SUMMARY
Organ transplantation is one of the most important medical achievements of the 20th century. Kidney transplantation is the most efficient method of renal replacement therapy. The first successful kidney transplantation in human was performed in 1954 in Boston, USA. In former Yugoslavia, the first kidney transplantation was performed on April 16, 1970 in Ljubljana, Slovenia, and second one on January 30, 1971 in Rijeka, Croatia. In both cases, the mother donated kidney to the son. In the article, we describe the prerequisite conditions for this operation, the characteristics of first patients, and the impact of transplantation program on the development of the hospitals and medical schools.
Key words: Organ transplantation; Kidney transplantation – history; Kidney failure, chronic
Introduction
The first successful kidney transplantation was performed in a dog on March 7, 1902 in Vienna (1, 2). The operation was performed by Emerich Ullmann, acknowledged pioneer of kidney transplantation. The graft was situated in the subcutaneous pocket in the neck with renal artery anastomosed to the carotid artery, renal vein to the jugular vein, and ureter was sutured to the skin. The animal was exhibited at the lecture hall of the Society of Physicians in Vienna. Urine was produced for several days. This surgical success was published in the same year in the Wiener Klinische Wochenschrift (3). The first transplantation was autotransplantation. After that, Ullmann performed homotransplantation and finally heterotransplantation from dog to goat. Ullmann also reported that he, unsuccessfully, transplanted a pig kidney to the elbow of a woman suffering from uremia (1). This was the first report of attempted human kidney transplantation.
Later in the same year, the famous French surgeon Alexis Carrel also performed kidney transplantation. He also used the neck as the place for graft but he implanted the ureter in the esophagus. Carrel’s major contribution to the field of transplantation was the work on vascular anastomosis and suture technique. He introduced fine needles and threads, developed the triangulation method of small-vessel anastomosis, upgraded the everting anastomosis technique, and developed the so-called ‘Carrel’s patch’ (4). Carrel’s work in the development of suture anastomosis and in the field of organ transplantation was widely recognized and he won the Nobel Prize for Physiology and Medicine in 1912. With the work of Carrel, the surgical aspects of kidney transplantation were solved, but it was the immunobiological factors that precluded transplantation between different subjects in those years.
On December 23, 1954 in Boston, the first successful human kidney transplantation was performed between identical twins (5). Ronald Herrick donated kidney to his twin brother Richard, who suffered from end-stage renal disease (ESRD). Since they were immunologically identical, there was no need for immunosuppression. With this kidney, Richard survived for another eight years (5). This transplantation had a great impact on medical but also on public opinion in favor of transplantation, and led to new discoveries in the field. Discovery of the first immunosuppressive drugs (corticosteroids and azathioprine) led to strong development of organ transplantation, kidney in particular. The first transplant centers were established in the United States and France, and after that, throughout Europe and the world. The influence became evident also in south-east Europe, in former Yugoslavia. At that time, Yugoslavia consisted of six republics with a strong federal government. In this article, we will present the beginning of kidney transplantation in that territory, in particular in Croatia and Slovenia, the two most western and thus most developed republics.
Slovenia
A major historic landmark in kidney and other solid organ transplantation in Slovenia was the establishment of the national histocompatibility laboratory in 1969. Since the beginning, this biochemical laboratory was part of the Blood Transfusion Centre of Slovenia. Its founder was Prof. Mateja Bohinjec (6, 7). She had been influenced by the work of Jean Dausset, a French scientist who in 1965 described the first group of antigens, which is now known as the HLA-system (human leukocyte antigens). Her work was also inspired by Dr. Jon J. van Rood from Leiden, who had proved that matching the HLA-type of donor to the one of recipient had a positive effect on the transplantation outcome, and who founded Eurotransplant in 1967 (8). Another important historic achievement was the introduction of dialysis treatment at the Ljubljana University Medical Centre. On April 27, 1959, urologists at the Department of Urology started treating patients with acute renal failure (Fig. 1). Based on their pioneering work, the first chronic hemodialysis unit was opened in 1970. This hemodialysis center was part of the Department of Nephrology (9). The existence of the hemodialysis unit was an important prerequisite to start with the regular transplantation program. The fundamental transplant persons were the urologists Prof. Slavko Rakovec and Prof. Ludvik Ravnik, and a nephrologist Prof. Saša Luzar, who started to assess the potential living kidney donors to evaluate their suitability for donation (Figs. 2 and 3) (10). Finally, on April 16, 1970, the first living-related kidney transplantation was performed at the Ljubljana University Medical Centre. It was the first kidney transplantation in former Yugoslavia. The surgical team consisted of Prof. Slavko Rakovec and Prof. Ludvik Ravnik, and the cardiovascular surgeon Prof. Miro Košak (7, 10). The recipient was a 36-year-old male with ESRD secondary to chronic glomerulonephritis. The donor was his mother. The renal artery was anastomosed to the internal iliac artery, the renal vein to the common iliac vein, and the ureter to the bladder. The transplantation procedure was uneventful and the recipient started to produce urine in the operating room. Immunosuppression consisted of azathioprine and prednisone. During the first postoperative year, the patient died due to pneumonia. Since that first case, transplantation activity including both living and cadaveric donors has continued (11-13).
