Abstract
Background
Effective emergency care (EC) reduces mortality, aids disaster and outbreak response, and is necessary for universal health coverage. Surge events frequently challenge Pacific Island Countries and Territories (PICTs), where robust routine EC is required for resilient health systems. We aimed to describe the current status, determine priority actions and set minimum standards for EC systems development across the Pacific region.
Methods
We used a prospective, multiphase, expert consensus process to collect data from PICT EC stakeholders using focus groups, electronic surveys and panel review between August 2018 and April 2019. Data were analysed using descriptive statistics, consensus agreement and graphic interpretation. We structured the research according to the World Health Organisation EC Systems and building block framework adapted for the Pacific context.
Findings
Over 200 participants from 17 PICTs engaged in at least one component of the multiphase process. Gaps in functional capacity exist in most PICTs for both facility-based and pre-hospital care. EC is a low priority across the Pacific and integrated poorly with disaster plans. Participants emphasised human resource support and government recognition of EC as priority actions, and generated 24 facility-based and 22 pre-hospital Pacific EC standards across all building blocks.
Interpretation
PICT stakeholders now have baseline indicators and a comprehensive roadmap for EC development within a globally recognised health systems framework. This study generates practical, context-appropriate tools to trigger further research, conduct evidence-based advocacy, drive future improvements and measure progress towards achieving universal health access for Pacific peoples.
Funding
Secretariat of the Pacific Community (partial)
Keywords: Emergency care, Emergency medical services, Pacific Islands/Pacific region, World Health Organisation, Health systems, Health Priorities, Consensus
Research in Context.
Evidence before this study
The 2019 World Health Assembly (WHA) Resolution 72.16 explicitly places emergency care (EC) as central within a health system in order to achieve universal coverage and provide timely care to the acutely ill and injured. As the frontline service between the community and health facilities, a weak EC system increases vulnerability to surge events and limits effective public health and clinical care interventions. Pacific Island Countries and Territories (PICTs) share a substantial burden of environmental, climatic and communicable disease threats and can work collaboratively to address regional health priorities that are locally identified, evidence-based and Pacific context-relevant. We searched PubMed, Google Scholar, WHO resources, Pacific and grey literature using search terms; ‘Pacific Islands / region’, ‘emergency care’, ‘emergency care systems and/or status’, ‘emergency care assessment’, ‘emergency care priorities / standards’ and found a paucity of information about EC systems in the Pacific region. There are few studies from individual PICTs highlighting specific components of clinical EC, a narrow focus on emergency capacity in disasters without linkage to everyday system resilience, and no previously identified EC priorities or standards specifically for the Pacific region. Examples of PICT collaboration and models of regional engagement exist to produce standards for peri‑operative practice and measure surgical indicators. Work from Africa describes a facility-based assessment tool and a multiphase consensus methodology for generating context-appropriate EC quality indicators. The WHO health system building blocks underpin tools specifically for EC, including a system assessment framework designed for national use, and which has been adapted for a proposed pre-hospital system assessment tool. We identified substantial evidence gaps about EC status, capacity and systems development in the Pacific region, but an opportunity for collaboration using the health systems framework and consensus approach.
Added value of this study
We engaged over 200 stakeholders from 17 different PICTs to generate 24 facility-based and 22 pre-hospital standards, matched with immediate and longer-term priority actions for EC development across all system building blocks. For the first time, we describe the status and basic functional capacity of EC systems across the Pacific region, gaining insight into the ability of PICTs to meet surge demands during the current COVID-19 global pandemic. We adapted the WHO health systems building blocks for the Pacific EC context, and applied this framework throughout a multiphase, iterative, consensus process involving both quantitative and qualitative methods, thereby modelling a collaborative approach to relevant data collection and interpretation. By analysing data both regionally and for each PICT, we have shown overall patterns and highlighted gaps where system components are least developed within individual countries. The Human Resources and Training building block is central to building effective EC systems in PICTs, with minimum regional standards set for training, staffing models, employment structures and legal protection. Regional recognition of EC as essential within the health system is a required standard, in order to drive specific priority actions and meet other standards for Infrastructure and Equipment, Leadership and Governance, Process, and Data building blocks.
Implications of all the available evidence
The Pacific region has limited capacity to provide safe and effective EC with low resilience to increase function at times of surge demand. PICT health leaders can see their EC system strengths and gaps, and now have a clear set of locally generated, context relevant priority actions and minimum regional standards that provide a roadmap for pre-hospital and facility-based systems development both within each PICT and across the Pacific region as a whole. By conforming to a globally recognised health systems framework, these tools align with the WHA Resolution 72.16 call to action and can be used for policy and planning, research, monitoring and future evaluation of individual PICT and regional progress. The research process has generated momentum for a Pacific EC community of practice, modelled a collaborative methodology and suite of tools that can be adapted for other regional contexts, and created advocacy aids to enhance PICT understanding about the role and importance of EC within the health system. This work enables PICT and Pacific regional health leaders to take positive steps that will build resilience and capacity within their health systems for future surge events and universal access for all Pacific peoples who need emergency health care.
Alt-text: Unlabelled box
Introduction
All people may experience acute illness or injury in their life-course that requires time-critical intervention to prevent deterioration, disability or death, regardless of whether urgent care is available or not. [1] The provision of safe, effective and timely emergency care (EC) is essential to a health system in order to achieve universal access [2] and meet Sustainable Development Goal (SDG) targets for communicable and non-communicable disease, maternal and child health, mental illness, addictions and injuries. [3] As the horizontal interface between the community and healthcare systems, EC is often the first or only contact with health services by patients and their carers. It is therefore essential to public health initiatives, [4] human rights [5] and effective outbreak, disaster and other surge responses. [6] Indeed, robust pre-hospital [7] and facility-based services [8] are critical to the health system response in the current COVID-19 pandemic.
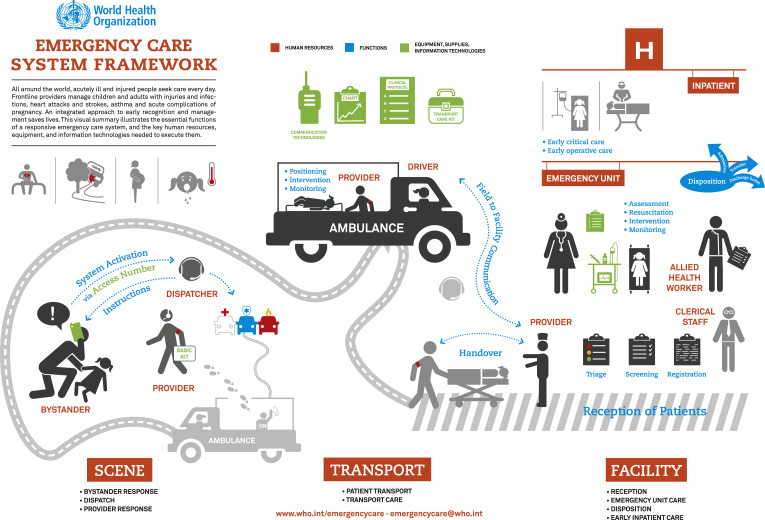
The World Health Organisation (WHO) describes EC within a Systems Framework (ECSF) [9] (Fig. 1); dividing care between the scene of illness or injury, during transport (pre-hospital) and at a facility, underpinned by essential and intersecting building blocks. [10] The burden of mortality and morbidity from conditions amenable to EC falls disproportionally on low- and middle-income countries (LMICs), [11] yet these countries are where access to safe, effective and reliable EC is often most limited. [12] By passing Resolution 72•16 in May 2019, the World Health Assembly (WHA) now recognises the urgency of building EC systems and calls on all countries to strengthen the provision of EC as part of universal health coverage to ensure timely and life-saving care to the acutely ill and injured. [2] Member states are urged to assess and build their capacity within the WHO framework and across all EC system building blocks.
