Abstract
Background
The COVID-19 pandemic has forced parents across the United States to quickly transition to a new way of living. These transitions present new stressors, including the stress associated with physical health, with the demands of social distancing placed on families, and with the possibility of losing a job or not being able to pay bills. Such stressors have the potential to disrupt basic functioning, such as sleep and daily energy levels. Furthermore, the impact of stress might have repercussions on parents' capacities to be psychologically flexible, thus putting their psychological functioning at risk. Drawing upon a contextual behavioral science perspective, the current study sought to examine links between COVID-19-related stressors and psychological flexibility/inflexibility through such basic processes as parents’ perceived sleep quality and daily energy level.
Methods
A total of 1003 parents (97% from the US; 74% female; M = 40.9 years old, SD = 8.5) of children (ages 5–18) completed an online survey from the end of March to the end of April of 2020.
Results
Path analyses suggested that, after controlling health-related stress and the stress of work and parenting demands due to the pandemic directly predicting greater inflexibility and lower inflexibility, two mediation paths emerged. Specifically, higher levels of health-related stress were associated with lower levels of energy, which, in turn predicted lower levels of psychological flexibility. In addition, higher levels of health-related stress were associated with lower perceived sleep quality, which, in turn, was associated with higher levels of psychological inflexibility. In secondary analyses on the specific dimensions of flexibility and inflexibility, results suggested that lower energy levels indirectly linked health-related stress to lower levels of all 6 dimensions of flexibility and poorer sleep quality indirectly linked health-related stress to higher levels of self-as-content, fusion, and inaction.
Conclusions
The stressors associated with COVID-19 pandemic have the potential to disrupt parents’ perceived sleep quality and daily energy levels, reducing their abilities to respond to difficult or challenging experiences in a flexible manner and instead promoting more reactive and inflexible responses.
Keywords: COVID-19, Stress, Sleep, Energy, Psychological flexibility, Psychological inflexibility
Highlights
-
•
COVID-19 health-stress predicted lower sleep quality and daily energy.
-
•
Low energy mediated links between COVID-19 health-stress and lower flexibility.
-
•
Poor sleep quality mediated links between health-stress and higher inflexibility.
-
•
Acute COVID-19 stress undermined flexibility by disrupting parents' sleep and energy.
The speed with which the novel coronavirus disease 2019 (COVID-19) has spread across the United States, much less the rest of the world, is astounding. The virus has affected millions of lives, forcing women and men across the country to quickly transition to a new way of living. These transitions present new stressors, including the stress associated with physical health, with the work and parenting demands due to social distancing orders being placed on parents, and with the possibility of losing a job or not being able to pay bills (see Brooks et al., 2020 for a review). Perhaps more than others, one group that has experienced these stressors across multiple levels is parents. Not only have parents been forced to confront the consequences of the pandemic on their own health as well as the health of loved ones, but due to the constraints of social distancing, they have also been forced in many cases to provide their own childcare and home-schooling while working from home (assuming that they are still able to work). Such stressors have the potential to disrupt basic and essential biologically-based behaviors, such as sleep and energy levels during the day (Cava, Fay, Beanlands, Mccay, & Wignall, 2005; Hanson & Chen, 2010; Hawryluck et al., 2004; Reeth et al., 2000; Sadeh, Keinan, & Daon, 2004). In this light, not only does research suggest that disturbances to sleep or energy levels have physical repercussions (Dongen, Maislin, Mullington, & Dinges, 2003; Grandner et al., 2020; Spiegel, Leproult, & Cauter, 1999), but there is also ample evidence suggesting that such problems can also disrupt psychological processes like psychological flexibility (Couyoumdjian et al., 2010; Daly-Eichenhardt, Scott, Howard-Jones, Nicolaou, & McCracken, 2016; Peltz, Rogge, Bodenlos, Newman, & Pigeon, 2020). Given the links between life stressors, sleep, and psychological functioning, the current study examined the potential for COVID-19-related stressors to impact psychological flexibility and inflexibility via perceived sleep quality and energy levels.
1. Stress and psychological flexibility and inflexibility
The current study draws on a conceptual framework from contextual behavioral science by using the construct of psychological flexibility (Hayes, Strosahl, & Wilson, 2011) to highlight how acute stress and sleep disruptions might impact individuals’ tendencies to respond to difficult or challenging experiences in psychologically open and accepting or rigid manners. Specifically, six dimensions of flexibility (acceptance, present moment awareness, self-as-context, defusion, values, and committed action) and six corresponding separate dimensions of inflexibility (experiential avoidance, lack of contact with the present moment, self-as-content, fusion, lack of contact with values, and inaction) serve as critical targets of intervention for acceptance and commitment therapy (ACT; see Hayes et al., 2011). Although forms of psychological flexibility and inflexibility have often been conceptualized as opposite extremes of a single underlying dimension, recent work suggests that conceptually similar pairs of dimensions (e.g., fusion vs. defusion, self-as-context vs. self-as-content, acceptance vs. experiential avoidance) are only modestly correlated with one another, show distinct patterns of correlation, and change independently of one another across time (e.g., Peltz et al., 2020; Rogge, Daks; Dubler, & Saint, 2019; Rolffs, Rogge, & Wilson, 2018). Consistent with this, the current study conceptualized the various dimensions of flexibility and inflexibility as separate and distinct outcomes.
Although psychological flexibility is conceptualized within ACT as a key set of skills or adaptive responses to difficult and challenging experiences that promote wellbeing (Hayes et al., 2011), individuals might find it challenging to engage those flexible responses during times of acute or chronic stress. In fact, parenting stress has been linked to greater psychological inflexibility and more rigid and inflexible parenting across a number of studies (e.g., Bluth & Wahler, 2011; Gouveia, Carona, Canavarro, & Moreira, 2016). Although stressors can take on diverse forms, at their roots, they often present situations that tend to be at the limit of or beyond personal control. Similar to past pandemic events (e.g., SARS outbreak; Bai et al., 2004; Brooks et al., 2020), COVID-19 presents a situation beyond parents' control, which forces them to confront numerous threats or challenges, including the fear of catching the virus, the need to transition to new patterns of living due to quarantining (e.g., new and ongoing work demands, extra child care burdens, homeschooling demands), and the fear of losing a job or not being able to pay bills. Thus, quarantining for an outbreak can have devastating psychological consequences (Bai et al., 2004). Accordingly, the current study sought to examine not only the direct impact of such stressors on parents’ psychological flexibility/inflexibility, but also to ascertain potential mechanisms (i.e., sleep quality, daily energy) through which such stressors might be associated with these psychological processes.
