Abstract
BACKGROUND
Type 2 myocardial infarction (MI) and myocardial injury are associated with increased short-term mortality. However, data regarding long-term mortality are lacking.
OBJECTIVES
This study compared long-term mortality among young adults with type 1 MI, type 2 MI, or myocardial injury.
METHODS
Adults age 50 years or younger who presented with troponin >99th percentile or the International Classification of Diseases code for MI over a 17-year period were identified. All cases were adjudicated as type 1 MI, type 2 MI, or myocardial injury based on the Fourth Universal Definition of MI. Cox proportional hazards models were constructed for survival free from all-cause and cardiovascular death.
RESULTS
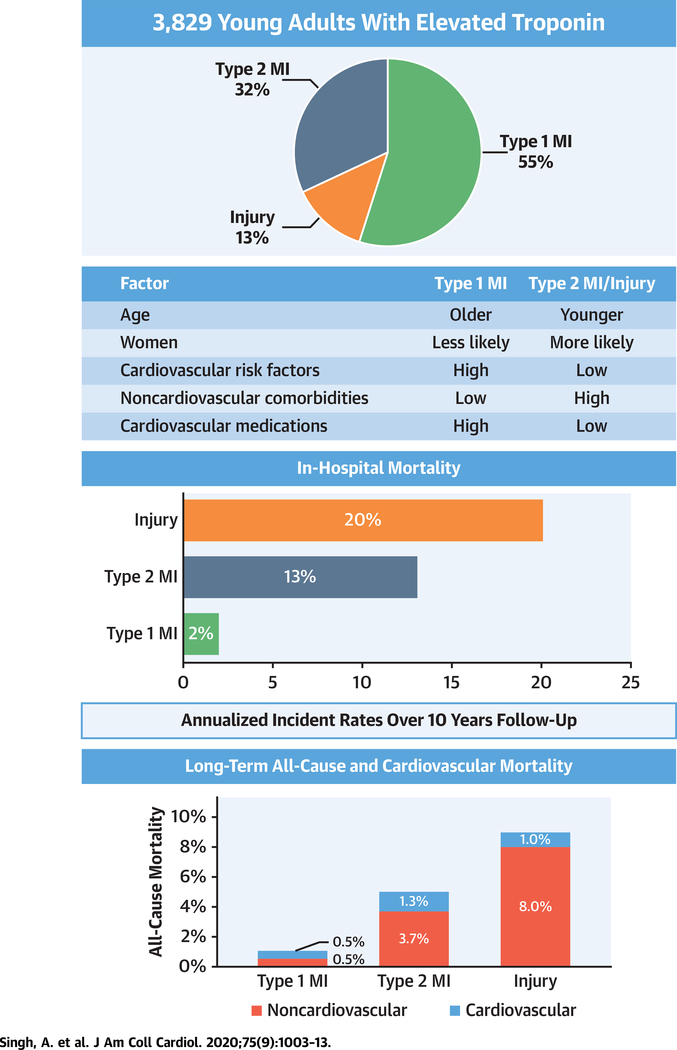
The cohort consisted of 3,829 patients (median age 44 years; 30% women); 55% had type 1 MI, 32% had type 2 MI, and 13% had myocardial injury. Over a median follow-up of 10.2 years, mortality was highest for myocardial injury (45.6%), followed by type 2 MI (34.2%) and type 1 MI (12%) (p < 0.001). In an adjusted model, type 2 MI was associated with higher all-cause (hazard ratio: 1.8; 95% confidence interval: 1.2 to 2.7; p = 0.004) and cardiovascular mortality (hazard ratio: 2.7; 95% confidence interval: 1.4 to 5.1; p = 0.003) compared with type 1 MI. Those with type 2 MI or myocardial injury were younger and had fewer cardiovascular risk factors but had more noncardiovascular comorbidities. They were significantly less likely to be prescribed cardiovascular medications at discharge.
CONCLUSIONS
Young patients who experience a type 2 MI have higher long-term all-cause and cardiovascular mortality than those who experience type 1 MI, with nearly one-half of patients with myocardial injury and more than one-third of patients with type 2 MI dying within 10 years. These findings emphasize the need to provide more aggressive secondary prevention for patients who experience type 2 MI and myocardial injury.
Keywords: outcomes, myocardial injury, troponin, type 2 myocardial infarction, young adults
The Fourth Universal Definition of Myocardial Infarction (UDMI) characterizes patients with elevated cardiac biomarkers into those with myocardial infarction (MI) versus those with nonischemic myocardial injury. Type 2 MI is defined as having an imbalance between myocardial oxygen supply and demand unrelated to acute coronary atherothrombosis, whereas myocardial injury has a similar mismatch driven by a secondary factor but without overt clinical evidence of myocardial ischemia (1).
Due to the increased recognition of this condition and the use of more sensitive troponin assays, type 2 MI is now commonly encountered in clinical practice, and, in some studies, has been even more common than type 1 MI (2). Furthermore, with the increased adoption of high-sensitivity troponin and the introduction of a dedicated administrative code for type 2 MI (I21.A1), this diagnosis may become even more prevalent (3).
Although previous studies have suggested that patients with type 2 MI have a higher in-hospital and short-term mortality than those who experience type 1 MI, there are limited data on long-term mortality, especially long-term cardiovascular mortality (4–7). The higher observed mortality in patients with type 2 MI is not unexpected because type 2 MI usually occurs in acutely ill hospitalized older patients with significant comorbidities (8), including a high proportion with underlying coronary artery disease (CAD). It is unknown if the higher mortality observed in these populations would similarly apply to younger subjects without known CAD. In addition, limited data are available regarding the etiology-specific prognosis of type 2 MI or myocardial injury.
Therefore, our objective was to compare the clinical characteristics, management, and long-term all-cause and cardiovascular mortality among young adults who experienced a first type 1 MI, type 2 MI, or myocardial injury at age 50 years or younger.