Fig. 1.
WHO emergency care systems framework.
As the greatest proportion of lives saved globally can occur in LMICs with safe and reliable EC, [13,14] guidance on how to prioritise action and set achievable standards of system development are essential. Delphi and expert consensus methods have been used to define key areas and priorities for EC development in LMICs, [15] and specify functional EC requirements at different facility levels in sub-Saharan Africa. [16] The WHO has recently developed a survey-based tool for national governments to assess status, identify gaps and prioritise actions for EC systems development using a structured framework; the Emergency Care Systems Assessment (ECSA) tool. [6] Using an accepted health systems approach to create EC standards enables global consistency, [17] but should be adapted to specific contexts to improve relevance and applicability. [18]
Pacific Island Countries and Territories (PICTs) are largely LMICs connected as a region through shared political, institutional, socio-cultural and language links, despite substantial variance in population size and geographies. [19] The Pacific region also shares an epidemic of non-communicable disease (NCDs) [20] coupled with the ongoing burden of communicable disease, maternal and child mortality, mental ill-health, gendered violence and road traffic injuries, plus the existential threat from an increasingly unstable climate and surge events. [21] Individual PICTs have particular burdens of fatal emergency conditions [11,14] such as obstetric complications (haemorrhage, sepsis, obstruction) in Papua New Guinea (PNG), childhood diarrhoeal and respiratory infections in Kiribati, and acute ischaemic events in Fiji. [22,23] All of these conditions require effective EC systems to address acute manifestations of disease or injury, yet robust systems for pre-hospital and facility-based EC in PICTs are lacking. As exemplified by their strong response to the NCD crisis, [24] PICT governments can accelerate regional progress to achieve health targets. Similarly, PICT clinicians have collaborated regionally to measure surgical indicators [25] and develop Pacific Island standards for perioperative practice. [26] In the context of the urgent need to assess and build safe, accessible and resilient EC systems in all PICTs, we aimed to describe the current status of EC, and define relevant standards and priority actions for EC development across the Pacific region using the WHO ECSF and health system building blocks adapted to the Pacific context.
Methods
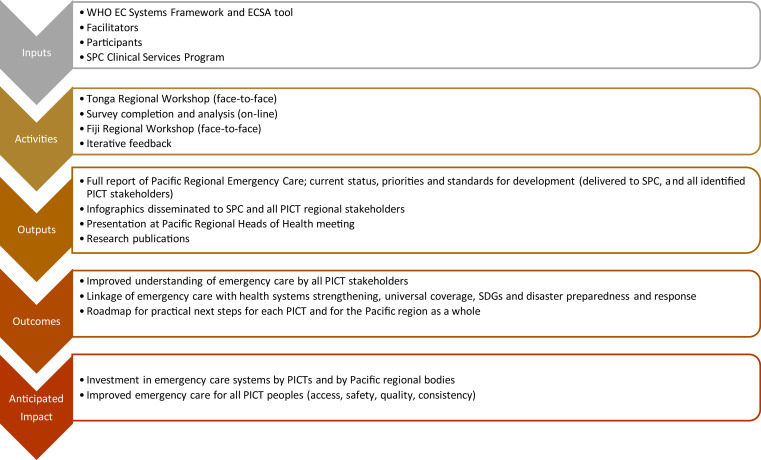
We conducted a prospective, three-phase, expert consensus process [27] over nine months from August 2018 to April 2019 to determine the current EC status, development priorities and regional standards for EC in the Pacific. We adopted a collaborative, participatory and strengths-based approach [28] and used a logical framework [29] to document inputs, activities, outputs, expected outcomes and anticipated impact (Fig. 2) across the three iterative, stepped phases of the project. The first phase was a regional face-to-face workshop held in Tonga in August 2018 involving key PICT stakeholders, followed by iterative feedback from participants. By introducing the WHO ECSF and brainstorming regional priorities for EC development at facilities and in the pre-hospital setting, this process enabled PICT participants to frame EC within the health system and provided content that informed the subsequent survey and workshop phases of the project.
Fig. 2.
Logical framework for the Pacific Regional Emergency Care project.
The second phase consisted of two cross-sectional on-line surveys (pre-hospital and facility-based, Appendix pp 1–32) with three sections each, exploring current EC status, priorities for EC development and standards for regional EC systems. Following the surveys we held another face-to-face workshop in Fiji in December 2018 where survey results were analysed, discussed, and consensus agreements ratified. The final project phase included feedback by PICT participants, ultimate analysis and interpretation of results, and presentation to the regional Pacific Heads of Health meeting in Fiji in April 2019. Each activity informed subsequent activities through a continuous, iterative and consultative process.
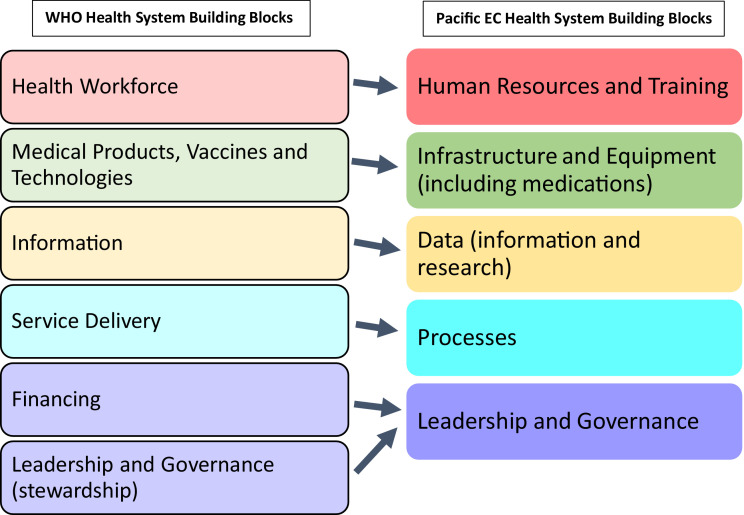
Survey tool development
We adapted the WHO health system building blocks for the Pacific EC context to emphasise the importance of facility infrastructure and EC processes such as triage (Fig. 3). Within the WHO ECSF, these Pacific EC system building blocks became the architecture for all data collection and analysis: Human Resources and Training, Infrastructure and Equipment, Data (information and research), Processes, Leadership and Governance. The first section of the facility-based survey contained ten questions that explored systems capacity and function from the national referral hospital to a district or provincial hospital level. Most questions required a graded response from five options ranging from no capacity or function, through to a high level of development across the entire country. Three questions about pre-hospital EC explored capacity for care at the scene of illness or injury, care during transport and the level of systems development overall. The second and third sections of both the facility-based and pre-hospital surveys explored regional priorities for EC development and minimum standards of EC that could apply across all PICTs. All EC functions and activities link to each building block, which are depicted as separate entities but are interdependent within a complex system. [30]
Fig. 3.
