was collapsed to US and non-US because of small numbers in most non-US countries. For US participants, states were grouped by US census regions (west, midwest, south, and northeast) for reporting purposes.
Free text comments for video platform use, benefits of video visits, and barriers to video visits were analyzed qualitatively through thematic grouping by the authors. For any comments on the same issue generated by multiple participants, a new response category was generated for inclusion in quantitative analysis, noting that these are likely underestimates because they were not specifically queried as the other items were.
Utilization of different telehealth modalities was compared between US and non-US participants for both the pre-COVID and peri-COVID time frames using the chi-square test or Fisher exact test when a cell size was less than 10. Change in utilization of each telehealth modality was compared pre-COVID and peri-COVID using the McNemar test. Ordinal age and clinical revenue categories were compared between users and nonusers of peri-COVID synchronous telehealth using the Mantel–Haenszel test for trend. Clinical practice environment and board certification were compared between users and nonusers of peri-COVID synchronous telehealth using the chi-square test. Proportions of participants perceiving barriers to use of synchronous telemedicine were compared between users and nonusers of synchronous telemedicine peri-COVID using the chi-square test. P < 0.05 was the threshold for statistical significance. Statistical analysis was performed using SPSS 26 (IBM Inc).
RESULTS
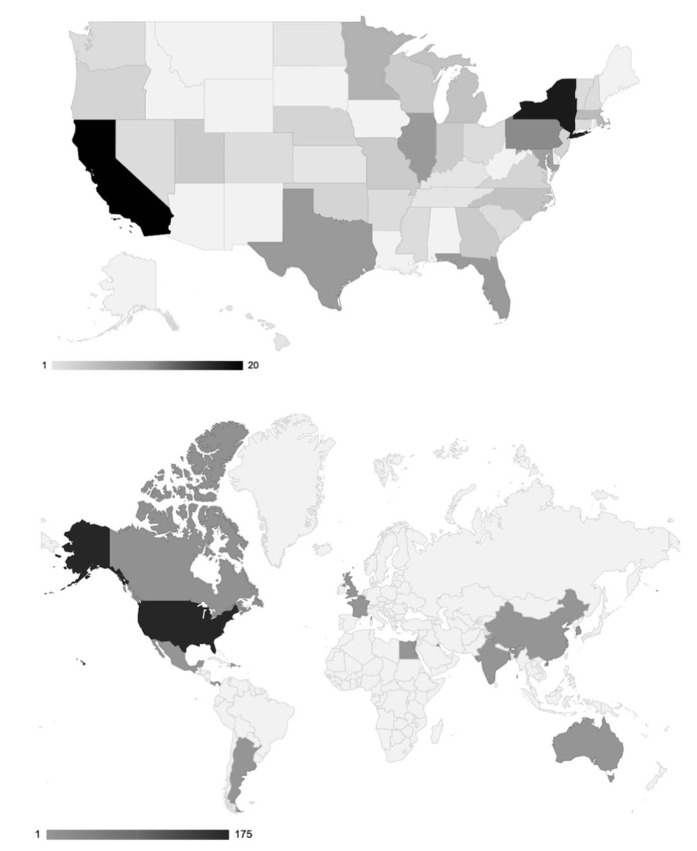
The survey invitation was delivered through email to 813 people (756 nontrainees). Two hundred fourteen responses were received. All confirmed independent practice and agreed to participation. Six did not answer any questions beyond demographics and were excluded from further analysis. Thus, 208 respondents were included in the final analysis (Table 1). The participants were mostly from the United States (81.3%, Fig. 1), with fairly even age and gender distribution. The US/non-US distribution is similar to that for NANOS membership (84% US and 16% non-US). A recent comprehensive effort to count the number of neuro-ophthalmologists in the United States identified 386 individuals in active clinical practice (187 clinical full-time equivalents) (L. Frohman, Personal communication, NANOS). Thus, we estimate that the US survey participants represent a 54% nonrandomized sample of the population of US-practicing neuro-ophthalmologists.
TABLE 1.
