Coronavirus disease 2019 (COVID-19) has the world in a firm grip. Individuals everywhere face challenges among novel conditions. As a result, countless unplanned or natural experiments (NEs) with health and disease, where conditions are altered in a way that is not within researchers’ control, are underway.1 Such experiments can be tantalizing, with possibly immense statistical power and causal insights that would otherwise not be achievable in controlled experimental studies or nonexperimental observational studies.
According to the New York Times, a 40% to 60% reduction in myocardial infarctions (MIs) during the pandemic has been observed anecdotally. Related NEs abound with questions: “Are MI rates really down?” “How many MIs may be missed or misdiagnosed?” “Do people with mild MI no longer visit hospitals because they fear contracting COVID-19?”
NEs are unique means to understand how policies and large-scale interventions may impact health.2 However, although the impact of COVID-19 gives great statistical power, this comes with great responsibility. This article outlines 4 ethical and scientific imperatives for the study of NEs arising from the COVID-19 pandemic. It focuses on physical distancing (PD) as a key intervention that triggers NEs.
PD and NE Possibilities
PD is key to tackling the COVID-19 crisis in almost all countries worldwide. A century ago, PD helped to control the great influenza pandemic, and is helping again today; however, it resembles a black box in terms of nonvirus health consequences. To cope with, and exit from, potentially several cycles of PD, we must understand and weigh virus details on the one hand against possible effects of PD—including benefits and collateral damage—on the other (Figure).
Figure.
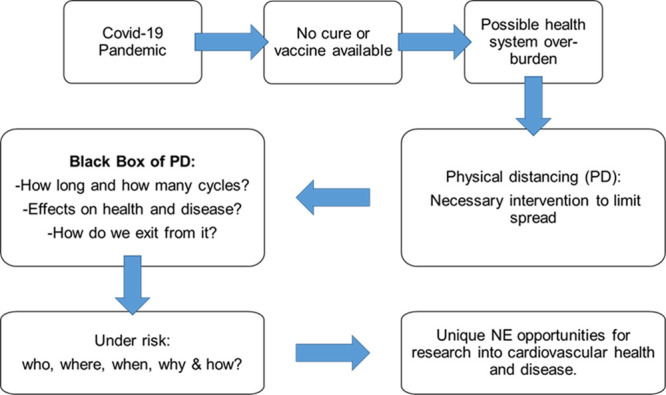
COVID-19 pandemic, physical distancing (PD), and arising natural experiments (NEs) as unique opportunities for cardiovascular research and beyond.
Important questions regarding PD-associated effects on cardiovascular risks abound. “Does psychosocial strain as a potential mediator of coronary disease develop or increase with ordered restrictions on moving, working, and living?” “How does reduced daylight from outdoor exposures and lost temporal organization usually provided from workplaces and schools affect circadian rhythms and MI risk?”3
NE Recommendations
According to The UK Medical Research Council, “[T]he case for adopting a natural experimental approach is strongest when: there is a reasonable expectation that the intervention will have a significant health impact, but scientific uncertainty remains about the size or nature of the effects; an RCT [randomized, controlled trial] would be impractical or unethical; and the intervention or the principles behind it have the potential for replication, scalability or generalisability.”2 We identify 4 additional ethical and scientific imperatives.
Imperative 1: Be Alert for NEs and Collect Data Now
In unanticipated times with strong potential for NEs, scientists must have the will and the antenna to identify what should be studied with priority and what can provide added value. Other research may have to be put aside as long as NEs are ongoing. Some data can only be collected now or never, and scientists must adapt quickly to important, rapidly emerging research gaps.
Imperative 2: Avoid the “Everest Fallacy”
Although scientists must collect and analyze data, unfocused climbing expeditions around new mountains of data must be avoided. The answer to “Why do you study these data?” must not be the same as the English mountaineer George Mallory’s answer to the question “Why do you want to climb Mount Everest?”—“Because it is there.” NEs should not be fishing expeditions in vast pools of data. Sound hypotheses should guide ethical science.
Preferably, researchers will ensure relevant hypotheses to explore NEs are established. However, the very nature of unplanned experiments in combination with Imperative 1 can imply that data may be collected for unspecified hypotheses. Ultimately, careful judgment is needed to decide whether hypotheses can be explored within the NE from which they originate.
Imperative 3: Apply Principles of Research Ethics
Whereas NEs do not require research ethics committee approval before they begin (by their very nature), researchers must adhere to ethical principles.4 For instance, whenever NE duration allows it, ethical approval from research ethics committees should be obtained while collecting and analyzing arising data. Privacy or confidentiality could still be breached in analysis and findings about different demographic groups must be reported in ways that minimize the potential for discrimination.
NEs can raise ethical issues4 that should be considered by a research ethics committee, such as the identification of “adventitious harm” from poorly implemented public health policies or harmful individual behaviors. For example, if researchers were to detect widespread infraction of PD restrictions, an ethical dilemma is presented: Should transgressions be reported to authorities, potentially disrupting the NE, or should they continue to be observed?4
Imperative 4: Be Prepared to Intervene if Necessary Before the NE Ends
Researchers might have an ethical duty to try to modify NEs or provide evidence geared toward modifying or stopping the intervention. This would be both an ethical and scientific requirement if an NE conveys intolerable side effects or if researchers uncover evidence of serious harm. If there is no option to stop the intervention, modifying strategies such as organizing social support for people living in precarious conditions exacerbated by an intervention such as PD should be considered. In instances showing early benefit, early translation or transfer to other settings may be required. One example is disseminating an app that reduces social isolation in one setting compared with another. Patients with comorbidities such as hypertension or cardiovascular disease may need to be shielded from PD-induced psychosocial strain, which may lead to worse outcomes. Researchers must be conscious of this imperative and become adept at solving such problems.
Conclusions
Because of COVID-19, we are witnessing extensive public health interventions such as PD. How lockdowns impact health and disease of hundreds of millions of people confined to homes—for instance, by affecting risk of MI—must be explored with NEs. Yet “Crises are no excuse for lowering scientific standards,”5 and researchers must always act ethically.
Disclosures
None.
Footnotes
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
References
- 1.Thomson B. The COVID-19 pandemic: a global natural experiment. Circulation 202014214–16doi: 10.1161/CIRCULATIONAHA.120.047538 [DOI] [PubMed] [Google Scholar]
- 2.Craig P, Cooper C, Gunnell D, Haw S, Lawson K, Macintyre S, Ogilvie D, Petticrew M, Reeves B, Sutton M, et al. Using natural experiments to evaluate population health interventions: new Medical Research Council guidance. J Epidemiol Community Health 2012661182–1186doi: 10.1136/jech-2011-200375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crnko S, Du Pré BC, Sluijter JPG, Van Laake LW. Circadian rhythms and the molecular clock in cardiovascular biology and disease. Nat Rev Cardiol 201916437–447doi: 10.1038/s41569-019-0167-4 [DOI] [PubMed] [Google Scholar]
- 4.Dawson A, Sim J. The nature and ethics of natural experiments. J Med Ethics 201541848–853doi: 10.1136/medethics-2014-102254 [DOI] [PubMed] [Google Scholar]
- 5.London AJ, Kimmelman J. Against pandemic research exceptionalism. Science 2020368476–477doi: 10.1126/science.abc1731 [DOI] [PubMed] [Google Scholar]