METHODS
STUDY POPULATION
The design of the Young-MI registry was previously described (9). This was a retrospective cohort study that included patients who presented to 2 large academic medical centers and were found to have elevated cardiac biomarkers or International Classification of Disease (ICD)-9 or −10 codes for acute MI. Subjects with known CAD (defined as previous MI or revascularization) were excluded. All records were adjudicated by a team of study physicians using the Third UDMI for acute MI and the type of MI (10). During the adjudication period, the Fourth UDMI was published and all events previously adjudicated as type 2 MI or myocardial injury were re-adjudicated to conform to the Fourth UDMI (1). During the study period, different assays were used to measure troponin. Therefore, each troponin value was standardized by dividing it by the 99th percentile (i.e., the upper limit of normal) for the particular assay that was used. Details are provided in Online Table 1.
To define an MI as type 1 or type 2, each case was adjudicated by 2 physicians during the initial review and then during a second review. If there was no consensus, the case was reviewed by an adjudication committee, and decision was reached by consensus.
Data were captured regarding symptoms of ischemia, the presence of dynamic ischemic electrocardiographic changes, and imaging evidence of loss of viable myocardium or of regional wall motion abnormalities to further classify type 2 MI into “true” type 2 MI (with evidence of ischemia) or myocardial injury (without evidence of ischemia), as suggested by the Fourth UDMI (1). Patients for whom the determination of symptoms of ischemia was not possible (i.e., sedated or unconscious patients who did not have evidence of ischemia on imaging or those who did not undergo imaging) were classified as having myocardial injury, as previously done by others (11) and suggested by the Fourth UDMI (1).
Subjects with myocardial injury secondary to clinical conditions in which the pathophysiology was distinct from the supply/demand mismatch (e.g., myocarditis and Takotsubo cardiomyopathy) were excluded, which aligned with expert recommendations considering these conditions separate from type 2 MI (1,12). Subjects were also excluded if key clinical data were missing or were classified as type 3, 4, or 5 MI. Patients with chronic myocardial injury secondary to conditions (e.g., end-stage renal disease) were also excluded.
ETIOLOGY OF TYPE 2 MI OR MYOCARDIAL INJURY
All cases of type 2 MI or myocardial injury were reviewed by a team of study physicians to determine the primary etiology of the demand/supply mismatch whether coronary (e.g., spasm, embolism, dissection) or noncoronary (e.g., hypertensive emergency, sepsis, respiratory failure and/or hypoxia). Because sepsis is often associated with tachycardia, hypotension, and hypoxia, if evidence of ischemia was present, these patients were classified as having type 2 MI with sepsis as the underlying etiology as also previously done in other studies (4,8,13). In cases in which there was uncertainty, adjudication was achieved by consensus of an adjudication committee. In cases in which the cause could not be determined, patients were marked as “unable to determine cause.”
RISK FACTORS
Presence of cardiovascular risk factors was ascertained by a detailed review of electronic medical records during or before the index admission. Diabetes was defined as hemoglobin A1c ≥6.5% or diagnosis and/or treatment for diabetes. Hypertension was defined as a systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or diagnosis and/or treatment of hypertension. Dyslipidemia was defined as total cholesterol ≥240 mg/dl, serum triglycerides ≥150 mg/dl, high-density lipoprotein cholesterol <40 mg/dl in men or <50 mg/dl in women, or diagnosis and/or treatment of dyslipidemia. Smoking was defined as current (tobacco products used within the last month), former, or never.
To adjust for comorbidities, we also calculated the Charlson Comorbidity Index (CCI), a validated method of predicting the risk of mortality based on comorbidities, for each patient as determined by ICD-9 diagnosis and billing codes associated with the index hospitalization (14,15). For patients within the sample with type 1 MI who were not coded for MI, we added an additional ICD-9 code of 410 (acute MI) before calculating the CCI.
MEDICATIONS UPON DISCHARGE
All charts were reviewed in detail through the electronic medical record to determine the number of subjects on guideline-appropriate medical therapy at the time of hospital discharge. Medications included aspirin, antiplatelet therapy, statins, beta-blockers, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers.
OUTCOMES
The outcomes of interest were in-hospital mortality, all-cause mortality, and cardiovascular mortality. Vital status was assessed with linkage to the Partners Healthcare electronic medical record system, the Social Security Administration’s Death Master File, and the National Death Index. The cause of death was adjudicated independently by 2 cardiologists (A.G., A.Q.) using electronic health records, records from the Massachusetts Department of Vital Statistics, and death certificates obtained from the National Death Index. In cases of disagreement, consensus for the cause of death was reached by the adjudication committee. The cause of death was categorized as cardiovascular death, noncardiovascular death, or undetermined cause of death. If the cause of death remained undetermined, patients were conservatively analyzed as noncardiovascular death. The definition of cardiovascular death was adapted from the 2014 American College of Cardiology definition for cardiovascular endpoint events (16) and was previously detailed in the study design publication (9). Cardiovascular deaths included death from acute MI, heart failure, sudden cardiac death, ischemic stroke, nontraumatic hemorrhagic stroke, immediate complications of a cardiovascular procedure, cardiovascular hemorrhage, and other cardiovascular causes (e.g., pulmonary embolism or peripheral artery disease).
DATA MANAGEMENT
Study data were stored on our customized secure electronic adjudication system and REDCap. REDCap is an encrypted, secure, Health Insurance Portability and Accountability Act compliant web platform for electronic data capture and serves as an intuitive interface to enter data with real-time validation (17). The Young-MI registry was approved by the Institutional Review Board at Partners Healthcare.
STATISTICAL ANALYSIS
Categorical variables were reported as frequencies and proportions and were compared with the chi-square test or Fisher exact test. Continuous variables were reported as median or mean and compared with Student’s t-tests or the Mann-Whitney U test. All analyses were performed using Stata software version 14.2 (StataCorp, College Station, Texas).
