Abstract
As participants in the California Medicaid 1115 waiver, the University of California San Diego Health (UCSDH) used population health informatics tools to address health disparities. This case study describes a modern application of health informatics to improve data capture, describe health disparities through demographic stratification, and drive reliable care through electronic medical record-based registries. We provide a details in our successful approach using (1) standardized collection of race, ethnicity, language, sexual orientation, and gender identity data, (2) stratification of 8 quality measures by demographic profile, and (3) improved quality performance through registries for wellness, social determinants of health, and chronic disease. A strong population health platform paired with executive support, physician leadership, education and training, and workflow redesign can improve the representation of diversity and drive reliable processes for care delivery that improve health equity.
Keywords: clinical informatics, health disparities, CMS 1115 waiver, population health, health IT
Lay summary
Healthcare informatics that are used to improve quality performance help to address population health disparities. This case study at an academic medical center provides a description of how electronic medical records can provide a foundation for improved data collection, quality performance profiling by demographics, and population health management. Here, we describe how a the federally supported Medicaid waiver initiative helped to support improved data collection, reporting stratified by demographics for 8 key quality measures, and population health infrastructure development. We assert that leadership, training, and end user workflows supported by technology can drive more reliable care that will serve as a foundation for health equity delivered from the health system.
INTRODUCTION
When the US Department of Health and Human Services developed the 2010 Healthy People measures, race and ethnic disparities were a central topic of discussion.1 As we approach 2020, significant trends continue to plague the US healthcare system; for potentially preventable health conditions such as hypertension, obesity, and alcohol and tobacco use.2,3 A limited understanding of disparities is likely to persist if accurate documentation of demographics, cultural competency, and access to inclusive services are not available.4 Minority populations with overlapping subgroups for sexual orientation and gender identity (SO/GI) as well as race, ethnicity, and language (REAL) are associated with increased undue burden of poor health outcomes,5 where stigma combined with vulnerable population status can lead to additional challenges for patients seeking health services.6 Existing quality measurement practices have been insufficient to identify and reduce racial and ethnic disparities.7 SO/GI disparities have been identified in cancer, heart disease, depression, and anxiety.8 Contributing factors for gender minority disparities include poverty, disproportionate uninsured status, delayed access to care, utilization of emergent primary care services, and exposure to violence.6
The incorporation of health information technology (HIT) has been proposed as an important tool for the reliable collection of race, ethnicity, language, sexual orientation, and gender identity to aid in identifying disparities.9 The Centers for Medicare and Medicaid Services and the Office of the National Coordinator have required electronic health records (EHRs) to be enabled for the data collection of SO/GI, but effective data collection in healthcare environments also requires consideration of provider training, patient education, and non-discrimination policies.10 Currently, the clinician workforce frequently lacks broad-based education to address sexual and gender minority health, contributing to patient perceptions of discomfort or offense.11 Collection of SO/GI through HIT can serve as an important tactical solution to reduce health disparities through standardization, automation, and EHR-based clinical decision support tools. While traditionally underserved communities may have access to mobile technology including smartphones, sociodemographic characteristics including lack of access to internet, English as a second language, and physical or mental challenges may contribute to persistent disparities.12
Publicly funded programs such as the Social Security Act Section 1115 waiver enable states to design innovative incentive programs addressing disparities in care, while improving quality, access, and efficiency.13 In California, the Public Hospital Redesign and Incentives in Medi-Cal (PRIME), a core program of the 1115 Medicaid waiver, provides incentive support of up to $3.26 billion to public hospitals and health systems state-wide for value-based care transformation with emphasis on prevention, early diagnosis, and treatment. The PRIME program provides payment for achievement of 90th percentile or incremental annual increase by a minimum of 10% gap closure compared with prior year performance. Sites are required to stratify 8 quality measures by race, ethnicity, language, sexual orientation, and gender identity data and develop initiatives to identify, monitor, and reduce health disparity for at least one measure.14,15 Universal screening for depression using the Patient Health Questionnaire (PHQ) 2 and 9 with follow-up has been demonstrated to have clinical utility across demographic groups.16
We present a case study at an academic health system to demonstrate how reliable care can be engineered through (1) standardized collection of race, ethnicity, language, sexual orientation, and gender identity data, (2) stratification of quality measures, and (3) EHR-based registries.