WHO and Pacific emergency carey health system building blocks.
In order for survey participants to rank priority development actions, we provided a table of EC inputs and functions across each building block, following a patient journey through the pre-hospital and facility system (Appendix pp 9–10, 25). Participants were asked to think regionally, and rank urgency of action as an immediate priority, something to be achieved within 5 years, or as a long-term goal; reflecting the real-life time frame of many development activities in the Pacific. Participants also provided an overall priority ranking of the Pacific EC system building blocks. To determine regional EC standards, participants were asked to select any (or all) of 5 options of potential EC standards applicable to all PICTs across each of the building blocks, apart from Human Resources and Training, which had additional questions specifically for training standards and requirements. Clinicians who did not work in PICTs but were familiar with resource-limited contexts piloted the surveys.
Setting, participants, sampling
Together with Australia, New Zealand, France and the United States of America (USA), the 22 PICTs of the Pacific region own and govern the Secretariat of the Pacific Community (SPC), which is the principal regional scientific, technical and international development organisation. [31] The Clinical Services Program (CSP) within the SPC Public Health Division aims to provide regional governance, support research and implement regional approaches to improve clinical service delivery. In partnership with the CSP, we sought to engage EC stakeholders from 16 different PICTs, excluding the French collectivities (New Calendonia, French Polynesia, Wallis and Futuna), the USA commonwealth territories (Guam, Commonwealth of the Northern Mariana Islands, American Samoa) and the British Overseas Territory (Pitcairn Island), and including Timor-Leste, a small Pacific country with strong socio-cultural links to the SPC PICTs.
Sampling for this project was purposive, opportunistic and enhanced through snowball methods. Participation throughout the process was open to any PICT stakeholder with an interest in EC: clinicians; administrators; policy-makers, without exclusion criteria. Workshop participants were mostly EC clinicians (doctors and nurses) nominated by their national governments or representative bodies, but highly dependant on individual availability and access to external funding. The Fiji workshop coincided with a regional EC conference, thereby enabling wider PICT engagement. Remote participation using real-time communications technology was not available at either workshop. Surveys were sent by email using researcher networks and SPC regional contacts. We deliberately targeted known EC leaders and other senior clinicians across PICTs in order to engender rapid stakeholder engagement and encourage survey snowball recruitment through internal networks within countries. As approximately 50 doctors with EC qualifications (Diploma or Masters degree) worked in ten of the target PICTs, and assuming an average of three nurse EC stakeholders per country, our estimated baseline denominator for survey response was 98 participants. Although survey response was voluntary and anonymous, participants had the opportunity to provide their contact details, receive feedback, provide further input and receive acknowledgement in all outcome documents.
Data collection, analysis and interpretation
Facility-based and pre-hospital surveys used a secure platform (SurveyMonkey Inc. San Mateo, California, USA. 2019) to collect data over six weeks from 1st November – 15th December 2018. Survey data was exported in to Microsoft Excel (Microsoft Corporation, 2016) for management and analysis. For the first section of both surveys (current status), we generated summary statistics of demographic details and question responses for the region as a whole and for each PICT individually. Proportions of the total regional responses for each graded level were summarised using percentages and are presented in tables separated in to pre-hospital and facility EC. Data on triage systems in use around the Pacific region were analysed using geographical mapping.
We compared results for each PICT against the EC standards determined through consensus in the associated components of this project. Where greater than 50% of the responses for each question met or exceeded the set standard, then we determined that this component of the EC system was at an acceptable level. A simple majority cut-off was used in this instance in the absence of equal representative sampling, or the ability to follow up directly with the anonymous participants from each PICT. At the request of SPC, tables were constructed to enable comparison between PICTs and to identify which EC system components were least developed across the region.
We conducted preliminary analyses for survey sections two and three immediately prior to the face-to-face workshop held on 5th December 2018 in Fiji, and presented this data to the workshop participants. For both development priority and regional standard statements, participants accepted a 70% survey agreement benchmark for adoption of each statement. Statements that received between 65 and 70% survey agreement were also open for discussion and adoption through consensus. The 70% benchmark was chosen to enable stratification of priorities and standards, and avoid either everything becoming a priority (unfeasible) or nothing identified for action (untenable). All priority and standard statements were open for re-wording, refinement and adaptation according to group consensus. Meticulous workshop minutes documented the discussion and agreed outcomes. Willing participants provided contact details and were able to provide subsequent feedback through both the survey tools and directly by email to the researchers. At all phases of the project, participants could provide written or verbal free-text responses to add or highlight any component of EC for consideration. All identified participants received draft versions of the consensus priorities and standards for comment prior to finalisation and presentation to regional health leaders.
For practical use, we grouped EC development priorities in to ‘immediate’, and ‘longer term’, thereby combining the survey categories ‘should achieve in 5 years’ with ‘long term goal’ in our data analysis. Priority and standard statements that met the 70% benchmark, or agreement through discussion, were ratified through group consensus as an adopted statement and not subject to further analysis. Both priority and standard data are presented as descriptive lists within each building block.
The Australasian College for Emergency Medicine (ACEM) collaborated to produce infographics using summary data of all survey component results for both pre-hospital and facility-based EC. These documents accompanied an infographic explaining what EC is and why it is important for PICTs, for wide dissemination and advocacy around the Pacific region (Appendix pp 33–35).
Role of the funding source
The Pacific Community CSP initiated and supported this project through funding and providing logistical support for regional delegates (including PA-E and PT) to attend and participate in face-to-face workshops. The CSP also facilitated on-line regional engagement, funded two researchers to perform specific tasks (GP and AC), participated as co-researchers (BK) and explicitly granted approval for publication of research outcomes. The corresponding author (GP) has not received payments to write this article, and had full access to all the data in the study. The corresponding author takes final responsibility for the submission of this paper for publication.
The Monash University (Australia) Human Research and Ethics Committee also approved all components of this research project (Project ID: 17220).