Cox proportional hazards models were constructed for survival free from all-cause death and cardiovascular death. Proportional hazards assumption was assessed by analyzing the Schoenfeld residuals. Multivariable risk adjustment was performed using variables that had significant univariate association with the outcome of interest or were known to be associated with either all-cause mortality or cardiovascular death. A landmark analysis was also performed, including only the subjects who survived until hospital discharge, to evaluate the long-term prognosis and to account for the high acuity of illness for certain patients.
RESULTS
BASELINE CHARACTERISTICS
The cohort consisted of 3,829 subjects who experienced an MI or myocardial injury. The median age was 44 years (interquartile range: 38 to 47 years); 1,138 (29.7%) were women and 2,675 (69.6%) were white. The adjudicated diagnoses were as follows: 2,097 (54.8%) patients with type 1 MI; 1,225 (31.9%) patients with type 2 MI; and 507 (13.2%) patients with myocardial injury.
Table 1 provides the baseline characteristics of patients with type 1 MI, type 2 MI, and myocardial injury. Compared with patients with type 1 MI, patients with type 2 MI and myocardial injury were younger and more likely to be women. In addition, patients with type 2 MI and patients with myocardial injury had a significantly lower prevalence of traditional cardiovascular risk factors, including lower rates of diabetes, hypertension, hyperlipidemia, and smoking (p < 0.001 for all). However, patients with type 2 MI and myocardial injury had worse renal function and a higher proportion of other comorbidities, as also reflected by a higher CCI (p < 0.001). Patients with type 2 MI and myocardial injury also had a significantly longer length of hospital stay (p < 0.001). Baseline characteristics of patients with type 2 MI compared with patients with myocardial injury are provided in Online Table 2.
TABLE 1.
Baseline Characteristics
| Type 1 MI (n = 2,097; 54.8%) | Type 2 MI (n = 1,225; 32%) | Injury (n = 507; 13.2%) | p Value | |
|---|---|---|---|---|
| Demographics | ||||
| Age, yrs | 45.0 (41.0–48.0) | 42.0 (34.0–47.0) | 41.0 (32.0–47.0) | <0.001 |
| Women | 404 (19.3) | 530 (43.3) | 204 (40.2) | <0.001 |
| White | 1,538 (73.3) | 792 (64.7) | 344 (67.9) | <0.001 |
| Income, $ | 71,392 (52,088–87,169) | 65,284 (50,718–86,240) | 64,178 (50,752–82,532) | <0.001 |
| Insurance type | ||||
| None | 191 (10.2) | 79 (8.0) | 22 (4.3) | <0.001 |
| Public | 310 (16.6) | 393 (39.9) | 171 (33.7) | |
| Private | 1,367 (73.2) | 513 (52.1) | 175 (34.5) | |
| Unknown | 229 (10.9) | 240 (19.6) | 139 (27.4) | |
| Comorbidities | ||||
| Diabetes | 405 (19.3) | 165 (13.5) | 79 (15.6) | <0.001 |
| Hypertension | 970 (46.3) | 419 (34.2) | 135 (26.6) | <0.001 |
| Dyslipidemia | 1,229 (58.6) | 172 (14.0) | 36 (7.1) | <0.001 |
| Current smoking | 1,063 (50.7) | 244 (19.9) | 85 (16.8) | <0.001 |
| eGFR, ml/min/m2 | 80.1 (67.8–91.6) | 65.8 (40.8–88.9) | 59.3 (32.5–87.0) | <0.001 |
| Creatinine, mg/dl | 1.1 ± 0.4 | 1.5 ± 1.4 | 1.7 ± 1.4 | <0.001 |
| Normalized troponin* | 41.4 (10.5–150.7) | 5.5 (2.1–17.0) | 3.3 (1.6–8.4) | <0.001 |
| Length of stay, days | 3.0 (2.0–5.0) | 5.0 (2.0–12.0) | 7.0 (3.0–16.0) | <0.001 |
| CCI | 1.0 (1.0–2.0) | 2.0 (1.0–3.0) | 2.0 (1.0–3.0) | <0.001 |
| Medications/treatment at discharge | ||||
| Aspirin | 1,945 (94.6) | 416 (39.0) | 62 (15.3) | <0.001 |
| P2Y12 inhibitor | 1,561 (76.0) | 47 (4.4) | 1 (0.2) | <0.001 |
| Statin | 1,840 (89.5) | 255 (23.9) | 43 (10.6) | <0.001 |
| Beta-blockers | 1,878 (91.3) | 513 (48.1) | 139 (34.3) | <0.001 |
| ACE inhibitors | 1,269 (61.7) | 271 (25.4) | 55 (13.6) | <0.001 |
| Coronary catheterization | 1,971 (94.0) | 269 (22.6) | 18 (3.6) | <0.001 |
| Coronary revascularization | 1,786 (85.2) | 27 (2.2) | 0 (0.0) | <0.001 |
| Outcomes | ||||
| In-hospital mortality | 42 (2.0) | 160 (13.1) | 102 (20.1) | <0.001 |
| All-cause mortality | 252 (12.0) | 419 (34.2) | 231 (45.6) | <0.001 |
| Cardiovascular mortality | 126 (6.0) | 106 (8.7) | 24 (4.7) | 0.002 |
Values are median (interquartile range), n (%), or mean ± SD.
Standardized to times >99th percentile for assay.
ACE = angiotensin-converting enzyme; CCI = Charlson Comorbidity Index; eGFR = estimated glomerular filtration rate; MI = myocardial infarction.