Fig. 1.
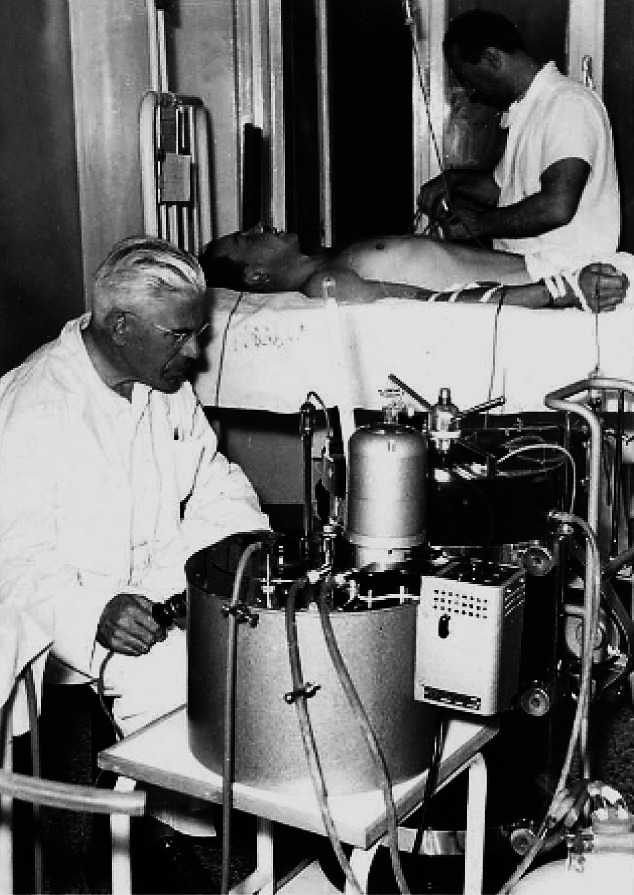
First hemodialysis in Slovenia (1959) with Prof. Rakovec next to the dialysis machine.
Fig. 2.

Prof. Slavko Rakovec in his younger days.
Fig. 3.
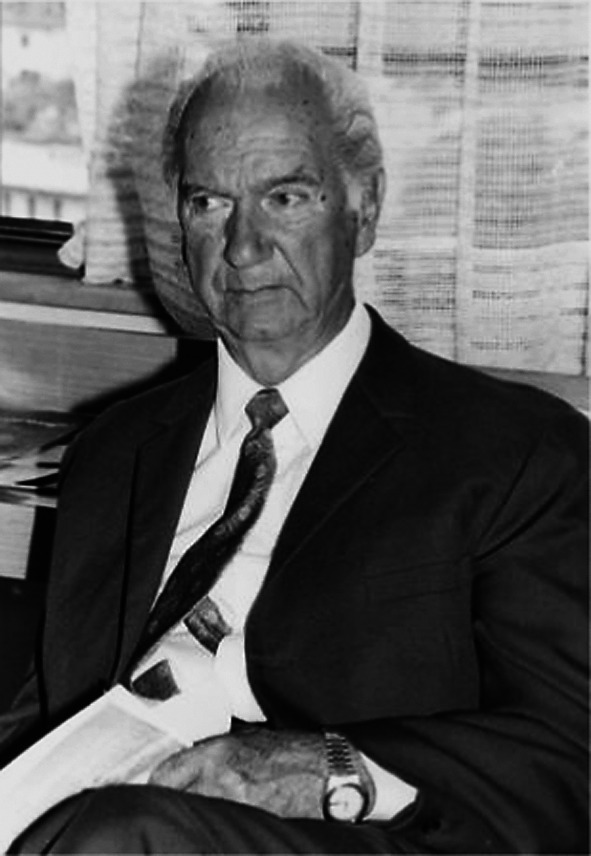
Prof. Ludvik Ravnik.