Description of survey participants
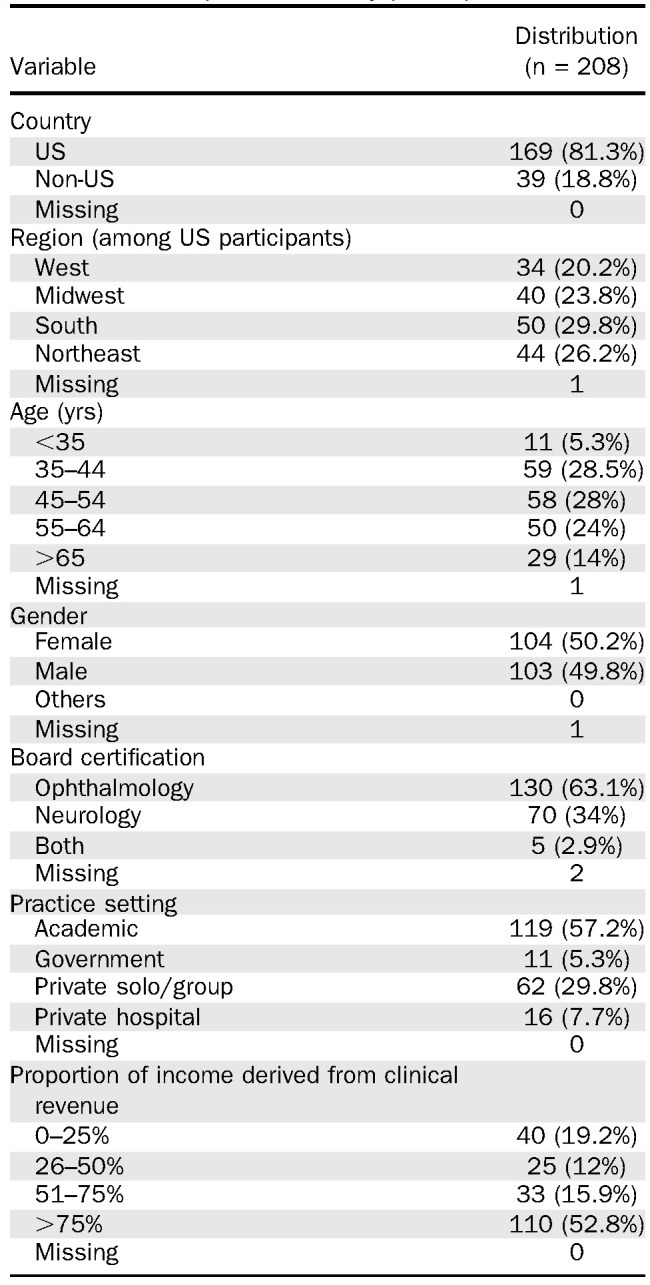
FIG. 1.
Geographic distribution of survey participants: Shade of world map (upper) and US map (lower) corresponds to the number of participants from each country (upper) and US state (lower).
Survey participants came from ophthalmology and neurology backgrounds (2:1). Multiple practice environments were represented with the majority in academic practice. Over half of participants derived more than 75% of their income from clinical revenue. More than 90% of participants reported using an EMR. About half had attended the telehealth symposium presented at the NANOS 2020 Annual Meeting on March 9, 2020. Among symposium attendees, two-thirds reported participating in the audience response questions at the symposium.