OUTCOMES
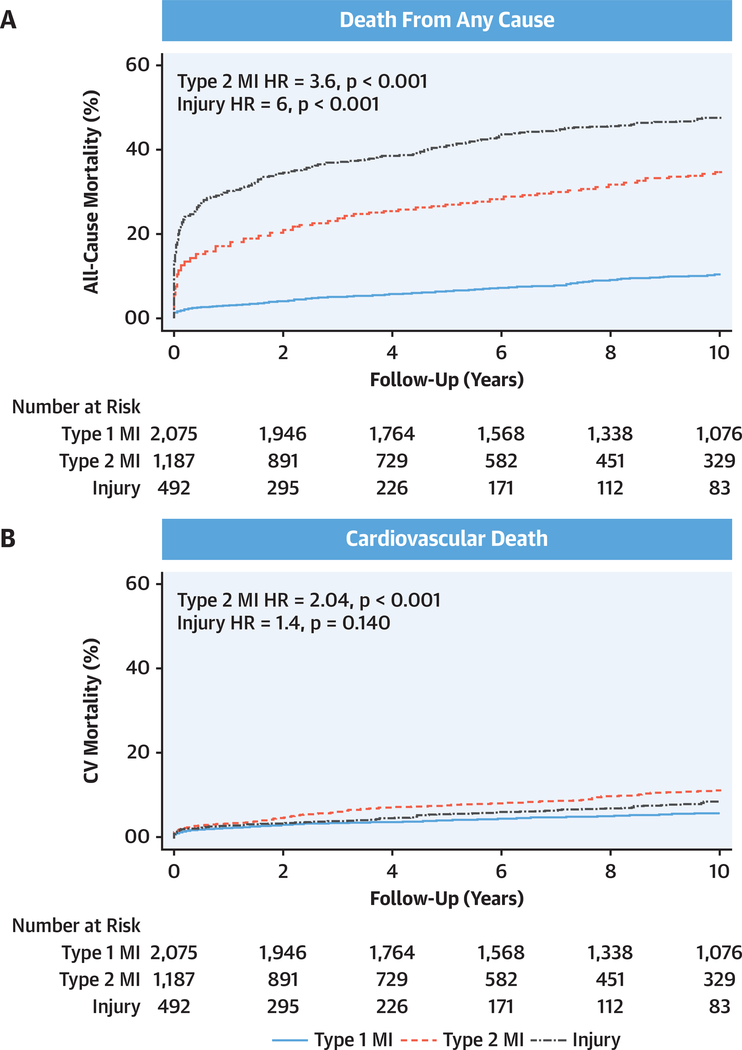
Death during hospitalization (median: 4 days; interquartile range: 2 to 8 days) was significantly higher in patients with myocardial injury and type 2 MI compared with patients with type 1 MI and occurred in 102 (20.1%) patients with myocardial injury, 160 (13.1%) patients with type 2 MI, and 42 (2%) patients with type 1 MI (p < 0.001). Over a median follow-up of 10.2 years (interquartile range: 6.2 to 13.7 years), there were 231 (45.6%) deaths among patients with myocardial injury, 419 (34.2%) deaths among those with type 2 MI, and 252 (12%) deaths among those with type 1 MI. Cardiovascular deaths were highest for type 2 MI (n = 106; 8.7%), followed by type 1 MI (n = 126; 6.0%) and myocardial injury (n = 24; 4.7%). The proportion of deaths due to cardiovascular causes was highest for type 1 MI (50%; 126 of 252 deaths), followed by type 2 MI (25.3%; 106 of 419 deaths), and myocardial injury (10.4%; 24 of 231 deaths). The Central Illustration displays the annual all-cause and cardiovascular death rates, whereas Figure 1 displays Kaplan-Meier failure curves for all-cause and cardiovascular death stratified by type 1 MI, type 2 MI, and myocardial injury.
CENTRAL ILLUSTRATION. Clinical Features and Outcomes of Young Adults With First-Time Type 1 Myocardial Infarction, Type 2 Myocardial Infarction, or Myocardial Injury.
The pie chart shows the distribution of the 3 groups. The table illustrates key differences in baseline characteristics. The horizontal bar graph displays in-hospital mortality of the 3 groups. Vertical bar graphs display annualized incidence rates of noncardiovascular and cardiovascular mortality, the sum of which (total height of bar) depicts all-cause mortality. Type 2 myocardial infarction (MI) and myocardial injury had high in-hospital mortality, as well as long-term noncardiovascular and cardiovascular mortality.
FIGURE 1. Kaplan-Meier Curves.
Kaplan-Meier failure curves for (A) all-cause and (B) cardiovascular death for type 1 myocardial infarction (MI), type 2 MI, and myocardial injury. All-cause mortality was significantly higher for type 2 MI and myocardial injury compared with type 1 MI, whereas cardiovascular mortality was significantly higher for type 2 MI. CV = cardiovascular; HR = hazard ratio.
Compared with patients with type 1 MI, patients with type 2 MI (unadjusted hazard ratio [HR]: 3.6; 95% confidence interval [CI]: 3.0 to 4.2; p < 0.001) and myocardial injury (unadjusted HR: 6.0; 95% CI: 4.9 to 7.2; p < 0.001) had significantly worse survival free from death from any cause over long-term follow-up. These findings persisted after adjustment for baseline differences (adjusted HR: 1.8; 95% CI: 1.2 to 2.7; p = 0.004 for type 2 MI and adjusted HR: 2.6; 95% CI: 1.7 to 4.0; p < 0.001 for myocardial injury, respectively).
Compared with type 1 MI, patients with type 2 MI had significantly worse survival free from cardiovascular death over long-term follow-up (unadjusted HR: 2.0; 95% CI: 1.6 to 2.7; p < 0.001). This association became even more pronounced after adjusting for baseline differences (adjusted HR: 2.7; 95% CI: 1.4 to 5.1; p = 0.003). Survival free from cardiovascular death was not significantly different between patients with type 1 MI and myocardial injury on unadjusted or adjusted analyses (Table 2).
TABLE 2.