2. Stress, sleep, and energy
The bifurcated role that stress appears to play in people's lives highlights its potential to disrupt both their abilities to sleep well and to function adequately during the day (Sadeh et al., 2004; Selye, 1983). In this light, Selye (1983) posits the stress response can take on two distinct modes: the “turn on” response and the “turn off” response. Stressful circumstances can thus render one hypervigilant (“turn on”), a state incompatible with sleep and one which can greatly compromise sleep quality. In turn, stress also has the potential to quickly lead one to feel exhausted, whereby one seeks to reduce activity in order to preserve energy (i.e., the “turn off” response; Selye, 1983). In the present context, the diverse stressors that have emerged due to the COVID-19 pandemic have the potential to impact both aspects of the sleep-wake cycle. For instance, the constant threat of catching COVID-19, or of a loved one catching the virus, might provoke sufficient anxiety to impede the sleep process. In contrast, the stress of having to work from home while parenting or of being out of work completely could serve to deplete parents' energy levels regardless of their current sleep quality, leaving parents wanting to withdraw from daily activities. The current study thus examined three stressors highlighted by the pandemic: health-related stress, the stress of work and parenting demands being placed on parents (working from home, lack of childcare), and financial stressors (fear of being furloughed or losing a job, mounting bills). Given the dual role of stress on the sleep-wake cycle, the current study sought to investigate the potential for such stressors to impact both parents' perceived sleep quality and their energy levels.
3. The role of sleep and energy in psychological flexibility and inflexibility
Building on the potential for stress to impact the sleep-wake cycle, there is small but growing body of research linking this cycle with psychological flexibility and inflexibility (Daly-Eichenhardt et al., 2016; Ong, Ulmer, & Manber, 2012; Peltz et al., 2020). For example, drops in emerging adults’ sleep quality over two months of college were linked to corresponding increases in psychological inflexibility, which in turn, predicted corresponding increases in depressive symptoms (Peltz et al., 2020). Consistent with this, randomized-controlled trials involving mindfulness meditation (to promote present moment awareness) have demonstrated some efficacy in treating insomnia (Ong et al., 2014; Ong, Xia, Smith-Mason, & Manber, 2018). More specifically, higher quality sleep has been linked to greater awareness of and attention to current experiences (Howell, Digdon, & Buro, 2010; Howell, Digdon; Buro, & Sheptycki, 2008). Accordingly, the current study sought to demonstrate concurrent links between perceived sleep quality and energy and psychological flexibility and inflexibility.
Research thus suggests that sleep and energy levels are tightly linked with psychological flexibility and inflexibility (e.g., Daly-Eichenhardt et al., 2016; Peltz et al., 2020), and it is likely that those processes are transactionally related, reciprocally influencing one another across time. The current proposed model conceptualized high quality sleep and high levels of energy as critical mechanisms that would provide individuals with the internal resources necessary to successfully engage psychologically flexible responses to difficult or challenging experiences rather than simply engaging more reactive and inflexible responses. In this light, the ongoing stressors associated with the COVID-19 pandemic are hypothesized to be disruptive to the quality of parents' sleep and daily energy, presenting an entirely new set of problems and worries for parents to handle – many without clear solutions – which could plague their thoughts as they try to fall asleep after a stressful day, exacerbating any fatigue they might already be experiencing. In fact, COVID-19 related stressors might even lead to more immediate biological changes in parents via their neuroendocrine systems (Buckley & Schatzberg, 2005; Smith & Vale, 2006). Specifically, the experience of COVID-19-related stressors is likely to activate parents' hypothalamic-pituitary-adrenal (HPA) axis to secrete glucocorticoids, such as cortisol, to support the body's response to such stressors (Buckley & Schatzberg, 2005; Smith & Vale, 2006). These secretions have been shown to decrease slow-wave sleep, which provides physical restoration, and increase light sleep and wakefulness (Buckley & Schatzberg, 2005). The resulting lower quality sleep and lower daily energy would then leave parents depleted, making it more challenging to successfully engage flexible responses to difficult experiences rather than just engaging in more rigid, inflexible and reactive responses. Thus, although psychological flexibility is likely to also shape and influence the quality of sleep and daily energy levels, the current study conceptualized psychological flexibility as an outcome rather than a predictor – focusing on how flexibility and inflexibility might fluctuate during periods of extreme crisis. This conceptualization therefore allowed the models to examine how COVID-19 related stress might influence those fluctuations by shaping the quality of sleep and daily energy levels.
4. The current study
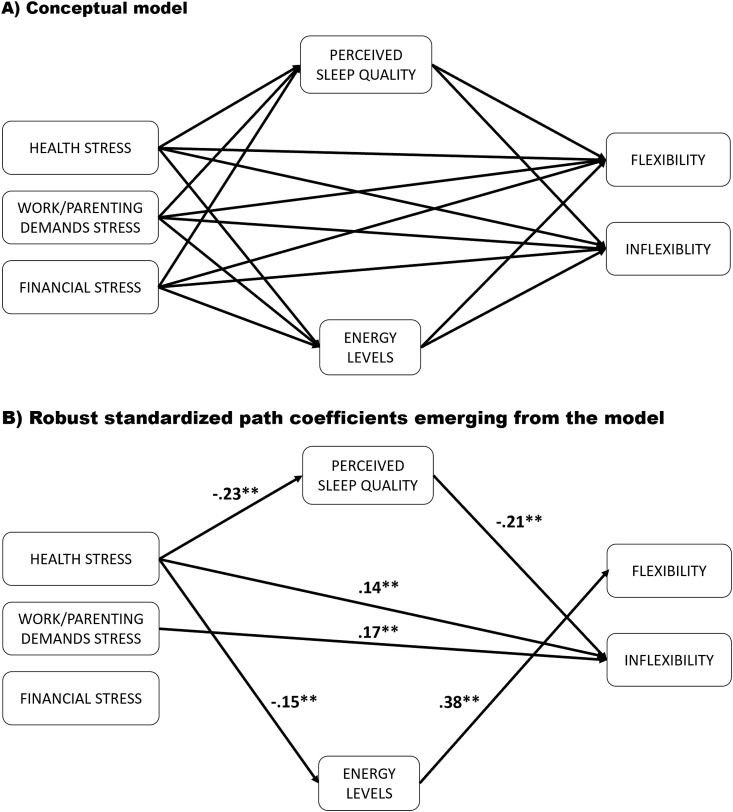
The current study therefore sought to examine a mediation model examining links between COVID-19-related stressors, perceived sleep quality, energy, and psychological flexibility and inflexibility (Fig. 1 A) within an online sample of 1003 parents recruited within the first five weeks of the pandemic breaking in the United States. The model included three salient stressors associated with the pandemic that would likely impact parents and their families – health-related stress, the stress of work and parenting demands, and financial stress – as the primary predictors. Given the framework of the “turn on” and “turn off” responses to stress (Sadeh et al., 2004; Selye, 1983) and the established links between stress and both sleep (“turn on”) and daily energy levels (“turn off”) (Sadeh et al., 2004), these constructs were conceptualized as mechanisms of action within the model. Finally, psychological flexibility/inflexibility were conceptualized as an interrelated set of specific skills or behavioral processes that individuals use to navigate difficult experiences throughout their days – viewing them as outcomes to be predicted.
