Abstract
Communication for non-medication order (CNMO) is a type of free text communication order providers use for asynchronous communication about patient care. The objective of this study was to understand the extent to which non-medication orders are being used for medication-related communication. We analyzed a sample of 26 524 CNMOs placed in 6 hospitals. A total of 42% of non-medication orders contained medication information. There was large variation in the usage of CNMOs across hospitals, provider settings, and provider types. The use of CNMOs for communicating medication-related information may result in delayed or missed medications, receiving medications that should have been discontinued, or important clinical decision being made based on inaccurate information. Future studies should quantify the implications of these data entry patterns on actual medication error rates and resultant safety issues.
Keywords: electronic health record, communication, safety, workaround
LAY SUMMARY
Communication for non-medication order (CNMO) is a type of free text communication order providers use for asynchronous communication about patient care. We conducted a study analyzing a large sample of CNMOs placed in 6 hospitals to understand the extent to which these non-medication orders are being used for medication-related communication. We identified that over 42% of CNMOs contain medication information. We identified large variation in the usage of CNMOs across hospitals, provider settings, and provider types. We also discuss the implications of these usage patterns.
INTRODUCTION
Communication is critical for safe and effective healthcare delivery, yet communication failures contribute to the majority of sentinel events that occur in hospitals1 and 38% of malpractice incidents involve miscommunication between providers.2 The Joint Commission has identified improving provider communication as a priority and included it in their 2019 National Patient Safety Goals.3
Electronic health records (EHRs) are now ubiquitous, with 99% of large hospitals using a certified EHR.4 With the increasing use of EHRs in place of face to face communication,5 it is essential that these technologies support effective communication. EHRs allow communication via structured (eg, computerized provider order entry [CPOE]) and unstructured pathways (eg, clinician notes). Structured information is highly specified and frequently used to convey information such as allergies, medications, and diagnostic testing. Unstructured information may have a general format, such a physician’s progress note with specific sections each containing free text, or may have very few restrictions on what can be entered, such as free text orders. Communication order is a text field of limited characters that allows the physician to place a computerized order with verbatim text for the nurse to follow. This is not a specific document type like a physician progress note or a nurse triage note. They are stand-alone orders like medication or procedure orders that support asynchronous communication. A communication for non-medication orders (CNMOs) is one type of free text communication order used for communication of information not appropriate for structured medication orders. However, anecdotal evidence suggests medication-related information is often included in CNMOs, which can represent a communication workaround and potential EHR usability concerns.
The purpose of this study is to understand the types of information contained in CNMOs, particularly the extent to which CNMOs are being used for medication-related communication. This study also seeks to identify whether this prevalence in using CNMOs to communicate medication-related information varies across hospitals, provider settings, and provider types.
METHODS
We conducted a retrospective analysis of free text CNMOs placed at 6 hospitals on the east coast comprised of 5 clinical settings (ie, Emergency, Inpatient, Outpatient, Ambulatory Service, and Observation). The 6 hospitals are a part of a single health system and have implemented the same large EHR vendor system, with some hospital-level customizations to the EHR. The health system has mix of academic and community hospitals. This study was approved by the health system IRB. We extracted 667 429 free text CNMOs written during 2017, representing 437 128 unique patients. We randomly sampled 26 524 orders for analysis, representing 21 333 unique patients (Raosoft calculator with error ≤ 0.99% and confidence level of 99.9%).6
Some of the 26 524 CNMOs contained identical text, so we analyzed the contents of the 5574 unique free text strings. We then extrapolated the findings to the full set of 26 524 CNMOs.
We coded each CNMO based on the information categories contained in the text, and each CNMO could contain information related to multiple information categories. Information categories were developed iteratively by 2 coders (DJH and SK) on 50 orders randomly sampled from the entire corpus. Differences in coding of information categories were reconciled through consensus by changing definitions or by merging, deleting, or adding information categories. Disagreements between the 2 coders were resolved by the third coder (AZH). Information categories were finalized after 5 rounds when (1) the coders did not make any changes to categories and (2) when there was an Inter rater reliability of at least 0.8 on a sample of 50 CNMOs. The final codebook included sixteen CNMO information categories. Table 1 details the definitions, inclusion, and exclusion criteria, and example text for each information category.
Table 1.
Code book
| Category | Description | Examples |
|---|---|---|
| Medication |
|
|
| ADT |
|
|
| Protocol |
|
|
| Documentation |
|
|
| Transport |
|
|
| Other clinical tasks |
|
|
| Procedure |
|
|
| Lines/tubes/drains |
|
|
| Vitals |
|
|
| Devices |
|
|
| Labs |
|
|
| Contact |
|
|
| Goal |
|
|
| Diet |
|
|
| Education |
|
|
| Non-clinical task |
|
|
Abbreviations: ADT, admission/discharge/transfer; BNP: Brain natriuretic peptide; CBC: Complete blood count; CPAP: Continuous positive airway pressure; CT: computed tomography; EHR: electronic health record; ICU: intensive care unit; LVAD: left ventricular assist device; MRI: Magnetic resonance imaging; NG: nasogastric; NPO: nil per os (nothing by mouth); OR: Operating Room; OT: Occupational therapy; PACU: Post-Anesthesia Care Unit; PO: per os (by mouth); PT: patient or physical theraphy; IV: Intravenous.