Long-Term Adjusted* All-Cause and CV Mortality
| Univariate |
Multivariate |
||||
|---|---|---|---|---|---|
| Endpoint | HR | p Value | HR | p Value | C-Statistic |
| All-cause death | |||||
| Type 1 MI | Reference | — | Reference | — | — |
| Type 2 MI | 3.6 (3.0–4.2) | <0.001 | 1.8 (1.2–2.7) | 0.004 | 0.79 |
| Injury | 6.0 (4.9–7.2) | <0.001 | 2.6 (1.7–4.0) | <0.001 | |
| CV death | |||||
| Type 2 MI | 2.0 (1.6–2.7) | <0.001 | 2.7 (1.4–5.1) | 0.003 | 0.75 |
| Injury | 1.4 (0.9–2.2) | 0.14 | 1.4 (0.6–3.2) | 0.47 | |
Adjusted for age, sex, race, income, insurance type, diabetes, hypertension, dyslipidemia, CCI, eGFR, length of stay, aspirin, P2Y12 inhibitors, beta-blocker, ACE inhibitor/angiotensin receptor blocker, and coronary revascularization.
CV = cardiovascular; HR = hazard ratio; other abbreviations as in Table 1.
Sensitivity analyses that only included patients who survived until hospital discharge showed similar results, with patients with both type 2 MI and myocardial injury having significantly worse survival free from all-cause death on unadjusted and adjusted analyses, and patients with type 2 MI (but not myocardial injury) having significantly worse survival free from cardiovascular death on unadjusted and adjusted analyses. Details are provided in Online Table 3.
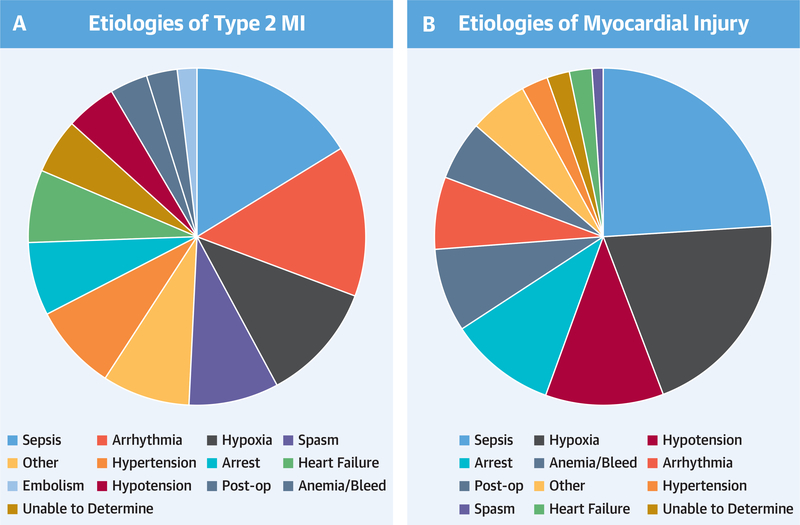
ETIOLOGIES OF TYPE 2 MI VERSUS MYOCARDIAL INJURY
Among patients with type 2 MI, the most common etiologies were sepsis (16.2%), arrhythmias (14.5%), and hypoxia and/or respiratory failure (11.5%). Among patients with myocardial injury, the most common etiologies were sepsis (24.1%), hypoxia and/or respiratory failure (20.1%), and hypotension (10.5%). The distribution of the various etiologies of the supply/demand mismatch is provided in Figure 2.
FIGURE 2. Distribution of Various Etiologies of Type 2 MI and Myocardial Injury.
A broad variety of underlying etiologies that result in demand/supply mismatch in (A) type 2 MI and (B) myocardial injury. The colors represent the various etiologies and remain the same across the 2 panels. Abbreviations as in Figure 1.
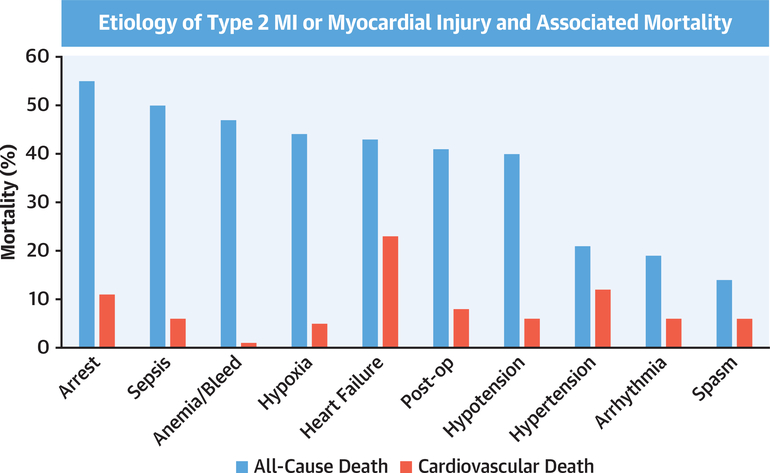
ETIOLOGY-SPECIFIC PROGNOSIS
When examining type 2 MI and myocardial injury events, there was wide variability in rates of all-cause mortality and cardiovascular mortality across the spectrum of etiologies that drove the supply/demand mismatch. Cardiac arrest (55%), sepsis (50%), and anemia and/or bleeding (47%) had the highest all-cause mortality, whereas coronary spasm had the lowest mortality (14%). In terms of cardiovascular death, heart failure (23%), hypertensive emergency (12%), and cardiac arrest (11%) had the highest cardiovascular mortality, whereas anemia and/or bleeding had the lowest cardiovascular mortality (1%). Figure 3 depicts the all-cause and cardiovascular mortality rates for the most frequent etiologies.
FIGURE 3. All-Cause and Cardiovascular Mortality by Etiology of Type 2 MI or Myocardial Injury.
The bar chart illustrates all-cause (blue) and cardiovascular mortality (red) among the most common etiologies of type 2 MI or myocardial injury, in descending order of all-cause mortality. This figure illustrates the wide spectrum of mortality and highlights the different associations between all-cause and cardiovascular mortality. Abbreviations as in Figure 1.