Results
Fifteen participants from seven different PICTs attended the Tonga workshop and 50 stakeholders representing nine different PICTs participated in the Fiji workshop. The survey email links were sent to 112 stakeholders in 16 different PICTs and by 4th December 2018 for the preliminary analysis, there were 156 facility-based and 119 pre-hospital survey responses from 17 different PICTs. At completion, the facility-based survey had 174 participants and pre-hospital survey 130 participants from 17 different PICTs, thereby exceeding our baseline response estimate. Although not included in the initial recruitment, a response was received from American Samoa, which was included in the analysis for breadth of regional representation. Table 1 shows details of PICT, role and facility-type of participants, including the initial number of surveys sent to each PICT. Not all respondents answered all demographic questions, and not all questions were completed by every participant. Survey completeness ranged from 84 – 94% in section one, and 70 – 85% for sections two and three.
Table 1.
Country, role and facility-type of participants.
| Tonga Workshop: Number | Facility Survey: Number by 4th Dec.2018 | Facility Survey: Total Number (%) | Pre-Hospital Survey: Number by 4th Dec.2018 | Pre-Hospital Survey: Total Number (%) | Fiji Workshop: Number | |
|---|---|---|---|---|---|---|
| Country (initial survey number (112)) | Total 15 | Total 152 | Total 170 | Total 117 | Total 127 | Total 50 |
| American Samoa (0) | •• | 1 | 1 (0.6) | 1 | 1 (0.8) | •• |
| Cook Islands (6) | 1 | 10 | 10 (5.9) | 7 | 7 (5.5) | 1 |
| Federated States of Micronesia (7) | •• | 2 | 2 (1.2) | 2 | 2 (1.6) | •• |
| Fiji (26) | 5 | 29 | 37 (21.7) | 21 | 25 (19.7) | 37 |
| Kiribati (7) | 1 | 8 | 8 (4.7) | 3 | 3 (2.4) | •• |
| Marshall Islands (4) | •• | 24 | 24 (14.1) | 15 | 15 (11.8) | •• |
| Nauru (2) | •• | 1 | 1 (0.6) | 1 | 1 (0.8) | •• |
| Niue (2) | •• | 3 | 3 (1.8) | 1 | 1 (0.8) | •• |
| Palau (2) | •• | 4 | 4 (2.3) | 4 | 4 (3.1) | •• |
| Papua New Guinea (14) | •• | 23 | 26 (15.3) | 18 | 18 (14.2) | 3 |
| Samoa (4) | 3 | 9 | 11 (6.5) | 17 | 19 (14.9) | 2 |
| Solomon Islands (14) | 2 | 15 | 16 (9.4) | 8 | 9 (7.1) | 2 |
| Timor-Leste (1) | •• | 2 | 2 (1.2) | 3 | 3 (2.4) | 1 |
| Tokelau (1) | •• | 1 | 1 (0.6) | 1 | 1 (0.8) | •• |
| Tonga (6) | 2 | 8 | 9 (5.3) | 4 | 5 (3.9) | 1 |
| Tuvalu (5) | •• | 3 | 5 (2.9) | 4 | 6 (4.7) | 1 |
| Vanuatu (11) | 1 | 9 | 10 (5.9) | 7 | 7 (5.5) | 2 |
| Role | Total 15 | Total 153 | Total 171 | Total 117 | Total 127 | Total 50 |
| Doctor | 7 | 111 | 123 (71.9) | 80 | 88 (69.3) | 32 |
| Nurse | 5 | 20 | 25 (14.6) | 18 | 20 (15.7) | 17 |
| Hospital administrator | •• | 1 | 1 (0.6) | 3 | 3 (2.4) | •• |
| Medical superintendent | 1 | 7 | 7 (4.1) | 3 | 3 (2.4) | •• |
| Director of nursing | 1 | 6 | 7 (4.1) | 5 | 5 (3.9) | •• |
| Ministry of Health staff | •• | 3 | 3 (1.7) | 1 | 1 (0.8) | •• |
| Pre-Hospital | •• | 2 | 2 (1.2) | 6 | 6 (4.7) | •• |
| Allied Health | •• | 2 | 2 (1.2) | 1 | 1 (0.8) | •• |
| Academic | 1 | 1 | 1 (0.6) | 0 | 0 (0.0) | 1 |
| Facility-type | Total 150 | Total 168 | Total 117 | Total 128 | ||
| National referral hospital | •• | 92 | 100 (59.5) | 68 | 76 (59.4) | •• |
| Provincial / Divisional hospital | •• | 30 | 40 (23.8) | 20 | 21 (16.4) | •• |
| District / Sub-divisional hospital | •• | 7 | 7 (4.2) | 9 | 10 (7.8) | •• |
| Small health facility / Health Centre / Private facility | •• | 17 | 17 (10.1) | 12 | 13 (10.2) | •• |
| Nursing station | •• | 1 | 1 (0.6) | 0 | 0 (0.0) | •• |
| Pre-Hospital service | •• | 1 | 1 (0.6) | 6 | 6 (4.7) | •• |
| Non-Clinical (office, university, Ministry of Health) | •• | 2 | 2 (1.2) | 2 | 2 (1.5) | •• |
For both facility-based and pre-hospital EC, participants ranked the Human Resources and Training building block, followed by; Infrastructure and Equipment; Leadership and Governance; Processes, and lastly Data as the overall order of priority for EC systems development activities in the Pacific region. At the final workshop, participants agreed to review all consensus priorities and standards after five years.
Facility
Current status
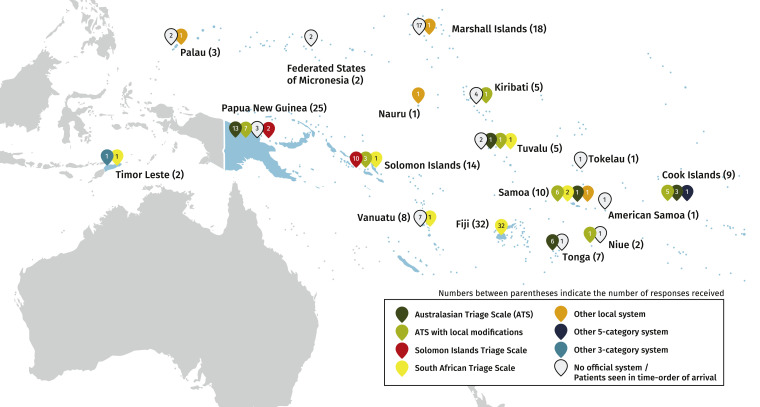
Across the Pacific, participants report a low level of training for EC, limited areas and incomplete equipment for care provision, complicated by care delivery in overcrowded and unsafe areas. Table 2 provides details of regional responses to questions about the capacity and function at EC facilities according to each building block. Participants report inconsistent triage and multiple triage systems in use around the region, with some countries using up to four different systems. Fig. 4 depicts a regional map illustrating the triage systems currently used in each PICT with the response numbers from each country included. Use of standardised clinical guidelines and collection of useful EC data is inconsistent across the region.
Table 2.
Continued
 |
Table 2.
Status of facility-based EC building block components across the Pacific region.
 |
Fig. 4.
Map of triage systems in use across the Pacific region.
Leadership and Governance was explored through the lens of disaster planning integrated with EC, and recognition and prioritisation of EC at the national level. Only 15 (10•1%) participants reported that EC staff were involved in planning, training and surge response drills for disasters at all hospital levels, integrated with local and national plans. One hundred (68•0%) participants reported that EC was either not a priority in their country or no action had been taken to plan for EC development.