Croatia
The prerequisite for kidney transplantation was a hemodialysis unit. This unit was established in Rijeka, at Dr. Zdravko Kučić Hospital. In 1962, the first hemodialysis was performed in a patient with acute renal failure. In 1966, Prof. Jerko Zec and his team started the program of chronic hemodialysis. The hemodialysis unit was, at that time, part of the Surgical Department at Sušak (Fig. 4). The existence of this unit was essential for the whole transplantation program because, in that way, the pool of the potential patients had increased. The crucial person in the transplantation program was a surgeon, Prof. Vinko Frančišković, head of the Surgical Department (Fig. 5). He was an outstanding surgeon with a vision. In the transplantation field, he had plans for solid organ transplantation, that is, not only for kidneys but also for the pancreas and the liver. He established an experimental laboratory with animals (dogs and pigs). In that laboratory, surgeons performed transplantation of kidney, pancreas, and liver. He also formed a multidisciplinary team consisting of various specialists such as urologists, anesthesiologists, nephrologists, immunologists, laboratory medicine, transfusion medicine, bacteriology specialists, etc. Members of that transplantation team were educated in Paris, Lyon, Aarhus, and other centers. With time, the team became ready for human kidney transplantation.
Fig. 4.
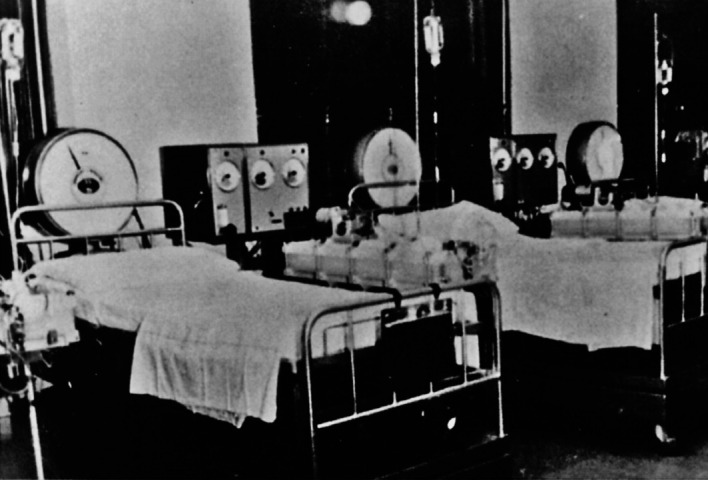
The first hemodialysis unit at Dr. Zdravko Kučić Hospital in Rijeka (Sušak) in the 1960s.
Fig. 5.
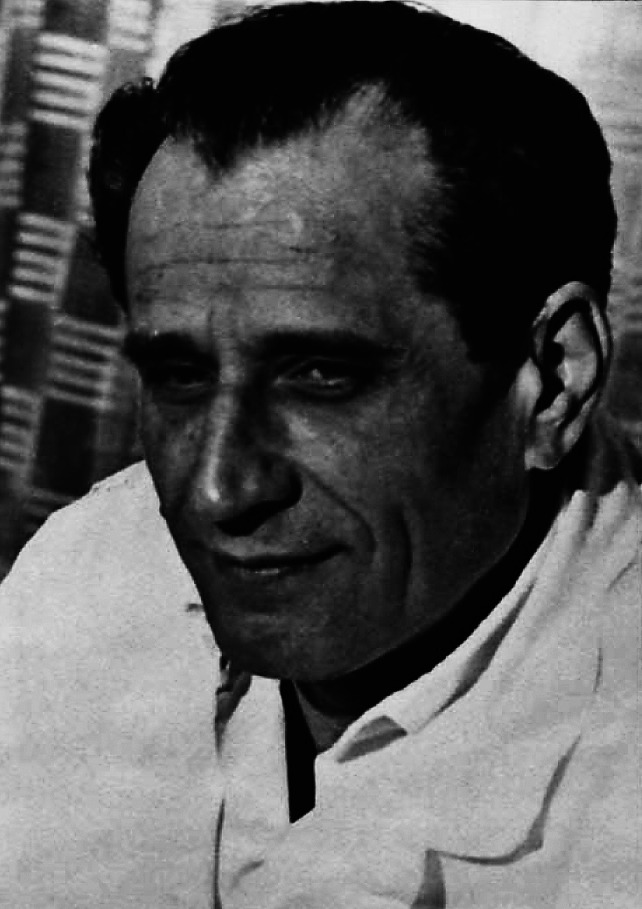
Prof. Vinko Frančišković, head of the Rijeka (Sušak) Surgical Department.