IN-HOSPITAL MANAGEMENT
Compared with type 1 MI, patients with type 2 MI were significantly less likely to undergo invasive testing. Cardiac catheterization was performed in 1,971 (94%) patients with type 1 MI, 269 (22.6%) patients with type 2 MI, and 18 (3.6%) patients with myocardial injury (p < 0.001). Coronary revascularization was performed in 1,786 (85.2%) patients with type 1 MI, 27 (2.2%) patients with type 2 MI, and none of the patients with myocardial injury (p < 0.001). Excluding the patients who died before hospital discharge, medical therapy was prescribed in a significantly higher proportion of patients with type 1 MI compared with patients with type 2 MI or myocardial injury. Specifically, aspirin, P2Y12 inhibitors, statins, beta-blockers, and angiotensin-converting enzyme inhibitors, and/or angiotensin receptor blockers all were prescribed in a significantly higher proportion of patients with type 1 MI compared with either patients with type 2 MI or myocardial injury (p < 0.001). Details are provided in Table 1.
DISCUSSION
To our knowledge, our study was the first to examine the frequency and prognosis of type 2 MI in young adults and provided the longest follow-up of any type 2 MI cohort reported to date. Our main findings were as follows. First, among young subjects who experienced an initial MI, patients with type 2 MI had a higher long-term all-cause mortality and cardiovascular mortality compared with those who experienced type 1 MI (Central Illustration). This association persisted after robust multivariable adjustment and when restricted to patients who survived until hospital discharge. Second, there was a large amount of heterogeneity in the prognosis of type 2 MI depending upon the underlying etiology of supply/demand mismatch. Third, patients with type 2 MI were less likely to receive secondary prevention medications on discharge compared with patients with type 1 MI. Our results reinforced the Fourth UDMI and provided data that categorizing the type of MI in young subjects might inform long-term cardiovascular prognosis. These findings also emphasized the need to identify and implement secondary prevention strategies to mitigate the high rate of cardiovascular death in patients with type 2 MI.
OUTCOMES OF TYPE 2 MI
Type 2 MI was reported to be a condition of older subjects with extensive comorbidities and critical illness, with the high mortality attributed to noncardiovascular causes (8). However, our data suggested that type 2 MI carries a significantly worse all-cause and cardiovascular prognosis. In a seminal paper, Chapman et al. (4) evaluated outcomes of 2,122 consecutive patients with elevated cardiac troponin I concentrations, of whom 55.2% had a type 1 MI, 20.2% had a type 2 MI, and 24.6% had myocardial injury. The mean age for patients with type 2 MI was 75 years. They observed that two-thirds of patients with type 2 MI or myocardial injury did not survive to 5 years after the initial event, which was twice the mortality rate of patients with type 1 MI. This was attributed primarily to an excess of noncardiovascular deaths. However, among patients with type 2 MI and myocardial injury who had known CAD, the risk of major adverse cardiovascular events was significantly higher.
Our study extended these results by showing that the high cardiovascular mortality of type 2 MI also applies to young subjects, a group in which one may expect a lower prevalence of underlying obstructive CAD and a lower burden of comorbidities. Thus, our findings highlighted the importance of diagnosing type 2 MI or myocardial injury in younger populations (18,19) and further underscored the need for development of strategies to treat this potentially lethal entity. The challenge with type 2 MI is that it is a widely heterogeneous condition with many underlying etiologies that impact both outcomes and management, and hence, a one-size-fits-all approach may not be ideal. Individualized treatment strategies based on inherent risk of mortality and cardiovascular-specific mortality are required.
UNCERTAINTY IN MANAGEMENT OF TYPE 2 MI
Unlike type 1 MI, for which there are clear guideline recommendations for management, the optimal treatment of type 2 MI remains uncertain. In our study, we observed a significant underuse of cardiovascular therapies in patients with type 2 MI with less than one-half of patients with type 2 MI receiving any form of CAD secondary prevention therapy upon discharge. This was similar to previous reports in older adults with type 2 MI (4,5,7,20). The underuse of such therapies likely stems from the uncertainty of efficacy, high frequency of comorbidities (e.g., major bleeding, chronic kidney disease, and cancer), and the wide variation in the prevalence of underlying CAD, a factor that may be even more important among young subjects.
Although the benefits of antiplatelet agents, statins, and beta-blockers have not been validated in type 2 MI, our study and others showed that these patients remained at elevated risk of cardiovascular events over long-term follow-up. Thus, there is an unmet need for clinical trials demonstrating the value of cardioprotective interventions in these patients. In a pre-specified analysis of the ODYSSEY Outcomes (Evaluation of Cardiovascular Outcomes After an Acute Coronary Syndrome During Treatment With Alirocumab) trial (21), alirocumab decreased the incidence of both type 1 and type 2 MI. This supported the notion that although there is a wide variability in the underlying etiology of type 2 MI, aggressive risk factor modification might help mitigate, at least to some extent, the high cardiovascular risk observed among these patients.
ROLE OF CAD
CAD has been shown to be independently associated with worse cardiovascular outcomes among patients with type 2 MI (4,20). However, CAD is challenging to assess in this population because most do not undergo angiography because of their acute illness and comorbidities. In the CASABLANCA (Catheter Sampled Blood Archive in Cardiovascular Diseases) study, in which a cohort of patients who underwent coronary angiography was followed prospectively for type 2 MI (n = 152; mean age 71 years), most patients had obstructive CAD in ≥2 vessels (22). In our study, the role of underlying CAD could not be fully examined because, by design, the patients had no known history of CAD, and only a small proportion of those with type 2 MI underwent further testing for CAD. In addition, it was possible that our cohort had a lower prevalence of obstructive CAD because of their young age.
The ACT-2 (Appropriateness of Coronary Investigation in Myocardial Injury and Type 2 Myocardial Infarction) randomized trial is currently underway, evaluating the clinical and economic impact of early invasive management with coronary angiography in type 2 MI (23). Until these results are available, careful assessment of patients’ clinical presentations is necessary to determine the need for further evaluation, especially if their coronary anatomy is unknown.