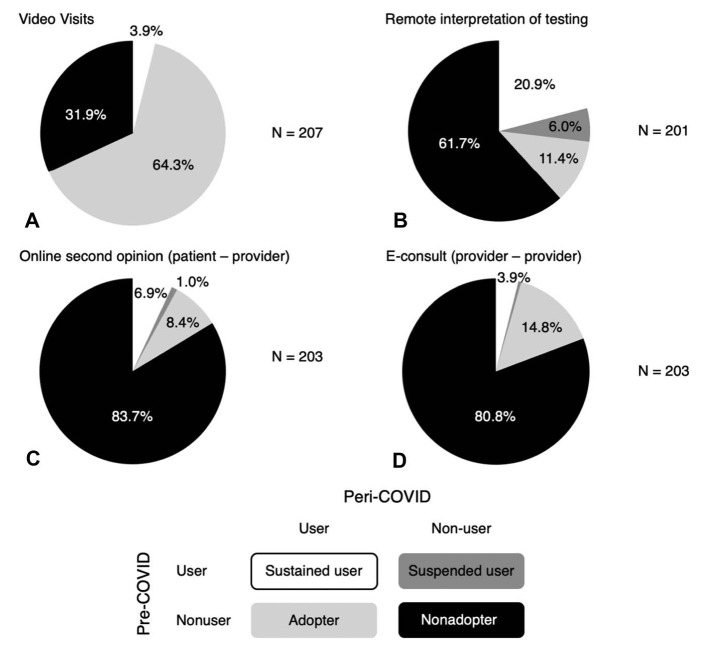
Video Visits
Before the COVID-19 pandemic, 3.9% (5.1% non-US and 3.6% US, P = 0.65 Fisher exact) of participants used video visits; of those participants using video visits, 87.5% performed 1–10 video visits per week. 12.6% of nonusers reported it was available to them. During the COVID-19 pandemic, 68.3% (38.5% non-US and 75.1% US, P < 0.0005, chi square) of participants used video visits (P < 0.0005 vs pre-COVID, McNemar; Fig. 2A). This figure included all pre-COVID users and 66.8% of pre-COVID nonusers. Among nonusers, it was available to 33.4%, of interest to 38%, and not of interest to 29%.
FIG. 2.
Changes in neuro-ophthalmologist telehealth service utilization during the COVID-19 compared with immediately prior. Each pie represents self-reported status of survey participants with regard to utilization of telehealth modalities in their clinical practice peri-COVID according to pre-COVID utilization of different telehealth modalities (Box 1 for definitions): Video visits (A), remote interpretation of ancillary testing (B), online second opinion (C), and E-consult (D).
Video visit use peri-COVID was higher in younger survey participants (72.3% <35 years old, 69.5% 35–44 years, 79.3% 45–54 years, 64% 55–64 years, and 48.3% ≥65 years old, P = 0.04, Mantel–Haenszel test for trend) and among those with neurology board certification (84.3% vs 59.2% ophthalmology, P = 0.001). Reasons for not adopting (available/not using, not available/interested, or available/not interested) did not differ by board certification (P = 0.88, χ2). Use was higher in academic, private solo/group, and private hospital–based practice than government-based practice (73.1%, 64.5%, and 75.0% vs 27.3%, P = 0.01 χ2). However, government-based practice participants were disproportionately outside the United States (72.7%), which confounds this relationship. Use did not differ by the proportion of revenue derived from clinical income (P = 0.58, Mantel–Haenszel).
The majority of peri-COVID video users (64%) saw 1–10 video visits per week. 27.4% saw 11–20 and 3 participants saw >40. Many platforms were used, led by EMR integration (41.5%), with Zoom, Doxy.me, FaceTime, and Doximity, all having >10 users. Many users used more than 1 video platform.