Finally, on Saturday morning, January 30, 1971, the first kidney transplantation in Rijeka was performed (14, 15). The operation was planned for Saturday because the whole capacity of the hospital had been focused on it. The recipient was a 34-year-old man with ESRD, and the donor was his mother. The cause of renal disease was chronic glomerulonephritis. The patient had stayed attached to dialysis for one year. His mother was very motivated, and angiography revealed one renal artery and vein of the donor kidney. Tissue typing was performed in Lyon, France, and the cross match resulted negative. The two operations were performed simultaneously. In one operating theater, the surgical team led by Dr. Vjerislav Peterković performed left-side donor nephrectomy. In another operating theater, Prof. Frančišković prepared the recipient for transplantation (Fig. 6). After successful nephrectomy, the kidney was perfused on a back table. The team of Prof. Frančišković first performed nephrectomy of the right-side recipient native kidney. Then, the transplantation procedure started and the renal artery was anastomosed to the internal iliac artery, the renal vein to the common iliac vein, and the ureter to the ureter. The ureteroureterostomy was protected by nephrostomy. The recipient started with urinary production during the operation. For immunosuppression, corticosteroids, azathioprine, and antilymphocyte serum were used. In the first postoperative week, the patient had an acute rejection episode successfully treated with high-dose corticosteroids. The diagnosis was based on a sudden decrease in urine production, elevation of serum creatinine value, and decreased level of urine sodium. The postoperative surgical course was uneventful (Fig. 7). The recipient lived for the next 14.5 years and died due to liver tumor with a well-functioning kidney.
Fig. 6.

A detail from the operation theater during the first kidney transplantation in Croatia: Prof. Frančišković first on the left.
Fig. 7.
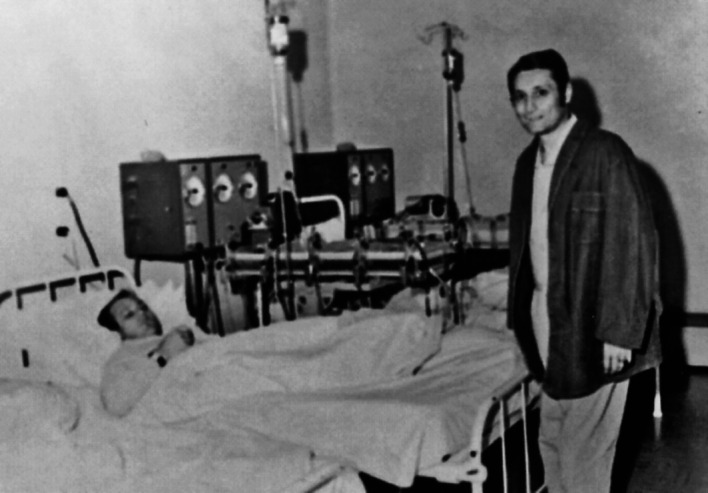
The first patient with transplanted kidney in Rijeka visits another patient in the Hemodialysis Unit. This patient used to encourage other patients to follow his example.
This first kidney transplantation in Rijeka inspired not only surgeons but many other specialists involved (Fig. 8). The transplantation program resulted in a substantial improvement in the field of immunology, transfusion medicine, nephrology, urology, anesthesiology, etc. In addition, a number of articles, conference papers, and dissertations were published on transplantation topics, and some scientific projects were launched as well. The transplantation program had a ‘locomotive’ effect on the development of the Hospital and School of Medicine in Rijeka. At the time, Rijeka became the center for kidney transplantation in ex-Yugoslavia, and surgeons (other specialists as well) started disseminating knowledge throughout the country. They significantly contributed to the establishment of transplantation centers in Zagreb, Sarajevo, and Skopje. Today, Department of Urology follows the tradition of the Surgical Department and carries the title of the Referral Centre for Kidney Transplantation in Croatia.