METHODS
Patients were eligible for inclusion either through assignment to University of California San Diego Health (UCSDH) for primary care by a Medicaid Managed Care Plan, or by completion 2 encounters in the measurement year with their UCSDH primary care medical home. EHR data were collected in our vendor system (Epic® Systems, Madison, WI, United States) in routine workflows. We tracked compliance with the PRIME program guidelines for complete documentation of demographic information of (1) REAL which was classified according to the National Library of Medicine17–19 and (2) SO/GI. Eight quality measure performances were then stratified by demographics. De-identified aggregate data sets were compared according to measure specifications from metric stewards across performance years, baseline year beginning July 1, 2016 through current, December 31, 2019. Population health informatics tools based on registries within the EHR were used to cohort, drive clinical decision support, and enable outreach (Table 1).
Table 1.
Summary of approach to health disparity through demographic data collection, stratification quality measures, and registry-based infrastructure
| Population health informatics approach | Quality measurement | Informatics workflows and registry infrastructure |
|---|---|---|
| Standardized demographic data collection |
|
Structured standardized fields for data collection of REAL and SOGI
|
| Stratification of quality measures by race, ethnicity, language, sexual orientation, and gender identity |
|
|
| Electronic health record-based registries to support population health informatics infrastructure |
|
Registry-based rule driven patient engagement, clinical decision support tools for providers, and care gap outreach
|
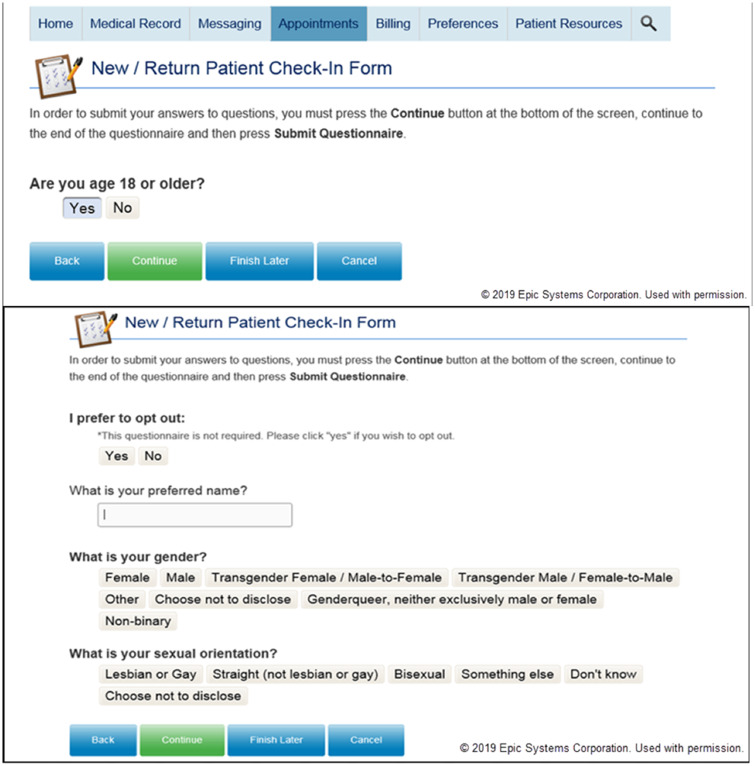
Informatics driven tactics for improved demographic documentation
To enhance our detailed demographic data capacity, we enabled enterprise-wide documentation of REAL in multiple workflows but devised mandatory completion in registration. In March of 2018, we launched enterprise wide adoption of sexual orientation and gender identity documentation. We built new electronic tools for clinical documentation; enabled patient web portal completion using the electronic check-in, or as part of ad hoc patient access to the questionnaire (Figure 1); revised terms that would be clinically meaningful and culturally appropriate; and created of enterprise-wide training. Electronic tools for collection for gender identity in the EHR were customized based on the recommendation of the SO/GI workgroup including more than 40 stakeholders inclusive of our community partners, the Pacific AIDS Education and Training Center as well as the University of California San Diego LGBT Resource Center. The SO/GI workgroup produced a 40-min web-based training that included concepts from the Fenway Institute (publically available with permission) as well as locally developed custom content. Cultural competency and technology use training were provided to more than 3800 healthcare providers (December 2019; UCSDH, Learning Health System internal data). Documentation completion was tracked as a quality measure with patients included in the numerator based on EHR data collection of SO/GI or specific notation in the patient record that a patient opted out or chose not to disclose.