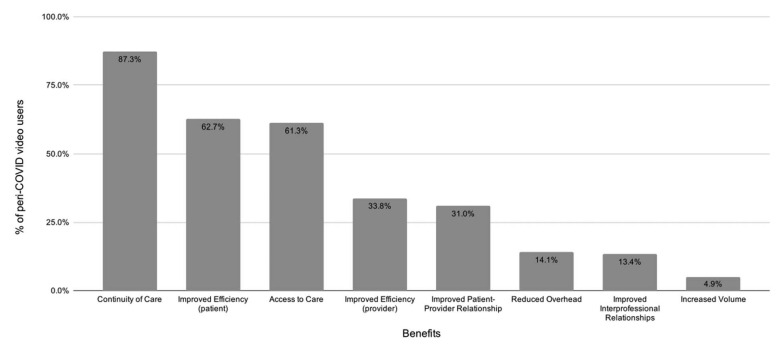
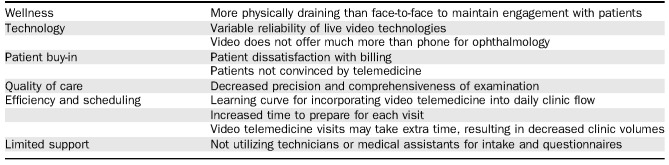
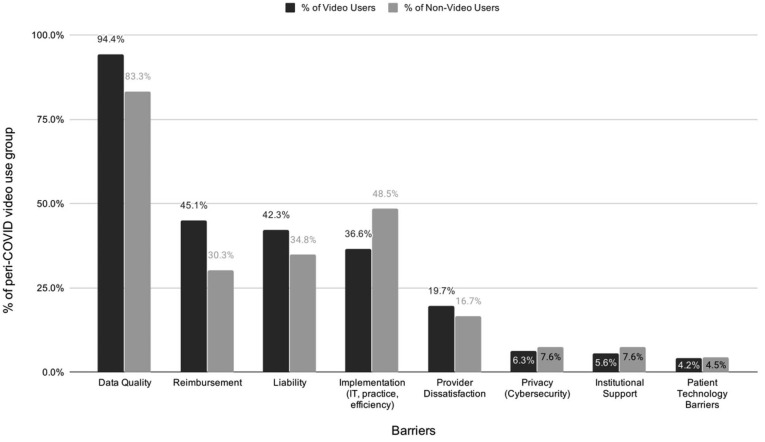
More than 50% of peri-COVID video users selected benefits of improved access to care, continuity of care, and efficiency of care for the patient (Fig. 3). Selected barriers were similar between peri-COVID video users and nonusers, except for reimbursement (45% users and 30% nonusers, P = 0.04 chi square) and data quality (90% users and 83% nonusers, P = 0.01 chi square). Data quality was the barrier selected by the largest proportion of both video users and nonusers (Fig. 4). Free text comments identified multiple other barriers and disadvantages of telehealth that had not been included in the multiple-choice options (Table 2). Assuming continued telehealth reimbursement, 73.9% of users plan to continue video visits in their practice after public health emergency, whereas 17.6% are unsure.
FIG. 3.
Benefits of video telehealth selected by neuro-ophthalmologists who are users of video visits during COVID-19: Each bar is the proportion of peri-COVID video users (n = 141) who selected that item as a benefit to video telehealth. Benefits are ordered by the proportion of peri-COVID video users selecting it.
FIG. 4.
Barriers to video telehealth selected by neuro-ophthalmologists according to video telehealth user status during COVID-19: Each bar is the proportion of peri-COVID video users (black, n = 141) or nonusers (gray, n = 66) who selected that item as a barrier to video telehealth. Patient technology barrier was not included in the survey choices but was added to the analysis based on inclusion in comments by multiple participants. Barriers are ordered by the proportion of peri-COVID video users selecting it.
TABLE 2.
Additional barriers to video telehealth generated by participants
Remote Interpretation of Tests
Before the COVID-19 pandemic, 26.7% of participants (28.7% US and 17.1% non-US, P = 0.21, Fisher exact) performed remote interpretation of tests with a mean of 4.7 per week (95% CI 3.4–6). Leading tests interpreted remotely were visual fields (87%) and optical coherence tomography (79.6%). A minority remotely interpreted visual evoked potentials, electroretinography, and other testing. 17.8% of nonusers preferred to see all patients having testing performed in-person.
During the COVID-19 pandemic, 32.2% of survey participants (30.7% US and 38.9% non-US, P = 0.43 Fisher exact) performed remote testing interpretation (P = 0.09 vs pre-COVID, McNemar) with a mean of 5.3 per week (95% CI 3.8–6.9). 22.2% of pre-COVID users ceased peri-COVID, whereas 15.6% pre-COVID nonusers adopted this practice (Fig. 2B). One participant noted that in-person testing was not being performed at their institution during the pandemic, which limited the opportunity. Ophthalmic imaging and visual fields remained the main types of tests being interpreted without seeing the patient. 84.6% of peri-COVID users plan to continue this practice, whereas 10.8% are unsure.