Fig. 8.
Multidisciplinary team that performed the first kidney transplantation in Croatia; sitting (from left to right): Dr. Petar Orlić (Department of Surgery), Dr. Ksenija Vujaklija-Stipanović (Department of Transfusiology), Prof. Šime Vlahović (Physiology, Rijeka School of Medicine), Prof. Vinko Frančišković (Surgery), Dr. Tomislav Tićac (Surgery), Dr. Jerko Zec (Surgery, Hemodialysis Unit); standing (from left to right): Dr. Giampaolo Velčić (Surgery), Dr. Miomir Zelić (Surgery), Dr. Damir Dimec (Surgery), Dr. Nikola Gržalja (Department of Microbiology, Rijeka School of Medicine), Dr. Daniel Rukavina (Physiology, Rijeka School of Medicine), Dr. Ante Šepić (Surgery), Dr. Alenka Suzanić (Anesthesiology), Dr. Vjerislav Peterković (Surgery), Dr. Duje Vukas (Surgery), Dr. Branimir Budisavljević (Surgery), Dr. Andrej Gudović (Surgery).
Discussion
In south-east Europe, the beginnings of kidney transplantation varied a great deal from one country to another; in Greece, the program started in 1968, as in Bulgaria and Turkey; in Romania, in 1980, and in Albania as late as 2009 (16). The program of kidney transplantation in former Yugoslavia started in two centers, Ljubljana and Rijeka, almost simultaneously. In both centers, first a hemodialysis unit was established. This was a prerequisite for the transplantation program. At the beginning, both centers started with acute dialysis, but the establishment of chronic dialysis program allowed the formation of a pool of patients suitable for kidney transplantation. These first patients were relatively young compared to the present-day patients and with a short hemodialysis history. Consequently, the recipients’ vessels demonstrated minimal atherosclerosis changes and the urinary bladders were functional. From the surgical point of view, those patients were more suitable for operation than the average patient today (with a poor vascular status and sometimes with a long period of bladder malfunction).
As in other centers, kidney transplantation started with the living-donor program. In the first decade, the living-donor transplantation program had much more patients than the cadaveric program. In both centers, the urologists had the most important role in starting and developing the transplantation program.
From the surgical point of view, it is interesting that both centers used the internal iliac artery for anastomosis. At that time, it was a widespread technique. With time, the external iliac artery has replaced the internal artery in most cases. Technically, it is easier to create anastomosis on the external vessels, and using the internal iliac artery can lead to erectile dysfunction and impaired quality of life. Ureteroureterostomy was popular in some centers but better results of ureteroneocystostomy replaced this technique. Nephrectomy of the native kidney is also abandoned today because it prolongs the operation and poses additional risks and complications.
Both patients had some complications in the posttransplant period. One patient developed acute rejection in the early postoperative period, diagnosed by a decreased urine output and altered laboratory parameters but without histologic confirmation. Renal biopsy guided by ultrasound as the gold standard in our days was not in use at that time. Death of both patients (from pneumonia and liver cancer) can be explained by the effect of immunosuppressive drugs. Unfortunately, these complications are still possible but their diagnosis and treatment have improved with time.
In both centers, the transplantation program was important for the development of many disciplines (clinical and preclinical) in hospitals and at medical schools. With time, kidney transplantation has become a routine procedure and more than 1000 patients with ESRD have been operated at the two centers up to this day. In the meantime, both Croatia and Slovenia gained their independence and became members of Eurotransplant, the largest European kidney-exchange organization.
Since its beginning, kidney transplantation has offered new hope to patients with ESRD, promising life prolongation and improvement. At the start, many things were guided by enthusiasm and conjecture without scientific evidence and tested outcome. However, improvement of patient health, prolonged life span and better quality of life were so evident that kidney transplantation has become the treatment of choice for ESRD patients. Good results of kidney transplantation have become a beacon for transplantation of other organs as well (liver, pancreas, heart, intestine, etc.).
