Abstract
Clinical presentation of patients with foreign bodies is highly variable. We received a 55-year-old female patient with fever and right flank pain. She was treated previously for kidney stones by percutaneous nephrolithtomy with partial resolution, requiring renal embolization during this procedure because of bleeding. CT evidenced metallic density images localized in kidney and ureter, associated with kidney stones located in lower calix. Semirigid ureteroscopy and retrograde intrarenal surgery were performed, revealing the presence of foreign bodies in both localizations and lower calix stones. Complete removal of foreign bodies and stones was performed. Foreign bodies were found to be embolization coils applied in the previous procedure.
Keywords: renal stone, ureteroscopy, urolithiasis, foreign bodies, retrograde intrarenal surgery
Introduction and Background
The presence of foreign bodies in the proximal urinary tract is a rare pathology.1–3 One of the most severe complications after a percutaneous nephrolithotomy is bleeding, generally treated using hemodynamic procedures. Coils used during renal embolization can migrate to the urinary tract, causing the presence of urinary foreign bodies.2 Urinary tract obstruction, stone nucleation, and infections are the major problems reported regarding foreign bodies.1
The objective of this communication is to report a case of simultaneous ureteral and renal foreign bodies.
Case Report
A female patient, 55 years old, was admitted to our center with fever and right flank pain.
She had a history of kidney stones and a percutaneous nephrolithotomy performed 6 months previous to this consultation, in another institution. During this procedure, embolization procedure was needed because of severe renal bleeding.
Kidney, ureter, and bladder X-ray showed stones located in the right kidney and metallic images in the urinary tract. CT reported mild hydronephrosis, a 15-mm stone in right renal lower calix, a stone in mid right ureter, and a linear metallic foreign body in both localizations (Figs. 1 and 2).
FIG. 1.

CT scan showing metallic foreign body in right renal lower calix.
FIG. 2.
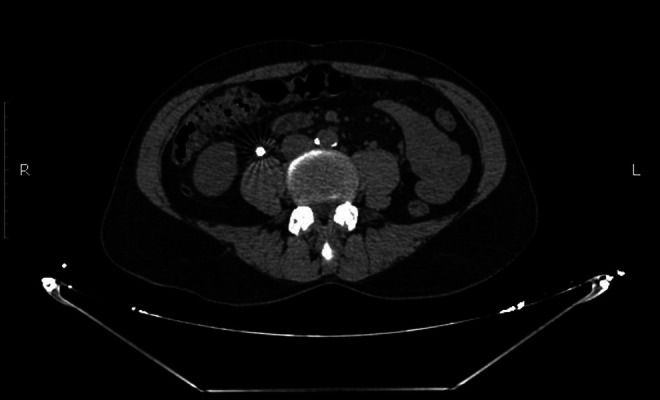
CT scan showing metallic foreign body in right proximal ureter.
Urine culture performed 1 week before was negative and laboratory tests showed normal parameters.
A retrograde intrarenal surgery (RIRS) was performed. The patient was placed in lithotomy position. Cystoscopy was performed using a 20F cystoscope (Karl Storz-Endoskope®, Tuttlingen, Germany); retrograde pyelography with fluoroscopic guidance confirmed the presence metallic bodies in proximal ureter and renal lower calix. A 0.035" hydrophilic guide (Cook Medical®, Bloomington, IN) was located.
Semirigid ureteroscopy was conducted using 7.5F–9F ureteroscope (Karl Storz-Endoskope) and using a second hydrophilic 0.035" guide (Cook Medical), with no evidence of ureteral stenosis. Ureteral stone and foreign body were reached and extracted using Holmium Laser Fibers OptiLite™ and Odyssey 30 Holmium Laser System™ (Cook Medical) and NGage Nitinol Stone Extractor (Cook Medical).
After this, RIRS was performed with a flexible ureteroscope Flex X2 (Karl Storz-Endoskope) of 7.5F diameter using a 12F ureteral sheath (Cook Medical). Access to the upper urinary tract was achieved without drawbacks and lithotripsy with laser was performed. Fragments were extracted with NCircle® Delta Wire® Nitinol Tipless Stone Extractor device (Cook Medical). Renal foreign body was also found and extracted using NGage Nitinol Stone Extractor (Cook Medical) (Fig. 3). Complete absence of residual stones and foreign bodies was confirmed by endoscopic vision and fluoroscopy.
FIG. 3.

Foreign bodies and stones extracted.
The procedure was completed with the placement of Double J ureteral catheter 6F-26 cm (Cook Medical).
A week after the procedure, Double J stent was removed without complications.