Hypothesis 1
It was expected that higher levels of COVID-19-related stressors would predict lower levels of perceived sleep quality (Hypothesis 1A) and lower levels of energy (Hypothesis 1B).
Hypothesis 2
It was hypothesized that higher levels of perceived sleep quality would be associated with higher levels of psychological flexibility (Hypothesis 2A) and lower levels of psychological inflexibility (Hypothesis 2B). In addition, it was hypothesized that higher levels of energy would be associated with higher levels of flexibility (Hypothesis 2C) and lower levels of inflexibility (Hypothesis 2D).
Hypothesis 3
It was hypothesized that perceived sleep quality would mediate the associations between COVID-19-related stressors and flexibility (Hypothesis 3A) and inflexibility (Hypothesis 3B).
Hypothesis 4
Finally, it was hypothesized that energy would mediate the associations between COVID-19-related stressors and flexibility (Hypothesis 4A) and inflexibility (Hypothesis 4B).
Fig. 1.
Mediation Model Predicting Psychological Flexibility and Inflexibility. NOTE. ** To focus the narrative on the most robust results (likely to replicate) o nly paths significant at the p < .001 level have been included in the figure. The model was fully identified and therefore yielded perfect fit.
Exploratory analyses: Secondary analyses examined how COVID-19-related stressors, perceived sleep quality, and daily energy were linked to the 6 distinct dimensions of flexibility and the 6 distinct dimensions of inflexibility. As this represented the first published paper examining those links at such a fine-grained level, these analyses were primarily exploratory in nature as the study did not have a priori assumptions about which specific dimensions of flexibility and inflexibility would demonstrate unique links. However, it was hypothesized that the directions of those links would be consistent with Hypothesis 2 (i.e., higher perceived sleep quality and higher daily energy predicting greater flexibility and lower inflexibility).
5. Method
5.1. Procedure
All procedures and materials for this study were approved by an Institutional Review Board and informed consent were obtained from all participants. The survey was hosted online via SurveyGizmo.com and took approximately 35–45 min to complete. Parents were recruited from March 27th to the end of April 2020 just as the COVID-19 pandemic was breaking in the US and a majority of the states started implementing stay-at-home and lockdown policies to slow the spread.
5.2. Participants
Recruitment. In order to participate, parents had to have been at least 18 years old and have a child between the ages of 5 and 18 (the typical ages of children for attending school outside the home) living with them. Participants were recruited through online platforms including ResearchMatch (50.5%), email (12.9%) Reddit forums (13.8%), Amazon. com's Mechanical Turk service (10.7%), social media posts (e.g., Facebook, Twitter, 11.3%), and local news articles (<1%). To incentivize participation, participants received individualized feedback after completing the survey on a number of domains of individual (i.e., psychological flexibility, parenting hassles) and relationship functioning (i.e., family functioning, coparental satisfaction, coparental conflict) as well as the chance to win a $250 amazon.com gift card.
Demographics. A total of 1003 parents primarily from the United States (97.3%) completed an online survey from March to April of 2020. The mean age of the current sample (73.6% female) was 40.9 years (SD = 8.5), and the majority of respondents reported being married, engaged, or in a long-term committed relationship (81.2%) for an average of 15.3 years (SD = 17.5). The majority of participants were Caucasian (82.4%), with 5.7% African American, 4.9% Latinx or Hispanic, 2.2% Asian or Pacific Islander, 1.8% Native American, and 3% identifying as “other.” The sample of families was geographically diverse, with 29.4% residing in the Northeast, 21.8% from the Midwest, 30.2% from the South, and 18.7% from the West. Parents reported a median family income of $80,000 – $90,000, with approximately 22.2% of parents reporting family incomes of $50,000 or less. In addition, 33% of respondents held a BA/BS degree, with 40% holding advanced graduate degrees (e.g., MA/MS, JD, PhD, MD), 22.7% with some college or an associate's degree, and 4.3% with a high school diploma or less. Families included an average of 1.8 children (SD = 1.0), and the children had a mean age of 9.9 years (SD = 4.5). In addition, 28.1% of families reported that they typically used some form of childcare, and, for those families, they typically used these services for an average of 24.1 h (SD = 16.0) per week. However, given the COVID-19 pandemic, those families reported using childcare for only an average of 4.2 h (SD = 11.4) per week in the week prior to completing the survey. Thus, not only were the families' school-aged children no longer in school due to the pandemic, but these parents were also challenged with a lack of the childcare support on which they typically rely. Finally, 39% of respondents reported that they were not working from home, with 19% working part-time from home, 39% working full-time from home, and 3% working 60 h per week or more from home.
5.3. Measures
The current study examined three unique forms of stress associated with the societal changes related to the pandemic: health-related stress, stress associated with work and parenting demands, and finance-related stress.
Health-related stress. Health-related stress was assessed with a 4-item variable, which measured respondent's level of stress or worry over the past week concerning their “own health,” “their children's health,” “health of a loved one,” and “the ongoing possibility of exposure to COVID-19.” The items were rated on a 6-point response scale (0 – “not at all” to 6 – “extremely”), and scores of the 4 items were averaged such that higher scores indicated higher levels of stress or worry related to health (α = 0.84).
Stress from work/parenting demands. Stress related to new and ongoing work and parenting-related demands placed on respondents due to the pandemic was assessed with a 3-item variable, which measured respondent's level of stress or worry over the past week concerning “ongoing work demands,” “new parenting demands (home schooling, lack of childcare),” and “adjusting to new working conditions (telecommuting, working from home).” The items were rated on a 6-point response scale (0 – “not at all” to 6 – “extremely”), and scores of the 3 items were averaged such that higher scores indicated higher levels of stress or worry related to work and parenting demands due to the pandemic (α = 0.71).
Financial stress. Financial stress was assessed with a 2-item variable, which measured respondent's level of stress or worry over the past week concerning “finances/bills” and “the stability of your own job (or your partner's/coparent's job).” The items were rated on a 6-point response scale (0 – “not at all” to 6 – “extremely”), and scores of the 2 items were averaged such that higher scores indicated higher levels of finance-related stress or worry (α = 0.76).
Perceived ssleep quality. Parents' perceptions of their sleep quality were assessed with the 8 items of the Patient-Reported Outcomes Measurement Information System (PROMIS) Sleep Disturbance scale (Yu et al., 2012). In addition to specifically rating sleep quality over the past week (“my sleep quality was …“), these items also assessed respondents’ perceptions of their sleep over the past week (e.g., “I was satisfied with my sleep,” “my sleep was refreshing,” “I had difficulty falling asleep” – reverse-scored, and “I had trouble sleeping” – reverse-scored). All items were rated on 5-point scales (sleep quality: “very poor” to “very good;” all other items: “not at all/never” to “very much/always”) and were averaged so that higher scores indicated higher levels of sleep quality (α = .92).