Asynchronous Telehealth
Before the COVID-19 pandemic, 7.9% (6.6% US and 13.9% non-US, P = 0.17 Fisher exact) and 4.4% (3.6% US and 8.3% non-US, P = 0.20, Fisher exact) of participants used online second opinions and e-consults, respectively. During COVID-19, 15.3% (14.4% US and 19.4% non-US, P = 0.45 Fisher exact) of participants used online second opinions and 18.7% (18.6% US and 19.4% non-US, P = 1.0, Fisher exact) used e-consults (P = 0.001 second opinion, P < 0.0005 e-consult, vs pre-COVID, McNemar, Fig. 2C–D). A limitation in offering second opinion services was prohibition by the participant's institution (24% pre-COVID and 17.8% peri-COVID).
Perception of Utility of Synchronous Telehealth (Video Visits) for Select Neuro-ophthalmic Diseases
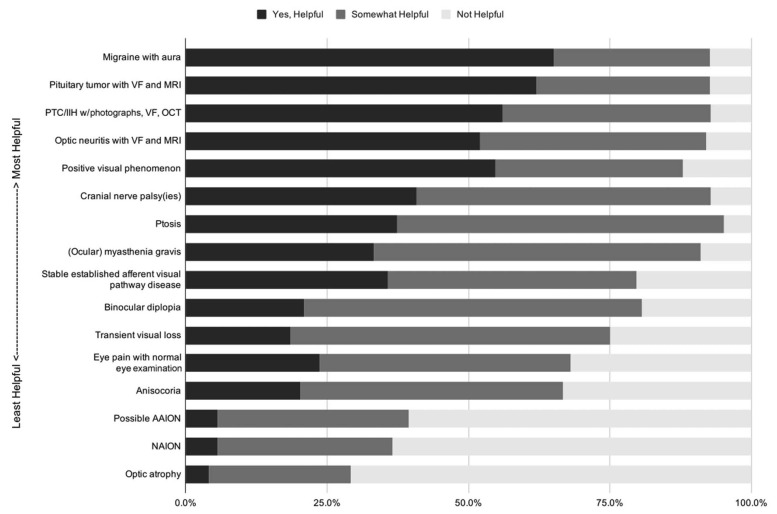
Some participants did not respond to questions of video visit utility for neuro-ophthalmic conditions (Table 3 and Fig. 5). The number of responses per condition varied between 120 and 125; proportions are reported according to the number of participants who selected a category for each condition. Conditions for which >50% of participants indicated video visits are helpful were migraine with aura (65.0%), pituitary tumor with prior visual fields, and MRI results (62.1%). Conditions for which >50% of participants indicated that video visits are not helpful were nonarteritic anterior ischemic optic neuropathy (63.4%), possible arteritic ischemic optic neuropathy (60.5%), and optic atrophy (70.8%).
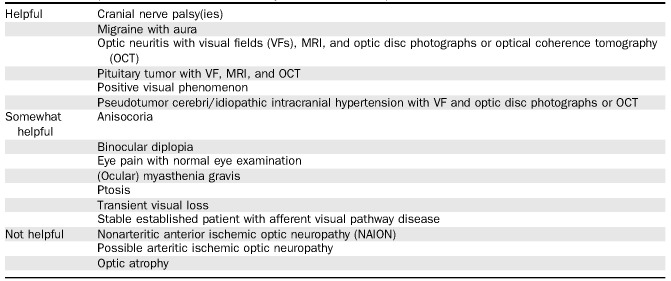
TABLE 3.
Perception of video telehealth utility in select neuro-ophthalmic conditions
FIG. 5.
Perception of video telehealth utility in select neuro-ophthalmic conditions: Each stacked bar represents a condition, with colors representing proportion who gave a response for that condition (n = 120–125), selecting that video telehealth is helpful (black), somewhat helpful (dark gray), or not helpful (light gray). Conditions are ordered by the proportion selecting “helpful.” AAION, arteritic anterior ischemic optic neuropathy; IIH, idiopathic intracranial hypertension; NAION, nonarteritic anterior ischemic optic neuropathy; OCT, optical coherence tomography; PTC, pseudotumor cerebri; VF, visual field.