Identifying underlying CAD in those with type 2 MI, which can be done either invasively or noninvasively, should encourage clinicians to start secondary prevention therapies. In addition to undergoing an evaluation for CAD, patients with type 2 MI or myocardial injury may benefit from screening for structural heart disease with an echocardiogram or cardiac magnetic resonance imaging. Such an approach is currently being evaluated by the DEMAND-MI (Determining the Mechanism of Myocardial Injury and Role of Coronary Disease in Type 2 Myocardial Infarction; NCT03338504) trial. This study will enroll 100 patients with type 2 MI, and all participants will undergo coronary artery imaging using coronary computed tomography angiography with and/or without computed tomography fractional flow reserve or invasive coronary angiography with optical coherence tomography and invasive fractional flow reserve. In addition, to further evaluate the pattern of myocardial injury and structural heart disease, cardiac magnetic resonance imaging will be used to provide structural phenotyping.
STUDY LIMITATIONS AND STRENGTHS
Our study was retrospective in nature, which allowed us to include a large number of subjects who all experienced their event at a young age. Our cohort was predominantly white, which limited the generalizability to other racial groups. In addition, patients with myocarditis, Takotsubo cardiomyopathy, and end-stage renal disease were excluded because of their distinct clinical presentation and management. Of note, according to the Fourth UDMI, these cases would be classified as nonischemic myocardial injury. As a result, the number of patients with injury in our cohort might represent an underestimate. However, the exclusion of some of these patients with potential injury from our study would not have any impact on our results comparing type 1 MI and type 2 MI, and thus our main findings that patients with type 2 MI had worse long-term mortality and cardiovascular mortality remained robust. Furthermore, despite performing a careful adjudication of events using the clinical information available, whereby each case was reviewed by multiple physicians with the final adjudication achieved by consensus of an expert adjudication committee, there remained a potential for misclassification because of the inherent challenges associated with distinguishing type 2 MI from type 1 MI or myocardial injury. However, because of our multistep adjudication process, we would not expect any potential misclassification to bias our results in a particular direction systematically. In addition, although we included cardiovascular risk factors, in-hospital treatment, length of hospital stays, and CCI in our models to adjust for baseline differences in risk, it remains possible that there were unmeasured confounders that we did not adjust for. Finally, MI was not diagnosed using high-sensitivity troponin assays, which—if measured—would be expected to increase the number of patients with myocardial injury. However, the availability of high-sensitivity troponin has not been shown to affect outcomes (24), and thus, it is unknown if inclusion of such assays would have affected our main findings.
Despite these limitations, there were several noteworthy strengths, including the young age of the population, the large proportion of type 2 MI events included, and the decade-long follow-up data. Our study included one of the largest cohorts of patients with type 2 MI, and was the first to evaluate a cohort of young patients with this condition. We used a standardized event adjudication process to differentiate type 2 MI from both type 1 MI and myocardial injury. In addition to all-cause death, our study provided data on cardiovascular deaths that were all adjudicated in a standardized fashion.
CONCLUSIONS
The risks of long-term mortality and cardiovascular mortality associated with type 2 MI and myocardial injury are significantly higher than those associated with type 1 MI. More than one-third of young patients with type 2 MI die within 10 years. Nevertheless, type 2 MI is a heterogenous condition with many underlying etiologies, and accordingly, a wide variation in outcomes. There is a significant underuse of secondary prevention and evaluation for CAD in young patients with type 2 MI. These findings emphasize the need to better phenotype and risk-stratify patients with type 2 MI to facilitate development of evidence-based strategies for improving outcomes.
Supplementary Material
PERSPECTIVES.
COMPETENCY IN PATIENT CARE AND PROCEDURAL SKILLS
Young adults who develop type 2 MI or myocardial injury face higher all-cause and cardiovascular mortality over the course of a decade than those with type I MI.
TRANSLATIONAL OUTLOOK
Better methods are needed to identify and manage young patients with type 2 MI or myocardial injury.
Acknowledgments
Drs. Divakaran and Gupta are supported by a T32 postdoctoral training grant from the National Heart, Lung, and Blood Institute (T32 HL094301). Dr. Jarolim has received research support from Abbott Laboratories, AstraZeneca, Daiichi-Sankyo, GlaxoSmithKline, Merck, Roche Diagnostics, Takeda Global Research and Development Center, and Waters Technologies Corporation; and has been a member of the Scientific Advisory Board for Roche Diagnostics. Dr. Di Carli has received research grants from Gilead Sciences and Spectrum Dynamics. Dr. Bhatt has served on the Advisory Board for Cardax, Cereno Scientific, Elsevier Practice Update Cardiology, Medscape Cardiology, PhaseBio, and Regado Biosciences; has served on the Board of Directors for Boston VA Research Institute, Society of Cardiovascular Patient Care, and TobeSoft; has served as Chair of the American Heart Association Quality Oversight Committee; has served on Data Monitoring Committees for Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute, for the PORTICO trial, funded by St. Jude Medical, now Abbott), Cleveland Clinic (including for the ExCEED trial, funded by Edwards), Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine (for the ENVISAGE trial, funded by Daiichi-Sankyo), and the Population Health Research Institute; has received honoraria from the American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org; Vice-Chair, ACC Accreditation Committee), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; RE-DUAL PCI clinical trial steering committee funded by Boehringer Ingelheim; AEGIS-II executive committee funded by CSL Behring), Belvoir Publications (Editor-in-Chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees, including for the PRONOUNCE trial, funded by Ferring Pharmaceuticals), HMP Global (Editor-in-Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), Medtelligence/ReachMD (CME steering committees), Population Health Research Institute (for the COMPASS operations committee, publications committee, steering committee, and USA national co-leader, funded by Bayer), Slack Publications (Chief Medical Editor, Cardiology Today’s Intervention), Society of Cardiovascular Patient Care (Secretary/Treasurer), and WebMD (CME steering committees); has served as Deputy Editor of Clinical Cardiology, NCDR-ACTION Registry Steering Committee (Chair), and VA CART Research and Publications Committee (Chair); has received research funding from Abbott, Afimmune, Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Chiesi, CSL Behring, Eisai, Ethicon, Ferring Pharmaceuticals, Forest Laboratories, Idorsia, Ironwood, Ischemix, Lilly, Medtronic, PhaseBio, Pfizer, Regeneron, Roche, Sanofi, Synaptic, and The Medicines Company; has received royalties from Elsevier (Editor, Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease); has been a site co-investigator for Biotronik, Boston Scientific, St. Jude Medical (now Abbott), and Svelte; is a trustee for the American College of Cardiology; and has received unfunded research from FlowCo, Fractyl, Merck, Novo Nordisk, PLx Pharma, and Takeda. Dr. Blankstein has received research support from Amgen Inc. and Astellas Inc. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose. Harvey White, MBChB, DSc, FRACP served as guest associate editor for this paper.