Energy levels. Levels of energy were measured with a 6-item scale, which assessed respondent's levels of energy and pep over the last 2 weeks (e.g., “I felt energized,” “I felt alive and vital,” and “I felt full of pep,” “I had energy and spirit,” “I had a lot of energy,” “I felt really up or lively”). All items were rated on 6-point scales (“not at all” to “extremely”) and were averaged so that higher scores indicated higher levels of energy (α = 0.96).
Psychological flexibility/inflexibility. Psychological flexibility and inflexibility were assessed with the 60-item Multidimensional Psychological Flexibility Inventory (MPFI; Rolffs et al., 2018). Grounded within the Hexaflex model, the MFPI assesses six dimensions of psychological flexibility (acceptance, present moment awareness, self-as-context, defusion, values, and committed action) and the six dimensions of psychological inflexibility (experiential avoidance, lack of contact with the present moment, self-as-content, fusion, lack of contact with values, and inaction). Respondents were asked to answer the items while considering the previous two weeks on a 6-point scale (0 - “Never True” to 5 – “Always True”) and were averaged to create 12 individual subscale scores as well as two broader composite scores (representing global flexibility and inflexibility separately) so that higher scores indicated greater levels of the specific domain (i.e., flexibility or inflexibility) being measured. The MPFI subscales all demonstrated high levels of internal consistency in the sample (α′s ranging from .90 to .95) as did the global flexibility composite (α = 0.96) and the global inflexibility composite (α = 0.96).
Socio-economic status (SES). Families' socioeconomic status was calculated by averaging the standardized values of total family annual income and the highest level of parents’ educational attainment (using the response options of: 9th grade or less, 10th grade, 11th grade, High school diploma or GED, some college or trade school, AA degree or trade-school certificate, BA/BS degree, MA/MS degree, law degree, PhD/PsyD, DDS, and MD; r = 0.40, p < .001), then standardizing this composite variable. Higher scores indicate higher family SES.
Analytic strategy – primary model. For the primary analysis, both global flexibility and global inflexibility were modeled as primary outcomes. This model tested both perceived sleep quality and energy as mediators of the associations between three COVID-19-related stressors (i.e., health stress, work and parenting demands stress, and financial stress) and psychological flexibility/inflexibility. MPlus (v. 8.1; Muthén & Muthén, 2017) was employed to test the mediation model (Fig. 1A), which used bootstrapping to accommodate the asymmetry in the confidence intervals of the indirect paths of interest (MacKinnon, Lockwood, & Williams, 2004). In the current study, the primary analysis employed a bias-corrected bootstrap model with confidence intervals resampled 10,000 times. Due to the significant associations between families' socio-economic status (SES) and COVID-19-related health stressors in addition to research suggesting that families of lower SES were being disproportionately affected by the pandemic (Pew Research Center, 2020), this variable was included as a control in the analyses. Controlling for respondents' SES, the mediation model allowed us to test the hypotheses regarding the indirect effect of COVID-19-related stressors on psychological flexibility and inflexibility via respondents’ levels of both sleep quality and energy. The current model was fully identified, thereby yielding a perfectly fitting model.
Given the current study's large sample size, even fairly weak associations (i.e., those close to zero) often emerged as statistically significant. The results narrative was therefore focused on the effects that emerged at significance levels of p < .001, as those effects were more robust, accounting for larger portions of covariance and offering a greater likelihood of replicating in future samples. Only results that met this threshold are presented in Fig. 1B. The path coefficients presented in the figures have all been standardized.
Analytic strategy – Secondary models. Following up the primary model, secondary analyses were used to examine how both perceived sleep quality and energy might serve as mechanisms of the association between COVID-19-related stressors and the 12 specific dimensions of flexibility and/or inflexibility. Accordingly, two separate modified versions of the original model were run. In the first of these two secondary models, the global flexibility composite was substituted with the 6 distinct psychological flexibility subscales. Similarly, in the second of these models, the global inflexibility composite was substituted with the 6 distinct psychological inflexibility subscales. These models were fully identified, thereby giving perfect model fit.
6. Results
6.1. Preliminary analyses
Bivariate associations. As shown in Table 1 , all bivariate correlations of the key variables were moderately correlated in the expected directions. COVID-19 related stress was associated with greater inflexibility and perceived sleep quality and energy level were linked to lower inflexibility and higher flexibility. Although SES (i.e., a composite of income and education) was associated with lower health stress and financial stress (as could be anticipated), higher SES was associated with higher levels of stress from work and parenting demands, suggesting that the transition to social distancing and other pandemic-related situations (i.e., having to work from home, loss of child care) might have been experienced more acutely by those families with greater means. Taken as a set, these correlations suggest reasonably modest amounts of covariance among the key constructs, supporting the planned multivariate analyses.
Table 1.
Baseline descriptives and bivariate correlations of modeled variables.
| Measures |
(N = 1003) |
Bivariate Correlations |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predicting Mediators | Range | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 1. Health stress | 1–6 | 3.6 | 1.2 | – | ||||||
| 2. Demands of Work/Parenting stress | 1–6 | 3.2 | 1.3 | .35 | – | |||||
| 3. Financial stress | 1–6 | 3.0 | 1.5 | .42 | .36 | – | ||||
| Mediating Variables | ||||||||||
| 4. Perceived Sleep quality | 1–5 | 3.1 | 1.0 | -.30 | -.16 | -.23 | – | |||
| 5. Energy | 1–6 | 2.7 | 1.2 | -.13 | .00 | -.05 | .44 | – | ||
| Outcome Variables | ||||||||||
| 6. Psychological flexibility | 1–6 | 3.9 | 0.8 | .01 | -.06 | -.01 | .18 | .38 | – | |
| 7. Psychological inflexibility | 1–6 | 2.7 | 0.9 | .34 | .28 | .31 | -.32 | -.09 | -.30 | – |
| Control Variable | ||||||||||
| 8. Socio-economic status (SES) | −3.1–3.6 | 0.0 | 1.0 | -.20 | .15 | -.23 | .15 | .04 | -.04 | -.21 |
Note. All bolded correlations are significant at the p < .05 level. SES is a standardized composite of the sum of the standardized versions of respondent's education and annual income.