DISCUSSION
Telehealth modalities as a way to deliver neuro-ophthalmic care have been of interest in the profession for many years, as demonstrated by inclusion of symposia on this topic in the annual meetings of NANOS in 2013 and 2020 (4,5). During the COVID-19 pandemic, interest in and utilization in this area increased throughout the medical profession and in neuro-ophthalmology (3,6). In this study, we demonstrate increased telehealth utilization by neuro-ophthalmologists during the COVID-19 pandemic. It builds upon previous single-institution qualitative reports by quantifying utilization by providers in different practice environments both in and outside of the United States. In addition, a higher level of evidence for perceived benefits, barriers, and utilization is provided, building on what has been previously stated by expert opinion.
Before COVID, the literature supported use of video visits and remote interpretation of testing for delivery of neuro-ophthalmic care (7–9). However, participants both in and outside the United States reported minimal use of video visits, online second opinions, and e-consults and moderate use of remote testing interpretation pre-COVID, similar to what was reported using the audience response system at the 2020 NANOS telehealth symposium. Increased utilization peri-COVID occurred for all modalities, although this increase did not meet the threshold of statistical significance for remote interpretation of testing. Remote interpretation of testing was the only modality surveyed for which some participants ceased utilization peri-COVID. Based on a comment by one participant, this change is likely attributed to cessation of all in-person testing in some practice environments during COVID-19.
Increase in telehealth modality utilization occurred for both US and non-US participants. Adoption was greatest in the younger survey respondents (<35 years old), which may reflect the greater numbers of digital natives within this age demographic (10). Participants board-certified in neurology were higher adopters, in line with the more established role of synchronous telemedicine in neurology (11), whereas ophthalmology telemedicine has traditionally focused more on remote imaging with automated interpretation (12). There was no association between telehealth adoption and proportion of income derived from clinical revenue. Although this lack of association may speak to altruistic motives for provision of care through telehealth modalities, such a conclusion is speculative because participants' motivations were not queried.
Although this survey did not explore the full extent of telehealth's impact on patient care, participants endorsed many benefits. However, the relative merit of these benefits is situational, currently consisting of a global pandemic. It remains to be seen how these benefits are valued as traditional methods of care delivery resume. This benefit is particularly relevant to neuro-ophthalmology where improved patient access and increased efficiencies facilitated by telehealth may address shortfalls in provider access, who are concentrated in major cities and academic centers with an average wait time of 6 weeks, and more than 20% of whom report wait times >3 months (M. Moster, personal communication of internal NANOS survey, NANOS).
Even among telehealth adopters, a high proportion of survey respondents identified data quality concerns including examination limitations as a significant barrier. This study did not ascertain which aspects of the examination posed the greatest barrier for telehealth implementation for our participants, but based on participant responses regarding utility of telehealth in various conditions, we suspect that a primary challenge is obtaining a proper internal assessment of the eyes. Conditions for which video visits were deemed most helpful by participants were those primarily relying on history or external examination to inform management and those for whom vision measurement and/or visualization of the posterior fundus was accomplished through ancillary testing. By contrast, video visits were deemed not helpful for conditions relying on an ophthalmoscopic finding for diagnosis. Of note, there was no consensus on the helpfulness of video visits for any condition, highlighting the heterogeneity of clinical practice style among neuro-ophthalmologists. Studies to validate data acquired through telehealth methods will be important to optimize telehealth care.
Differences in data acquired through telehealth and in-person visits, and the implications of basing management decisions on these, may be the cause of medical liability concerns (13). Before COVID, telemedicine coverage was available as part of liability plans. During this pandemic, new federal acts grant immunity from liability for health care workers acting in good faith. Protections at the state level vary with many states amending existing Good Samaritan statutes to provide broad civil immunity to health care professionals during the pandemic (14).
In the United States, telehealth reimbursement pre-COVID was restricted and disproportionately low compared with in-person visits, acting as a disincentive. Peri-COVID, CMS and many private insurers are covering telehealth visits at a level equivalent to in-person visits, effectively lowering this barrier (15). Future reimbursement regulations remain uncertain and continue to rapidly evolve. Regular provision of education regarding billing and coding for neuro-ophthalmologists will be essential to lower these barriers.