ABBREVIATIONS AND ACRONYMS
- CAD
coronary artery disease
- CCI
Charlson Comorbidity Index
- CI
confidence interval
- HR
hazard ratio
- ICD
International Classification of Diseases
- MI
myocardial infarction
- UDMI
Universal Definition of Myocardial Infarction
Footnotes
APPENDIX For supplemental tables, please see the online version of this paper.
REFERENCES
- 1.Thygesen K, ALpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol 2018;72:2231–64. [DOI] [PubMed] [Google Scholar]
- 2.Diaz-Garzon J, Sandoval Y, Smith SW, et al. Discordance between ICD-coded myocardial infarction and diagnosis according to the universal definition of myocardial infarction. Clin Chem 2017;63:415–9. [DOI] [PubMed] [Google Scholar]
- 3.McCarthy CP, Vaduganathan M, Januzzi JL Jr. Type 2 myocardial infarction-diagnosis, prognosis, and treatment. JAMA 2018;320:433–4. [DOI] [PubMed] [Google Scholar]
- 4.Chapman AR, Shah ASV, Lee KK, et al. Long-term outcomes in patients with type 2 myocardial infarction and myocardial injury. Circulation 2018; 137:1236–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stein GY, Herscovici G, Korenfeld R, et al. Type-II myocardial infarction-patient characteristics, management and outcomes. PLoS One 2014;9: e84285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saaby L, Poulsen TS, Diederichsen AC, et al. Mortality rate in type 2 myocardial infarction: observations from an unselected hospital cohort. Am J Med 2014;127:295–302. [DOI] [PubMed] [Google Scholar]
- 7.Baron T, Hambraeus K, Sundstrom J, et al. Type 2 myocardial infarction in clinical practice. Heart 2015;101:101–6. [DOI] [PubMed] [Google Scholar]
- 8.Sandoval Y, Jaffe AS. Type 2 Myocardial infarction: JACC review topic of the week. J Am Coll Cardiol 2019;73:1846–60. [DOI] [PubMed] [Google Scholar]
- 9.Singh A, Collins B, Qamar A, et al. Study of young patients with myocardial infarction: design and rationale of the YOUNG-MI Registry. Clin Cardiol 2017;40:955–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol 2012;60:1581–98. [DOI] [PubMed] [Google Scholar]
- 11.Devereaux PJ, Duceppe E, Guyatt G, et al. Dabigatran in patients with myocardial injury after non-cardiac surgery (MANAGE): an international, randomised, placebo-controlled trial. Lancet 2018;391:2325–34. [DOI] [PubMed] [Google Scholar]
- 12.Ghadri JR, Wittstein IS, Prasad A, et al. International expert consensus document on takotsubo syndrome (part I): clinical characteristics, diagnostic criteria, and pathophysiology. Eur Heart J 2018;39:2032–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arora S, Strassle PD, Qamar A, et al. Impact of type 2 myocardial infarction (MI) on hospital-level MI outcomes: implications for quality and public reporting. J Am Heart Assoc 2018;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40:373–83. [DOI] [PubMed] [Google Scholar]
- 15.Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011;173:676–82. [DOI] [PubMed] [Google Scholar]
- 16.Hicks KA, Tcheng JE, Bozkurt B, et al. 2014 ACC/AHA key data elements and definitions for cardiovascular endpoint events in clinical trials: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Cardiovascular Endpoints Data Standards). J Am Coll Cardiol 2015;66:403–69. [DOI] [PubMed] [Google Scholar]
- 17.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eggers KM, Jernberg T, Lindahl B. Cardiac troponin elevation in patients without a specific diagnosis. J Am Coll Cardiol 2019;73:1–9. [DOI] [PubMed] [Google Scholar]
- 19.Januzzi JL Jr., McCarthy CP. Trivializing an elevated troponin: adding insult to injury? J Am Coll Cardiol 2019;73:10–2. [DOI] [PubMed] [Google Scholar]
- 20.Baron T, Hambraeus K, Sundstrom J, et al. Impact on long-term mortality of presence of obstructive coronary artery disease and classification of myocardial infarction. Am J Med 2016; 129:398–406. [DOI] [PubMed] [Google Scholar]
- 21.White HD, Steg PG, Szarek M, et al. Effects of alirocumab on types of myocardial infarction: insights from the ODYSSEY OUTCOMES trial. Eur Heart J 2019;40:2801–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gaggin HK, Liu Y, Lyass A, et al. Incident type 2 myocardial infarction in a cohort of patients undergoing coronary or peripheral arterial angiography. Circulation 2017;135:116–27. [DOI] [PubMed] [Google Scholar]
- 23.Lambrakis K, French JK, Scott IA, et al. The appropriateness of coronary investigation in myocardial injury and type 2 myocardial infarction (ACT-2): a randomized trial design. Am Heart J 2019;208:11–20. [DOI] [PubMed] [Google Scholar]
- 24.Shah ASV, Anand A, Strachan FE, et al. High-sensitivity troponin in the evaluation of patients with suspected acute coronary syndrome: a stepped-wedge, cluster-randomised controlled trial. Lancet 2018;392:919–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.