6.2. Primary analyses
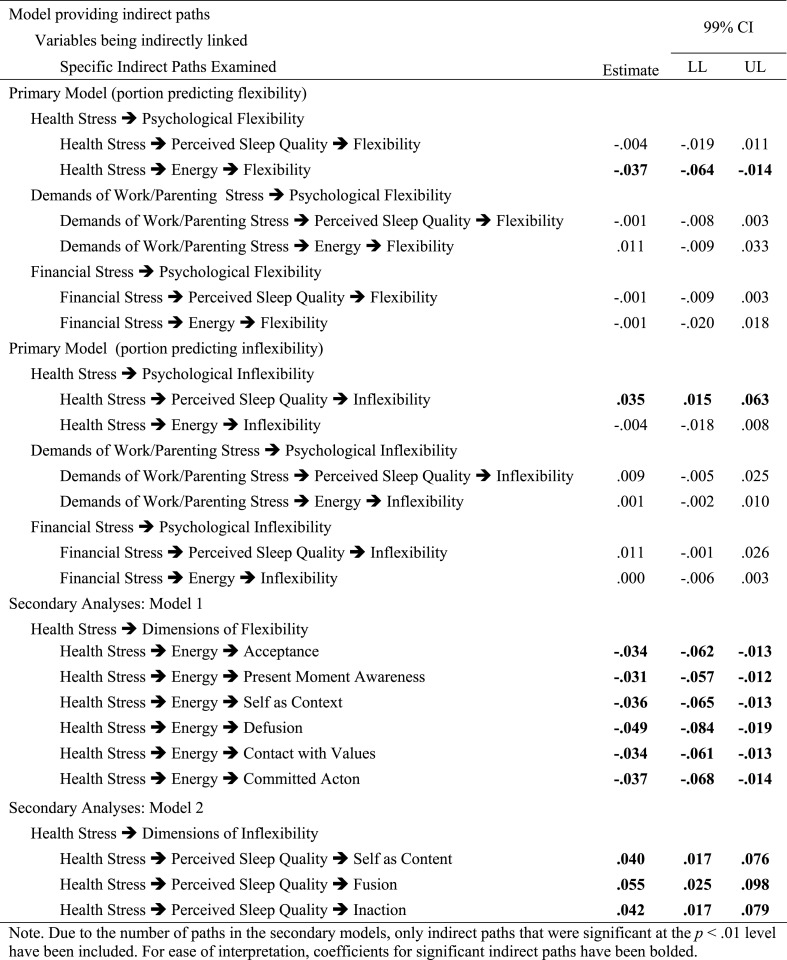
Predicting global composites of psychological flexibility and inflexibility. As shown in Table 2 and Fig. 1B, after controlling for all other paths in the model, health stress (β = 0.14, SE = 0.04) and work and parenting demands stress (β = 0.17, SE = 0.04) demonstrated direct predictive links to greater psychological inflexibility, suggesting that acute stress might promote the use of more rigid and inflexible responses to difficult thoughts, feelings, and experiences in the midst of that stress. Higher levels of health stress also predicted worse perceived sleep quality (β = −0.23, SE = 0.04; R2 = 0.12) and lower levels of energy (β = −0.15, SE = 0.04; R2 = 0.02), providing partial support for Hypotheses 1 A and 1 B. These results suggest that, for instance, respondents reporting 1 SD higher in health stress (approximately 1.2 points on health stress scale) would be expected to have .23 standard deviations (approximately .22 points) lower on their level of perceived sleep quality. Thus, higher levels of stress over concerns of contracting COVID-19 at the start of the pandemic in the United States were predictive of poorer perceived sleep and lower daily energy. Consistent with Hypothesis 2 B, higher levels of perceived sleep quality, in turn predicted lower levels of psychological inflexibility (β = −.21, SE = 0.04), supporting the possibility that sleep might serve as a key mechanism explaining the links between acute stress and the use of more rigid and inflexible responses to difficult thoughts, feelings, and experiences. Correspondingly, the indirect path linking COVID-19 related health stress to psychological inflexibility via poor perceived sleep quality emerged as statistically significant, supporting sleep quality as a possible mediational mechanism (Hypothesis 3 B; Table 3 ). Finally, consistent with Hypothesis 2C, higher levels of energy, in turn predicted higher levels of psychological flexibility (β = 0.38, SE = 0.03), supporting that possibility that lowered daily energy levels might serve as a key mechanism linking acute COVID-19 stress to the less frequent use of flexible responses to challenging experiences. Consistent with this, the indirect path linking COVID-19 related health stress to psychological flexibility via energy levels emerged as statistically significant, supporting levels of energy as a mediational mechanism (Hypothesis 4 A; Table 3).
Table 2.
Results from Mediation Model Predicting Psychological Flexibility and Inflexibility Global Composites.
| Portion of model | β | SE | p |
|---|---|---|---|
| Predicting Mediator: Perceived Sleep Quality | |||
| Health Stress | -.226 | .041 | <.0005 |
| Demands of Work/Parenting Stress | -.063 | .040 | .111 |
| Financial Stress | -.091 | .038 | .018 |
| SES | .103 | .036 | .004 |
| Predicting Mediator: Daily Energy | |||
| Health Stress | -.149 | .037 | <.0005 |
| Demands of Work/Parenting Stress | .052 | .037 | .161 |
| Financial Stress | -.006 | .037 | .868 |
| SES | -.005 | .035 | .886 |
| Predicting Outcome: Global Flexibility | |||
| Health Stress | .091 | .038 | .017 |
| Demands of Work/Parenting Stress | -.084 | .037 | .023 |
| Financial Stress | -.005 | .037 | .890 |
| SES | -.032 | .035 | .362 |
| Perceived Sleep Quality | .026 | .038 | .487 |
| Energy | .377 | .032 | <.0005 |
| Predicting Outcome: Global Inflexibility | |||
| Health Stress | .138 | .039 | <.0005 |
| Demands of Work/Parenting Stress | .170 | .035 | <.0005 |
| Financial Stress | .106 | .035 | .003 |
| SES | -.148 | .036 | <.0005 |
| Perceived Sleep Quality | -.209 | .037 | <.0005 |
| Energy | .035 | .040 | .384 |
Note. All coefficients presented are standardized (STDXY) values. Paths significant at p < .001 have been bolded for ease of interpretation.
Table 3.
Indirect Paths from COVID-Related-Stressors to Psychological Flexibility/Inflexibility (Primary Model) and their Individual Dimensions (Secondary Models).
Secondary analyses: Predicting specific dimensions of flexibility & inflexibility. When the flexibility composite was replaced with the 6 specific dimensions of flexibility in a secondary model, health stress demonstrated indirect links to each of the dimensions of flexibility via lower daily energy (see the bottom half of Table 3), supporting Hypothesis 4 A. As shown in Table 3, results of a separate secondary model in which the inflexibility composite was replaced with the 6 specific dimensions of inflexibility further revealed unique, indirect links between health stress and 3 of the 6 dimensions of inflexibility via perceived sleep quality: self-as-content, cognitive fusion, and inaction. These secondary results begin to highlight some of the more specific forms of flexibility and inflexibility most directly impacted by poor perceived sleep quality and daily energy levels.