At the end, we might recall one famous quote from Winston Churchill: “Never was so much owed by so many to so few”. We can agree that the pioneers of kidney transplantation (“so few”) made tremendous efforts and, together with their followers, have improved the life of hundreds of thousands of ESRD patients (“so much”).
References
- 1.Druml W, Druml C. Emerich Ullmann (1861-1937): not only a pioneer of kidney transplantation. J Nephrol. 2004;17:461–6. [PubMed] [Google Scholar]
- 2.Markić D, Valenčić M, Maričić A, Španjol J, Rački S, Fučkar Ž. Kidney transplantation – successful story started 110 years ago. Acta Med Croatica. 2012;66 Suppl 2:59–63. [PubMed] [Google Scholar]
- 3.Ullmann E. Experimentelle Nierentransplantation. Wien Klin Wochenschr. 1902;15:281–2. [in German] [PubMed] [Google Scholar]
- 4.Shaw R, Stubenbord WT. Alexis Carrel, M.D. Contribution to kidney transplantation and preservation. N Y State J Med. 1980;80(9):1438–42. [PubMed] [Google Scholar]
- 5.Sade RM. Transplantation at 100 years: Alexis Carrel, pioneer surgeon. Ann Thorac Surg. 2005;80:2415–8. 10.1016/j.athoracsur.2005.08.074 [DOI] [PubMed] [Google Scholar]
- 6.Vončina J, Avsec-Letonja D. Transplantation programme in Slovenia. In: Bren AF, Ferluga D, Olsen S, Rossmann P, eds. International Conference on Transplantation with Emphasis on Kidney; 1988 October 8-9; Ljubljana, Slovenia. Ljubljana: Institute of Pathology, Medical Faculty University of Ljubljana, Department of Nephrology, University Medical Centre Ljubljana; 1988. p. 1-5. [Google Scholar]
- 7.Vončina J. Sprehod skozi zgodovino. In: Blumauer R, ed. 5. obletnica ustanovitve Slovenija-transplanta in 1. strokovno srečanje Slovenskega združenja za transplantacijo pri Slovenskem zdravniškem društvu; 2006 May 25.-26.; Terme Čatež in Grad Mokrice, Slovenija. Ljubljana: Slovensko združenje za transplantacijo, Slovenija-transplant, Klinični center Ljubljana; 2006. p. 27-30. (in Slovene) [Google Scholar]
- 8.van Rood JJ, Freudenberg J, van Leeuwen A, Schippers HM, Zweerus R, Terpstra JL. Eurotransplant. Transplant Proc. 1971;3:933–41. [PubMed] [Google Scholar]
- 9.Buturović-Ponikvar J. Report on the symposium celebrating the 40th anniversary of chronic dialysis and kidney transplantation in Slovenia. Ther Apher Dial. 2011;15:225–7. 10.1111/j.1744-9987.2011.00941.x [DOI] [PubMed] [Google Scholar]
- 10.Luzar S. Zgodovina novodobnega presajanja organov, sedanje stanje in razvoj. Med Razgl. 1988;27 Suppl 3:291–387. [in Slovene] [Google Scholar]
- 11.Drinovec J, Malovrh M, Kandus A, Čizman B, Luzar S, Košak M, et al. Follow-up of donors in living related renal transplantation. Transplant Proc. 1987;19:3645–6. [PubMed] [Google Scholar]
- 12.Kandus A, Arnol M, Bren AF. Renal transplantation in Slovenia after joining Eurotransplant. Nephrol Dial Transplant. 2006;21:36–9. 10.1093/ndt/gfi277 [DOI] [PubMed] [Google Scholar]
- 13.Vončina J. Transplant activities in Slovenia. Organs Tissues. 1999;2:115–7. [Google Scholar]
- 14.Fučkar Ž, Markić D, Španjol J, Valenčić M. The history of kidney transplantation at Sušak Hospital. Acta Med Croatica. 2011;65:323–9. [PubMed] [Google Scholar]
- 15.Frančišković V, Vlahović Š, Zec J, Orlić P, Peterković V. Kidney transplantation – case report. Lijec Vjesn. 1971;93:849–57. [PubMed] [Google Scholar]
- 16.Boletis JN. Renal transplantation in Greece. Nephrol Dial Transplant. 2001;16(6):137–9. 10.1093/ndt/16.suppl_6.137 [DOI] [PubMed] [Google Scholar]