Table 3 illustrates how each PICT is rated across each of the EC building block components according to the consensus standard determined by the PICT stakeholders.
Table 3.
Comparison of facility-based EC between PICTs across the region.
 |
Development priorities
We present the agreed priority inputs and functions per building block for regional facility-based EC development in Table 4, divided in to immediate and longer-term priorities. Training staff, providing essential equipment and standardising triage and clinical guidelines are building block components that neared or exceeded the 70% benchmark for urgent action and were adopted unequivocally by consensus. Although not initially reaching the benchmark, workshop participants agreed through discussion to adopt highly ranked components incorporating clinical leadership, government recognition and information systems for basic data collection as immediate priority actions.
Table 4.
Priority inputs and functions for facility-based and pre-hospital EC systems development.
 |
Consensus standards
Minimum Pacific regional standards for facility-based EC are presented by building block in Table 5. Ten of the 24 standards generated pertain to Human Resources and Training. Training standards were amended during workshop discussion to be more proscriptive (eg. ‘at least two doctors’ and ‘at least one nurse per shift’ with specialised EC training) yet allow for the substantial variation between PICT populations and resources. Specific EC short course training standards differed for providers working at the national hospital from those working in provincial or district level facilities. Infrastructure and Equipment standards regarding space, equipment and medications for resuscitation met the 70% benchmark and were adopted, along with a fourth standard concerning regional ED design guidelines that was approved after discussion. All Leadership and Governance standards exceeded the benchmark and were strongly endorsed by the workshop participants. The Process standard regarding consistent use of a recognised triage system exceeded the benchmark, along with amended standards to enable specific adaptation and use of clinical guidelines within each PICT context. Data standards that enshrined collection of core EC information, including triage category, reached or approximated the benchmark and were adopted through consensus.
Table 5.
Pacific regional minimum standards for facility-based emergency care (EC).
 |
Through free comments in the survey and key discussion items during the workshops, participants clarified that the consensus outcomes should apply to both public and private facilities in PICTs, and that flexibility to adapt all EC components to the local context was inherent in the priorities and standards generated.
Pre-Hospital
Current status
Table 6 provides details of responses exploring the level of EC currently available across the Pacific at the scene of illness or injury, and during transport of the patient to or between facilities. Very few respondents reported access to trained first responder care and expert advice in most parts of their country. Most commonly, participants reported a limited and unreliable transport system providing basic EC care, and less than 5% reported an overall pre-hospital system with high quality and reliable care in most parts of their country.
Table 6.
Status of pre-hospital EC across the Pacific region.
| Number | Percentage% | |
|---|---|---|
| System for access to EC and first aid from trained first responders | Total 122 | |
| No system exists | 17 | 13.9 |
| Some groups are trained in first aid, but without any standard training or coordination | 25 | 20.5 |
| There are some formally trained first responders but no system for the public to access them | 36 | 29.5 |
| There are organised, trained first responder services that the public can access in some parts of the country | 33 | 27.1 |
| There is access to trained first responder care and advice from the ambulance / central facility service in most parts of the country | 11 | 9.0 |
| System to provide EC during transport between scene and facility, or between facilities | Total 122 | |
| No system exists | 17 | 13.9 |
| A transport system exists but access to it is limited and unreliable | 16 | 13.1 |
| A transport system with basic emergency care provision exists but access is limited and unreliable | 49 | 40.2 |
| A transport system exists and access is reliable in most parts of the country, but providers do not provide emergency care during transport | 20 | 16.4 |
| A transport system exists and access to transport and emergency care during transport is reliable in most parts of the country | 20 | 16.4 |
| System to access EC from trained first responders and the scene and urgent transport to a health facility (overall system of pre-hospital care) | Total 121 | |
| No system exists | 23 | 19.0 |
| Some parts of the system exist but access to care in not reliable | 35 | 28.9 |
| Most parts of the system exist, but access to care is not reliable in all parts of the country | 34 | 28.1 |
| Most parts of the system exist and access to care is reliable in most parts of the country, but not of high quality | 24 | 19.9 |
| Most parts of the system exist and access to care is reliable and of high quality in most parts of the country | 5 | 4.1 |
Table 7 illustrates whether each PICT meets an acceptable standard for pre-hospital care (care at scene, during transport and overall system development).
Table 7.
Comparison of pre-hospital EC between PICTs across the region.
 |
Development priorities
Table 4 also provides the immediate and longer-term priority inputs and functions for pre-hospital EC systems development. Overall, there are very few longer-term priorities for pre-hospital EC. Workshop participants agreed that all components of provider training required immediate priority status, despite none of them reaching the initial 70% benchmark. After discussion, immediate priority actions were also adopted supporting government leadership, protective legislation, medical oversight and basic data collection. All three of the priority areas for Infrastructure and Equipment met or exceeded the 70% survey benchmark, as with all Process priority actions covering communication, clinical guidelines and standard procedures during disaster events.
Consensus standards
Table 8 presents the 22 minimum standards for Pacific regional pre-hospital EC. All Human Resources and Training standards were adopted after discussion. Basic life support and trauma care training for pre-hospital providers were highly endorsed, along with equipment and safety standards for ambulances and Process components covering clinical and operational protocols to standardise care. Workshop participants made minor amendments to incorporate non-road transport and adaption of guidelines for PICT context. Data standards regarding logging and recording of clinical cases reached 70% survey agreement and were adopted. Participants strongly endorsed all Leadership and Governance standards, which included government and clinical leadership, practice certification and protective and safety legislation.
Table 8.
Pacific regional minimum standards for pre-hospital emergency care (EC).
 |
During the workshop and in free-text survey responses, participants emphasised the importance of pre-hospital EC coordinating with other services during disasters and surge events, according to the specific context within each PICT.
Discussion
We present the first Pacific-wide description of EC status, development priorities and regional standards structured within a health systems framework. Overwhelmingly, the Human Resources and Training building block received the highest priority rating and number of regional standards to achieve across both facility-based and pre-hospital EC. This reflects important current workforce gaps highlighted by limited formal post-graduate training for EC and lack of permanent staff in EC facilities, which hinders health worker performance through lack of skill, knowledge and motivation. [32] Pacific stakeholders emphasised the importance of building and nurturing staff capacity; in the regional context where populations are isolated or small, higher education opportunities can be restricted, and professional development may be limited. PICT participants clearly desire standardised and certified EC training for providers at the pre-hospital, district and national hospital level and have articulated the types of skills required at each level by identifying particular short course requirements. Short courses (typically 2–3 days) may not lead to sustained skill and knowledge retention and have uncertain impacts on patient outcomes, [33] but by specifying standards for the region, PICTs now have a clear framework for ensuring donor-driven teaching activities conform to the needs and requirements of local clinicians and are consistent across the region.