Beyond information technology infrastructure, implementation challenges of integrating video with in-person practice and lack of ancillary support for video visits in current practice models were identified by survey participants. These were noted to have negative impacts on provider wellness. Ongoing use and further adoption of telehealth modalities will require organizations to continue providing and improving telehealth infrastructure. Protocols for incorporating nonprovider staff into telehealth delivery, strategies to optimize patient selection, and scheduling to optimize both efficiency and outcomes and train trainees and providers will need to be expanded and refined (16).
Even when presuming continued telehealth reimbursement, over one-quarter of peri-COVID video visit users either plan to discontinue or remain uncertain regarding future video visit utilization following the end of the public health emergency. This survey did not elicit responses for participants' motives regarding their reluctance to continue telehealth services. Perhaps this reflects the favorable benefit:barrier ratio during this pandemic when traditional care delivery has not been possible; this ratio may revert post-COVID, resulting in increased barriers, both broadly (reimbursement and liability) and locally (practice delivery and efficiency).
The main limitations of this study relate to the survey methodology used (17). Specifically, sampling and questionnaire development were performed in an accelerated fashion because of the time sensitivity of the research question. By collecting responses during the COVID-19 pandemic, recall bias was likely minimized. The nonrandomized sample with voluntary response likely biased toward overestimates of adoption given that those not interested likely had reduced rates of participation. Benefits and barriers not specifically queried (e.g., patient technology issues) were likely underestimated. There were areas of interest not captured by the survey including use of phone calls, online portal and email communications with patients, remote interpretation of patient submitted data, and “virtual check-in” encounters, as well as stratifying benefits and barriers pre-COVID, peri-COVID, and post-COVID.
CONCLUSIONS
During a time of pandemic, neuro-ophthalmologists have rapidly adopted telehealth by 17-fold, providing patients with continued access to care and partially recovering revenue lost due to public policies restricting traditional in-person clinical practice patterns. Similar to many neurological subspecialties and in contrast to other ophthalmic subspecialties, neuro-ophthalmology is amenable to telehealth visits, which still allow for careful history taking and external examination to obtain actionable data for patient triage and management (18). The future of telehealth in neuro-ophthalmology remains uncertain. It is a promising modality for continued patient access and practice revenue, but barriers remain, including some over which individual practitioners have limited control, such as federal and state policies on telehealth reimbursement and liability. Important areas for future study include the benefits of telehealth and patient access to neuro-ophthalmic care and strategies to address barriers under practitioners' control, including data quality, practice efficiency, and patient selection.
Author Contributions: H. E. Moss and K. E. Lai contributed equally to this work.
STATEMENT OF AUTHORSHIP
Category 1: a. Conception and design: H. Moss, K. Lai, and M. Ko; b. Acquisition of data: H. Moss, K. Lai, and M. Ko; c. Analysis and interpretation of data: H. Moss and K. Lai. Category 2: a. Drafting the manuscript: H. Moss, K. Lai, and M. Ko; b. Revising it for intellectual content: H. Moss, K. Lai, and M. Ko. Category 3: a. Final approval of the completed manuscript: H. Moss, K. Lai, and M. Ko.
Footnotes
Research to Prevent Blindness unrestricted grant to the Stanford Department of Ophthalmology, NIH P30 086277.
The authors report no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jneuro-ophthalmology.com).