7. Discussion
Drawing upon a contextual behavioral science framework, the current study is one of the first to examine stressors generated from the COVID-19 pandemic and their connection to parents' capacities to be psychologically flexible. Although the cross-sectional nature of these findings cannot confirm the direction of influence between the constructs, the primary model demonstrated that COVID-19-related stressors were associated with both psychological flexibility and inflexibility via parents' perceived sleep quality and daily functioning (i.e., energy), providing an initial mechanistic model linking stress to inflexibility. Furthermore, the secondary models highlighted that perceived sleep quality indirectly linked COVID-19-related stressors to three specific forms of inflexibility (i.e., self as content, fusion, inaction) and that parents' energy levels indirectly linked these stressors to all six dimensions of flexibility. Taken together, results from the current study not only help to clarify parents' behavioral responses to pandemic-related stressors, but they also highlight potential avenues through which parents’ psychological functioning might become impaired. As people navigate this unprecedented time, the current results offer a contextual behavioral science perspective to highlight the additional physical and psychological tolls (beyond getting physically sick with COVID-19) exacted on parents by the COVID-19 pandemic and the associated societal changes enacted to curb its spread.
7.1. Implications
Highlighting a stress-response framework. In his influential model of responses to stress, Selye (1983) distinguishes between “turn on” and “turn off” processes for handling stressful or uncontrollable circumstances. In the “turn on” state, individuals become hypervigilant to threat and thus struggle to return to a relaxed state, which is necessary for initiating and maintaining sleep (Pillar, Malhotra, & Lavie, 2000; Sadeh et al., 2004). In the “turn off” state, stressed individuals seek to conserve energy and withdraw from overly taxing behaviors, which might further deplete their resources (Selye, 1983). Accordingly, the model demonstrated robust associations between health-related stress and both perceived sleep quality and energy, thereby impacting the sleep-wake cycle at both ends. Specifically, it appeared that parents' concerns about their health and the health of their children and other loved ones were associated with maladaptive responses in the “turn on” state (i.e., sleep quality) and in the “turn off” state (i.e., energy). Taken together, it seems likely that health-related stress impacted parents’ engagement in restorative behaviors, such as sleep, in addition to their capacity to draw on energy stores needed to handle their current situations.
Possible biological mechanisms to explore. In biological terms, it is possible that such stress resulted in high levels of activity in the hypothalamic-pituitary-adrenal (HPA) axis, which would tend to impede sleep onset and maintenance (Reeth et al., 2000). Furthermore, the constant stress associated with the threat of getting sick potentially resulted in the HPA axis' heightened state. The increased and prolonged activity in the HPA axis, which is integral in the production of the stress hormone cortisol, might also have affected parents’ capacities to access the energy resources needed to respond to such stress (Smith & Vale, 2006). Although such physiological mechanisms were beyond the scope of the current investigation, future work could examine such processes to better characterize the impact of acute stress on sleep quality and daily energy levels.
Stress's impact on psychological flexibility/inflexibility. Both health-related stress and the stress associated with work and parenting posed by the pandemic (e.g., home schooling, providing childcare) were directly associated with psychological inflexibility. Previous findings have suggested that psychological flexibility could potentially buffer the adverse effects of stress on psychological health (e.g., Gloster, Meyer, & Lieb, 2017) and have highlighted that psychological flexibility might even serve as a key treatment mechanism to explain how ACT-based interventions can reduce stress (e.g., Wersebe; Lieb, Meyer, Hofer, & Gloster, 2018). The current results therefore build on this work by underscoring how the acute stress associated with a global pandemic might also serve to undermine psychological flexibility and instead promote the use more rigid and inflexible responses to difficult or challenging experiences. The current work extended this further by identifying both perceived sleep quality and energy as possible mechanisms explaining those links. The current findings therefore not only speak to the debilitating nature that stress potentially plays on psychological functioning, but also highlight two processes through which this occurs. Building on research linking sleep and psychological inflexibility (e.g., Peltz et al., 2020), the current study suggests that parents' perceptions of poor sleep quality likely facilitated the link between health-related stress and their tendencies to engage in reactive and overly rigid interpretations of their experiences of their current situations (i.e., psychological inflexibility). In a parallel manner, health-related stress also seems to have limited parents' energy levels, which negatively impacted their abilities to flexibly engage with the world and adaptively process challenging experiences.
Lack of internal resources as a mechanism. The current results suggested that parents’ lower energy levels might have exhausted the cognitive resources needed to engage the diverse components of flexibility, such as accepting difficult feelings, gently experiencing them (i.e., defusion), maintaining a broader perspective (i.e., self-as-context), and taking action toward deeper goals and priorities even in the face of difficult experiences and setbacks. Similarly, disrupted and poor-quality sleep would seem to have left parents depleted, rendering them more susceptible to engaging in more reactive and rigid responses, by either avoiding difficult feelings and experiences entirely, or by fusing with them and judging or shaming oneself for having those thoughts and experiences.
Potential avenues of intervention. As illustrated in the conceptual model (Fig. 1A), it appears that the stress created by the pandemic has a dual impact on the sleep-wake cycle, wherein it not only impairs parents' capacities to sleep well, but it also limits their energy levels during the day. In that light, there are multiple avenues through which parents might be able to inoculate themselves to health-related stress' deleterious consequences on their sleep and daily energy, and its potential impact on their psychological functioning. First, parents can pursue proper sleep hygiene (e.g., avoiding caffeine in the afternoon, creating a quiet, dark, and cool sleep environment), as these behaviors have been shown to improve sleep quality (Brown, Buboltz, & Soper, 2006; LeBourgeois, Giannotti, Cortesi, Wolfson, & Harsh, 2005). Second, parents can incorporate strategies to decrease stress, such as mindful meditation (Hoge et al., 2018), exercise (Salmon, 2001), and other forms of self-care (e.g., seeking social support). Not only has social support been shown to decrease occupational stress, but it has also been associated better sleep quality (e.g., Pow, King, Stephenson, & Delongis, 2017). Finally, although a large literature has demonstrated the benefits of cognitive behavioral therapy for insomnia (CBT-I; see Bos, 2018 for a review), the current results linking perceived sleep quality to psychological inflexibility highlight the unique benefits of using ACT to address sleep problems. In fact, ACT-based interventions have been shown to be effective in improving both adults' sleep and mental health (e.g., Daly-Eichenhardt et al., 2016). Thus, the current results suggest that augmenting self-care and sleep hygiene strategies with ACT could powerfully promote the use of psychologically flexible responses over the use of psychologically inflexible responses in the midst of a global crisis like the COVID-19 pandemic. It must also acknowledge that the analyses included parents' reports of poor sleep quality and energy levels as simultaneous predictors in the mediation models due to the potential impact of COVID-19-related stressors on these processes. Although Selye’s (1983) model supports the dual effect of stress on both sleep and energy, it is also possible that parents' poor sleep might have led to lower energy levels during the day. Future studies that can examine these processes longitudinally would benefit by examining models that test these assumptions in a more systematic way.