RESULTS
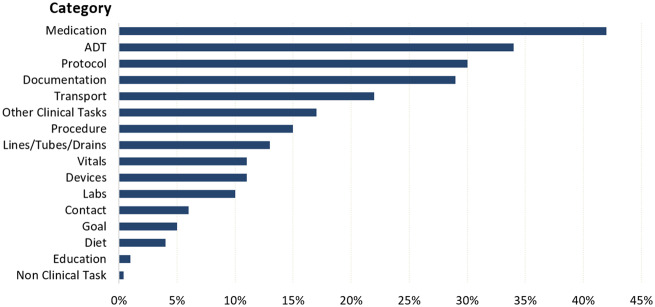
Figure 1 shows the prevalence of each information category within the CNMOs. Forty-two percent of the CNMOs contained information about medications, despite their intention to be used for non-medication-related communication. ADT (admissions/discharges/transfers), protocol, and documentation information were also in the top 4 categories included in CNMOs.
Figure 1.
Prevalence of information categories included in free text communication for non-medication orders. Abbreviation: ADT: admission/discharge/transfer.
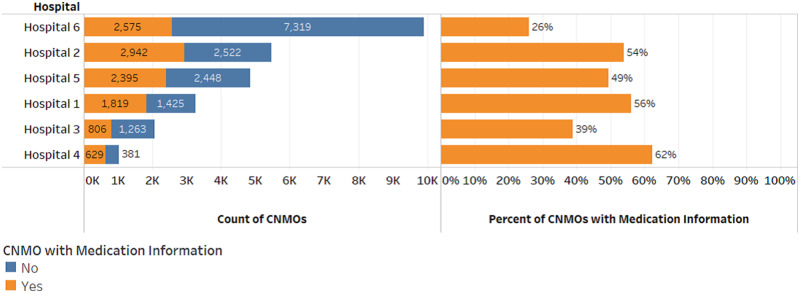
Figure 2 shows the variation in the prevalence of CNMOs containing medication information across hospitals. There was a large range in the total number of CNMOs (1010–9894) and proportion of CNMOs containing medication information (26%–62%) across hospitals. The largest number of CNMOs containing medication information was written at hospital 2 (2942 orders). When normalizing the number of CNMOs containing medication information by the total number of CNMOs written at each hospital, hospital 4 had the highest proportion of overall CNMOs containing medication information (62%), but the lowest total number of CNMOs (1010 orders). Hospital 6 had the lowest proportion of CNMOs containing medication information (26%), but the highest total number of CNMOs (9894).
Figure 2.
Variation in the use of CNMOs for medication information across hospitals. Abbreviation: CNMO: communication for non-medication order.
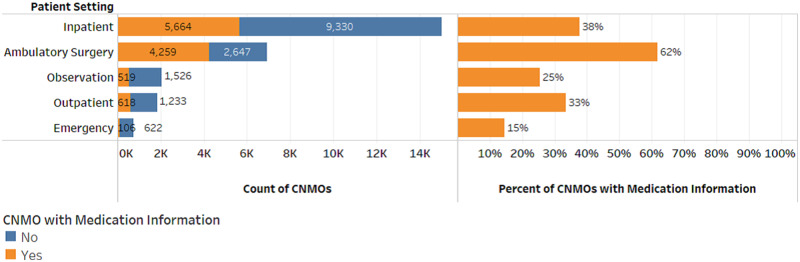
Figure 3 shows the variation in the prevalence of CNMOs containing medication information across patient settings. Like hospitals, there was a large range in the total number of CNMOs (728–14 994) and proportion of CNMOs containing medication information (15%–62%) across patient settings. The largest number of CNMOs containing medication information was written by providers caring for inpatients (5664). When normalizing the number of CNMOs containing medication information by the total number of CNMOs written in each patient setting, the ambulatory surgery setting had the highest proportion of overall CNMOs containing medication information (62%). The inpatient setting had the lowest proportion of CNMOs containing medication information (15%), but the highest total number of CNMOs (14 994).
Figure 3.
Variation in the use of CNMOs for medication information across patient settings. Abbreviation: CNMO: communication for non-medication order.
The prevalence of medication information in the CNMOs also varied across provider types. Fifty-six percent of CNMOs written by nurses contained medication-related information, compared to 37% for nurse practitioners, 27% for resident physicians, and 21% for attending physicians.
DISCUSSION
The presence of medication information in free text CNMOs may pose patient safety risks. For example, if “increase argatroban now by 0.1 mcg/kg/min” is entered in a CNMO but not entered as a medication order, a nurse may not see this information or there may be conflicting rates based on the original order. This may either over or under anticoagulate the patient’s blood if the nurse or ordering provider is working from different information. Safety risks may also arise when CNMOs are used for other standard CPOE order types, such as diet orders. A CNMO requesting a patient to not eat after midnight for a procedure may leave a diet order in place that triggers delivery of breakfast to the patient, potentially resulting in a delay to a procedure or aspiration risk for the patient.