Figure 1.
Patient data entry of gender identity and sexual orientation.
Types of registry driven population health interventions for quality measures
We systematically constructed EHR-based registries over the past decade to better identify patients needing wellness, social determinants of health, and chronic disease screening and management. As of December 2019, we had constructed more than 100 EHR-based registries. These registries serve to underpin the standardization of cohort and metric definition that are crucial for deploying the right care to the right patient. We have included a high-level summary of the registry-based interventions in Table 1 and will further provide 2 examples of how quality measures are supported by the registry infrastructure.
In order to improve the consistency of mental health screening, we built a depression registry to help identify patients with depression as well as patients due for follow-up. We commenced universal depression screening using the PHQ-2 including deployment for patient completion as part of electronic check-in, and used a score of 2 or higher to trigger PHQ-9 completion. A PHQ-9 score equal to 10 or greater has a reported sensitivity of 88% and specificity of 88% for major depression.20 Providers are given a best practice alert via a red banner in the header for patients with high risk and clicking the banner results in linkage to pre-set orders for medication therapy and mental health referrals. Post-encounter, patients are monitored using the registry by behavioral health clinicians which are on-site available at 7 of our primary care sites to provide outreach and engagement to re-assess patient status.
Our wellness, tobacco, hypertension, and diabetes registries also support a number of age-based routine quality screening, intervention, and follow-up within our EHR as shown in this provider-specific performance dashboard (Figure 2). This dashboard has a hyperlink to patient-level outlier reports that can be accessed by clicking the title of the quality measure. The patient list within the EHR enables clinically appropriate interventions to patients with care gaps whether that result in telephonic outreach, bulk orders, or patient portal-based bulk messages. At baseline, we identified differences in tobacco screening and follow-up by race for our Black/African American patients, 94.29% (1288/1366) at baseline compared with the population average, 97.02% (34 415/35 473). We altered our primary care workflows mandating through a hard stop so that the back office staff rooming the patient is forced to document tobacco status, and for user’s readiness to quit and counseling. Patients who have care gaps can be accessed through the tobacco registry-based report and sent either individual or bulk group intervention such as education, referral, or communication.
Figure 2.
Physician performance report in the EHR based on registry inclusion with direct linkage to patients with care gaps.
RESULTS
Of the total 17 designated public hospitals in California participating in the PRIME program with submitted data through June 20, 2018; performance targets were met or exceeded by 16/17 for complete REAL documentation and for 15/17 for sexual orientation and gender identity.21 We increased the demographic documentation for complete REAL from 27.10% (9672/35 696) at baseline to 94.48% (38 956/41 233) December 31, 2019. We improved complete documentation of SO/GI from 0.15% (53/34 907) at baseline to 71.34% (28 744/40 293) December 31, 2019. Eight quality measures were stratified by year across REAL and SO/GI as shown in Table 2. We eliminated our difference in tobacco assessment and counseling with the population performance 98.72% (40 443/40 968) as compared to the Black/African American race 98.83% (1524/1542) as of December 31, 2019.
Table 2.