REFERENCES
- 1.Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020;ocaa072 (epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, Curtis S, Roman M, Poon EG, Ferranti J, Katz JN, Tcheng J. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27:957–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grossman SN, Calix R, Tow S, Odel JG, Sun LD, Balcer LJ, Galetta SL, Rucker JC. Neuro-ophthalmology in the era of COVID-19: future implications of a public health crisis. Ophthalmology. 2020;S0161-6420(20)30429-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bruce B, Subramanian P, Ko MW, Chiang M. Telemedicine for Neuro-Ophthalmology. Neuro-ophthalmology Virtual Education Library, 2013:387–419. North American Neuro-Ophthalmology Society 39th Annual Meeting; February 14, 2013; Snowbird Ski Resort, Snowbird, UT. Available at: https://novel.utah.edu/collection/NAM/program/20130214_nanos_telemedicinesympos/year/2013/. [Google Scholar]
- 5.Ko MW, Lai K, Zimmer-Galler IE, Gold DR, Moss HE. Telemedicine and Neuro-Ophthalmology: 20/20 in 2020. North American Virtual Education Library, 2020:259–284. North American Neuro-Ophthalmology Society 46th Annual Meeting; March 9, 2020; Omni Amelia Island Plantation Resort, Amelia Island, FL. Available at: https://novel.utah.edu/collection/NAM/program/20200309_nanos_telemedicine_1/year/2020/. [Google Scholar]
- 6.Lai KE, Ko MW, Rucker JC, Odel JG, Sun LD, Winges KM, Ghosh A, Bindiganavile SH, Bhat N, Wendt S, Scharf J, Dinkin MJ, Rasool N, Galetta SL, Lee AG. Tele-Neuro-Ophthalmology during the age of COVID-19. J Neuroophthalmol. 2020. doi: 10.1097/WNO.0000000000001024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Friedman DI, Rajan B, Seidmann A. A randomized trial of telemedicine for migraine management. Cephalalgia. 2019;39:1577–1585. [DOI] [PubMed] [Google Scholar]
- 8.Bruce BB. Nonmydriatic ocular fundus photography in the emergency department: how it can benefit neurologists. Semin Neurol. 2015;35:491–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.VI L, JA L. Visual Fields with Interpretation Only—a Preliminary Evaluation. Neuro-ophthalmology Virtual Education Library, 2014:370 North American Neuro-Ophthalmology Society 40th Annual Meeting; March 4, 2014; Rio Grande, Puerto Rico. Available at: https://collections.lib.utah.edu/ark:/87278/s6sx9kzz. [Google Scholar]
- 10.Telehealth Index: 2019 Consumer Survey. 2020. Available at: https://static.americanwell.com/app/uploads/2019/07/American-Well-Telehealth-Index-2019-Consumer-Survey-eBook2.pdf. Accessed May 8, 2020. [Google Scholar]
- 11.Wechsler LR. Advantages and limitations of teleneurology. JAMA Neurol. 2015;72:349–354. [DOI] [PubMed] [Google Scholar]
- 12.Rathi S, Tsui E, Mehta N, Zahid S, Schuman JS. The current state of teleophthalmology in the United States. Ophthalmology. 2017;124:1729–1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Public Readiness and Emergency Preparedness Act. 2020. Available at: phe.gov/Preparedness/legal/prepact/Pages/deault.aspx. Acccessed May 26, 2020. [Google Scholar]
- 14.Liability Protections for Health Care Professionals During COVID-19. 2020. Available at: https://www.ama-assn.org/practice-management/sustainability/liability-protections-health-care-professionals-during-covid-19. Accessed May 20, 2020. [Google Scholar]
- 15.Medicare Telehealth Frequently Asked Questions (FAQs). 2020. Available at: https://edit.cms.gov/files/document/medicare-telehealth-frequently-asked-questions-faqs-31720.pdf. Accessed April 14, 2020. [Google Scholar]
- 16.Afshari M, Witek NP, Galifianakis NB. Education Research: an experiential outpatient teleneurology curriculum for residents. Neurology. 2019;93:170–175. [DOI] [PubMed] [Google Scholar]
- 17.Draugalis JR, Coons SJ, Plaza CM. Best practices for survey research reports: a synopsis for authors and reviewers. Am J Pharm Educ. 2008;72:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saleem SM, Pasquale LR, Sidoti PA, Tsai JC. Virtual ophthalmology: telemedicine in a covid-19 era. Am J Ophthalmol. 2020;S0002-9394(20)30214-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baum S. Can a virtual specialist consult program help hospitals break down geographic barriers. MedCity News. 2015. Available at: https://medcitynews.com/2015/11/virtual-specialist-consults/. Accessed July 3, 2020. [Google Scholar]
- 20.Reddy S. New ways for patients to get a second opinion: online services from established medical centers and independent businesses. Wall Street J. 2015:2015 Available at: wjs.com/articles/new-ways-to-get-a-second-opinion-1440437584. Accessed July 5, 2020. [Google Scholar]