7.2. Limitations and future directions
Several limitations in the current study must be acknowledged. First, due to the cross-sectional nature of the data, the mediation analyses preclude any conclusions to be drawn about the direction of influences amongst the constructs. Although the models can provide insight into possible mechanisms, longitudinal data is necessary to determine the directionality of the mediation tested. For instance, increased inflexibility remains a robust predictor of sleep problems (e.g., Lundh, 2005), and psychologically flexible people tend to engage in more adaptive responses to stressful situations (Kashdan & Rottenberg, 2010). Future studies should examine these associations across multiple timepoints to better ascertain the direction of effects. Second, all measures are self-report, increasing the potential for response-bias. In addition, the survey measure of perceived sleep quality focused on subjective ratings and did not include more objective indicators of sleep quality (e.g., latency, waking after sleep onset episodes). It also must be acknowledged that the COVID-19-related stress variables (i.e., health stress, stress from parenting/work demands, and financial stress) were created by the authors for this specific study. Although they all demonstrated adequate internal consistency (α′s ranging from .71 to .84), they had not been previously empirically validated, due, in part, to the relative novelty of assessing these emerging constructs during the current COVID-19 pandemic. Future studies should augment self-report surveys with additional methods (i.e., daily sleep diaries, actigraphy, examining cortisol levels for objective measurements of individuals' stress responses) and ideally include empirically validated measures to test the presented models more thoroughly. Third, potential influences on sleep quality and energy levels, such as sleep medications and other substances, were not assessed in the current study. As a consequence, the degree to which such factors could have influenced the results remains unclear. Future studies would benefit from including these constructs in their assessments to characterize the unique influence of these potential constructs and the degree to which the current findings remain consistent after controlling for those factors. Finally, the sample was predominately Caucasian, female, and had engaged in more years of schooling than a nationally representative sample. Because the effects of the novel coronavirus and the subsequent consequences (e.g., job loss) have been shown to disproportionately affect lower income and minority populations in the United states (Gross et al., 2020; Parker et al., 2020), the results primarily speak to the potential impact of COVID-related stressors on psychological processes within a more advantaged population of the United States who might have experienced less severely disruptive consequences as a result of the pandemic. To the degree that this restricted the range on the COVID-19 stress captured in this sample, this could have served to attenuate the strength of the associations examined, rendering them slight underestimations of the actual links between these processes. Despite this limitation, the level of family disruption captured within the current sample provided robust support for the proposed model. Accordingly, future studies should seek more diverse populations to ensure the current results generalize to a broad population.
8. Conclusion
The current study underscores the wide-ranging consequences occurring during the COVID-19 pandemic. Not only have families had to confront an unprecedented health crisis, but the stressors associated with the virus, social isolation, and the dire repercussions on people's jobs and the economy also appear to be exacting a toll on parents. Given the systemic and interrelated nature of relationships within families (Cox & Paley, 2003), it seems likely that the stress parents are experiencing due to the pandemic will reverberate to other parts of the family (e.g., marital functioning, parent-child relationships) and that parents will also be affected by the stress experienced by their children and other members of their family system. Although this study is one of the first to link pandemic-related stressors to the domains of psychological flexibility and inflexibility and will thus benefit from replication, the findings highlight key components of psychological flexibility impacted in the current crisis that could be directly addressed by ACT, such as fusion and inaction. Future research should continue to investigate the ways in which poor sleep or low day-to-day levels of energy might impede parents' capacities to be psychologically flexible, and it highlights the growing need to further develop the understanding of the connections between sleep and mindfulness (e.g., Ong et al., 2012). In the end, until the pandemic and the related stressors that it is causing cease, parents will need as much support as possible to maintain health behaviors and psychological health. It is hoped that by underscoring the importance of sleep and of energy in the face of the pandemic-related stressors that parents will not forget that self-care is essential during this crisis.
Declaration of competing interest
None.
Contributor Information
Jack S. Peltz, Email: jpeltz@daemen.edu.
Jennifer S. Daks, Email: jdaks@ur.rochester.edu.
Ronald D. Rogge, Email: ronald.rogge@rochester.edu.
References
- Bai Y., Lin C.-C., Lin C.-Y., Chen J.-Y., Chue C.-M., Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatric Services. 2004;55(9):1055–1057. doi: 10.1176/appi.ps.55.9.1055. [DOI] [PubMed] [Google Scholar]
- Bluth K., Wahler R.G. Does effort matter in mindful parenting ? Mindfulness. 2011;2:175–178. doi: 10.1007/s12671-011-0056-3. [DOI] [Google Scholar]
- Bos T. The efficacy of CBT-I on insomnia and depressive symptoms in comorbid adult patients: A systematic review and meta-analysis. Sleep. 2018;41(July):A166. [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown F.C., Buboltz W.C., Soper B. Development and evaluation of the sleep treatment and education program for students (STEPS) Journal of American College Health. 2006;54(4):231–237. doi: 10.3200/JACH.54.4.231-237. [DOI] [PubMed] [Google Scholar]
- Cava M.A., Fay K.E., Beanlands H.J., Mccay E.A., Wignall R. The experience of quarantine for individuals affected by SARS in Toronto. 2005;22(5):398–406. doi: 10.1111/j.0737-1209.2005.220504.x. [DOI] [PubMed] [Google Scholar]
- Couyoumdjian A., Sdoia S., Tempesta D., Curcio G., Rastellini E., De Gennaro L. The effects of sleep and sleep deprivation on task-switching performance. Journal of Sleep Research. 2010;19:64–70. doi: 10.1111/j.1365-2869.2009.00774.x. 1 PART. 1. [DOI] [PubMed] [Google Scholar]
- Cox M.J., Paley B. Understanding families as systems. Current Directions in Psychological Science. 2003;12(5):193–196. doi: 10.1111/1467-8721.01259. [DOI] [Google Scholar]