Sample of stratification of 3 quality measures by race, December 2019
| Quality measure | Race | Percentage of population (%) | Denominator | Numerator | Numerator/denominator (%) |
|---|---|---|---|---|---|
| Screening for clinical depression and follow-up | American Indian or Alaska Native | 0.29% | 87 | 64 | 73.56% |
| Asian | 17.46% | 4800 | 3872 | 80.67% | |
| Black or African American | 3.58% | 1014 | 793 | 78.21% | |
| Native Hawaiian or Other Pacific Islander | 0.44% | 132 | 98 | 74.24% | |
| Other Race or Mixed Race | 12.89% | 3719 | 2859 | 76.88% | |
| Unknown (Cannot or refuses) | 2.03% | 581 | 451 | 77.62% | |
| White | 63.29% | 18 576 | 14 033 | 75.54% | |
| Blank | 0.01% | 7 | 2 | 28.57% | |
| Total | 18.16% | 28 916 | 22 172 | 76.68% | |
| Tobacco assessment and counseling | American Indian or Alaska Native | 0.32% | 131 | 129 | 98.47% |
| Asian | 14.11% | 5727 | 5686 | 99.28% | |
| Black or African American | 3.78% | 1543 | 1523 | 98.70% | |
| Native Hawaiian or Other Pacific Islander | 0.43% | 176 | 175 | 99.43% | |
| Other Race or mixed Race | 12.75% | 5215 | 5138 | 98.52% | |
| Unknown (cannot or refuses) | 1.73% | 712 | 696 | 97.75% | |
| White | 66.86% | 27 314 | 26 948 | 98.66% | |
| Blank | 0.02% | 8 | 8 | 100.00% | |
| Total | 33.00% | 40 826 | 40 303 | 98.72% | |
| Colorectal cancer screening | American Indian or Alaska Native | 0.30% | 64 | 51 | 79.69% |
| Asian | 12.84% | 2483 | 2195 | 88.40% | |
| Black or African American | 4.10% | 824 | 701 | 85.07% | |
| Native Hawaiian or Other Pacific Islander | 0.36% | 79 | 61 | 77.22% | |
| Other Race or mixed Race | 10.25% | 2157 | 1751 | 81.18% | |
| Unknown (cannot or refuses) | 1.06% | 256 | 182 | 71.09% | |
| White | 71.08% | 14 226 | 12 148 | 85.39% | |
| Blank | 0.01% | 2 | 1 | 50.00% | |
| Total | 13.99% | 20 091 | 17 090 | 85.06% |
DISCUSSION
In clinical health environments, health information technology has the potential to improve quality of care as well as improving equity-in-care15 to deliver high-reliability healthcare.22 Population health informatics processes should be anchored on a strong foundation of continuous improvement, system-wide training, development of cultural competency, and leadership.23 These activities can enhance our efforts to model, measure, and manage systems to improve health equity.24 We found that a targeted informatics-enabled approach to health equity included patient entered demographic data, culturally inclusive standard work, measurement of health disparities, development of community partnerships, outreach to populations with care gaps by teams trained in cultural competency, and progress supported in celebration by the executive leadership.
One of the most vital steps involves patient engagement for self-documentation of demographics. Next, EHR-based registries aggregate population cohorts to drive both the delivery and exclusion of standard care to the appropriate patients. Tools can more efficiently be used to deliver care through the use of: (1) dynamic order sets,25 (2) health maintenance inclusion of individual needs, and (3) population-level bulk activity. Our outreach activities have been developed by teams that regularly work with the patient education committee to use inclusive terminology in the provision of culturally competent care. Importantly, bulk activities provide necessary system redundancies in an efficient method that help to fill care gaps that can result in complex sociotechnical environments.
This case study is limited by location at an academic medical center, access to indepth technology through registry infrastructure, limited patient population to the PRIME attributed denominator, and disparities by REAL and SO/GI to healthcare access and technology. Reports must be constructed with credible underlying data to help guide interventions for patients with unmet needs.26,27 There are further opportunities to define how HIT infrastructure can better identify and address disparities in an innovative and cost effective means.28,29
The 1115 waiver program provides vital funding to incentivize providers to create high-reliability systems in improving health equity. Innovative approaches to seek, address, and eliminate disparities require programmatic attention requiring fiscal support. PRIME’s role rigorous performance measures and targets drive health care systems and public hospitals toward advanced data capture, stratification of quality measures, EHR-based infrastructure development, and aligned incentive payment for measurable improvements in care for vulnerable populations.