At the national hospital level, every PICT should have doctors and nurses with specialist post-graduate training in EC. This standard presents challenges to many PICTs because training is costly and limited to few sites, thereby necessitating clinicians to study away from home for years at a time. A supportive model that enables PICTs to continue clinical service provision through regional provider accreditation enabling workforce mobility is desirable, [34] but requires recognition of EC as an essential speciality discipline and substantial commitment by national governments. Aspiring to prevent known burnout risks for sole clinician leaders (a common issue in the Pacific region), [35] PICT stakeholders deliberately specified minimum numbers, recognition and protection of trained staff through employment structures, career pathways and safe working hours.
Many facilities where EC is delivered are not fit for purpose. Most participants reported a resuscitation area at their national hospital, but areas for other essential components of EC, such as triage, assessment, intervention and monitoring were often lacking. Some PICTs meet an acceptable standard for EC equipment, which may reflect a popular focus on tangible products as a symbol of EC investment, but can also perpetuate a common myth that EC is expensive and requires high technology. [36] Cardiac monitors and defibrillators are rarely found outside of the national hospital (82% of responses), despite rapidly increasing non-communicable disease across the region. [20] The inability to correctly diagnose and rapidly intervene in acute myocardial infarction or serious dysrhythmia can result in preventable loss of life.
Many of the Infrastructure and Equipment building block standards require further collaborative work to articulate the core ED design, equipment and medication features that can apply to all PICTs. External donors to the Pacific commonly provide large infrastructure items, such as hospitals and ambulances, and design these for models of care not practiced in the region. By creating Pacific guidelines that outline core layout, spatial, functional and equipment requirements of EDs, resuscitation rooms and ambulances, PICT EC stakeholders can ensure that new infrastructure acquisitions meet their needs, are consistent across the region, and fit yet adaptable for local context purpose.
ED overcrowding is a global, hospital-wide problem that adversely affects patient outcomes and increases mortality. [37] Considering resource limitations in PICTs, we agreed on a 12-hour benchmark as the acceptable maximum time a patient should spend in the ED between arrival and disposition. Several PICTs reported serious overcrowding and care delivery in unsafe areas, likely because of poor infrastructure, limited human resources, high burden of EC disease and immature processes such as triage and patient flow management. Daily ED overcrowding is likely to negatively impact patient experience and care outcome, and has substantial implications for the ability of hospitals to safely manage an influx of patients during surge events such as the current COVID-19 pandemic. [38]
We elevated the importance of Processes as a key manifestation of service delivery in EC by defining this as an EC system building block. PICT stakeholders endorsed this approach by consistently rating proposed Process priorities and standards highly across pre-hospital and facility-based data collection. Triage systems are used inconsistently in the region, with multiple system use likely reflecting lack of consensus within a country. Mapping enables patterns to emerge, including the general lack of recognised triage system use in the northern Pacific, spread of the LMIC-context South African Triage Scale out from Fiji and adoption of the Solomon Islands Triage Scale [39] in PNG. Triage systems now should be recognised and standardised at all facilities across PICTs and incorporated in to ED infrastructure priorities.
Most EC stakeholders reported using a standardised resuscitation guideline at their national hospital, but agreed that further guideline development with widespread and consistent implementation was a priority. Examples of evidence-based, context appropriate clinical guidelines to improve EC exist for trauma care in Fiji [40] and acute asthma in PNG, [41] as well as a framework for developing and sharing locally adapted clinical EC guidelines. [42] The need for pre-hospital clinical practice guidelines is highlighted in Timor-Leste, [43] as one component of many essential Process priorities and standards required to build an effective pre-hospital system.
Data received less attention as a priority building block in this study, perhaps reflecting the high proportion of clinician participants who are often consumed with service delivery at the expense of clinical audit and research. The burden of EC disease in the Pacific region is largely unknown, and data collection extremely limited. Achieving standards for computer-based collection of basic demographic and clinical information will enable PICT leaders to understand the acute health needs of their populations and better plan for universal access to safe and effective care. PICT stakeholders nominated ‘Presenting Complaint’ as a feasible descriptor of EC disease, but a globally or regionally accepted lexicon that would enable consistent data collection and comparison between PICTs is difficult to obtain, [44] yet highly desirable.
Pre-hospital EC is profoundly underdeveloped across the entire Pacific region, with none of the 17 PICTs surveyed reporting an adequate level of pre-hospital system development in their countries. Based on our pre-existing knowledge, we chose not to use the building block framework to gather data on pre-hospital capacity; instead focusing on three core functional components (care at scene, during transfer, and overall system). Rather than document overwhelming deficit, the consensus priorities and standards now outline how a pre-hospital system may be built in the Pacific region across all building block components.
Recognition of EC as a speciality discipline and critical component of the health care system is an urgent Leadership and Governance priority and a standard for all PICTs to meet. Currently EC is not a priority in most countries and not well integrated with disaster planning, yet central to an effective health system response as highlighted by the recent COVID-19 pandemic. As predominantly clinicians, our PICT stakeholders understood the pivotal influence of government support underpinning all other building block components; particularly staff support, quality and safety oversight and surge response integration at both facility and pre-hospital levels. In entirety, these priorities and standards provide PICT leaders with a roadmap for comprehensive and consistent EC systems development across the region, including measurable indicators for progress evaluation over time. This work also provides a Pacific EC research agenda, and critical advocacy tools to inspire individual PICT and regional government action.
Our model of iterative consultation, extensive engagement and intellectual collaboration illustrates a respectful research approach recommended for the Pacific, [45] and addresses a call for regional partnership to meet the WHA Resolution 72.16. [46] Regional facility and service mapping exercises can shed some light on access to EC, [47] but often over-estimate capacity to deliver care if detailed functional assessments are not available. [48] Our approach attempts to both map availability and describe some functional capacity across the Pacific region, therefore enabling identification of gaps in core components of effective EC service delivery. With deliberate engagement of Pacific EC clinical leaders, we have generated practical outcomes of integrity, that can be implemented through local ownership. Unmeasured project benefits include improved regional cooperation and unanimity towards the establishment of a Pacific regional society for EC.
Because of resource differences, we did not include EC stakeholders from all 22 PICTs, thereby limiting total regional applicability of our consensus data and confining it to the English-speaking Pacific. Furthermore, participants were unequally represented by role, facility or country, and heavily weighted towards clinicians who may be unaware of national health priorities and policy planning within their countries, yet are at the frontline of EC provision. Engaging participants through personal relationships and professional networks around the region resulted in extremely high participation rates that are unlikely to have occurred with probability sampling methods. While this may compromise the robustness of the numerical estimates, it should not undermine the validity of the conclusions drawn around EC system components in the Pacific. Not every PICT that responded to the surveys was represented in the final consensus workshop, thereby risking bias in agreed priorities and standards. Workshop participants were cognisant of their regional roles in representing EC stakeholders from the large (PNG), small island (Tuvalu), middle income (Fiji) and least developed (Solomon Islands) PICTs, and contributed to the consensus outcomes accordingly.