Discussion and Literature Review
One of the most feared problems after a percutaneous nephrolithotomy is bleeding, with an estimated rate of 2%–20%.4,5 Pseudoaneurysms of distal branches of the renal artery is a well-known complication, and has a reported incidence of 0.36%–1.0%.2,4,6 Therapeutic angiography performed with stainless steel or titanium coils has evolved as the treatment of choice with success rates that exceed 90%.4,7,8 The aim is to achieve a super selective embolization of the injured vessel.4,9
Complications may occur during transarterial embolization as well as in the immediate perioperative period, as postembolization syndrome, renal insufficiency, embolization of nontarget organs, infective complications, and migration of embolization coils may appear.4,10 Migration of coils and encrustation with renal calculi are compatible with reports of migrated coils acting as the nidus for stone formation.4,9,11 Physiopathology of this phenomenon is related to the mechanism of arteriovenous fistula formation; this is linked to the forceful dilation of the calix, with consequent division of the caliceal wall, exposing the underlying vessels. After coil embolization, healing of the caliceal wall over the coils can result in focal areas of weakness through which the coil can migrate into the urinary collecting system.8
This migration of embolization coils has been reported to occur in <2% of all cases.12 Migrated coils can get encrusted and act as nidus for the stone formation, leading to obstruction, infection, or may mimic a renal neoplasm. Its clinical presentation may be as a typical renal colic with or without gross hematuria. Urinary tract infection is usually caused by urea-splitting organisms, which lead to the formation of struvite stones.4,11,13
For this reason, these objects should be removed from the kidney to establish a definitive treatment, especially if symptomatic1,13; stone disintegration and removal can be combined with removal of the stone-inducing foreign body if it is possible.10
Methods for extraction of such foreign bodies depend on the anatomical location, size, shape, and mobility of the object. Surgical approach for such foreign bodies can be open, or endourologic, anterograde, or retrograde.13 In our case, complete extraction of stones and ureteral and renal foreign bodies was performed using ureteroscopy and RIRS.
Conclusion
Foreign bodies in urinary tract can appear after renal embolization. RIRS may be an adequate procedure to treat this complication.
Abbreviations Used
- CT
computed tomography
- RIRS
retrograde intrarenal surgery
Disclosure Statement
No competing financial interests exist.
Cite this article as: Lopez Silva M, Sanguinetti H, Battiston S, Alvarez P, Bernardo N (2019) Simultaneous ureteral and renal foreign bodies, Journal of Endourology Case Reports 5:1, 1–3, DOI: 10.1089/cren.2017.0039.
References
- 1. Sener TE, Jonathan Cloutier J, Audouin M, et al. A guidewire introducer as a ureteral foreign body: A case report. Can Urol Assoc J 2015;9:E384–E386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chen WC, Wang SC, Chen SL, et al. Foreign body in the ureter: A particle of glue after transarterial embolization of a renal pseudoaneurysm during percutaneous nephrostomy. J Chin Med Assoc 2012;75:183–186 [DOI] [PubMed] [Google Scholar]
- 3. Restrepo N, Belis J. Ureteral foreign body after laser lithotripsy. J Endourol 1994;8:29–31 [DOI] [PubMed] [Google Scholar]
- 4. Kumar S, Jayant K, Singh SK, et al. Delayed migration of embolized coil with large renal stone formation: A rare presentation. Case Rep Urol 2014;2014:687965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Un S, Cakir V, Kara C, et al. Risk factors for hemorrhage requiring embolization after percutaneous nephrolithotomy. Can Urol Assoc J 2015;9:E594–E598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Inci K, Cil B, Yazici S, et al. Renal artery pseudoaneurysm: Complication of minimally invasive kidney surgery. J Endourol 2010;24:149e54. [DOI] [PubMed] [Google Scholar]
- 7. Gallucci M, Fortunato P, Schettini M, et al. Management of haemorrhage after percutaneous renal surgery. J Endourol 1998;12:509–512 [DOI] [PubMed] [Google Scholar]
- 8. Reed A, Suri R, Marcovich R. Passage of embolization coil through urinary collecting system one year after embolization. Urology 2007;70:1222.e17–e18 [DOI] [PubMed] [Google Scholar]
- 9. Blaut S, Zecha H, Schneider M, et al. Foreign body in proximal ureter after selective embolisation of a renal artery. Urologe A 2008;47:1607–1610 [DOI] [PubMed] [Google Scholar]
- 10. Poyet C, Grubhofer F, Zimmermann M, et al. Therapy-resistant nephrolithiasis following renal artery coil embolization. BMC Urol 2013;13:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rutchik S, Wong P. Migration of arterial embolization coils as nidus for renal stone formation. J Urol 2002;167:2520. [PubMed] [Google Scholar]
- 12. Schwartz MJ, Smith EB, Trost DW, et al. Renal artery embolization: Clinical indications and experience from over 100 cases. BJU Int 2007;99:881–886 [DOI] [PubMed] [Google Scholar]
- 13. Upadhyay SP, Zahir M, Al Muttari H, et al. A rare case of unusual migrated foreign bodies in kidney and their successful extraction using retrograde percutaneous nephrostomy. Qatar Med J 2015;2015:7. [DOI] [PMC free article] [PubMed] [Google Scholar]