Particular areas of quality (such as lack of care or quality of care), systemic challenges (such as poor cultural competency, resources, e-literacy, poor communication, and distrust), and/or competing priorities will continue to be a challenge. Nonetheless, increasing clinical informatics capacity to improve health equity is needed to reduce gaps in the digital divide between those who receive high-quality care and those who do not.
FUNDING
This work was supported by the National Library of Medicine Training Grant, NIH Grant [T15LM011271].
AUTHOR CONTRIBUTIONS
The authors AMS, BB, MTS, CAL provided substantial contributions to the conception of work, data analysis, and data interpretation. AMA, AS, LSF, MM, and PM provided substantial contributions to the conception of work and data interpretation. All authors provided feedback and approval of the draft, revision, and final approval of the version to be published with agreement on the accuracy and integrity of this work.
ACKNOWLEDGMENTS
A special thanks to Dr. David Lown and Amanda Clarke from the Safety Net Institute for their guidance and support. Thanks to the University of California Altman Clinical and Translational Research Institute for statistical guidance. We also appreciate the clinical quality efforts underpinning these improvements via superb program management from Heather Erwin, Jennifer Holland, Chad VanDenBerg and clinical quality leadership from Dr. David Folsum, Dr. William Perry, Dr. Gene Kallenberg, Dr. Dustin Lillie, and Dr. Khai Nguyen.
CONFLICT OF INTEREST STATEMENT
The authors have no competing interests to declare.
REFERENCES
- 1. Warnecke RB, Oh A, Breen N, et al. Approaching health disparities from a population perspective: the National Institutes of Health Centers for Population Health and Health Disparities. Am J Public Health 2008; 98 (9): 1608–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Liang H, Beydoun MA.. Modifiable health risk factors, related counselling, and treatment among patients in health centres. Health Soc Care Community 2019; 27 (3): 693–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hooper MW, Carpenter K, Payne M, Resnicow K.. Effects of a culturally specific tobacco cessation intervention among African American Quitline enrollees: a randomized controlled trial. BMC Public Health 2018; 18 (1): 123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Frohlich KL, Potvin L.. Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. Am J Public Health 2008; 98 (2): 216–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Richardson LJ, Brown TH.. (En) gendering racial disparities in health trajectories: A life course and intersectional analysis. SSM Popul Health 2016; 2: 425–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Liszewski W, Peebles JK, Yeung H, et al. Persons of nonbinary gender—awareness, visibility, and health disparities. N Engl J Med 2018; 379 (25): 2391–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fiscella K, Franks P, Gold MR, et al. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA 2000; 283 (19): 2579–84. [DOI] [PubMed] [Google Scholar]
- 8. Bjarnadottir R, Bockting W, Dowding D.. Patient perspectives on answering questions about sexual orientation and gender identity: an integrative review. J Clin Nurs 2017; 26 (13–14): 1814–33. [DOI] [PubMed] [Google Scholar]
- 9. Haider AH, Pronovost PJ.. Health information technology and the collection of race, ethnicity, and language data to reduce disparities in quality of care. Jt Comm J Qual Patient Saf 2011; 37 (10): 435–6. [DOI] [PubMed] [Google Scholar]
- 10. Cahill SR, Baker K, Deutsch MB, et al. Inclusion of sexual orientation and gender identity in stage 3 meaningful use guidelines: a huge step forward for LGBT health. LGBT Health 2016; 3 (2): 100–2. [DOI] [PubMed] [Google Scholar]
- 11. Ard KL, Keuroghlian AS.. Training in sexual and gender minority health—expanding education to reach all clinicians. N Engl J Med 2018; 379 (25): 2388–91. [DOI] [PubMed] [Google Scholar]
- 12. Pratap A, Renn BN, Volponi J, et al. Using mobile apps to assess and treat depression in Hispanic and Latino populations: fully remote randomized clinical trial. J Med Internet Res 2018; 20 (8): e10130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.California Association of Public Hospitals and Health Systems. The Medi-Cal 2020 waiver: Medi-Cal 2020 overview 2018. https://caph.org/priorities/medi-cal-2020-waiver/#1472501468697-6f653413-1626 Accessed December 31, 2018.