In order to provide universal health coverage, EC systems must be prioritised in the global health agenda. [2] The Pacific region urgently requires robust EC systems to respond to routine, climatic and disease outbreak health emergencies, yet substantial gaps in functional capacity exist in most PICTs within all of the building blocks of facility-based and pre-hospital EC. For the first time, PICT EC stakeholders have collaborated regionally to document current status, and produce priority actions and minimum standards for EC development that conform to a globally recognised health systems framework. These consensus outcomes provide both individual PICT and regional health leaders with a key resource to commence the critical work towards improving EC for all peoples of the Pacific.
Contributors
GP conducted both project workshops, conceived, developed and disseminated the surveys, performed all data analyses and interpretation, wrote the manuscript and was the overall project lead. AC assisted with survey development, Fiji workshop facilitation and data analysis and interpretation. PT and PAE provided survey and workshop input, recruited participants and provided expert advice and support throughout the project. BK conceived the project, assisted with data interpretation and provided expert advice and logistic support throughout the project. GOR and PC provided scientific oversight to the project. All authors had access to the data, reviewed the manuscript for critical content and approved the paper for publication.
Declaration of Competing Interest
GP and AC report personal fees and non-financial support, and PAE and PT report non-financial support from The Pacific Community (SPC) Clinical Services Program, during the conduct of the study. GP and AC are visiting emergency medicine specialists at the Fiji National University. GP is also a visiting emergency medicine specialist at the University of Papua New Guinea and is a Trustee of the Primary Trauma Care (PTC) Foundation, a non-profit, non-government UK charity that oversees global PTC courses. All other authors declare no other competing interests.
Acknowledgements
We would like to thank the Australasian College for Emergence Medicine who assisted with graphics associated with this project. Graduates of the University of Papua New Guinea and Fiji National Universityemergency medicine programs and all participants who consented to be identified are acknowledged by name in Appendix pp 36–39.
Footnotes
Editor note: The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanwpc.2020.100002.
Appendix. Supplementary materials
References
- 1.Kobusingye O.C., Hyder A.A., Bishai D., Hicks E.R., Mock C., Joshipura M. Emergency medical systems in low-and middle-income countries: recommendations for action. Bull World Health Organ. 2005;83:626–631. [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Assembly. Resolution 72.16. Emergency care systems for universal health coverage: ensuring timely care for the acutely ill and injured. Geneva: world Health Organisation, 2019. https://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_R16-en.pdf?ua=1 (Accessed 3 April 2020).
- 3.Shanahan T., Risko N., Razzak J., Bhutta Z. Aligning emergency care with global health priorities. Int J Emerg Med. 2018;11:52. doi: 10.1186/s12245-018-0213-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson P., Petrino R., Halpern P., Tintinalli J. The globalization of emergency medicine and its importance for public health. Bull World Health Organ. 2006;84:835–839. doi: 10.2471/blt.05.028548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burkholder T.W., Hill K., Hynes E.J.C. Developing emergency care systems: a human rights-based approach. Bull World Health Organ. 2019;97:612–619. doi: 10.2471/BLT.18.226605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reynolds T.A., Sawe H., Rubiano A.M., Shin S.D., Wallis L., Mock C.N. Strengthening health systems to provide emergency care. In: Jamison D, Gelband H, Horton S, editors. 3rd edition. Vol. 9. The World Bank; Washington DC: 2017. pp. 247–265. (Disease control priorities). Improving Health and Reducing Poverty. [PubMed] [Google Scholar]
- 7.Spina S., Marrazzo F., Migliari M., Stucchi R., Sforza A., Fumagalli R. The response of Milan's emergency medical system to the COVID-19 outbreak in Italy. Lancet. 2020;395:e49–e50. doi: 10.1016/S0140-6736(20)30493-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baker T., Schell C.O., Petersen D.B. Essential care of critical illness must not be forgotten in the COVID-19 pandemic. Lancet. 2020;395:1253–1254. doi: 10.1016/S0140-6736(20)30793-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organisation. Emergency Care Systems Framework2019. https://www.who.int/emergencycare/emergencycare_infographic/en/ (Accessed 20 March 2020).
- 10.World Health Organisaton. Health systems. Everybody's business: strengthening health systems to improve health outcome. WHO's framework for action: world Health Organisation; 2007. https://www.who.int/healthsystems/strategy/en/ (Accessed 20 March 2020).
- 11.Chang C.Y., Abujaber S., Reynolds T.A., Camargo C.A., Obermeyer Z. Burden of emergency conditions and emergency care usage: new estimates from 40 countries. Emerg Med J. 2016;33:794–800. doi: 10.1136/emermed-2016-205709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Obermeyer Z., Abujaber S., Makar M. Emergency care in 59 low-and middle-income countries: a systematic review. Bull World Health Organ. 2015;93:577–586. doi: 10.2471/BLT.14.148338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thind A., Hsia R., Mabweijano J., Romero Hicks E., Zakariah A., Mock C. Prehospital and emergency care. In: Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN, editors. 3rd edition. Vol. 1. The World Bank; Washington DC: 2015. pp. 245–262. (Essential surgery). [Google Scholar]
- 14.Razzak J., Farooq Usmani M., Bhutta Z.A. Global, regional and national burden of emergency medical diseases using specific emergency disease indicators: analysis of the 2015 global burden of disease study. BMJ Glob Health. 2019;4 doi: 10.1136/bmjgh-2018-000733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hodkinson P.W., Wallis L.A. Emergency medicine in the developing world: a Delphi study. Acad Emerg Med. 2010;17:765–774. doi: 10.1111/j.1553-2712.2010.00791.x. [DOI] [PubMed] [Google Scholar]
- 16.Calvello E.J., Tenner A.G., Broccoli M.C. Operationalising emergency care delivery in sub-Saharan Africa: consensus-based recommendations for healthcare facilities. Emerg Med J. 2016;33:573–580. doi: 10.1136/emermed-2015-204994. [DOI] [PubMed] [Google Scholar]
- 17.Mehmood A., Rowther A.A., Kobusingye O., Hyder A.A. Assessment of pre-hospital emergency medical services in low-income settings using a health systems approach. Int J Emerg Med. 2018;11:53. doi: 10.1186/s12245-018-0207-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mounier-Jack S., Griffiths U.K., Closser S., Burchett H., Marchal B. Measuring the health systems impact of disease control programmes: a critical reflection on the WHO building blocks framework. BMC Public Health. 2014;14:278. doi: 10.1186/1471-2458-14-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pacific Islands Forum Leaders. The framework for Pacific regionalism. Pacific Islands forum secretariat; Suva, Fiji: 2014. https://www.forumsec.org/wp-content/uploads/2017/09/Framework-for-Pacific-Regionalism.pdf (Accessed 13 March 2020).