- Daly-Eichenhardt A., Scott W., Howard-Jones M., Nicolaou T., McCracken L.M. Changes in sleep problems and psychological flexibility following interdisciplinary acceptance and commitment therapy for chronic pain: An observational cohort study. Frontiers in Psychology. 2016;7:1–12. doi: 10.3389/fpsyg.2016.01326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dongen H.P., Maislin G., Mullington J.M., Dinges D.F. The cumulative cost of additional wakefulness : Dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26(2):117–126. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- Gloster A.T., Meyer A.H., Lieb R. Psychological flexibility as a malleable public health target: Evidence from a representative sample. Journal of Contextual Behavioral Science. 2017;6:166–171. doi: 10.1016/j.jcbs.2017.02.003. [DOI] [Google Scholar]
- Gouveia M.J., Carona C., Canavarro M.C., Moreira H. Self-compassion and dispositional mindfulness are associated with parenting styles and parenting stress: The mediating role of mindful parenting. Mindfulness. 2016;7:700–712. doi: 10.1007/s12671-016-0507-y. [DOI] [Google Scholar]
- Grandner M.A., Tubbs A., Jean-Louis G., Seixas A., Hale L., Branas C. Daytime sleepiness in the community: Implications for sleep, circadian, and physical health. Sleep. 2020;43:A155–A156. [Google Scholar]
- Hanson M.D., Chen E. Daily stress, cortisol, and sleep: The moderating role of childhood psychosocial environments. Health Psychol. 2010;29(4):394–402. doi: 10.1037/a0019879. [DOI] [PubMed] [Google Scholar]
- Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerging Infectious Diseases. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes S.C., Strosahl K.D., Wilson K.G. Guilford Press; 2011. Acceptance and commitment therapy: The process and practice of mindful change. [Google Scholar]
- Hoge E.A., Bui E., Palitz S.A., Schwarz N.R., Owens M.E., Johnston J.M. The effect of mindfulness meditation training on biological acute stress responses in generalized anxiety disorder. Psychiatry Research. 2018;262:328–332. doi: 10.1016/j.psychres.2017.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell A.J., Digdon N.L., Buro K. Mindfulness predicts sleep-related self-regulation and well-being. Personality and Individual Differences. 2010;48(4):419–424. doi: 10.1016/j.paid.2009.11.009. [DOI] [Google Scholar]
- Howell A.J., Digdon N.L., Buro K., Sheptycki A.R. Relations among mindfulness, well-being, and sleep. Personality and Individual Differences. 2008;45(8):773–777. doi: 10.1016/j.paid.2008.08.005. [DOI] [Google Scholar]
- Kashdan T.B., Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review. 2010;30(4):865–878. doi: 10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBourgeois M.K., Giannotti F., Cortesi F., Wolfson A.R., Harsh J. The relationship between reported sleep quality and sleep hygiene in Italian and American adolescents. Pediatrics. 2005;115(1 Suppl):257–265. doi: 10.1542/peds.2004-0815H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundh L.G. The role of acceptance and mindfulness in the treatment of insomnia. Journal of Cognitive Psychotherapy. 2005;19(1):29–39. doi: 10.1891/jcop.19.1.29.66331. [DOI] [Google Scholar]
- MacKinnon D.P., Lockwood C.M., Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39(1):99–128. doi: 10.1207/s15327906mbr3901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L.K., Muthén B.O. Muthén & Muthén; Los Angeles, CA: 2017. Mplus user's guide. [Google Scholar]
- Ong J.C., Manber R., Segal Z., Xia Y., Shapiro S., Wyatt J.K. A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep. 2014;37(9):1553–1563. doi: 10.5665/sleep.4010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong J.C., Ulmer C.S., Manber R. Improving sleep with mindfulness and acceptance: A metacognitive model of insomnia. Behaviour Research and Therapy. 2012;50(11):651–660. doi: 10.1016/j.brat.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong J.C., Xia Y., Smith-Mason C.E., Manber R. A randomized controlled trial of mindfulness meditation for chronic insomnia: Effects on daytime symptoms and cognitive-emotional arousal. Mindfulness. 2018;9(6):1702–1712. doi: 10.1007/s12671-018-0911-6. [DOI] [Google Scholar]
- Peltz J.S., Rogge R.D., Bodenlos J.S., Newman J.N., Pigeon W.R. Changes in psychological in flexibility as a potential mediator of longitudinal links between college students ’ sleep problems and depressive symptoms. Journal of Contextual Behavioral Science. 2020;15:110–122. doi: 10.1016/j.jcbs.2019.12.003. [DOI] [Google Scholar]
- Pew Research Center P.R. 2020. About half of lower-income Americans report household job or wage loss due to COVID-19. [Google Scholar]
- Pillar G., Malhotra A., Lavie P. Post-traumatic stress disorder and sleep—what a nightmare! Sleep Medicine Reviews. 2000;4(2):183–200. doi: 10.1053/smrv.1999.0095. [DOI] [PubMed] [Google Scholar]
- Pow J., King D.B., Stephenson E., Delongis A. Does social support buffer the effects of occupational stress on sleep quality among paramedics? A daily diary study. 2017;22(1):71–85. doi: 10.1037/a0040107. [DOI] [PubMed] [Google Scholar]
- Reeth O. Van, Weibel L., Spiegel K., Leproult R., Dugovic C., Maccari S. Interactions between stress and sleep. From basic research to clinical situations. 2000;4(2):201–219. doi: 10.1053/smrv.1999.0097. [DOI] [Google Scholar]
- Rogge R.D., Daks J.S., Dubler B.A., Saint K.J. It's all about the process: Examining the convergent validity, conceptual coverage, unique predictive validity, and clinical utility of ACT process measures. Journal of Contextual Behavioral Science. 2019;14:90–102. doi: 10.1016/j.jcbs.2019.10.001. [DOI] [Google Scholar]
- Rolffs J.L., Rogge R.D., Wilson K.G. Disentangling components of flexibility via the Hexaflex model: Development and validation of the multidimensional psychological flexibility inventory (MPFI) Assessment. 2018;25(4):458–482. doi: 10.1177/1073191116645905. [DOI] [PubMed] [Google Scholar]
- Sadeh A., Keinan G., Daon K. Effects of stress on sleep: The Moderating role of coping style. Health Psychol. 2004;23(5):542–545. doi: 10.1037/0278-6133.23.5.542. [DOI] [PubMed] [Google Scholar]
- Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: A unifying theory. Clinical Psychologist. 2001;21(1):33–61. doi: 10.1016/s0272-7358(99)00032-x. [DOI] [PubMed] [Google Scholar]
- Selye H. The stress concept: Past, present and future. In: Cooper C.L., editor. Stress research. Wiley; New York, NY: 1983. pp. 1–20. [Google Scholar]
- Smith S.M., Vale W.W. The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues in Clinical Neuroscience. 2006;8(4):383–395. doi: 10.31887/DCNS.2006.8.4/ssmith. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel K., Leproult R., Cauter E. Van. Vol. 354. 1999. pp. 1435–1439. (Impact of sleep debt on metabolic and endocrine function). [DOI] [PubMed] [Google Scholar]
- Wersebe H., Lieb R., Meyer A.H., Hofer P., Gloster A.T. The link between stress, well-being , and psychological flexibility during an Acceptance and Commitment Therapy self-help intervention. International Journal of Clinical and Health Psychology. 2018;18:60–68. doi: 10.1016/j.ijchp.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L., Buysse D.J., Germain A., Moul D.E., Stover A., Dodds N.E. Development of short forms from the PROMIS sleep disturbance and sleep-related impairment item banks. Behavioral Sleep Medicine. 2012;10(6):6–24. doi: 10.1080/15402002.2012.636266. [DOI] [PMC free article] [PubMed] [Google Scholar]