- 14. Harbage P, King ML.. A Bridge to Reform: California’s Medicaid Section 1115 Waiver. Prepared for California HealthCare Foundation; 2012. https://www.chcf.org/wp-content/uploads/2017/12/PDF-BridgeToReform1115Waiver.pdf Accessed March 14, 2020. [Google Scholar]
- 15. Lee W-C, et al. Improving the collection of race, ethnicity, and language data to reduce healthcare disparities: a case study from an academic medical center. Perspect Health Inf Manag 2016; 13 (Fall): 1g. [PMC free article] [PubMed] [Google Scholar]
- 16. Patel JS, Oh Y, Rand KL, et al. Measurement invariance of the patient health questionnaire-9 (PHQ-9) depression screener in U.S. adults across sex, race/ethnicity, and education level: NHANES 2005-2016. Depress Anxiety 2019; 36 (9): 813–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nerenz DR, McFadden B, Ulmer C.. Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Public health information network vocabulary access and distribution system (PHIN VADS): Ethnicity data. 2019. https://phinvads.cdc.gov/vads/ViewValueSet.action?oid=2.16.840.1.114222.4.11.6066 Accessed January 4, 2019.
- 19.Centers for Disease Control and Prevention. Public health information network vocabulary access and distribution system (PHIN VADS): Race. 2019. https://phinvads.cdc.gov/vads/ViewValueSet.action?id=67D34BBC-617F-DD11-B38D-00188B398520 Accessed January 4, 2019.
- 20. Kroenke K, S R, Williams JB.. The PHQ‐9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16 (9): 606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.California Association of Public Hospitals and Health Systems. CALIFORNIA’S PROGRESS IN PRIME. 2019. https://caph.org/wp-content/uploads/2019/01/2018.12.17-presentation_prime-program-update.pdf Accessed March 10, 2020.
- 22. Chassin MR, Loeb JM.. High‐reliability health care: getting there from here. Milbank Q 2013; 91 (3): 459–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Medicare and Medicaid Services. Evaluation Design for the public hospital redesign and incentives in Medi-Cal (PRIME) program. 2018. https://www.dhcs.ca.gov/provgovpart/Documents/PRIMEFinalEvalDesign.pdf Accessed March 10, 2020.
- 24. Carney TJ, Kong AY.. Leveraging health informatics to foster a smart systems response to health disparities and health equity challenges. J Biomed Inform 2017; 68: 184–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rajkomar A, Hardt M, Howell MD, et al. Ensuring fairness in machine learning to advance health equity. Ann Intern Med 2018; 169 (12): 866., [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Koh HK, Oppenheimer SC, Massin-Short SB, et al. Translating research evidence into practice to reduce health disparities: a social determinants approach. Am J Public Health 2010; 100 (S1): S72–S80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jarlenski M, Rocco P, Tipirneni R, et al. Shaping health policy for low-income populations: an assessment of public comments in a new medicaid waiver process. J Health Polit Policy Law 2017; 42 (6): 1039–64. [DOI] [PubMed] [Google Scholar]
- 28. Braithwaite RS. Population health could do far more to mitigate health disparities. Popul Health Manag 2019; 22 (2): 96–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nazi KM, Hogan TP, Woods SS, Simon SR, Ralston JD.. Consumer health informatics: engaging and empowering patients and families In: Finnell JT, Dixon BE, eds. Clinical Informatics Study Guide. Switzerland: Springer International Publishing; 2016: 459–500. [Google Scholar]