- 20.Tuitama L.T., Young-soo S., Clark H., Tukuitonga C., Beaglehole R. Acting on the Pacific crisis in non-communicable diseases. Lancet. 2014;384:1823–1824. doi: 10.1016/S0140-6736(14)61824-9. [DOI] [PubMed] [Google Scholar]
- 21.Editorial Saving the Pacific islands from extinction. Lancet. 2019;394:359. doi: 10.1016/S0140-6736(19)31722-2. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization; Geneva: 2019. World health statistics 2019: monitoring health for the SDGs, sustainable development goals.https://www.who.int/gho/publications/world_health_statistics/2019/en/ [Google Scholar]
- 23.Institute for health metrics and evaluation (IHME). Country profiles. Seattle, WA: IHME, University of Washington, 2018. http://www.healthdata.org/results/country-profiles (Accessed 22 June 2020).
- 24.Piukala S., Clark H., Tukuitonga C., Vivili P., Beaglehole R. Turning the tide on non-communicable diseases in the Pacific region. Lancet Glob Health. 2016;4:e899–e900. doi: 10.1016/S2214-109X(16)30205-4. [DOI] [PubMed] [Google Scholar]
- 25.Guest G.D., McLeod E., Perry W.R. Collecting data for global surgical indicators: a collaborative approach in the Pacific Region. BMJ Glob Health. 2017;2 doi: 10.1136/bmjgh-2017-000376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davies M., Sutherland-Fraser S., Hazelman Taoi M., Williams C. Developing standards in Pacific Island countries: the Pacific perioperative practice bundle. ACORN J. 2016;29:42–47. [Google Scholar]
- 27.Broccoli M.C., Moresky R., Dixon J. Defining quality indicators for emergency care delivery: findings of an expert consensus process by emergency care practitioners in Africa. BMJ Glob Health. 2018;3 doi: 10.1136/bmjgh-2017-000479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bushe G. Appreciative inquiry. Theory and critique. In: Boje D, Burnes B, Hassard J, editors. The Routledge companion to organizational change. Routledge; 1st ed. London, UK: 2012. pp. 87–103. [DOI] [Google Scholar]
- 29.Sartorius R.H. The logical framework approach to project design and management. Eval Pract. 1991;12:139–147. [Google Scholar]
- 30.Moresky R.T., Razzak J., Reynolds T. Advancing research on emergency care systems in low-income and middle-income countries: ensuring high-quality care delivery systems. BMJ Glob Health. 2019;4 doi: 10.1136/bmjgh-2018-001265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Secretariat of the Pacific community. http://www.spc.int/ (Accessed 13 March 2020).
- 32.Rowe A.K., Rowe S.Y., Peters D.H., Holloway K.A., Chalker J., Ross-Degnan D. Effectiveness of strategies to improve health-care provider practices in low-income and middle-income countries: a systematic review. Lancet Glob Health. 2018;6:e1163–e1e75. doi: 10.1016/S2214-109X(18)30398-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meaney P.A., Topjian A.A., Chandler H.K. Resuscitation training in developing countries: a systematic review. Resuscitation. 2010;81:1462–1472. doi: 10.1016/j.resuscitation.2010.06.024. [DOI] [PubMed] [Google Scholar]
- 34.McKimm J., Newton P.M., de Silva A. Accreditation of healthcare professionals’ education in Pacific Island Countries: evidence and options. UNSW Human Res Health Knowl Hub. 2013 https://sphcm.med.unsw.edu.au/sites/default/files/sphcm/Centres_and_Units/SI_Accreditation_Report.pdf [Google Scholar]
- 35.Phillips G., Lee D., Shailin S., O'Reilly G., Cameron P. The Pacific emergency medicine mentoring program: a model for medical mentoring in the Pacific region. Emerg Med Australas. 2019;31:1092–1100. doi: 10.1111/1742-6723.13366. [DOI] [PubMed] [Google Scholar]
- 36.Hirshon J.M., Risko N., Calvello E.J. Health systems and services: the role of acute care. Bull World Health Organ. 2013;91:386–388. doi: 10.2471/BLT.12.112664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Richardson D.B. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust. 2006;184:213–216. doi: 10.5694/j.1326-5377.2006.tb00204.x. [DOI] [PubMed] [Google Scholar]
- 38.Phillips G., Cox M.COVID-19 and emergency care in the Pacific. Canberra, Australia: development policy centre, Australian National University. 2020https://devpolicy.org/covid-19-and-emergency-care-in-the-pacific-20200428/ (Accessed 7 May 2020).
- 39.Wanefalea L.E., Mitchell R., Sale T., Sanau E., Phillips G.A. Effective triage in the Pacific region: the development and implementation of the Solomon Islands Triage Scale. Emerg Med Australas. 2019;31:451–458. doi: 10.1111/1742-6723.13248. [DOI] [PubMed] [Google Scholar]
- 40.Raj L.K., Creaton A., Phillips G. Improving emergency department trauma care in Fiji: implementing and assessing the trauma call system. Emerg Med Australas. 2019;31:654–658. doi: 10.1111/1742-6723.13225. [DOI] [PubMed] [Google Scholar]
- 41.Heath R., Tomaszewski P., Kuri M., Atua V., Phillips G. Message in a bottle: how evidence-based medicine and a programme change model improved asthma management in a low-income emergency department in Papua New Guinea. Emerg Med Australas. 2019;31:97–104. doi: 10.1111/1742-6723.13212. [DOI] [PubMed] [Google Scholar]
- 42.Therapuetic Guidelines Foundation, Australia. Fiji and Solomon Islands Guideline Host Apps. 2019. https://tgfl.org.au/news/new-guidelines-fiji-solomon-islands-apps-february-2019/ (Accessed 3 April 2020).
- 43.Moores J., de Jesus G.A. Management of post-partum haemorrhage in the Timor Leste national ambulance service. Emerg Med Australas. 2018;30:814–819. doi: 10.1111/1742-6723.13153. [DOI] [PubMed] [Google Scholar]
- 44.Rice B.T., Bisanzo M., Maling S., Joseph R., Mowafi H., Global Emergency Care Investigators Group Derivation and validation of a chief complaint shortlist for unscheduled acute and emergency care in Uganda. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2017-020188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ekeroma A. Collaboration as a tool for building research capacity in the Pacific Islands. Ann Hum Biol. 2018;45:295–296. doi: 10.1080/03014460.2018.1454510. [DOI] [PubMed] [Google Scholar]
- 46.Mitchell R., Phillips G., O'Reilly G., Creaton A., Cameron P. World health assembly resolution 72.16: what are the implications for the Australasian College for Emergency Medicine and emergency care development in the Indo-Pacific? Emerg Med Australas. 2019;31:696–699. doi: 10.1111/1742-6723.13373. [DOI] [PubMed] [Google Scholar]
- 47.Ouma P.O., Maina J., Thuranira P.N. Access to emergency hospital care provided by the public sector in sub-Saharan Africa in 2015: a geocoded inventory and spatial analysis. Lancet Glob Health. 2018;6:e342–ee50. doi: 10.1016/S2214-109X(17)30488-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Geduld H., Hynes E.J.C., Wallis L.A., Reynolds T. Hospital proximity does not guarantee access to emergency care. Lancet Glob Health. 2018;6:e731. doi: 10.1016/S2214-109X(18)30235-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.