Our findings point to several avenues of future work. Our method of extracting free text EHR orders, and coding and analyzing those data for patterns proved feasible and useful. We anticipate this methodology could be extended to other scenarios where anecdotal evidence suggests there may be potentially unsafe or inefficient EHR data entry patterns.
While we assessed variation across hospitals, patient settings, and provider types, we do not know if differences in data entry patterns exist across different EHR vendor systems. A comparative analysis of a similar health system using a different EHR could provide insight into the impact of interface design on these patterns.
Our findings suggest a need for a robust qualitative analysis to better understand why standard EHR medication orders do not appear to be adequate for communicating medication information. Our initial hypotheses from the note contents are that standard EHR medication orders may be cumbersome or lack some necessary functionalities. For example, 1 free text CNMO asked nurses to cancel the third and fourth runs of potassium as they had an updated lab result for potassium. Canceling part of an order is not supported well in the EHR standard medication orders, so the ordering provider may have used the CNMO as a necessary workaround. The example above creates a potential risk for a commission error, with the patient receiving unnecessary medications. This qualitative analysis must also account for the varied impact of hospitals, patient settings, and provider types on these note entry patterns. The variability in our data may be a reflection complex socio-technical issues and differences in factors such as organizational policies and procedures, patient loads, workflows, communication needs, and local EHR customizations. For example, some CNMOs are used to provide explicit instruction about medication administration, such as, “give medication on call to MRI/operating room” or “give medication A then medication B to prevent side effects”. Another example included holding continuous drip medications instead of discontinuing the order. If the order was canceled, then the remaining medication would have to be thrown out or returned to pharmacy per policy which could result in a delay of restarting the medication if the patient’s condition changed acutely.
The large number of CNMO orders written by nurses may reflect standing nursing protocols and physician initiated verbal orders. Because of these differences, interventions that address the appropriate use of CNMOs will likely need to be tailored to organizations, settings, and providers.
Many studies have identified unintended consequences due to the use of EHRs7,8 and clinicians may not be aware of the unintended consequences or errors associated with using the EHR in ways it was not designed for.9 The use of CNMOs for communicating medication-related information has potential patient safety implications, but future studies should attempt to quantify the implications of these data entry patterns on actual medication error rates and resultant safety issues. We hypothesize that this unintended use of CNMOs may result in delayed or missed medications, receiving medications that should have been discontinued, or important clinical decision being made based on inaccurate information. Additionally, EHR features such as decision support, allergy alerts, and medication interactions typically do not review free text content, creating a significant safety hazard. It would be useful to know the scale and types of the consequences associated with this use of CNMOs.
This study is limited in its analysis of 1 year of data from 1 EHR in a single healthcare system and lack of individual chart review for each CNMO containing medication information. However, this work details a valuable method for understanding EHR data entry practices and brings to light an EHR data entry patterns with potential patient safety implications.
FUNDING
This manuscript was supported by AHRQ R21 HS024755 and AHRQ R01 HS025136.
AUTHOR CONTRIBUTIONS
All authors conceived of and designed the study. SK and DJH extracted the data. SK, DJH, and AZH developed codebook. SK analyzed the data and drafted the manuscript. All authors made critical manuscript revisions and approved the final version for submission.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.Joint Commission. Sentinel Event Statistics Data—Root Causes by Event Type (2004–2015). Sentinel Event Data—Root Causes by Event Type 2016.
- 2. Medical Malpractice in America Boston: CRICO; 2018.
- 3.Hospital: 2019 National Patient Safety Goals. The Joint Commission 2018. https://www.jointcommission.org/assets/1/6/NPSG_Chapter_HAP_Jan2019.pdf Accessed March 19, 2019.
- 4.Office of the National Coordinator for Health Information Technology. Office-based Physician Electronic Health Record Adoption. Health IT Quick-Stat #50. 2019. dashboard.healthit.gov/quickstats/pages/physician-ehr-adoption-trends.php Accessed March 19, 2019.
- 5. Taylor SP, Ledford R, Palmer V, et al. We need to talk: an observational study of the impact of electronic medical record implementation on hospital communication. BMJ Qual Saf 2014; 23 (7): 584–8. [DOI] [PubMed] [Google Scholar]
- 6.Sample Size Calculator by Raosoft, Inc. http://www.raosoft.com/samplesize.html Accessed March 19, 2019.
- 7. Campbell EM, Sittig DF, Ash JS, et al. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc 2006; 13 (5): 547–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ash JS, Sittig DF, Dykstra R, et al. Exploring the unintended consequences of computerized physician order entry. Stud Health Technol Inform 2007; 129 (Pt 1): 198–202. [PubMed] [Google Scholar]
- 9. Sittig DF, Ash JS, Guappone KP, et al. Assessing the anticipated consequences of computer-based provider order entry at three community hospitals using an open-ended, semi-structured survey instrument. Int J Med Inform 2008; 77 (7): 440–7. [DOI] [PMC free article] [PubMed] [Google Scholar]